Abstract
Background
Relapse is a continuing process and should be evaluated on a long rather than short term.
Materials and Methods
Treatment records of 46 patients who underwent mandibular orthognathic surgery were divided into two groups, i.e. Group 1: Mandibular Advancement (MA) surgery (n = 26) and Group 2: Mandibular Setback (MS) surgery (n = 20). Lateral cephalograms were traced at T0 (01 week before surgery), T1 (01 week after surgery), T2 (01 year after surgery) and T3 (minimum 05 years after surgery) to study short- and long-term skeletal and dental relapse in horizontal, vertical and angular parameters selected for the study. Relapse was correlated with gender, age, amount of surgical movement and intra-operative change in mandibular plane angle to study effect of these factors on relapse.
Results
All horizontal, vertical and angular parameters studied showed significant relapse at short term (from T1 to T2) which continued significantly till long-term evaluation (T2 to T3) in both groups (P value < 0.001). Horizontal relapse in all parameters, vertical relapse in all parameters (except Pog and overbite at T1–T2) and angular relapse in all parameters (except Ramus inclination at T1–T2) was significantly higher in Group 2 compared to Group 1 (P value < 0.001 for all). Relapse showed significant and positive correlation with amount of surgical movement and intra-operative change in mandibular plane angle in both groups (P value < 0.05 for all).
Conclusion
Both MA and MS surgeries show significant relapse on both short- and long-term evaluation which it is higher in MS as compared to MA surgeries.
Keywords: Long-term relapse, Mandibular orthognathic surgery, Advancement surgery, Setback surgery
Introduction
Orthognathic surgery is a commonly employed procedure for correction of severe dentofacial deformities which otherwise cannot be managed by orthodontics alone or in combination with growth modulation [1, 2]. Though the efficacy of orthognathic surgery is time tested in terms of improving facial aesthetics and oral functions, the issue of possible post-treatment relapse has always bothered the researchers and clinicians [3, 4].
Mandibular single jaw surgery (advancement or setback) with Bilateral Sagittal Split Ramus Osteotomy (BSSRO) is a relatively common procedure for management of skeletal deformity with mandibular component. The success of these procedures is gauged depending on stability of the treatment results over a long duration. Any loss of intended skeletal or dental corrections after the surgery is termed as ‘relapse’ [4, 5]. Although with the introduction of rigid internal fixation, the relapse with the post-treatment results have reduced; relapse is a continuous process and is resultant of various short- and long-term factors. The short-term relapse is usually attributed to improper positioning of the condyles in the glenoid fossa intra-operatively resulting in displacement/rotation post-surgically, osteotomy slippage due to condylar morphologic changes and muscle tension resulting from excessive surgical movement. The long-term relapse is usually attributed to progressive resorptive and adaptive changes in the condyles and the continuing skeletal growth [5–8].
Mandibular Advancement (MA) surgery to correct mandibular retrognathism/hypoplasia is considered to be a highly stable procedure whereas Mandibular Setback (MS) surgery to correct mandibular prognathism is considered problematic [4]. There is sufficient literature which describes the stability of these procedures on a short-term basis (06 months to 02 year post-surgically) [1, 3, 9–11]. However, there is very limited literature which describes the stability of mandibular orthognathic procedures on a long-term follow-up. Further, very few studies are available which compare the amount of relapse between MA and MS surgeries on a long-term follow-up and correlate with different likely etiological factors. Therefore, this study was undertaken to augment the existing evidence in this regard.
Aim
To study skeletal and dental relapse in patients who underwent mandibular orthognathic surgery (MA/MS) with BSSRO on a short- and long-term follow-up.
Objectives
-
(i)
To quantify relapse in horizontal and vertical directions after MA and MS surgeries on a short- (01 year) and long-term (minimum 05 years) follow-up.
-
(ii)
To compare the amount of relapse between the two mandibular surgeries.
-
(iii)
To correlate the relapse with gender, age, amount of surgical movement and change in mandibular plane (MP) angle.
Materials and Methods
This cross-sectional study was undertaken at a tertiary care institute imparting post-graduate training. The records of patients who were operated at the institute from 01 January 2010 to 31 December 2014 for mandibular orthognathic surgery were retrieved. The permission of the institutional ethical committee was obtained prior to the start of study. Only those patients who consented to participate in the study with a minimum follow-up of 05 years post-surgery were selected for the study. Other inclusion criteria were: skeletally mature patients with minimum age of 18 years at the time of surgery, minimum advancement/setback ≥ 5 mm with ANB ≥ 4° for Class II and ≤ − 2° for Class III patients, patients who underwent single jaw surgery of mandible with BSSRO and cases treated with conventional ortho-surgical protocol, i.e. pre-surgical orthodontic treatment followed by orthognathic surgery and post-surgical orthodontics. The cases excluded were: patients treated with Surgery First Orthognathic After (SFOA) approach, patients who underwent bijaw surgery, BSSRO with Intraoral Vertical Ramus Osteotomy (IVRO) procedure, cases which underwent asymmetric advancement or setback, cases treated with Distraction Osteogenesis (DO), syndromic cases including patients with Cleft Lip and/or Palate, patients with history of trauma to jaws or jaw surgery, and patients with any systemic disease/condition affecting bone metabolism. Intra-operatively, the osteotomized segments for all cases were stabilized with 4 hole titanium mini bone plate with or without gap depending on the requirement (2 mm system) and 7 mm long self tapping screws (Stryker Leibinger, USA). A standard post-operative protocol was followed for all cases. The splint was fabricated as per standard procedure with tripod contacts, i.e. 2 posterior and 1 anterior contact for all cases which maintained the vertical height. The splint was luted at second day post-operatively and neuromuscular training was done for 06 weeks with guiding elastics in Class II or III pattern depending on the case. The splint was progressively trimmed and the posterior open bite (if present) between the tripod contacts was closed with settling elastics. After removal of splint, post-surgical orthodontics of average 10-month duration was carried out for all cases.
Forty six cases matching the inclusion criteria could be recalled for follow-up records (photographs, study models and lateral cephalogram). The cases included 26 females and 20 males. The mean duration of follow-up was 7.2 years (range = 05–09 years). The cases were divided into two groups:
Group 1 Cases who underwent MA surgery (14 females and 12 males, aged 18–26 years at the time of surgery, mean age 22.6 years).
Group 2 Cases who underwent MS surgery (12 females and 08 males, aged 20–29 years at the time of surgery, mean age 24 years).
The lateral cephalogram for all patients selected for the study was taken on the same machine (Model: ADVAPX cephalostat machine, Company: Panorraitic System, Printer: Fujifilms DRY PIX 7000) with a standardized technique with the patient in natural head position (NHP). The lateral cephalogram of all patients were traced at T0 (01 week before surgery), T1 (01 week after surgery), T2 (01 year after surgery) and T3 (at follow-up, minimum 05 years after surgery) (Fig. 1). A surrogate horizontal plane (XN) was constructed 7° above the SN plane. A perpendicular (X′Y) was drawn from XN at Sella (S) point. The rectilinear distances were measured from XN and X′Y planes to study vertical and horizontal relapse at Menton (Me), Pogonion (Pog), Point B and Gonion (Go) at above time frames as per methodology of Eggensperger [5] suitably modified as per our study requirements. The angular parameters studied were: SNB angle (for change in mandibular sagittal position); Mandibular plane angle [for change in mandibular plane (ML) in relation to Frankfort Horizontal (FH) plane]; changes in gonial angle and ramus inclination. The changes in overjet and overbite were noted. The change in incisor inclination was ascertained by UI to NA (Upper incisor to Nasion-Point A line), LI to NB (Lower incisor to Nasion-Point B line) and interincisor angles. The magnitude and percentage of relapse between the two study group were compared at T2 (short term) and T3 (long term). The relapse at T2 and T3 was also correlated with gender, age, amount of surgical movement and intra-operative change in mandibular plane angle to study the effect of these factors on relapse. Cephalometric tracings were done by a single operator (SSA). To ascertain intra and inter-operator bias, randomly selected twenty five cephalogram were retraced by the same operator and also a senior orthodontist (SD) after a period of 01 week. The kappa score was 0.9, which indicated excellent intra and inter-operator agreement. The data was compiled in MS-excel sheets and subjected to statistical analysis.
Fig. 1.
Landmarks measured on lateral cephalogram
Statistical Analysis
The entire data was statistically analysed using Statistical Package for Social Sciences (SPSS version 22.0, IBM Corporation, USA) for MS Windows. The inter-group statistical comparison of distribution of categorical variables was tested using Chi Square test and Fisher’s exact probability test for 2 × 2 contingency table. The inter-group statistical comparison of means of continuous variables was done using independent sample t test. The intra-group statistical comparison of means of continuous variables was done using repeated measures analysis of variance (RMANOVA). The underlying normality assumption was tested before subjecting the study variables to t test and RMANOVA. Correlation analysis was done using Spearman’s method. The P values less than 0.05 were considered to be statistically significant.
Results
Gender and Age Distribution
The distribution of gender and mean age of cases studied did not differ significantly between the two study groups (P value > 0.05) (Table 1).
Table 1.
Gender and age distribution
| Gender | Sample size (n) | Age (years) | ||||||
|---|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | P value | ||||||
| Group 1 | Group 2 | P value | Mean | SD | Mean | SD | ||
| Male | 12 | 08 | 0.676NS | 22.4 | 3.6 | 24.2 | 4.2 | 0.869NS |
| Female | 14 | 12 | 22.8 | 3.2 | 23.8 | 3.6 | ||
| Total | 26 | 20 | 22.6 | 3.4 | 24.0 | 3.8 | ||
P value < 0.05 was considered to be statistically significant. *P value < 0.05, **P value < 0.01, ***P value < 0.001, NS statistically significant
Short- and Long-Term Relapse in Horizontal, Vertical and Angular Parameters Studied in Group 1
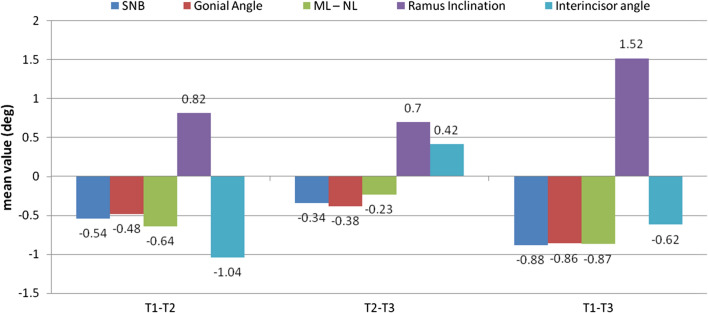
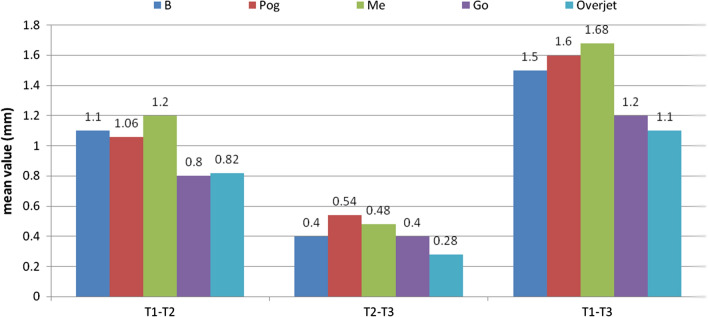
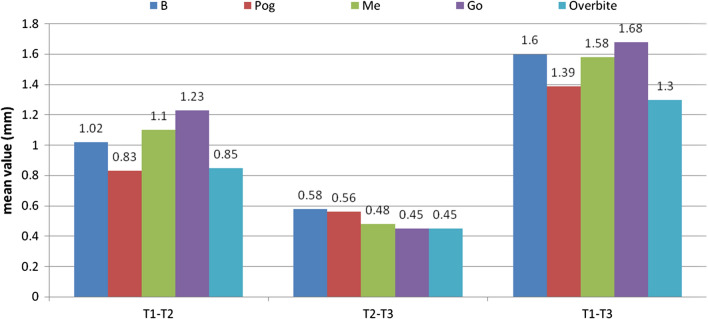
All linear horizontal parameters (Table 2, Fig. 2), linear vertical parameters (Table 2, Fig. 3) and angular parameters (Table 2, Fig. 4) studied showed significant relapse at short term (from T1 to T2) which continued significantly till long-term evaluation (T2 to T3) (P value < 0.001).
Table 2.
Short- and long-term relapse in horizontal, vertical and angular parameters studied in Group 1
| Surgical movement (T0–T1) (a) | SD | P value | Short-term relapse at 01 year (T1–T2) (b) | SD | P value | % of relapse (c) = b/a × 100 | Long-term relapse from 01 to ≥ 05 years (T2–T3) (d) | SD | P value | % of relapse (e) = d/a × 100 | Total relapse (T1–T3) (f) = b + d | % of relapse (g) = f/a × 100 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Horizontal change (mm) | |||||||||||||
| B | 5.30 | 2.20 | 0.001*** | − 0.65 | 1.12 | 0.001*** | − 12.68% | − 0.35 | 0.47 | 0.001*** | − 6.78% | − 1.00 | − 19.12% |
| Pog | 5.61 | 2.52 | 0.001*** | − 0.61 | 0.92 | 0.001*** | − 11.21% | − 0.34 | 0.82 | 0.001*** | − 6.23% | − 0.95 | − 17.19% |
| Me | 5.22 | 2.53 | 0.001*** | − 0.66 | 1.01 | 0.001*** | − 12.75% | − 0.37 | 0.79 | 0.001*** | − 7.13% | − 1.03 | − 20.14% |
| Go | 4.63 | 2.73 | 0.001*** | − 0.42 | 0.88 | 0.001*** | − 9.56% | − 0.29 | 0.21 | 0.001*** | − 6.13% | − 0.71 | − 15.23% |
| Overjet | 5.14 | 3.23 | 0.001*** | − 0.62 | 1.14 | 0.001*** | − 12.19% | − 0.33 | 1.01 | 0.001*** | − 6.53% | − 0.95 | − 18.92% |
| Vertical change (mm) | |||||||||||||
| B | 2.92 | 3.60 | 0.001*** | 1.10 | 1.08 | 0.001*** | 95.62% | 0.28 | 0.76 | 0.001*** | 25.96% | 1.38 | 47.26% |
| Pog | 2.86 | 3.99 | 0.001*** | 0.84 | 1.14 | 0.001*** | 78.22% | 0.20 | 0.80 | 0.001*** | 19.23% | 1.04 | 36.36% |
| Me | 3.08 | 2.70 | 0.001*** | 0.74 | 0.88 | 0.001*** | 62.67% | 0.32 | 0.67 | 0.001*** | 26.43% | 1.06 | 34.41% |
| Go | 2.78 | 2.49 | 0.001*** | 0.62 | 1.02 | 0.001*** | 35.21% | 0.18 | 0.69 | 0.001*** | 10.13% | 0.80 | 28.78% |
| Overbite | 2.90 | 3.58 | 0.001*** | 0.88 | 0.44 | 0.001*** | 77.63% | 0.12 | 0.58 | 0.001*** | 10.95% | 1.00 | 34.48% |
| Angular change (degree) | |||||||||||||
| SNB | 4.00 | 2.40 | 0.001*** | − 0.54 | 1.48 | 0.001*** | − 13.69% | − 0.34 | 2.10 | 0.001*** | − 8.92% | − 0.88 | − 22.43% |
| Gonial Angle | 2.42 | 4.60 | 0.001*** | − 0.48 | 1.70 | 0.001*** | − 20.21% | − 0.38 | 1.20 | 0.001*** | − 16.21% | − 0.86 | − 35.49% |
| MP Angle | 2.78 | 3.38 | 0.001*** | − 0.64 | 2.10 | 0.001*** | − 36.39% | − 0.23 | 1.45 | 0.001*** | − 13.15% | − 0.87 | − 31.29% |
| Ramus Inclination | − 2.80 | 4.70 | 0.001*** | 0.82 | 1.04 | 0.001*** | − 46.53% | 0.70 | 1.84 | 0.001*** | − 39.13% | 1.52 | − 54.28% |
| Interincisor angle | 4.10 | 4.30 | 0.001*** | − 1.04 | 2.90 | 0.001*** | − 26.46% | 0.42 | 1.36 | 0.001*** | 10.29% | − 0.62 | − 16.18% |
Fig. 2.
Short- and long-term relapse in horizontal parameters studied in Group 1
Fig. 3.
Short- and long-term relapse in vertical parameters studied in Group 1
Fig. 4.
Short- and long-term relapse in angular parameters studied in Group 1
Short- and Long-Term Relapse in Horizontal, Vertical and Angular Parameters Studied in Group 2
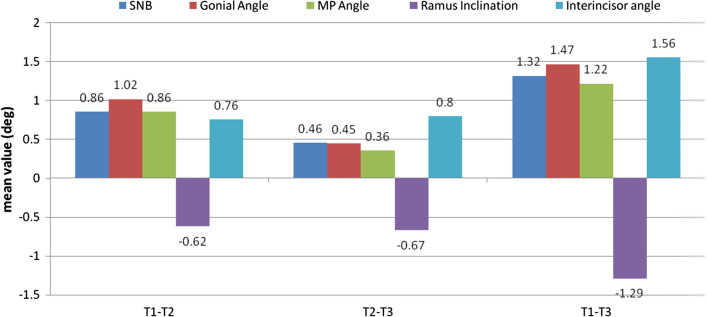
All linear horizontal parameters (Table 3, Fig. 5), linear vertical parameters (Table 3, Fig. 6) and angular parameters (Table 3, Fig. 7) studied showed significant relapse at short term (from T1 to T2) which continued significantly till long-term evaluation (T2 to T3) (P value < 0.001).
Table 3.
Short- and long-term relapse in horizontal, vertical and angular parameters studied in Group 2
| Surgical movement (T0–T1) (a) | SD | P value | Short-term relapse at 01 year (T1–T2) (b) | SD | P value | % of relapse (c) = b/a × 100 | Long-term relapse from 01 to ≥ 05 years (T2–T3) (d) | SD | P value | % of relapse (e) = d/a × 100 | Total relapse (T1–T3) (f) = b + d | % of relapse (g) = f/a × 100 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Horizontal change (mm) | |||||||||||||
| B | − 6.10 | 3.94 | 0.001*** | 1.10 | 1.84 | 0.001*** | − 18.03% | 0.40 | 0.68 | 0.001*** | − 6.56% | 1.5 | − 24.59% |
| Pog | − 6.96 | 5.59 | 0.001*** | 1.06 | 0.96 | 0.001*** | − 15.23% | 0.54 | 1.87 | 0.001*** | − 7.76% | 1.6 | − 22.99% |
| Me | − 6.18 | 4.80 | 0.001*** | 1.20 | 1.20 | 0.001*** | − 19.42% | 0.48 | 0.98 | 0.001*** | − 7.77% | 1.68 | − 27.18% |
| Go | − 5.42 | 3.79 | 0.001*** | 0.80 | 0.90 | 0.001*** | − 14.76% | 0.40 | 0.28 | 0.001*** | − 7.38% | 1.2 | − 22.14% |
| Overjet | − 5.70 | 4.26 | 0.001*** | 0.82 | 0.98 | 0.001*** | − 14.39% | 0.28 | 1.10 | 0.001*** | − 4.91% | 1.1 | − 19.30% |
| Vertical change (mm) | |||||||||||||
| B | − 4.38 | 3.62 | 0.001*** | 1.02 | 2.42 | 0.001*** | − 30.18% | 0.58 | 0.68 | 0.001*** | − 17.16% | 1.6 | − 36.53% |
| Pog | − 4.12 | 4.26 | 0.001*** | 0.83 | 4.13 | 0.001*** | − 26.60% | 0.56 | 0.56 | 0.001*** | − 17.95% | 1.39 | − 33.74% |
| Me | − 4.74 | 3.74 | 0.001*** | 1.10 | 3.45 | 0.001*** | − 40.15% | 0.48 | 1.34 | 0.001*** | − 17.52% | 1.58 | − 33.33% |
| Go | − 4.05 | 2.45 | 0.001*** | 1.23 | 2.84 | 0.001*** | − 60.00% | 0.45 | 0.45 | 0.001*** | − 21.95% | 1.68 | − 41.48% |
| Overbite | − 3.88 | 3.55 | 0.001*** | 0.85 | 3.44 | 0.001*** | − 53.80% | 0.45 | 1.33 | 0.001*** | − 28.48% | 1.3 | − 33.51% |
| Angular change (degrees) | |||||||||||||
| SNB | − 5.10 | 3.20 | 0.001*** | 0.86 | 1.68 | 0.001*** | − 16.86% | 0.46 | 2.24 | 0.001*** | − 9.02% | 1.32 | − 25.88% |
| Gonial Angle | − 3.83 | 2.64 | 0.001*** | 1.02 | 1.67 | 0.001*** | − 26.63% | 0.45 | 1.88 | 0.001*** | − 11.75% | 1.47 | − 38.38% |
| MP Angle | − 3.94 | 3.04 | 0.001*** | 0.86 | 2.88 | 0.001*** | − 21.83% | 0.36 | 1.89 | 0.001*** | − 9.14% | 1.22 | − 30.96% |
| Ramus Inclination | 3.12 | 4.25 | 0.001*** | − 0.62 | 1.46 | 0.001*** | − 29.25% | − 0.67 | 1.46 | 0.001*** | − 31.60% | − 1.29 | − 41.35% |
| Interincisor angle | − 4.22 | 2.96 | 0.001*** | 0.76 | 1.92 | 0.001*** | − 34.23% | 0.80 | 1.46 | 0.001*** | − 36.04% | 1.56 | − 36.97% |
Fig. 5.
Short- and long-term relapse in horizontal parameters studied in Group 2
Fig. 6.
Short- and long-term relapse in vertical parameters studied in Group 2
Fig. 7.
Short- and long-term relapse in angular parameters studied in Group 2
Inter-group Comparison of Short- and Long-Term Relapse in Horizontal, Vertical and Angular Parameters Studied
The mean linear horizontal relapse (T1–T2 and T1–T3) in all parameters was significantly higher in Group 2 compared to Group 1 (P value < 0.001 for all) (Table 4).
Table 4.
Inter-group comparison of short- and long-term relapse in horizontal, vertical and angular parameters studied
| Group 1 | Group 2 | P value | Group 1 | Group 2 | P value | Group 1 | Group 2 | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0–T1 | SD | T0–T1 | SD | T1–T2 | SD | T1–T2 | SD | T1–T3 | SD | T1–T3 | SD | ||||
| 5.30 | 2.20 | 6.10 | 3.94 | 0.001*** | 0.65 | 1.12 | 1.10 | 1.84 | 0.001*** | 1.00 | 0.37 | 1.50 | 0.38 | 0.001*** | |
| 5.61 | 2.52 | 6.96 | 5.59 | 0.001*** | 0.61 | 0.92 | 1.06 | 0.96 | 0.001*** | 0.95 | 0.42 | 1.60 | 0.41 | 0.001*** | |
| 5.22 | 2.53 | 6.18 | 4.80 | 0.001*** | 0.66 | 1.01 | 1.20 | 1.20 | 0.001*** | 1.03 | 0.29 | 1.68 | 0.28 | 0.001*** | |
| 4.63 | 2.73 | 5.42 | 3.79 | 0.001*** | 0.42 | 0.88 | 0.80 | 0.90 | 0.001*** | 0.71 | 0.21 | 1.20 | 0.24 | 0.001*** | |
| 5.14 | 3.23 | 5.70 | 4.26 | 0.001*** | 0.62 | 1.14 | 0.82 | 0.98 | 0.001*** | 0.95 | 0.24 | 1.10 | 0.20 | 0.001*** | |
| 2.92 | 3.60 | 4.38 | 3.62 | 0.001*** | 1.10 | 1.08 | 1.02 | 2.42 | 0.001*** | 1.38 | 0.36 | 1.60 | 0.38 | 0.001*** | |
| 2.86 | 3.99 | 4.12 | 4.26 | 0.001*** | 0.84 | 1.14 | 0.83 | 4.13 | 0.209NS | 1.04 | 0.50 | 1.39 | 0.46 | 0.001*** | |
| 3.08 | 2.70 | 4.74 | 3.74 | 0.001*** | 0.74 | 0.88 | 1.10 | 3.45 | 0.001*** | 1.06 | 0.51 | 1.58 | 0.34 | 0.001*** | |
| 2.78 | 2.49 | 4.05 | 2.45 | 0.001*** | 0.62 | 1.02 | 1.23 | 2.84 | 0.001*** | 0.80 | 0.39 | 1.68 | 0.41 | 0.001*** | |
| 2.90 | 3.58 | 3.88 | 3.55 | 0.001*** | 0.88 | 0.44 | 0.85 | 3.44 | 0.441NS | 1.00 | 0.38 | 1.30 | 0.33 | 0.001*** | |
| 4.00 | 2.40 | 5.10 | 3.20 | 0.001*** | 0.54 | 1.48 | 0.86 | 1.68 | 0.027* | 0.88 | 0.21 | 1.32 | 0.24 | 0.001*** | |
| 2.42 | 4.60 | 3.83 | 2.64 | 0.001*** | 0.48 | 1.70 | 1.02 | 1.67 | 0.001*** | 0.86 | 0.20 | 1.47 | 0.27 | 0.001*** | |
| 2.78 | 3.38 | 3.94 | 3.04 | 0.001*** | 0.64 | 2.10 | 0.86 | 2.88 | 0.033* | 0.87 | 0.18 | 1.22 | 0.19 | 0.001*** | |
| 2.80 | 4.70 | 3.12 | 4.25 | 0.001*** | 0.82 | 1.04 | 0.62 | 1.46 | 0.104NS | 1.52 | 0.18 | 1.29 | 0.17 | 0.001*** | |
| 4.10 | 4.30 | 4.22 | 2.96 | 0.001*** | 1.04 | 2.90 | 0.76 | 1.92 | 0.001*** | 0.62 | 0.21 | 1.56 | 0.24 | 0.001*** | |
P value < 0.05 was considered to be statistically significant. *P value < 0.05, **P value < 0.01, ***P value < 0.001, NS statistically significant
The mean linear vertical relapse (T1–T2 and T1–T3) in all parameters (except for Pog and overbite at T1–T2) was significantly higher in Group 2 compared to Group 1 (P value < 0.05 for all) (Table 4).
The mean angular relapse (T1–T2 and T1–T3) in all parameters (except for Ramus inclination at T1–T2) was significantly higher in Group 2 compared to Group 1 (P value < 0.05 for all) (Table 4).
Correlation of Relapse with Age, Gender, Amount of Surgical Movement and Change in MP Angle
The relapse T1–T2 and T1–T3 showed statistically significant and positive correlation with amount of surgical movement and intra-operative change in mandibular plane angle in both groups (P value < 0.05 for all). However, the relapse T1–T2 and T1–T3 did not show statistically significant positive correlation with gender and age in both groups (P value > 0.05 for all) (Table 5).
Table 5.
Correlation of total relapse with age, gender, amount of surgical movement (T0–T1) and change in Mandibular Plane (MP) angle
| Surgical Procedure | Correlation with | R value | P value | R value | P value |
|---|---|---|---|---|---|
| T1–T2 | T1–T3 | ||||
| Mandibular advancement | Gender (coded 1: male, 2: female) | 0.087 | 0.784NS | 0.093 | 0.688NS |
| Age | 0.181 | 0.356NS | 0.109 | 0.469NS | |
| Amount of surgical movement | 0.312 | 0.001*** | 0.317 | 0.001*** | |
| Change in MP angle | 0.318 | 0.001*** | 0.338 | 0.001*** | |
| Mandibular setback | Gender (coded 1: male, 2: female) | 0.189 | 0.455NS | 0.102 | 0.405NS |
| Age | 0.241 | 0.122NS | 0.203 | 0.243NS | |
| Amount of surgical movement | 0.413 | 0.001*** | 0.407 | 0.001*** | |
| Change in MP angle | 0.341 | 0.001*** | 0.351 | 0.001*** | |
P value < 0.05 was considered to be statistically significant. *P value < 0.05, **P value < 0.01, ***P value < 0.001, NS statistically significant
Discussion
The management of severe malocclusion and dentofacial deformities in adults often necessitate a combined ortho-surgical approach. BSSRO along with rigid fixation, the most commonly used method for mandibular orthognathic surgery [12] is often followed by post-operative complications, the magnitude of which differs from case to case. The most frequently encountered complications are nerve injury, infections, haemorrhage and relapse [13]. Prediction of relapse has always been an enigma to the ortho-surgical team. Relapse encountered is of multifactorial aetiology which depends upon various factors such as expertise of the ortho-surgical team, seating of condyles in glenoid fossa, amount of surgical movement, muscle tension, condylar resorption, preoperative mandibular plane angle etc. [14]. Though there are several studies predicting relapse after mandibular orthognathic surgery [1, 3, 9–11], most of them are short-term studies assessing relapse after 06 months to 02 year post-surgically and only very few have assessed relapse on a long term (greater than 05 years). Since, relapse is a continuing process; it is prudent to study it on a long term. Therefore, the present study was undertaken with a minimum follow-up of 05 years (range = 05–09 years) to augment the existing evidence in this regard.
Most of the available literature has focussed on study of relapse in a sagittal plane. But studies have shown that relapse occurs in all planes, i.e. even in vertical and transverse planes [11, 15]. Therefore, the present study assessed relapse in both sagittal and vertical planes along with relapse in various angular parameters at short- and long-term follow-up.
Relapse After MA Surgery (Group 1)
The results of the present study show a statistically significant relapse in all horizontal parameters studied at short term and this relapse continued till long-term follow-up. The mean relapse at B point was 0.65 mm (12.68%) at T2 and 0.35 mm (6.78%) on long-term follow-up at T3 (overall 01 mm, 19.12%). This relapse at T2 is similar to a study [16] which observed that there is 90% chance of < 2 mm relapse at 01 year after MA surgery irrespective of the type of fixation used. Long-term follow-up > 01 year was not done in the above study. Another study [5] observed a relapse of 1.2 mm at point B at 14 months and 0.8 mm on a long term (total relapse around 2 mm) which is higher to that observed in our study both at short and long terms. This higher relapse can be attributed to a longer follow-up duration up to 14 years in the above study which indicates the need of further follow-up of our study sample. The horizontal relapse observed in the present study is lesser as compared to other studies [17, 18] at both short and long term with similar follow-up duration as our study. There are studies which have observed less than 10% relapse on 01-year follow-up which is lesser compared to the present study [19]. These variations may be attributed to the variation in study design, surgical and fixation techniques among studies.
A significant relapse in all vertical and angular parameters was observed in the present study both at short and long term. These finding contradict an earlier study [19] in which the Lower Anterior Facial Height (LAFH) increased on a short term and remained stable thereafter on a long term. The short term described in the above study is immediate post-surgical and long term was 01 year post-surgical. However, 01 year post-surgical has been described as short-term follow-up period in the present study. Our study findings are in agreement with other studies which reported counter-clockwise rotation of the proximal segment and reduction in vertical dimensions on a long-term follow-up [5, 20].
In the present study, the relapse at short and long term showed statistically significant positive correlation with amount of MA. These findings are similar to earlier studies which concluded that the amount of MA is a major contributing factor in relapse. This has been attributed to excessive stretch of the associated musculature and lesser bony interface at the site of osteotomy subsequent to a larger MA [12, 24]. These findings however contradict other studies [5, 25] which did not find any correlation between the amounts of MA and relapse. Our study also observed a positive correlation between the intra-operative change in mandibular plane angle and post-surgical relapse in mandibular plane. These findings are similar to other studies [5, 25, 26]. There is limited literature on this aspect and prospective studies with a larger sample size are required to validate these findings.
Relapse After MS Surgery (Group 2)
The results of the present study show a statistically significant relapse in all horizontal parameters studied at T2 and this relapse continued till T3. The mean relapse at B point was 1.10 mm (18.03%) at T2 and 0.40 mm (6.56%) at T3 (overall 1.5 mm, 24.59%). These findings are similar to earlier studies which reported significant relapse after setback surgeries [19, 20]. These findings contradict a recent systematic review which observed insignificant amount of horizontal relapse after setback surgeries [21]. However, the follow-up duration in the above study is limited to ≤ 01 year.
A significant relapse in all vertical and angular parameters was observed in the present study both at short and long term. These findings contradict earlier studies [19, 22, 23] in which the LAFH did not vary considerably on a short- and long-term follow-up which indicates pure MS without any post-surgical rotation of the condyles in the glenoid fossa. The authors attributed it to a careful surgical technique and minimal muscle stretch post-operatively which markedly reduced relapse. The findings of the present study concur with an earlier study which observed significant vertical change (1.8 mm at Pogonion) on a short-term follow-up [23]. This study however did not observe a statistically significant vertical change on a long-term follow-up as observed in the present study. The long-term follow-up described in the above study was 01 year against minimum 05 years in the present study.
In the present study, the relapse at short and long term showed statistically significant positive correlation with amount of MS. These findings are similar to earlier studies [27] which observed that the magnitude of MS is a major contributing factor in relapse. The present study also found a positive correlation between the intra-operative change in mandibular plane angle and post-surgical relapse. These findings are similar to other studies which observed that a steep pre-surgical mandibular plane angle is associated with a higher relapse [23, 28]. Since there is limited literature in this regard, further studies are recommended to substantiate these findings.
Comparison of Relapse Between MA and MS Surgeries (Group 1 Versus Group 2)
In the present study, significantly higher relapse was observed in group 2 as compared to group 1 at both T2 and T3. These findings are similar to other studies in literature [4, 15, 16, 19, 20]. Studies have reported that MA is a more stable procedure especially with advancement ≤ 10 mm and patients with normal/short LAFH whereas MS has a higher post-surgical relapse (around 40%–50% chance of 2–4 mm post-surgical relapse) [19, 29]. In contrary to our study results, a study [11] observed higher skeletal relapse in MS surgery (30%) as compared to the MA surgery (12%). The above study also observed that skeletal Class II patients with retrognathic mandible and with hyperdivergent facial pattern had higher chance of relapse whereas hypodivergent facial patterns were associated with lesser relapse in both MA and MS surgeries. The available data is this aspect is mainly short-term and long-term research comparing both groups may add further evidence.
Conclusions
The findings of the present study indicate that relapse is a continuing process and should be evaluated on a long rather than short term. The accurate prediction of anticipated relapse will assist the ortho-surgical team in treatment planning and instituting any changes in the proposed treatment plan to minimize it. Both MA and MS surgeries show significant relapse on both short- and long-term evaluation and it is higher in MS as compared to MA surgeries. The magnitude of relapse is positively correlated with the amount of surgical movement and intra-operative change in mandibular plane angle. Further research based on long-term prospective studies is recommended to validate these findings.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
N. K. Sahoo, Email: colnksahoo@gmail.com
Shiv Shankar Agarwal, Email: docshivagarwal@rediffmail.com.
Sanjeev Datana, Email: drdatana@rediffmail.com.
S. K. Bhandari, Email: kumarsdel@gmail.com
References
- 1.Thiele OC, Kreppel M, Bittermann G, Bonitz L, Desmedt M, Dittes C. Moving the mandible in orthognathic surgery—a multicenter analysis. J Cranio Maxillofac Surg. 2016 doi: 10.1016/j.jcms.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 2.Paunonen J, Helminen M, Peltomaki T. Long-term stability of mandibular advancement with bilateral sagittal split osteotomy. J Cranio Maxillofac Surg. 2018 doi: 10.1016/j.jcms.2018.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Haan IF, Ciesielski R, Nitsche T, Koos B. Evaluation of relapse after orthodontic therapy combined with orthognathic surgery in the treatment of skeletal class III. J Orofac Orthop. 2013;74(5):362–369. doi: 10.1007/s00056-013-0161-0. [DOI] [PubMed] [Google Scholar]
- 4.Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007;3:21. doi: 10.1186/1746-160X-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eggensperger N, Smolka K, Luder J, Iizuka T. Short- and long-term skeletal relapse after mandibular advancement surgery. Int J Oral Maxillofac Surg. 2006;35:36–42. doi: 10.1016/j.ijom.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Hwang SJ, Haers PE, Sailer HF. The role of a posteriorly inclined condylar neck in condylar resorption after orthognathic surgery. J Craniomaxillofac Surg. 2000;28:85–90. doi: 10.1054/jcms.2000.0129. [DOI] [PubMed] [Google Scholar]
- 7.Lee JY, Lee SM, Kim SH, Kim Y. Long-term follow-up of intersegmental displacement after orthognathic surgery using cone-beam computed tomographic superimposition. Angle Orthod. 2020 doi: 10.2319/061119-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Politi M, Costa F, Cian R, Polini F, Robiony M. Stability of skeletal Class III malocclusion after combined maxillary and mandibular procedures: rigid internal fixation versus wire osteosynthesis of the mandible. J Oral Maxillofac Surg. 2004;62:169–181. doi: 10.1016/j.joms.2003.04.010. [DOI] [PubMed] [Google Scholar]
- 9.Gassmann CJ, Van Sickels JE, Thrash WJ. Causes, location, and timing of relapse following rigid fixation after mandibular advancement. J Oral Maxillofac Surg. 1990;48:450–454. doi: 10.1016/0278-2391(90)90229-U. [DOI] [PubMed] [Google Scholar]
- 10.Gomes MA, Wisth PJ, Tornes K, Boe OE. Skeletofacial changes by mandibular advancement using sagittal split osteotomies. Int J Adult Orthodon Orthognath Surg. 1993;8:87–94. [PubMed] [Google Scholar]
- 11.Eggensperger N, Smolka W, Zahal R, Iizuka T. Skeletal relapse after mandibular advancement and setback in single-jaw surgery. J Oral Maxillofac Surg. 2004;62:1486–1496. doi: 10.1016/j.joms.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Tabrizi R, Nili M, Aliabadi E, Pourdanesh F. Skeletal stability following mandibular advancement: is it influenced by the magnitude of advancement or changes of the mandibular plane angle? J Korean Assoc Oral Maxillofac Surg. 2017;43:152–159. doi: 10.5125/jkaoms.2017.43.3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jędrzejewski M, Smektała T, Sporniak-Tutak K, Olszewski R. Preoperative, intraoperative, and postoperative complications in orthognathic surgery: a systematic review. Clin Oral Investig. 2015;19:969–977. doi: 10.1007/s00784-015-1452-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg. 2009;67(2):301–313. doi: 10.1016/j.joms.2008.06.060. [DOI] [PubMed] [Google Scholar]
- 15.Bailey L, Cevidanes LH, Proffit WR. Stability and predictability of orthognathic surgery. Am J Orthod Dentofacial Orthop. 2004;126(3):273–277. doi: 10.1016/j.ajodo.2004.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watzke IM, Turvey TA, Phillips C, Proffit WR. Stability of mandibular advancement after sagittal osteotomy with screw or wire fixation: a comparative study. J Oral Maxillofac Surg. 1990;48(2):108–121. doi: 10.1016/S0278-2391(10)80197-1. [DOI] [PubMed] [Google Scholar]
- 17.Bouwman JP, Tuinzing DB, Kostense PJ, van Teeseling RA, Mokhtari H. The value of long-term follow-up of mandibular advancement surgery in patients with a low to normal mandibular plane angle. Mund Kiefer Gesichtschir. 1997;1:311–315. doi: 10.1007/BF03043574. [DOI] [PubMed] [Google Scholar]
- 18.Simmons KE, Turvey TA, Phillips C, Proffit WR. Surgical-orthodontic correction of mandibular deficiency: five year follow-up. Int J Adult Orthodon Orthognath Surg. 1992;7:67–79. [PubMed] [Google Scholar]
- 19.Darshan SV, Ronad YA, Kishore MS, Shetty KS, Rajesh M, Suman SD. Long term stability and relapse following mandibular advancement and mandibular setback surgeries: a cephalometric study. J Int Oral Health. 2014;6(5):42–46. [PMC free article] [PubMed] [Google Scholar]
- 20.Mobarak KA, Espeland L, Krogstad O, Lyberg T. Mandibular advancement surgery in high-angle and low-angle class II patients: different long-term skeletal responses. Am J Orthod Dentofacial Orthop. 2001;119:368–381. doi: 10.1067/mod.2001.110983. [DOI] [PubMed] [Google Scholar]
- 21.AlZayer MA, Leung YY. Skeletal and airway stability after mandibular setback in patients with mandibular prognathism: a systematic review. Saudi Dent J. 2020 doi: 10.1016/j.sdentj.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson SW, Speidel TM, Isaacson RJ, Worms FW. Soft tissue profile change produced by reduction of mandibular prognathism. Angle Orthod. 1972;42(3):227–235. doi: 10.1043/0003-3219(1972)042<0227:STPCPB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Rao SH, Selvaraj L, Lankupalli AS. Skeletal stability after bilateral sagittal split advancement and setback osteotomy of the mandible with miniplate fixation. Craniomaxillofac Trauma Reconstr. 2014;7(1):9–16. doi: 10.1055/s-0033-1356763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frey DR, Hatch JP, Van Sickels JE, Dolce C, Rugh JD. Alteration of the mandibular plane during sagittal split advancement: short- and long-term stability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:160–169. doi: 10.1016/j.tripleo.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 25.Perrott DH, Lu YF, Pogrel MA, Kaban LB. Stability of sagittal split osteotomies. A comparison of three stabilization techniques. Oral Surg Oral Med Oral Pathol. 1994;78:696–704. doi: 10.1016/0030-4220(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 26.Yoshida K, Rivera GA, Matsuo N, Takaishi M, Inamoto H, Kurita K. Long-term prognosis of BSSO mandibular relapse and its relation to different facial types. Angle Orthod. 2000;70:220–226. doi: 10.1043/0003-3219(2000)070<0220:LTPOBM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, van’t Hof MA. Stabilization of sagittal split setback osteotomis with miniplates: a prospective, multicentre study with two- year follow-up. Int J Oral Maxillofac Surg. 2005;34(5):487–494. doi: 10.1016/j.ijom.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 28.Chung DH, Hatch JP, Dolce C, Van Sickels JE, Bays RA, Rugh JD. Positional change of the hyoid bone after bilateral sagittal split osteotomy with rigid and wire fixation. Am J Orthod Dentofacial Orthop. 2001;119(4):382–389. doi: 10.1067/mod.2001.112670. [DOI] [PubMed] [Google Scholar]
- 29.Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthod Orthognath Surg. 1996;11:191–204. [PubMed] [Google Scholar]