Abstract
Eagle’s syndrome was first described with all signs and symptoms by W. W. Eagle in the year 1949. It was characterized by abnormal ossification of styloid process leading to either morphological increase in the length of the styloid process itself or abnormal calcification of the stylohyoid ligament. It has been reported in patients of fourth to sixth decade. The surgical management of removal of the elongated styloid was first performed in 1842 even before Eagle’s syndrome was completely understood. The establishment of the diagnosis is a challenge in itself as we need to differentiate it from the neuralgias such as glossopharyngeal neuralgia and superior laryngeal neuralgias. Furthermore, the decision of whether to operate or not is another dilemma in itself. We report a case of a 19-year-old girl with classic Eagle’s syndrome along with the transcervical surgical management of the same.
Keywords: Stylohyoid ligament, Reichert’s cartilage, Eagle’s syndrome, Transcervical approach, Carotid styloid syndrome
Introduction
Eagle’s syndrome, first noted in 1652 by Pietro Marchetti, was described by W. W. Eagle in 1949 [1, 2] as abnormal ossification of styloid process leading to morphological increase in the length of the styloid process or abnormal calcification of the stylohyoid ligament causing unexplained pain in throat, anterior part of the neck which radiates to the ear. Complaints of deglutition and dysphonia have also been reported [1, 3]. Majority of patients are handled symptomatically in pain clinics as many go undiagnosed because the diagnosis itself is a challenge. We present a case of Eagle’s surgically treated through transcervical approach with adequate approval from patient and review board of CIMS.
The average length of the styloid process has been determined to be 15.4–18.8 mm in Asian population and 20–30 mm in Caucasian population [1, 4]. The incidence of the presentation is about 4 to 8 per 10,000 individuals.
Etiology and Its Various Hypotheses
The elongated styloid process is mainly considered to be anomalous persistent embryonic cartilaginous outgrowth of the Reichert’s cartilage or the cartilage of the second pharyngeal arch. However, another school of thought exists where it is thought that the stylohyoid ligament could be calcified or bony formation could occur at the insertion of the ligament to the lesser cornu of the hyoid bone [1, 5, 6].
Case Report
A 19-year-old girl presented with gnawing pain in the right submandibular region, aggravated on swallowing for past 2 years. On turning her head to the left, she had a feeling of a foreign body poking in her right side of the throat. She was treated with analgesics and antibiotics at various centers and pain clinics. On clinical examination, no abnormality was present in the neck, thyroid, ear, sinuses or lymph nodes. Thorough intraoral examination had been performed to rule out any source of dental infection and was unremarkable.
The OPG showed elongated radio-opacity just behind the angle of mandible (Fig. 1). The 3D CT of face depicted right styloid was longer with calcification of the stylohyoid ligament (Fig. 2).
Fig. 1.
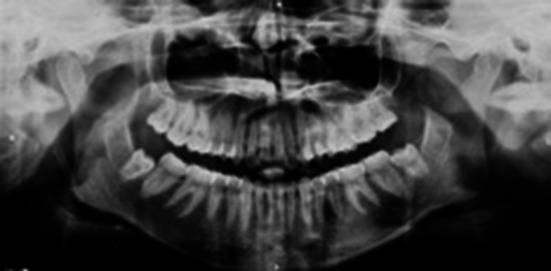
Preoperative OPG appreciating the elongated styloid process behind the posterior border of right-side mandible
Fig. 2.
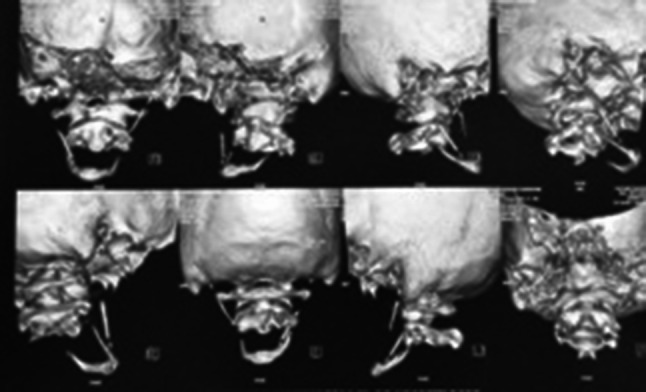
Preoperative 3D CT recon of face showing spatial relation of elongated styloid process and the stylohyoid apparatus
The surgery for elective removal of right styloid process was performed transcervically. The digastric muscle was retracted superiorly and hypoglossal nerve anteriorly for exposure. The aberrant calcification was rongeured as cephalic as possible and closure was performed. Immediate postoperatively no weakness of hypoglossal or marginal mandibular nerve was noted. The immediate postoperative OPG (Fig. 3) showed the absence of styloid process. Four months postoperative, patient had no notable complaints.
Fig. 3.
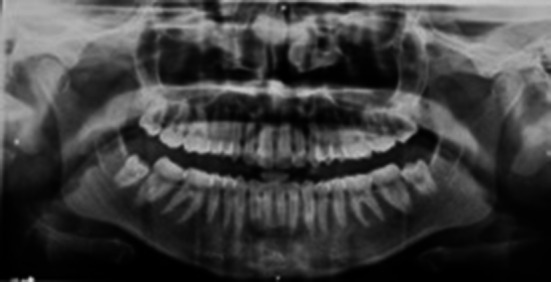
Postoperative OPG showing the absence of the styloid process of the right side
Discussion
Eagle’s syndrome and its clear sign and symptoms were described by W. W. Eagle in 1949 [1]. It is furthermore of interest that surgical management of removal of the elongated styloid was first performed in 1842 even before Eagle’s syndrome was completely understood [7, 8]. It has been well documented that about 19% of the general population have an elongated styloid process, but only 6% of the affected are symptomatic with males being more affected than females [1, 9–12]. Eagle’s syndrome is generally observed in fourth to sixth decade. Individuals of a younger age being diagnosed of the same are rarely reported.
Among the various radiographs for viewing the elongated styloid process, most used were pantomographs and lateral oblique view of skull as well as Towne’s view. However after advent of 3D CT, it has now become the gold standard for both radiographic examination and evaluation. In the ortho-pantomograph, the major disadvantage at times was the superimposition of the mandible and dentition over the styloid process and thus not only identifying the styloid process but also evaluating the length of it is very difficult [13]. Three-dimensional CT thus does have an advantage in this respect as complete evaluation of the Eagle’s syndrome in spatial geometry is possible and also facilitates the accurate measurement of the elongated styloid [13].
Langlais et al. [14] classified the elongated styloid process as uninterrupted, pseudoarticulated and segmented. Our case followed Langlais classification type III (Fig. 4).
Fig. 4.
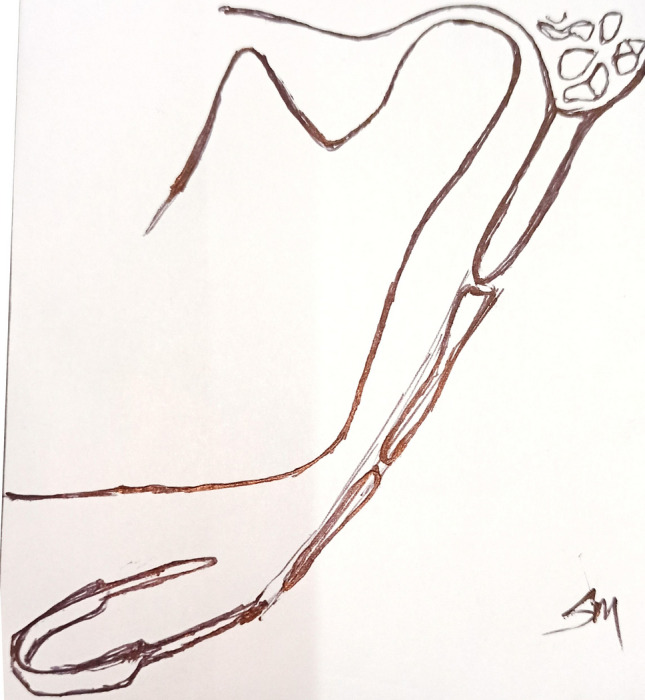
Our case according to Langlais’ classification
Classic Eagle’s syndrome is elongation of styloid process causing stylalgia, a pain of unexplained etiology in oropharynx localized to the tonsillar fossa, and unexplained otalgia. It often begins as vague complaint of a discomfort mimicking of a foreign body being lodged in the throat [1, 3, 9]. It is also associated with dysphagia, dysphonia, transient hoarseness of voice and hypersalivation.
The entire stylohyoid apparatus comprises the styloid process—the long osseous extension of the temporal bone and the lesser cornu of hyoid bone are both derived from the second pharyngeal arch or the Reichert’s cartilage during embryogenesis. The stylohyoid ligament is considered to be the remnant of the Reichert’s cartilage by some researchers. This entire apparatus lies medially, anteriorly and caudally toward the maxilla-vertebro-pharyngeal recess. This has in its medial relation the carotid sheath with its components of carotid arteries, the internal jugular vein and the vagus nerve. The stylohyoid apparatus also runs in close proximity to the hypoglossal nerve [13, 15].
The condition of styloid compressing the carotid arteries and sympathetic fibers is termed as styloid–carotid syndrome [3] consisting of peri-orbital pain, symptoms of transient ischemic attack as dizziness, syncope, headache or stroke [1].
The elongated styloid process causes compression of the carotid arteries as well as the sympathetic fibers. This is termed as styloid–carotid syndrome [9, 16]. It is carotid-type Eagle’s syndrome and may comprise of extensive clinical symptoms of peri-orbital pain or produce symptoms of transient ischemic attack as dizziness, syncope, headache or stroke [7]. Sun et al. [17] reported a case where turning of head caused syncope.
The multiple differential diagnoses to Eagle’s are cranial nerve neuralgias as glossopharyngeal, superior laryngeal, sphenopalatine, impacted molar tooth, temporomandibular joint diseases, faulty dental prostheses, chronic pharyngotonsillitis and pharyngeal or tongue base tumors [18].
Conservative and invasive management of Eagle’s syndrome has been both reported. Medical or conservative management of Eagle’s syndrome is mostly advised that mostly comprises of gabapentin 75 mg, alone or in combination with antidepressants such as amitriptyline or with anticonvulsants as valproic acid [9]. They are majorly handled with medications in pain clinics as many such patients go undiagnosed because the diagnosis of Eagle’s syndrome in itself is a diagnostic challenge.
Uses of hydrocorticoids in combination with long acting local anesthetics in clinically symptomatic areas have been documented. Glucocorticoids are majorly used for the reduction of the pharyngeal swelling thereby reducing the pain of discomfort thus produced [19–21].
Han et al. recommended use of 25 mg of hydrocortisone with 1 ml 25% lignocaine injected around the styloid process or clinically most tender area. This is combined with 400 mg carbamazepine for 2–3 weeks. Gabapentin 300 mg per day has also been used in combination with amitriptyline 1.5 mg per day along with tramadol 37.5 mg per day or with acetaminophen [22]. He also further recommended that next step of medical management would be performing a less invasive procedure—blocking the stellate ganglion once per week for 1 month.
Surgical management of Eagle’s syndrome is either by transoral or transcervical approach [1]. Upon review for surgical management of Eagle’s syndrome from 2001 to 2014, about 92 patients were operated of which 50 were performed transorally and 42 performed transcervically [7, 8, 23–26].
Transoral approach can be performed under local anesthesia, does not produce any scar and requires less operating time. The access and direct visualization to the entire length of the process are not possible. For this procedure, a sagittal split osteotomy incision is generally preferred and placed followed by subperiosteal dissection performed to reach the medial pterygoid muscle to obtain an avascular plane. The muscle is either retracted or divided to get access to the styloid process. The part of the process is removed with rongeur, though the access to the entire length of the process is not possible, but the amount causing the problem can be removed. Then, closure performed with resorbable sutures.
It is a skill-dependent surgery [18]. The risk of bacterial contamination is high in the intraoral approach. With the pharyngeal mucosa very thin and a restricted operating field, it becomes a skill-dependent surgery [18]. However, the operating field thus created was very restricted and the pharyngeal mucosa being thin closure was a technical difficulty. The potential disadvantage is that in case of an event of iatrogenic injury to the carotid system it is difficult to obtain carotid control and then the option would be the transcervical approach to obtain carotid control. The surgery would also cause oropharyngeal edema leading to respiratory embarrassment. Postoperative trismus is very common. Lastly, complete direct visualization of the entire length of the elongated styloid process is also not possible in this approach.
The transcervical method produces an extraoral scar and requires general anesthesia, but the access obtained and direct visualization are better [18].
The control over asepsis and sterilization is also possible as compared to the intraoral approach [18]. Even though greater vessels of the neck are in the field as well as nerves, access is adequate to also obtain optimum control of any iatrogenically created vascular insults.
Marginal mandibular nerve paresthesia has been reported with this approach. Only T J Martin in his article has reported occurrence of transient marginal mandibular nerve paresthesia in two of the five patients he operated [19]. Stenmann had reported of tendinosis at junction of stylohyoid ligament and lesser cornu of hyoid bone [27]. In such cases, it results in abnormal calcified elongation of lesser cornu of hyoid bone. Thus, not only resection of the styloid process but also amputation of lesser cornu of hyoid could be treatment option [28].
Cernea et al. reported a case of first bite syndrome as complication of transcervical approach of surgical management of Eagle’s syndrome which was managed with carbamazepine 400 mg [29]. This is the first and only reported case of first bite syndrome being a potential complication [29].
Conclusion
The diagnosis of Eagle’s syndrome is a challenge! Any case of unexplained and persistent pain in the neck should be delved rather seriously than as a case of unexplained lymphadenopathy which would repeatedly be either challenged with antibiotics unnecessarily or as any neuralgias which would eventually end up in the pain clinic for medical management. The 3D CT scan is the gold standard to radiographically diagnose the Eagle’s syndrome. Mostly, individuals affected show the classic form of Eagle’s, but carotid variety is not unheard of.
A surgical intervention is more dependable and single-step answer to the management of Eagle’s syndrome. Both transcervical and transoral management of the styloid process could be performed, and it is decided by the length of the styloid process and the skill of the operating surgeon.
Authors’ Contribution
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. AD and Dr. SM: The first draft of the manuscript was written by Dr. AD, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of Data and Materials
All authors confirm that all data and materials as well as software application support their published claims and comply with field standards.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Approval was obtained from the ethics committee of Calcutta Institute of Maxillofacial Surgery and Research. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate
The patient has consented to the submission of the case report for submission to the journal.
Consent to Publish
The participant has consented to the submission of the case report to the journal.
Footnotes
The article Eagle’s Syndrome: A Diagnostic Challenge and Surgical Dilemma, written by Annuradha Dey, Srijon Mukherji was originally published electronically on the publisher’s internet portal 10.1007/s12663-020-01396-x on 26 June 2020 with open access. With the author(s)’ decision to step back from Open Choice, the copyright of the article changed on 7 August 2020 to ©The Association of Oral and Maxillofacial Surgeons of India 2020 and the article is forthwith distributed under the terms of copyright.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
8/20/2020
A Correction to this paper has been published: 10.1007/s12663-020-01433-9
References
- 1.Saccomanno S, Greco F, De Corso E, Lucidi D, Deli R, D’addona A, Paludetti G (2018) Case series and reports Eagle’s syndrome, from clinical presentation to diagnosis and surgical treatment: a case report Sindrome di Eagle: aspetti clinici, diagnostici e trattamento chirurgico. Acta Otorhinolaryngol Ital 38:166–169 [DOI] [PMC free article] [PubMed]
- 2.Baddour HM, Mc Anear J, Tilson AB. Eagles syndrome report of case. J Oral Surg. 1978;36:486. doi: 10.1016/0030-4220(78)90378-X. [DOI] [PubMed] [Google Scholar]
- 3.Blatchford SJ, Coulthard SW. Eagle’s syndrome: an atypical cause of dysphonia. Ear Nose Throat J. 1989;68(1):48–51. [PubMed] [Google Scholar]
- 4.Sokler K, Sandev S. New classification of styloid process length–clinical application on the biological base. Coll Antropol. 2001;25(2):627–632. [PubMed] [Google Scholar]
- 5.Radak D, Tanaskovic S, Kecmanovic V, et al. Bilateral Eagle syndrome with associated internal carotid artery kinking and significant stenosis. Ann Vasc Surg. 2016;34:15–18. doi: 10.1016/j.avsg.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 6.Rodríguez-Vázquez JF, Mérida-Velasco JR, Verdugo-López S, Sánchez-Montesinos I, Mérida-Velasco JA. Anatomical Society of Great Britain and Ireland; morphogenesis of the second pharyngeal arch cartilage (Reichert’s cartilage) in human embryos. J Anat. 2006;208:179–189. doi: 10.1111/j.1469-7580.2006.00524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al AS, Miloro M. Transoral endoscopic-assisted styloidectomy: How should Eagle syndrome be managed surgically? Int J Oral Maxillofac Surg. 2015 doi: 10.1016/j.ijom.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 8.Kalvin MM. Elongated styloid processes, their formation and clinical significance. Laryngoscope. 1930;40:907. doi: 10.1288/00005537-193012000-00008. [DOI] [Google Scholar]
- 9.Taheri Arman, Firouzi-Marani Shahram, Khoshbin Masoud. Nonsurgical treatment of stylohyoid (Eagle) syndrome: a case report. J Korean Assoc Oral Maxillofac Surg. 2014;40:246–249. doi: 10.5125/jkaoms.2014.40.5.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagga MB, Kumar CA, Yeluri G. Clinicoradiologic evaluation of styloid process calcification. Imaging Sci Dent. 2012;42:155–161. doi: 10.5624/isd.2012.42.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phulambrikar T, Rajeshwari A, Rao BB, Warhekar A, Reddy P. Incidence of elongated styloid process: a radiographic study. J Indian Acad Oral Med Radiol. 2011;23:S344–S346. doi: 10.5005/jp-journals-10011-1165. [DOI] [Google Scholar]
- 12.Ilgüy M, Ilgüy D, Güler N, Bayirli G. Incidence of the type and calcification patterns in patients with elongated styloid process. J Int Med Res. 2005;33:96–102. doi: 10.1177/147323000503300110. [DOI] [PubMed] [Google Scholar]
- 13.Savranlar A, Uzun L, Uğur MB, Özer T. Three-dimensional CT of Eagle’s syndrome. Diagn Interv Radiol. 2005;11:206–209. [PubMed] [Google Scholar]
- 14.Langlais RP, Miles DA, Van Dis ML. Elongated and mineralized stylohyoid ligament complex: a proposed classification and report of a case of Eagle’s Syndrome. Oral Surg Oral Med Oral Pathol. 1986;61:527–532. doi: 10.1016/0030-4220(86)90400-7. [DOI] [PubMed] [Google Scholar]
- 15.Fini G, Gasparini G, Filippini F, Becelli R, Marcotullio D. The long styloid process syndrome or Eagle’s syndrome. J Craniomaxillofac Surg. 2000;28:123–127. doi: 10.1054/jcms.2000.0128. [DOI] [PubMed] [Google Scholar]
- 16.Soldati AB, Miguelote C, Quero C, Pereira R, Santos R, Soares C. Eagle’s syndrome. Arq Neuropsiquiatr. 2013;71:265–266. doi: 10.1590/0004-282X20130015. [DOI] [PubMed] [Google Scholar]
- 17.Sun CK. Eagle syndrome: an unusual cause of head and neck pain. Arch Neurol. 2006;63:294. doi: 10.1001/archneur.63.2.294. [DOI] [PubMed] [Google Scholar]
- 18.Straus M, Zohar Y, Laurian N. Elongated styloid process syndrome: intraoral versus external approach for styloid surgery. Laryngoscope. 1985;95:976–979. [PubMed] [Google Scholar]
- 19.Martin TJ, Friedland DR, Merati AL. Transcervical resection of the styloid process in Eagle syndrome. Ear Nose Throat J. 2008;87:399–401. doi: 10.1177/014556130808700714. [DOI] [PubMed] [Google Scholar]
- 20.Gervickas A, Kubilius R, Sabalys G. Clinic, diagnostics, and treatment peculiarities of Eagle’s syndrome. Stomatol Balt Dent Maxillofac J. 2004;6:11. [Google Scholar]
- 21.Glogoff MR, Baum SM, Cheifetz I. Diagnosis and treatment of Eagle’s syndrome. J Oral Surg. 1981;39:941–944. [PubMed] [Google Scholar]
- 22.Han M, Kim D, Yang J. Nonsurgical treatment of Eagle’s syndrome: a case report. Korean J Pain. 2013;26:169–172. doi: 10.3344/kjp.2013.26.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fusco D, Asteraki S, Spetzler R. Eagle’s syndrome: embryology, anatomy, and clinical management. Acta Neurochir. 2012;154:1119–1126. doi: 10.1007/s00701-012-1385-2. [DOI] [PubMed] [Google Scholar]
- 24.Torres AC, Guerrero JS, Silva HC. A modified transoral approach for carotid artery type Eagle syndrome: technique and outcomes. Ann Otol Rhinol Laryngol. 2014;18:6–11. doi: 10.1177/0003489414538770. [DOI] [PubMed] [Google Scholar]
- 25.Bertossi D, Albanese M, Chiarini L, Corega C, Mortellaro C, Nocini P. Eagle syndrome surgical treatment with piezosurgery. J Craniofac Surg. 2014;25:811–813. doi: 10.1097/SCS.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 26.Dong Z, Bao H, Zhang L, Hua Z. Eagle’s syndrome associated with lingual nerve paresthesia: a case report. J Oral Maxillofac Surg. 2014;72:e1–e4. doi: 10.1016/j.joms.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 27.Steinmann EP. Styloid syndrome in absence of an elongated process. Acta Otolaryngol. 1968;66:347–356. doi: 10.3109/00016486809126301. [DOI] [PubMed] [Google Scholar]
- 28.van der Westhuijzen AJ, van der Merwe J, Grotepass FW. Eagle’s syndrome: lesser cornu amputation: An alternative surgical solution? Int J Oral Maxillofac Surg. 1999;28:335–337. doi: 10.1016/S0901-5027(99)80076-9. [DOI] [PubMed] [Google Scholar]
- 29.Cernea CR, Hojaij FC, De Carlucci D, Plopper C, Vanderley F, Guerreiro CA, et al. First-bite syndrome after resection of the styloid process. Laryngoscope. 2007;117:181–187. doi: 10.1097/01.mlg.0000245059.40028.ed. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All authors confirm that all data and materials as well as software application support their published claims and comply with field standards.


