Abstract
Masseter hypertrophy is an uncommon condition, characterized by an increase in the volume of the masseter region, with the patient presenting functional and aesthetic complaints. Several therapeutic modalities have been suggested for this condition, however, a surgical approach usually presents consistent results in more complex cases. The objective of this article is to report a clinical case of masseter hypertrophy associated with class IV of Kin, treated through partial removal of the masseter muscle, bichectomy and genioplasty. Surgery was performed under general anesthesia in a hospital setting. The planning was previously carried out through prototyped models and radiographs to remove the excess bone shown in the mandibular angle region. Surgical treatment of masseter hypertrophy is effective and long-lasting in severe cases. Additional surgical procedures must be performed in order to provide the best possible result according to the facial deformity found.
Keywords: Masseter hypertrophy, Buccal fat pad, Genioplasty, Surgical treatment
Introduction
Masseter hypertrophy is a rare, asymptomatic, benign condition with uncertain etiology, which can result in functional problems and aesthetic complaints. Most patients complain of an enlargement in the lower third of the face, close to the mandibular angles and muscle pain in that region, which are characteristic of muscle hyperactivity and which, due to the excessive traction force exerted by the muscle in this region, can result in changes in morphology normal of the mandibular angle, the most common being the bone spur, which can be observed through imaging exams and in some cases through palpation [1–3].
Several therapeutic modalities have been used over the years for the treatment of masseter hypertrophy with the main emphasis on Botulinum Toxin A and surgical treatment, with both showing good results [2–4].
Although botulinum toxin A is a less invasive method, it has disadvantages such as the need for several applications, the possibility of inducing changes in muscle structure as well as recurrences in cases of large hypertrophies [4–6].
Surgical management has been described in the literature for many years. In this type of treatment, an excess part of the muscle is surgically removed (approximately 2/3 of the internal face of the muscle), as well as the bone spur [2, 3]. Although surgery can be performed through extra-oral access [1], intra-oral access is undoubtedly the most recommended today. In many cases, additional procedures to optimize facial harmonization can be performed at the same time and even though the same surgical access as in the case of bichectomy, where part of the Bichat's adipose body can be removed, aesthetically improving the contour of the middle third of the face, allowing a better demarcation between this and the lower third, leaving them with a more triangular shape [7]. As well as the association with chin repair for vertical chin augmentation, in order to minimize the brachycephalic pattern, especially in Kim's class IV cases [8].
The aim of this study is, through a case report of masseter hypertrophy and retrogenia, to describe the surgical steps for the partial removal of the masseter muscle bilaterally, the buccal fat pad and the genioplasty, to correct this clinical condition.
Case Report
In order to carry out this study, the patient's free and informed consent was obtained, who authorized the publication of her images and exams in this journal.
KCL patient, 20 years old, attended an Oral and Maxillofacial Surgery service, complaining of enlargement of the lower third of the face in the region of mandibular angles, the constant bite of the cheek mucosa and mild myalgia. The clinical examination showed an increase in the thickness of the masseter muscle bilaterally asymmetrically, with greater volume on the right, as well as hyperfunction (Fig. 1). In addition, he complained of a protrusion in the middle third of his face and that his chin was small. Imaging exams revealed the absence of pathological lesion in the mandible, however, it was possible to observe the bone spur in the region of the mandibular angle bilaterally, uniform hypodensity in the hypertrophied masseteric musculature and retrogenia (Fig. 2). During the initial anamnesis, no parafunctional habits that could influence the presented muscle hypertrophy were identified. After clinical and tomographic evaluation with prototyping, the following planning was defined: Myotomy of approximately 2/3 of the right masseter muscle and 1/3 of the left one; ostectomy of the bone spurs in the region of the mandibular angle bilaterally, with quantification of bone volume removed through previous measurements in the prototype; bilateral bichectomy and genioplasty for vertical enlargement and chin advancement, with interposition of a bone graft in a block from the right mandibular angle.
Fig. 1.
Preoperative frontal and lateral clinical view in A and B
Fig. 2.
Preoperative panoramic radiography showing the large bone spur in the bilateral mandibular angle region in A; side view of rapid prototyping showing excess bone in the bilateral mandibular angle region in B and C
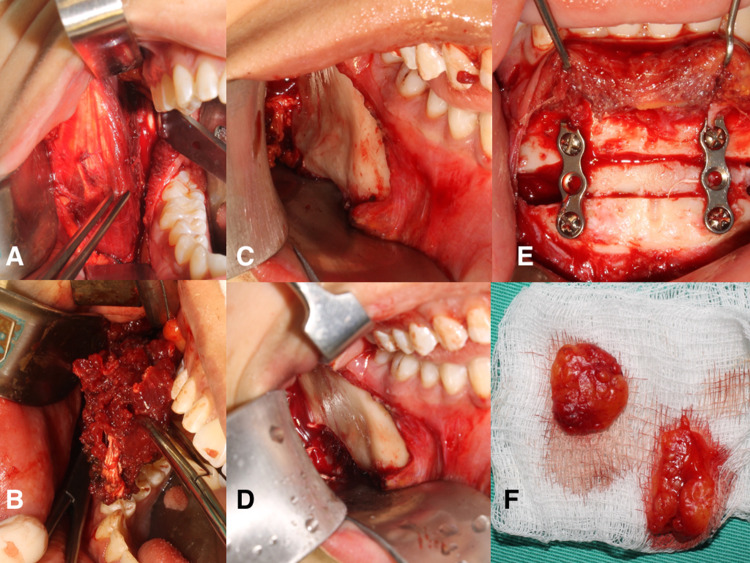
Initially, an incision was made in the mucosa of the retromolar region, in order to visualize and individualize the masseter muscle in that region. After identifying the muscle, blunt divulsion was performed in the anteroposterior direction, isolating the medial portion to be resected, thus avoiding injuries to the Stensen’s duct and branches of the facial nerve (Fig. 3A). Myotomy of this portion was performed with electrocautery, guaranteeing local hemostasis (Fig. 3B). The detachment of the fibers of the masseter was performed laterally to the pterygomasteric aponeurosis, with exposure of the mandibular angle, to remove the bone spur, in your full bone thickness. The execution was performed with a reciprocating saw and surgical drill 702 (Fig. 3C, D). Through the upper part of the same access, a blunt dissection was performed to reach the buccal fat pad, which was identified and removed bilaterally in a symmetrical way. This removal of the buccal fat pad was performed after the emergence of the parotid papilla in order to avoid damage to the Stensen’s duct. Genioplasty occurred through intraoral access in the mandibular vestibule, with a vertical increase of 4 mm and 2 mm advancement, using the spur as an interpositional bone graft in the chin gap, which was fixed with two 2.0 mm straight plates. and monocortical screws (Fig. 3D, E). The sutures were performed with 4-0 Monocryl resorbable thread.
Fig. 3.
Initial view of the masseter muscle after the intraoral incision in A; excess masseter muscle being removed with the aid of electrocautery in B; Vista clínica do esporão ósseo no ângulo mandibular direito in C; removal of the bone spur on the right side of the mandibular angle in D; genioplasty for correction of vertical chin deficiency, with interposition of an autogenous bone block removed from the right mandibular angle in E; buccal fat pad removed from the adipose body of the cheek bilaterally in F
After 3 days postoperatively, the patient was referred for physiotherapy, for early return of muscle function and this was maintained for 4 weeks. At the moment, the patient is in the 16-month postoperative period, with good masticatory function, without palpable bone step at the angle of the mandible and signs of recurrence, and with a harmonious and symmetrical facial contour (Fig. 4A, B).
Fig. 4.
Frontal and lateral postoperative view 18 months after surgery in A and B
Discussion
Masseter hypertrophy is a rare benign condition that, however, can bring chewing, psychological and aesthetic discomfort. The choice of treatment modality must consider the type and magnitude of the deformity, the patient's profile and the professional's experience, with surgical treatment being a safe option with acceptable morbidity with low recurrence [1–3].
Partial removal of the masseter muscle was initially described by Gurney 1947 [9], where the author recommends the removal of 2/3 to 3/4 of the hypertrophied masseter muscle. This approach is still followed to these days, with other authors recommending the same amount of removal in order to minimize the effects of masseter hypertrophy [1, 3]. It is also important that the removal is performed on the innermost surface of the muscle, in order to avoid noble structures such as the Stensen’s duct and the facial nerve [2]. In this article, we chose to remove 2/3 of the masseter on the right side and 1/3 of the masseter on the left side, since there was an asymmetry, with greater volume on the right side, and this removal in different amounts of both sides aimed to correct not only the muscular hypertrophy, but also the facial asymmetry presented by the patient.
The technique of partial removal of the masseter muscle through intraoral access is undoubtedly the most accepted. It allows a good visualization of the operative field and less morbidity when compared to the extra-oral technique. As for disadvantages, we can mention mainly a greater difficulty to remove the bone spur at the base of the angle of the mandible, which should be performed with the aid of special retractors, piezo tips or reciprocating saws [2, 10]. We did not observe any technical difficulties to perform the surgery by intraoral route when using the instruments described above.
Due to the surgical procedure leading to a partial removal of the masseter muscle, some phenomena in the postoperative period are expected, such as: Pain, trismus, hematoma, and edema [2]. In order to minimize these complications, intense postoperative physiotherapy should be instituted as early as possible, so that masticatory function and aesthetics can be recovered more quickly, in addition to greater pain control [11]. This physiotherapy should be performed initially with compressive bandages to prevent bruising and edema [2, 12] and later with manual therapy in order to allow an early function of the muscle [11]. In our routine, postoperative physiotherapy is always performed by an experienced and qualified professional, through initial bandages in the first three days, manual therapy for early jaw movement and low-level laser therapy, in order to control edema, and promote rapid tissue healing, small muscle fibrosis formation and precocious return of normal mandibular movement. A well-directed and well-conducted physiotherapy are essential for muscle recovery after partial removal of the masseter muscle, in order to avoid the formation of fibrous tissue that can generate excessive trismus in the postoperative period.
As a result of the excessive traction of the masseter muscle in the region of the mandibular angle, there is a stimulus for the formation of new bone in this region, a phenomenon known as "Wolff’s law", and therefore it is observed that the action of a muscle directly contributes to bone morphology, case of masseter hypertrophy, with the formation of a bone spur in the region of the “gonion” [13]. Following the philosophy of this line of thought, only the removal of the spur would not be enough to correct the asymmetry, since the muscle stimulus would still exist, meaning that the partial removal of the muscle, as well as the spur, would appear to be adequate for the aesthetic–functional resolution of these cases.
The prominence of the mandibular angle was well described by Kim et al. 2001 [8], who established four classifications based on the prominence of the mandibular angle. In the most complex (class IV), there is an excessive prominence of the mandibular angle associated with retrogenia, generating aesthetic and functional problems. In these cases, the authors recommend the performance of an osteoplasty in the mandibular angle region associated with masseter myotomy and chin repair to correct the aesthetic problem [8]. This correction of the chin can be performed in conjunction with bilateral sagittal osteotomy of the mandibular ramus when the patient has dentofacial discrepancies or just genioplasty, when there is a dentofacial and maxillomandibular balance, as in the present case.
There is still no consensus in the literature regarding the removal of the bony prominence together with the partial removal of the masseter muscle to correct bilateral masseter hypertrophy. It is known that the excessive force generated by the hypertrophied muscle creates this prominence [14], and that is why some authors claim that only the removal of the bone spur at the angle of the mandible would be enough to correct the problem [2, 15], however other authors recommend the simultaneous partial removal of the masseter muscle in order to promote a better facial contour and improved esthetics, an opinion that is also followed by the authors of this article [3, 10]. Removal of the spur in the mandibular angle region generally does not generate visible or even palpable deformities, due to the existing tissue and muscle volume in this region that masks these changes [16].
Another co-adjuvant procedure performed in conjunction with the circular treatment of masseter hypertrophy is the removal of Buccal fat pad (Bichat's adipose body), known as a bichectomy. In these patients, it is common to find a greater projection of the middle third of the face in the transverse direction and the performance of bichectomy can generate greater harmony of the face making the middle third thinner and proportional to the lower third [2, 7]. This procedure has become very popular among professionals and patients in recent years, and although it is technically simple, it can present important sequelae such as: Hematoma, persistent hemorrhage, injury to the parotid duct and facial nerve injuries [17, 18]. We recommend that this procedure be performed only by experienced facial surgeons, avoiding complications or bypassing them when they occur.
Although the surgical treatment of masseter hypertrophy is aesthetically beneficial, some complications can occur, especially those related to asymmetries. The amount of hypertrophic muscle to be removed is usually performed empirically, depending largely on the experience of the surgical team [1, 7]. This increases the possibility of facial asymmetries, which can be treated with dermal fillers, which are minimally invasive techniques with good aesthetic results [19].
Conclusion
Bilateral masseter hypertrophy is an uncommon condition that can trigger aesthetic, functional and psychological problems. Surgical treatment is effective in correcting this condition, however, prior planning, specific instruments, and intense and specialized physiotherapy are necessary in order to guarantee better results and the early return of patients to their normal functions.
Funding
The financial support was provided by the authors and there was no corporate involvement.
Declarations
Conflict of interest
There are no conflicts of interest regarding the authors listed on the title page.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
The patient in this study signed a free and informed consent form in which she authorizes the publication of her images or photographs in any type of media with an educational purpose, research and dissemination of scientific knowledge.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rispoli DZ, Camargo PM, Pires Junior JL, Fonseca VR, Mandelli KK, Pereira MAC. Benign masseter muscle hypertrophy. Braz J Otorhinolaryngol. 2008;74:790–793. doi: 10.1016/S1808-8694(15)31393-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andreishchev AR, Nicot R, Ferri J. Mandibular angle resection and masticatory muscle hypertrophy—a technical note and morphological optimization. Rev Stomatol Chir Maxillofac Chir Orale. 2014;115:301–307. doi: 10.1016/j.revsto.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Ozkan BT, Tabrizi R. Management of bilateral masseter muscle hypertrophy. J Craniofac Surg. 2012;23:14–15. doi: 10.1097/SCS.0b013e31824207a2. [DOI] [PubMed] [Google Scholar]
- 4.Al-Muharraqi M, Fedorowicz Z, Al Bareeq J, Al Bareeq R, Nasser M. Botulinum toxim for masseter hypertrophy. Cochrane Database Syst Rev. 2009;21:CD007510. doi: 10.1002/14651858.CD007510.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Huang JH, Chen G, Chen XD, Zhou BR, Luo D. A comparative study of the efficacy and safety of radiofrequency ablation and botulinum toxin A in treating masseteric hypertrophy. Exp Ther Med. 2014;7:1203–1208. doi: 10.3892/etm.2014.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gedrenge T, Gredes T, Spassov A, Mai R, Kuhn DU, Dominiak M, et al. Histological changes and changes in the myosin mRNA content of the porcine masticatory muscles after masseter treatment with botulinum toxin A. Clin Oral Investig. 2013;17:887–896. doi: 10.1007/s00784-012-0750-0. [DOI] [PubMed] [Google Scholar]
- 7.Carbonell A, Salavert A, Planas J. Ressection of the buccal fat pad in the treatment of the hypertrophy of the masseter muscle. Aesth Plast Surg. 1991;15:219–222. doi: 10.1007/BF02273861. [DOI] [PubMed] [Google Scholar]
- 8.Kim SK, Han JJ, Kim JT. Classification and treatment of proeminent mandible angle. Aesth Plast Surg. 2001;25:382–387. doi: 10.1007/s002660010150. [DOI] [PubMed] [Google Scholar]
- 9.Gurney CE. Chronic bilateral benign hypertrophy of the masseter. Ann J Surg. 1947;73:137–139. doi: 10.1016/0002-9610(47)90304-8. [DOI] [PubMed] [Google Scholar]
- 10.Trento GS, Benato LS, Rebellato NLB, Kluppel L. Surgical resolution of bilateral hypertrophy of masseter muscle through intraoral approach. J Craniofac surg. 2017;28:400–402. doi: 10.1097/SCS.0000000000003779. [DOI] [PubMed] [Google Scholar]
- 11.Albertin A, Kerppers II, Amorim CF, Costa RV, Ferrari Corrêa JC, Oliveira CS. The effect of manual theraphy on masseter muscle pain and spasm. Electromyogr Clin Neurophysiol. 2010;50:107–112. [PubMed] [Google Scholar]
- 12.Roncevic R. Masseter muscle hypertrophy. Aetiology and therapy. J Maxillofac Surg. 1986;14:344–348. doi: 10.1016/S0301-0503(86)80322-8. [DOI] [PubMed] [Google Scholar]
- 13.Hoyte DA, Enlow DH. Wolff`s law and the problem of the muscle attachment on resorptive surfaces of bone. Am J Phys Anthropol. 1966;24:205–213. doi: 10.1002/ajpa.1330240209. [DOI] [PubMed] [Google Scholar]
- 14.Beckers HL. Masseteric muscle hypertrophy ans its intra-oral surgical correction. J Maxillofac Surg. 1977;5:28–35. doi: 10.1016/S0301-0503(77)80072-6. [DOI] [PubMed] [Google Scholar]
- 15.Bocchialini G, Castellani A, Negrini S, Rossi A. New management in bilateral masseter muscle hypertrophy. Craniomaxillofac Trauma Reconstr. 2017;10:325–328. doi: 10.1055/s-0036-1592089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Landes C, Tran A, BAllon A, et al. Low to hig oblique ramus piezoosteotomy: a pilot study. J Craniomaxillofac Surg. 2014;42:901–909. doi: 10.1016/j.jcms.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 17.Alcantara MTD, Ribeiro NRB, Abreu DF. Complications associated with bichectomy surgery: a literature review. Minerva Dent Oral Sci. 2021; Aug 3. 70(4):155–160 [DOI] [PubMed]
- 18.Moura LB, Spin JR, Spin Neto R, Pereira Filho VA. Buccal fat pad removal to improve facial aesthetics: an established technique? Med Oral Patol Oral Cir Bucal. 2018;23:478–484. doi: 10.4317/medoral.22449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farolch-Prats L, Nome-Chamorro C. Facial contouring by using dermal fillers and botulinum toxin A: a pratical approach. Aesth Plast Surg. 2019;43:793–802. doi: 10.1007/s00266-019-01361-1. [DOI] [PMC free article] [PubMed] [Google Scholar]