Abstract
This article reports a case of glandular odontogenic cyst in a 70-year-old male and discusses the clinical, radiological and histopathological features. The present case shows treatment of GOC which effected the body of mandible with infiltration into submandibular gland.
Keywords: Glandular odontogenic cyst, Mucoepidermoid carcinoma, GOC, MEC, Mucous cells
Introduction
Glandular odontogenic cyst (GOC), relatively a rare cyst occurring in tooth-bearing areas, was first described by Padayachee and Van Wyk et al. (1987) in two cases presenting features of both botryoid odontogenic cyst and central mucoepidermoid tumor [1, 4]. In 1988, Gardener based upon clinical, radiological and histological features suggested this cyst to be odontogenic in origin [4]. Classification of WHO head and neck tumors(1992) suggests GOC is a developmental cyst with epithelial features that simulate salivary gland [2]. Due to similar microscopic and clinical features of GOC to other lesions, a proper differential diagnosis is imperative and should include central giant cell granuloma for anterior lesions and ameloblastoma or odontogenic keratocyst (OKC) for posterior lesions [3]. GOC is known for its aggressive behavior, attributed to the rate of recurrence which has been reported as high as 30% and often compromised cortical integrity [7]. GOC can be easily misdiagnosed microscopically as a mucoepidermoid carcinoma(MEC) [7]. MEC is the most common malignant salivary gland tumor with 8% to 13% in the submandibular gland region [5].
This article reports a case of glandular odontogenic cyst in a 70-year-old male and discusses the clinical, radiological and histopathological features. The present case shows treatment of GOC which affected the body of mandible with infiltration into submandibular gland (Figs. 1, 2, 3, 4, 5, 6, 7).
Fig. 1.

Extraoral swelling in right submandibular region
Fig. 2.

Intraoral swelling over right retromolar trigone (pre-op)
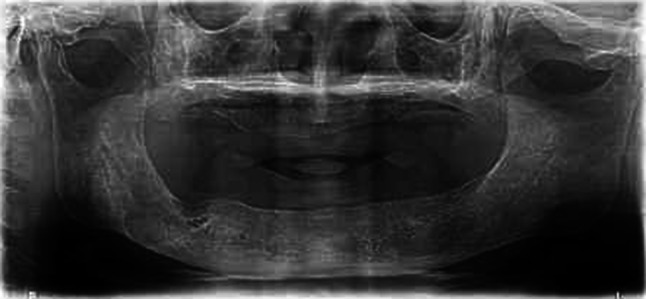
Fig. 3.

OPG showing two radiolucencies in the retromolar area (pre-op)
Fig. 4.

Surgical specimen showing excised cystic lesion along with salivary gland
Fig. 5.
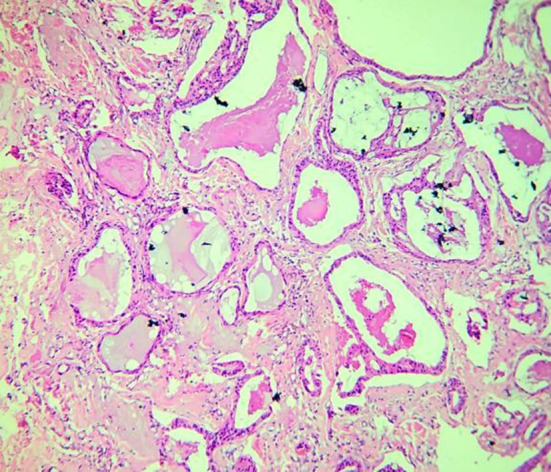
H&E stained sections showing numerous areas of mucous pooling lined by epithelial cells and some areas of ductal-like formations
Fig. 6.
Twenty-month postoperative radiograph showing diffuse margins of the excised lesion with interlaced diffuse pattern of trabeculae in the right retromolar area
Fig. 7.
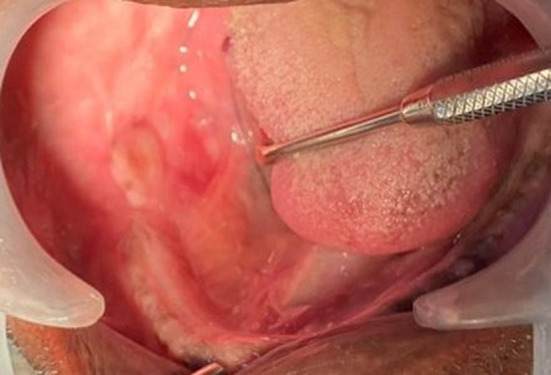
Postoperative intraoral view after twenty months
Case Report
A 70-year-old Indian male patient reported to our unit with the chief complaint of pain and swelling in the right lower back region of jaw since 6 months, with a history of gradual increase in size. Extraorally, a well-recognizable swelling of 3 cm anterio-posteriorly and 2 cm medio-laterally was noted in right submandibular region. Medially swelling did not cross the midline. On intraoral examination, a complete edentulous arch with pale overlying mucosa was seen. The swelling involved medial side of the mandible extending to the floor of the mouth. It was palpable from the premolar region to the retromolar trigone. The swelling was firm, had a lobulated border and measured around 3 × 5 cm, with slight elevation over right sublingual region. Nerve paresthesia was absent. Mouth opening was 45 mm.
Opg showed two, well-defined unilocular radiolucencies measuring around 2 × 2cm seen over the posterior alveolus in the fourth quadrant suggestive of cystic lesion.
Based on the clinical and radiological presentation, provisionally suggestive of cystic lesion, an incisional biopsy was done, and decorticated thin buccal cortex was removed with a portion of the cystic lining. The samples were submitted for histological examination with differential diagnosis of GOC, MECC, KCOT. Histopathological analysis was suggestive of GOC.
Patient was subjected to enucleation and curettage followed by chemical cauterization using Carnoy’s solution, under general anesthesia by an extraoral submandibular approach. The facial artery and the vein were identified and ligated. Hypoglossal nerve was preserved, and the submandibular duct was identified and ligated. The deep part of the gland was separated from the surrounding tissue by blunt dissection, and the entire gland was removed. Cyst was filled with mucin and gel-like fluid, and an evidence of bone resorption of the medial side of the mandible was seen. Drain was placed and the closure achieved. No complications were noted, and the patient was discharged on third day. Patient shows no signs of recurrence with 20 months of follow-up.
Final histopathological report suggestive of GOC after immunofluorescence confirmed cytokeratin 19 antibody to establish odontogenic origin of lesion.
Discussion
GOC, accounting for 0.012–1.3% of all jaw cysts, is recently recognized as a rare developmental odontogenic cyst with age range of 14-75, mean 45.7 and most often M/F ratio being 1.3:1. GOC has a predilection for mandible (70%), affecting both anterior and posterior areas, and most often cortical plate integrity is compromised in 85.4% of cases [4, 7]. On aspiration, clear and low viscosity fluid content may be a helpful clinical indication of GOC [6].
Table 1 shows the histopathological criteria for diagnosis by Kaplan et al. [7] which suggests that at least the focal presence of each of the major criteria is mandatory, whereas the minor criteria need not be present for the diagnosis but may just support it.
Table 1.
Histopathological diagnostic criteria given by Kaplan et al. [7]
| Major criteria | Minor criteria |
|---|---|
|
Non–keratinized squamous epithelial lining with a flat interface Presence of “spherules”/knobs or “whorls” or focal luminal proliferations Epithelial lining exhibits surface cuboidal eosinophilic cells or “hob–nail” cells Mucous/goblet cells with intraepithelial mucous pools with or without crypts lined by mucous-producing cells Intraepithelial glandular microcystic or duct–like (pseudoglandular) structures |
Papillary proliferation Ciliated cells Multicystic or multiluminal architecture Clear or vacuolated cells in basal or spinous layer |
The mucous cells are stained positively by periodic acid Schiff (PAS) stain and are considered to be a result of metaplasia. These metaplastic mucous cells are generally seen in many other odontogenic cysts; however, in GOCs they are seen in abundance. The vacuolated and clear cells observed near the mucous cells may represent an initial stage in the histogenesis of mucus cell metaplasia [3].
Many of the histological features overlap with lesions of less aggressive nature, yet a higher frequency or in the case of low-grade MEC, potentially more dangerous lesions occur with lesser frequency. As with other aggressive pathologic lesions, GOC tends to recur with a rate directly related to the size of the lesion, 14.4% in small lesions as in contrast to 85.6% in larger lesions if treated with enucleation or curettage alone, while other modalities like peripheral ostectomy or segmental resection can significantly reduce the recurrence rate [7, 8].
Conclusion
It shows varying clinical and radiographic findings, and its diagnosis depends on its microscopic features. Histopathologically, it may prove to be a diagnostic dilemma due to its close resemblance to BOC, dentigerous cyst and most importantly MEC. It is mandatory to differentiate GOC from the much more aggressive lesions like MEC, and we recommend the use of cytokeratin 19 antibody to establish odontogenic origin when in doubt [9, 10].
Funding
Nil.
Compliance with Ethical Standards
Conflict of interest
There are no conflict of interest.
Informed Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patient understands that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Padayachee A, Van Wyk CW. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol. 1987;16:499–504. doi: 10.1111/j.1600-0714.1987.tb00680.x. [DOI] [PubMed] [Google Scholar]
- 2.Speight P, Fowler CB, Kessler H. Glandular odontogenic cyst. In: El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ, editors. World health organization classification of head and neck tumours. 4. Lyon: IARC Press; 2017. pp. 238–239. [Google Scholar]
- 3.Krishnamurthy A, Sherlin HJ, Ramalingam K, Natesan A, Premkumar P, Ramani P, et al. Glandular odontogenic cyst: report of two cases and review of literature. Head Neck Pathol. 2009;3:153–158. doi: 10.1007/s12105-009-0117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah AA, Sangle A, Bussari S, Koshy AV. Glandular odontogenic cyst: a diagnostic dilemma. Indian J Dent. 2016;7:38–43. doi: 10.4103/0975-962X.179371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neville WB, Damm DD, Allen CM, et al. Salivary gland pathology. Oral Maxillofacial Pathol. 2002;105:420–423. [Google Scholar]
- 6.Osny FJ, Azevedo LR, Santana E, Lara VS. Glandular odontogenic cyst: case report and review of the literature. Quintessence Int. 2004;35:385–389. [PubMed] [Google Scholar]
- 7.Kaplan I, Anavi Y, Hirshberg A. Glandular odontogenic cyst: a challenge in diagnosis and treatment. Oral Dis. 2008;14:575–581. doi: 10.1111/j.1601-0825.2007.01428.x. [DOI] [PubMed] [Google Scholar]
- 8.Barth CT, Chamberlain JA, III, Wessel JR. Treatment of a mandibular glandular odontogenic cyst with peripheral ostectomy, bone allograft, and implant reconstruction: a case report. Int J Periodontics Restorative Dent. 2017;37(4):245. doi: 10.11607/prd.2885. [DOI] [PubMed] [Google Scholar]
- 9.Anchlia S, Bahl S, Shah V, Vyas S. Glandular odontogenic cyst: a rare entity revealed and a review of the literature. BMJ Case Rep. 2015;5:45–51. doi: 10.1136/bcr-2015-211502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mascitti M, Santarelli A, Sabatucci A, Procaccini M, Lo Muzio L, Zizzi A, et al. Glandular odontogenic cyst: review of literature and report of a new case with cytokeratin-19 expression. Open Dent J. 2014;8:1–12. doi: 10.2174/1874210601408010001. [DOI] [PMC free article] [PubMed] [Google Scholar]


