Abstract
Urinary tract infections (UTIs) are among the most frequent bacterial diseases in infants and children. Physician adherence to recommendations is notoriously often poor, but no data are available on UTIs management in the emergency setting. In this multicenter national study, we investigated the policies regarding UTIs management in children aged 2 months to 3 years in Italian emergency units. Between April and June 2021, directors of the emergency units were invited to answer an online survey on the following items: diagnostic approach to children with fever without an apparent source, therapeutic approach to UTIs, the use of kidney and urinary tract ultrasound, and the criteria for hospitalization. A total of 121 (89%) out of 139 of invited units participated in the study. Overall, units manage children with a suspected or confirmed UTI according to available recommendations for most of the items. However, in almost 80% (n = 94) of units, a sterile perineal bag is used to collect urine for culture. When urine is collected by cathether, heterogeneity exists on the threshold of bacterial load considered for UTI diagnosis.
Conclusions: Available recommendations on UTIs in children are followed by Italian emergency units for most of the items. However, the methods to collect urine specimens for culture, one of the crucial steps of the diagnostic work-up, often do not align with current recommendations and CFU thresholds considered for diagnosis largely vary among centers. Efforts should be addressed to validate and implement new child and family friendly urine collection techniques.
|
What is Known: • Several guidelines are published on the management of children with suspected or confirmed urinary tract infection. • No data are available on the management of pediatric urinary tract infections in the emergency setting. | |
|
What is New: • Almost 80% of the Italian emergency units employ a sterile perineal bag to collect urine for culture. • Diagnostic CFU thresholds largely vary among centers. |
Supplementary Information
The online version contains supplementary material available at 10.1007/s00431-022-04457-0.
Keywords: Infants, Urine, Urinary tract, Infection, Guidelines, Survey, Catheter, Emergency department
Introduction
Urinary tract infections (UTIs) are among the most common bacterial diseases in childhood. To improve their management, both national and international guidelines have been developed in the last decades [1–8]. However, physician adherence to available recommendations is often poor [9]. For instance, previous surveys among primary care physicians showed that antimicrobials are widely prescribed for outpatient UTI cases without urine culture testing [10, 11]. The difficultness associated to the urine collection might, at least in part, explain these findings [12, 13].
Although UTIs are a frequent cause of emergency unit encounters [14], no data are available on their management in this setting. Therefore, the aim of this study was to investigate the policies regarding pediatric UTIs management in emergency units.
Material and methods
We conducted a multicenter national survey (the Italian Urinary Tract Infection—ItaUTI—study) among Italian emergency units between April and June 2021. Eligible for this study were all (both general and pediatric) emergency units taking care of children.
Invitation of the units
The heads of the emergency units were invited to fill-in an online structured survey on Google Forms platform. To obtain representative, national data, all directors of the emergency units of the national society of pediatric emergency physicians (“Accademia Medica Infermieristica di Emergenza e Terapia Intensiva Pediatrica, AMIETIP”) were invited. Moreover, we invited the directors of the main emergency units of Italian provinces even if not affiliated to the AMIETIP society. Three e-mail reminders (one every two weeks) were sent. If no answer was obtained after these attempts, a phone call to the unit was performed.
Questionnaire development
The survey was initially developed by two pediatric nephrologists (G.M. and M.G.B.) and two pediatric emergency physicians (G.P.M. and F.C.) based on current Italian recommendations on UTIs management [2] on subjects aged 2 months to 3 years. A pilot test was then undertaken among 10 members or active collaborators of the scientific committee of AMIETIP. Two of them asked to modify only one question to increase its clarity (overall agreement of 95%). The final version of the questionnaire (supplementary material, section “Methods”) comprised three main sections: (1) the first section addressed the characteristics of the emergency unit including the name and town of the hospital, the total number of children and the number of children with UTIs seen on average every year, the frequency of pediatric infectious disease or kidney disease specialist consultations, and the availability of written recommendations on UTIs diagnosis and management in the emergency unit; (2) the second section investigated the diagnostic approach to children with fever without an apparent source including the use of urine dipstick in children, the urine dipstick findings considered for the diagnosis of UTI, the urine microscopy employment, the methods of urine collection for urinary dipstick and urine culture, the threshold of colony-forming units (CFU)/ml assumed for the diagnosis of UTI on urine culture, and the blood testing (e.g. blood cell count, inflammatory markers, renal function and electrolytes) in children with a suspected UTI; (3) the last section addressed policies about therapeutic approach of confirmed cases, including timing of antimicrobial prescription, choice of empiric antimicrobial treatment, the use of kidney-urinary tract ultrasound and the criteria for hospitalization. Only a single choice was possible for all questions, except for the question concerning the criteria for hospitalization for which more than one option could be selected. The answers were automatically collected into an online database and then transferred to an excel spreadsheet.
Data analysis
No missing data were expected since completion of all answers was mandatory. Categorical variables were reported as frequencies and percentages. The percentages of agreement between the policies adopted by the emergency units and recommendations from the Italian [2] and European Urology Association [1], the National Institute for Health and Care Excellence (NICE) [5], and the American Academy of Pediatrics [7, 8] guidelines were also assessed. For questions with a discrepancy > 50% between the units’ answers and the Italian guidelines recommendations, the Fisher exact test was used to assess a possible difference between units managing ≥ 100 UTIs cases per year and the other units and units with available written recommendations on UTIs diagnosis and management and the other units. A p < 0.05 was assumed as significant.
Results
Participant unit characteristics
A total of 121 (89%) out of 139 of invited units participated in the survey. The characteristics of the participating units are given in Table 1. The centers were located throughout Italy as shown in the Fig. 1.
Table 1.
Characteristics of the Italian emergency units involved in the survey
| N (%) | |
|---|---|
| Geographical area | |
| North | 62 (51) |
| Center | 25 (21) |
| South and Islands | 34 (28) |
| Number of visits per year | |
| < 5000 | 30 (25) |
| 5000–10,000 | 33 (27) |
| 10,000–20,000 | 35 (29) |
| > 20,000 | 23 (19) |
| Number of pediatric UTI managed per year | |
| < 50 | 46 (38) |
| 50–100 | 45 (37) |
| 100–200 | 14 (12) |
| > 200 | 16 (13) |
| Frequency of consultation with a pediatric infectious disease specialist for UTI management | |
| Never | 109 (90) |
| < 50% | 0 (0.0) |
| ≥ 50% | 0 (0.0) |
| Always | 12 (10) |
| Frequency of consultation with a pediatric nephrologist for UTI management | |
| Never | 75 (62) |
| < 50% | 33 (27) |
| ≥ 50% | 9 (7.4) |
| Always | 4 (3.3) |
| Availability of recommendations on UTI management | |
| Yes | 90 (74) |
| No | 31 (26) |
Fig. 1.
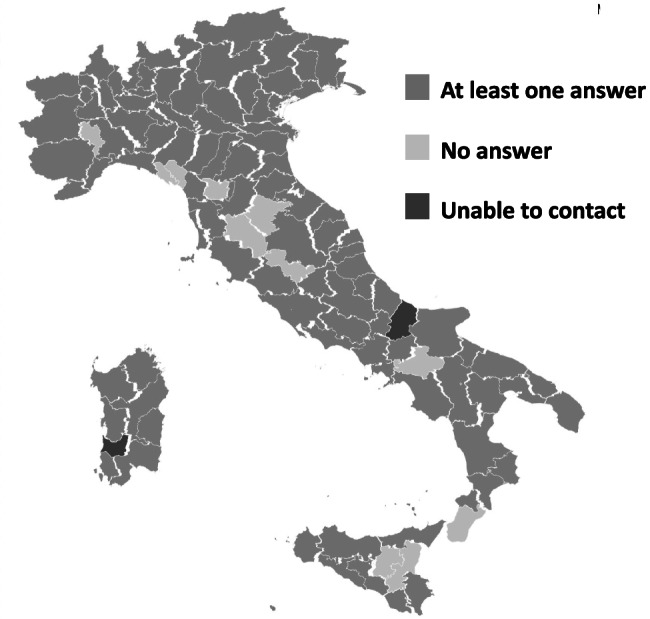
Italian provinces with at least one unit invited: in grey color those with at least one participant center, in light gray color those without any participating unit. We were not able to invite any unit in two provinces (dark gray color)
Diagnostic approach to pediatric UTIs
Urinary dipstick
In the majority (N = 102, 84%) of units, a urine dipstick is always performed in the diagnostic work-up of a febrile child with no apparent source. In 14% of the units, a urinary dipstick is performed in ≥ 50% of cases, while in 2 units in < 50% of cases. For this purpose, a sterile perineal bag is employed in 95% (N = 115) of the units and in only 4 (3.3%), a clean catch is used. The concurrent positivity for leukocyte esterase and nitrites is considered for the diagnosis of UTIs in 76% of units and the positivity for only leukocyte esterase in 13%.
Urine culture
In more than three quarter of units (n = 94, 78%), a sterile perineal bag is used to collect urine for culture. In only 16 (13%) and 9 (11%) of the units, either a bladder catheter or a clean catch of urine is chosen, respectively.
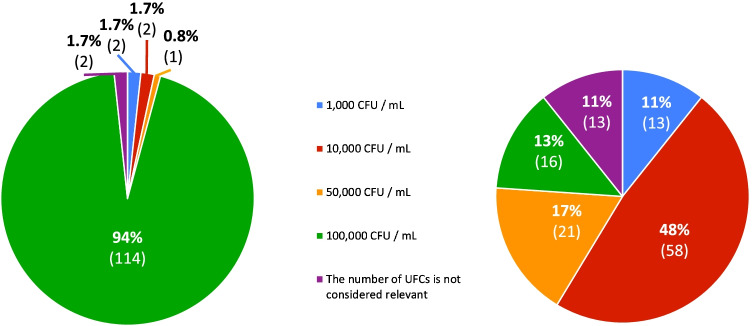
The CFU/ml thresholds adopted for the diagnosis of UTI are shown in Fig. 2: overall, 94% of centers consider 100.000 CFU/ml in specimens collected by sterile perineal bag and 50% consider 10.000 CFU/ml in specimens collected by bladder catheter.
Fig. 2.
Left: bacterial load (colony-forming units/ml) considered diagnostic for urinary tract infection in urine collected by perineal bag. Right: bacterial load (colony-forming units/ml) considered diagnostic in urine collected by bladder catheter
Further investigations
Microscopic urinalysis is never performed in 33 (27%) units. On the contrary, in 30 (25%) units, it is always requested in the diagnostic work-up of UTIs. Blood tests are always performed in 45% (N = 56) of the units and never in only 7% (N = 8).
Therapeutic approach and management of confirmed cases of UTIs
Antimicrobial therapy
An antimicrobial treatment is prescribed immediately after urine collection for culture in the majority (N = 105, 87%) of units. On the contrary, antimicrobial treatment is immediately prescribed without urine collection for bacteriological studies in a low percentage (N = 4, 3.3%) of units. Amoxicillin-Clavulanic acid is prescribed as first-line empiric treatment (N = 105, 87%) at a dosage between 50 and 90 mg/kg body weight (N = 100, 95%) in most units. Amoxicillin alone is used by a minority of units (N = 10, 8.3%).
Criteria for hospitalization
The criteria adopted for hospitalization are given in Table 2. The persistence of fever despite a 3-day course of antimicrobial treatment and an expected poor adherence to treatment are the most common criteria implemented in most units (83% and 78%, respectively).
Table 2.
Criteria for hospitalization of children with UTIs. The question allowed multiple answers
| N (%) | |
|---|---|
| Persistence of fever despite an appropriate 3-day course of antimicrobial treatment | 101 (84) |
| Expected poor adherence to treatment | 94 (78) |
| Age < 6 months | 72 (59) |
| Fever with chills | 59 (48) |
| Children on antibiotic prophylaxis for previous UTIs episodes | 54 (45) |
| Age < 12 months | 22 (18) |
Kidney and urinary tract ultrasound
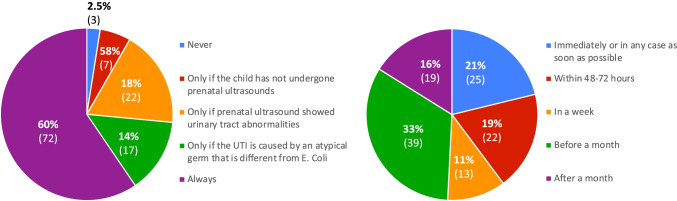
Most units (N = 72, 60%) always perform a kidney and urinary tract ultrasound following the first episode of UTI. A total of 22 units (18%) perform an ultrasound only in children with pathological prenatal ultrasound findings and 17 (14%) if UTI is caused by microorganism other than E. coli. Approximately 40% (N = 47) of units perform ultrasound immediately or within 48–72 h and 19 (16%) one month after the UTI episode (Fig. 3). The remaining results are reported in the online supplementary material.
Fig. 3.
Left: indications for kidney-urinary tract ultrasound in a febrile child in a good condition with a first episode of UTI. Right: timing of kidney-urinary tract ultrasound
The agreement between the policy adopted by the emergency units and the recommendations of the Italian and European Urology Association, the NICE, and the American Academy of Pediatrics guidelines and are given in Table 3. The features considered in the urinary dipstick for the diagnosis of an upper urinary tract infection in a febrile child, the method used for urine collection for culture, the bacterial load considered diagnostic for a UTI in urine, the request of blood exam and the timing of kidney and urinary tract ultrasound were the items with a discrepancy > 50% between the Italian guidelines and units’ answers. Units managing ≥ 100 UTIs yearly used more frequently bladder catheterization to collect urine compared to the other units (27% vs 8.8%, p = 0.02). No other difference was observed for units managing ≥ 100 UTIs or those with the availability of written recommendations on the other items.
Table 3.
Agreement between available recommendations on UTIs for children and the policies of the emergency units (N = 121) included in the survey
| Item | Italian guidelines | AAP guidelines | NICE guidelines | European Society of Urology guidelines |
|---|---|---|---|---|
| Collection of a urinary dipstick in subjects with fever without an apparent source of infection | 84% | NA | 84% | 84% |
| Urine collection for urinary dipstick | 98% | 1.6% | 98% | 98% |
| Features considered in the urinary dipstick for the diagnosis of an upper urinary tract infection in a febrile child | 13% | 13% | 75% | 75% |
| Urine collection for culture | 13% | 13% | 9.1% | 13% |
| Bacterial load considered diagnostic for a UTI in urine collected by perineal sterile bag | 94% | NA | NA | NA |
| Bacterial load (colony-forming units / CFU) considered diagnostic for a UTI in urine collected by bladder catheter | 48% | 17% | 11% | 59% |
| Blood exams | 24% | 24% | 24% | NA |
| Empirical antimicrobial oral treatment | 87% | 87% | 87% | 4.9% |
| Dosage of oral Amoxicillin Clavulanate | 88% | 0.8% | 88% | NA |
| Timing of antimicrobial oral treatment | 87% | NA | 87% | 87% |
| Kidney and urinary tract ultrasound at the first UTI episode | 60% | 60% | 14%a | 60% |
| Timing of kidney and urinary tract ultrasound | 33% | 49% | NA | 21% |
NA not applicable, AAP American Academy of Pediatrics, NICE National Institute for Health and Care Excellence
a Kidney and urinary tract ultrasound is also recommended in cases > 6 months of age
Discussion
Here, we report the first study investigating the diagnosis and management of pediatric UTIs in the emergency units. The findings of this nationwide survey, which had a remarkably good response rate at almost 90%, point out that children aged 2 months to 3 years with a suspected or confirmed UTI are mostly managed according to currently available recommendations.
On the other hand, the survey shows that the adopted techniques to collect urine for culture are often not performed in accordance with the guidelines, and CFU thresholds for diagnosis vary among centers.
The discussion will focus on three points of the survey: 1. the diagnostic work-up, 2. the criteria for hospitalization, 3. the therapeutic approach.
In febrile infants without an apparent source of fever, urinalysis is currently recommended by many authorities [1–3]. In line with this advice, our study shows that in most of the Italian emergency units (84%), a urine dipstick is obtained in children without an apparent source of fever. However, some units do not routinely perform a urine dipstick in these patients. The latter finding should be considered since the rule-out of a UTI may be helpful to establish the likelihood of a viral infection and avoid an overprescription of antimicrobials.
The evidence of pyuria is currently considered more relevant than the presence of nitrituria in the diagnostic workup of UTIs [2]. Most units require the positivity for both pyuria and nitrituria to rule in a diagnosis of UTIs, while a minority of units considers leucocytes only. This attitude likely reflects that currently available dipsticks determine both parameters. Considering the tendency to overprescribe antimicrobials [15], future studies should investigate the impact of these different attitudes on the management of suspected cases of UTI.
The growth of pathogens in an uncontaminated urine specimen is the cornerstone for UTI diagnosis [16]. For this purpose, bladder catheterization and suprapubic puncture are considered the gold standard to collect urine both in infants and in not-toiled trained children [2]. Due to the risk of contamination, the current guidelines advise against the use of perineal bag [1–8]. This survey shows that sterile perineal bag is used in most of the emergency units. This finding is in line with figures observed among European primary care physicians [10]. It is fairly predictable that invasive techniques such as bladder catheterization and suprapubic puncture might be challenging in the outpatients setting. However, the widespread use of perineal bag also in the emergency units suggests that this attitude is likely an ingrained habit among pediatricians. Emergency care providers would rather rarely employ bladder catheterization or suprapubic puncture likely because these are personnel and time intensive, and a possible source of pain for children and distress for caregivers [17, 18]. New strategies, such as the collection of urine from nappy pad or bladder stimulation technique to obtain midstream urine, might be an interesting and promising alternative [16, 19]. We suggest that the emergency units review their practice by considering and validating new urine collection methods for culture that may be effective and safe also in centers with limited staffing and resources, and in small centers.
As for the CFU cut-off for UTI diagnosis, the standard threshold of ≥ 105 CFU/ml on urine obtained in a sterile perineal bag is utilized by almost all units. The threshold for urine collected by more invasive procedures is heterogenous. These data confirm that no consensus exists as to what threshold should be considered for the diagnosis of UTIs [20] and new studies are needed to define this gap of knowledge.
More and more data suggest that children affected by a febrile UTI can be feasibly managed as outpatients [21]. The results of our survey are in line with this approach, because only an expected poor adherence to treatment and fever persistence despite an appropriate 3-day antimicrobial course are reasons for hospitalization in most units.
The results of this study point out that oral Amoxicillin, alone or more frequently associated with Clavulanate, is the empirical treatment prescribed by most emergency units. This policy likely reflects the fact that in Italy, four out of five community acquired childhood UTIs are caused by E. coli and ~ 70% of these pathogens are sensitive to Amoxicilline-Clavalunate [22].
This study has limitations and strengths. First, our questionnaire was pilot tested but not validated. Second, the responses are based on self-reports and might not fully reflect the day-to-day clinical practice. Future studies with data from medical records of the patients might further support the results of this study and quantitate the magnitude of overtreatment associated with the use of perineal bag instead of that of bladder catheter for urine culture. Third, the study was limited to diagnosis and management of UTIs within Italian emergency units and not all the Italian units and scientific societies were invited. Finally, we did not investigate if units followed Italian or other guidelines on UTI. The major strength is that this nationwide inquiry benefited from a response rate of about 90%. Information was gathered from units throughout all Italy including both small and large emergency units. Finally, almost all aspects of UTI management in children aged 2 months to 3 years in the acute setting were investigated.
In conclusion, this study shows that currently available recommendations on UTIs in children are followed by Italian emergency units for most of the items. On the other hand, the methods to collect urine specimens for culture, one of the crucial steps for UTI diagnosis, are not performed according to the recommendations and CFU thresholds are heterogenous. Efforts should be addressed to develop and validate new child and family friendly urine collection techniques.
Supplementary information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the Accademia Medica Infermieristica di Emergenza e Terapia Intensiva Pediatrica (AMIETIP) and especially Dr. Marco Binotti for the support to perform the study.
Abbreviations
- AAP
American Academy of Pediatrics
- NA
Not applicable
- NICE
National Institute for Health and Care Excellence
- UTI
Urinary tract infection
Authors’ contributions
GPM and GM conceptualized the study. FC, GPM, MGB, AM, and GM designed the study. All authors contributed to data interpretation. FC, GPM, MGB, and GM drafted the initial manuscript, and revised the manuscript. All authors critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted.
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. This work was supported by the Italian Ministry of Health, grant “Ricerca corrente 2020.”
Availability of data and material
Upon reasonable request to the corresponding author.
Declarations
Ethics approval
Not required for this study.
Consent to participate
Participants gave their consent to participate.
Consent for publication
All authors gave their consent for publication. No further consent is required.
Competing interests
The authors declare no competing interests.
Footnotes
The original online version of this article was revised: The Collaborators' name under "ItaUTI study group" has been added.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Francesca Cenzato and Gregorio P. Milani equally contributed to the study
Change history
7/18/2022
Missing Open Access funding information has been added in the Funding Note.
Change history
4/28/2022
A Correction to this paper has been published: 10.1007/s00431-022-04479-8
Contributor Information
Francesca Cenzato, Email: dr.francesca.cenzato@gmail.com.
Gregorio P. Milani, Email: milani.gregoriop@gmail.com
Angela Amigoni, Email: angela.amigoni@aopd.veneto.it.
Francesca Sperotto, Email: francesca.sperotto@gmail.com.
Mario G. Bianchetti, Email: mario.bianchetti@usi.ch
Carlo Agostoni, Email: carlo.agostoni@unimi.it.
Giovanni Montini, Email: giovanni.montini@unimi.it.
on behalf of the ItaUTI study group:
Giovanni Farello, Francesco Chiarelli, Rita Greco, Franco Di Lollo, Fabio Rocco Forte, Sergio Manieri, Luigi Carpino, Mimma Caloiero, Anastasia Cirisano, Salvatore Braghò, Roberto Della Casa, Felice Nunziata, Carmine Pecoraro, Rosario Pacifico, Marcello Lanari, Chiara Ghizzi, Laura Serra, Marcello Stella, Giuseppe Maggiore, Roberto Fiorini, Icilio Dodi, Andrea Morelli, Lorenzo Lughetti, Andrea Cella, Gianluca Vergine, Alessandro De Fanti, Danica Dragovic, Daniele Santori, Giorgio Cozzi, Paola Cogo, Marilena Raponi, Riccardo Lubrano, Mauro de Martinis, Antonio Gatto, Maria Antonietta Barbieri, Antonino Reale, Giorgio Bracaglia, Emanuela Piccotti, Riccardo Borea, Alberto Gaiero, Laura Martelli, Alberto Arrighini, Paola Cianci, Claudio Cavalli, Leonardina De Santis, Benedetta Chiara Pietra, Andrea Biondi, Marco Sala, Laura M. Pogliani, Simonetta Cherubini, Marta Bellini, Paola Bruni, Giovanni Traina, Paola Tommasi, Paolo Del Barba, Sergio Arrigoni, Filippo M. Salvini, Luca Bernardo, Giuseppe Bertolozzi, Silvia Fasoli, Gian Luigi Marseglia, Emilio Palumbo, Annalisa Bosco, Gianpaolo Mirri, Elisabetta Fabiani, Ermanno Ruffini, Luisa Pieragostini, Martina Fornaro, Gabriele Ripanti, Donnina Pannoni, Felici Enrico, Anna Perona, Eleonora Tappi, Oscar Nis Haitink, Ivana Rabbone, Pina Teresa Capalbo, Antonio Urbino, Andrea Guala, Gianluca Cosi, Maria Gabriella Barracchia, Baldassarre Martire, Fabio Cardinale, Fulvio Moramarco, Carmelo Perrone, Angelo Campanozzi, Valerio Cecinati, Alessandro Canetto, Ciro Clemente, Antonio Cualbu, Fabio Narducci, Giuseppina Mula, Pasquale Bulciolu, Roberto Antonucci, Giuseppe Gramaglia, Giuseppe Cavaleri, Carmelo Salpietro, Giovanni Corsello, Rosario Salvo, Marcello Palmeri, Maria Assunta Vitale, Ambra Morgano, Susanna Falorni, Diego Peroni, Stefano Masi, Alessio Bertini, Angelina Vaccaro, Pierluigi Vasarri, Petra Reinstadler, Massimo Soffiati, Maurizio Stefanelli, Alberto Verrotti di Pianella, Catherine Bertone, Stefano Marzini, Liviana Da Dalt, Simone Rugolotto, Floriana Scozzola, Luca Ecclesio Livio, Mauro Cinquetti, Davide Silvagni, and Massimo Bellettato
References
- 1.'t Hoen LA, Bogaert G, Radmayr C, Dogan HS, Nijman RJM, Quaedackers J, Rawashdeh YF, Silay MS, Tekgul S, Bhatt NR, Stein R (2021) Update of the EAU/ESPU guidelines on urinary tract infections in children. J Pediatr Urol 17:200–207 [DOI] [PubMed]
- 2.Ammenti A, Alberici I, Brugnara M, Chimenz R, Guarino S, La Manna A, La Scola C, Maringhini S, Marra G, Materassi M, Morello W, Nicolini G, Pennesi M, Pisanello L, Pugliese F, Scozzola F, Sica F, Toffolo A, Montini G (2020) Italian Society of Pediatric Nephrology. Updated Italian recommendations for the diagnosis, treatment and follow-up of the first febrile urinary tract infection in young children. Acta Paediatr 109:236–247 [DOI] [PMC free article] [PubMed]
- 3.Buettcher M, Trueck J, Niederer-Loher A, Heininger U, Agyeman P, Asner S, Berger C, Bielicki J, Kahlert C, Kottanattu L, Meyer Sauteur PM, Paioni P, Posfay-Barbe K, Relly C, Ritz N, Zimmermann P, Zucol F, Gobet R, Shavit S, Rudin C, Laube G, von Vigier R, Neuhaus TJ. Swiss consensus recommendations on urinary tract infections in children. Eur J Pediatr. 2021;180:663–674. doi: 10.1007/s00431-020-03714-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen R, Raymond J, Faye A, Gillet Y, Grimprel E (2015) Société française de pédiatrie; Société de pathologie infectieuse de langue française. Management of urinary tract infections in children. Recommendations of the Pediatric Infectious Diseases Group of the French Pediatrics Society and the French-Language Infectious Diseases Society. Arch Pediatr 22:665–671 [DOI] [PubMed]
- 5.Baumer JH, Jones RW. Urinary tract infection in children, National Institute for Health and Clinical Excellence. Arch Dis Child Educ Pract Ed. 2007;92:189–192. doi: 10.1136/adc.2007.130799. [DOI] [PubMed] [Google Scholar]
- 6.Hewitt IK, Montini G. Childhood urinary tract infections: a Swedish perspective and comparison with other published guidelines. Acta Paediatr. 2021;110:1708–1710. doi: 10.1111/apa.15779. [DOI] [PubMed] [Google Scholar]
- 7.Roberts KB (2011) Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics 128(3):595–610 [DOI] [PubMed]
- 8.Subcommittee On Urinary Tract Infection (2016) Reaffirmation of AAP clinical practice guideline: the diagnosis and management of the initial urinary tract infection in febrile infants and young children 2–24 months of age. Pediatrics 138:e20163026 [DOI] [PubMed]
- 9.Barth JH, Misra S, Aakre KM, Langlois MR, Watine J, Twomey PJ, Oosterhuis WP. Why are clinical practice guidelines not followed? Clin Chem Lab Med. 2016;54:1133–1139. doi: 10.1515/cclm-2015-0871. [DOI] [PubMed] [Google Scholar]
- 10.Hadjipanayis A, Grossman Z, Del Torso S, van Esso D, Dornbusch HJ, Mazur A, Drabik A, Montini G. Current primary care management of children aged 1–36 months with urinary tract infections in Europe: large scale survey of paediatric practice. Arch Dis Child. 2015;100:341–347. doi: 10.1136/archdischild-2014-306119. [DOI] [PubMed] [Google Scholar]
- 11.Selekman RE, Sanford MT, Ko LN, Allen IE, Copp HL. Does perception of catheterization limit its use in pediatric UTI? J Pediatr Urol. 2017;13:48.e1–48.e6. doi: 10.1016/j.jpurol.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Kaufman J, Sanci L, Temple-Smith M (2020) What’s the catch? Urine sample collection from young pre-continent children: a qualitative study in primary care. BJGP Open 4:bjgpopen20X101060 [DOI] [PMC free article] [PubMed]
- 13.Selekman RE, Allen IE, Copp HL. Determinants of practice patterns in pediatric UTI management. J Pediatr Urol. 2016;12:308.e1–308.e6. doi: 10.1016/j.jpurol.2016.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montini G, Tullus K, Hewitt I. Febrile urinary tract infections in children. N Engl J Med. 2011;365:239–250. doi: 10.1056/NEJMra1007755. [DOI] [PubMed] [Google Scholar]
- 15.Covino M, Buonsenso D, Gatto A, Morello R, Curatole A, Simeoni B, Franceschi F, Chiaretti A (2022) Determinants of antibiotic prescriptions in a large cohort of children discharged from a pediatric emergency department. Eur J Pediatr. Online ahead of print. [DOI] [PMC free article] [PubMed]
- 16.Harkensee C, Clennett J, Wilkinson S, Tse Y. Diagnosing urinary tract infection in children: time to ditch the pad? Arch Dis Child. 2021;106:935–936. doi: 10.1136/archdischild-2020-320290. [DOI] [PubMed] [Google Scholar]
- 17.Kleiber C, McCarthy AM. Parent behavior and child distress during urethral catheterization. J Soc Pediatr Nurs. 1999;4:95–104. doi: 10.1111/j.1744-6155.1999.tb00042.x. [DOI] [PubMed] [Google Scholar]
- 18.Kaufman J. How to… collect urine samples from young children. Arch Dis Child Educ Pract Ed. 2020;105:164–171. doi: 10.1136/archdischild-2019-317237. [DOI] [PubMed] [Google Scholar]
- 19.Demonchy D, Ciais C, Fontas E, Berard E, Bréaud J, Rohrlich PS, Dubos F, Fortier C, Desmontils J, Hérisse AL, Donzeau D, Haas H, Tran A (2019) Evaluation of bladder stimulation as a non-invasive technique for urine collection to diagnose urinary tract infection in infants under 6 months: a randomized multicenter study ("EE-Sti.Ve.N"). Trials 20:783 [DOI] [PMC free article] [PubMed]
- 20.Doern CD, Richardson SE. Diagnosis of urinary tract infections in children. J Clin Microbiol. 2016;54:2233–2242. doi: 10.1128/JCM.00189-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hensey CC, Sett A, Connell TG, Bryant PA. A comparison of hospital versus outpatient parenteral antibiotic therapy at home for pyelonephritis and meningitis. Pediatr Infect Dis J. 2017;36:827–832. doi: 10.1097/INF.0000000000001605. [DOI] [PubMed] [Google Scholar]
- 22.Calzi A, Grignolo S, Caviglia I, Calevo MG, Losurdo G, Piaggio G, Bandettini R, Castagnola E. Resistance to oral antibiotics in 4569 Gram-negative rods isolated from urinary tract infection in children. Eur J Pediatr. 2016;175:1219–1225. doi: 10.1007/s00431-016-2763-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Upon reasonable request to the corresponding author.