Abstract
Introduction and importance
Heterotopic pregnancy is the occurrence of pregnancies in at least two different implantation sites in the same time. The diagnosis is one of the most difficult of the gynecological emergencies. In 2021 this pathology still underdiagnosed and remains unknown by physicians. Most patients are admitted in critical stage.
Cases presentations
We reported 5 cases of heterotopic pregnancies in symptomatic women admitted from January 2021 to December 2021, in maternity department, mother and child hospital abderrahim Harouchi, Ibn Rochd University Hospital of Casablanca. The frequency of this pathology in our hospital in 2021 is about 10% of ectopic pregnancies (5/52 cases of ectopic pregnancies). All the cases were received in critical phase of the pathology (vascular collapsus or hemodynamic shock). The mean diagnostic was suspected in gray scale ultrasound that show an intrauterine pregnancy associated with adnexal mass corresponding to hematosalpinx or gestational sac in the uterine tubes with medium to high abundance hemoperitoneum. All of our cases were treated by laparotomy in emergency after resuscitation measures.
Clinical discussion
The existence of intrauterine pregnancy does not exclude an ectopic pregnancy and often confuses the physician who consults the patient in early stage of symptoms. The clinical symptomatology is often related to a threatened or ongoing abortion, the diagnosis of heterotopic pregnancy is usually made in the stage of hemoperitoneum secondary to a rupture of the ectopic pregnancy. The standard treatment is conservative surgery, preferably by laparoscopy. The manipulation of the uterus must be careful to preserve the intra uterine pregnancy. Laparotomy retains its indications especially in forms with hemorrhagic shock. The abortion is not rare after surgery. A progestin treatment is always indicated.
Conclusion
The diagnosis of heterotopic pregnancy should not be delayed by the discovery of an intra-uterine gestational sac in symptomatic women and the adnexa must be systematically examined in the first trimester sonographic exam. The Diagnosis is often difficult and management should be initiated as soon as possible given the risk of maternal mortality.
Keywords: Heterotopic pregnancy, Ectopic pregnancy, Hemoperitoneum, Acute pelvic pain, Abdominal pregnancy, Case report
Highlights
-
•
Heterotopic pregnancy is the occurrence of pregnancies in at least two different implantation sites in the same time.
-
•
The diagnosis of heterotopic pregnancy should not be delayed by the discovery of a intra uterin gestational sac in symtomatic women and the adnexa must be systematically examined in the first trimester by sonographic exam.
-
•
The main treatment consists of removing the ectopic pregnancy, while preserving the intra uterine pregnancy, that make the second challenge after diagnoses.
1. Introduction and importance
Heterotopic pregnancy (HP) is the occurrence of an intrafallopian pregnancy and an ectopic pregnancy (EP) simultaneously, whatever its location [1]. The most common ectopic pregnancies are located in the fallopian tubes. Abdominal location increases the risk of maternal mortality up to 90 times higher than a normal IUP [2]. The diagnosis of a heterotopic pregnancy is still underdiagnosed and difficult. The presence of the intrauterine pregnancy at the sonographic exam can make confusion to the physician. The main treatment consists of removing the ectopic pregnancy, while preserving the IUP, that make the second challenge after diagnoses.
We report 5 cases of heterotopic pregnancy, diagnosed all of them in our maternity service, hospital mother and child Abderrahim Harrouchi, university hospital of Casablanca between January and December 2021. All of them were complicated by a large hemoperitoneum with vascular collapse. This pathology constitutes in this year 10% of all ectopic pregnancies (52 cases). Those cases reports have been reported in line with the SCARE 2020 criteria [3].
2. Cases presentations
For comparative approach of the cases, we aim to resume our cases in tables (Table 1, Table 2, Table 3, Table 4).
Fig. A.
Suspubic and transvaginal pelvic ultrasound showing and heterotopic pregnancy.
A1: Intrauterine pregnancy with embryo associated with a heterogenous left uterine adnexal mass without any embryological structures corresponding to hematosalpinx measuring 60 mm.
A2: Large hemoperitonum with floating intestines.
A3: Sagittal view of the pelvis showing an intra uterine pregnancy and retrouterine heterogenous mass with a large hematoma taking all the Douglas pouch. Pelvic organs floating on the hemoperitoneum.
A4: Axial view of the pelvis showing a left hematosalpinx.
Fig. B.
Transvaginal (B1) and suspubic (B2) pelvic ultrasound: Heterotopic pregnancy, double gestational sac in the uterus and fallopian tube, with embryo in each one. We can see the hemoperitoneum around the ectopic pregnancy.
Fig. C.
Intra operative finding of the heterotopic abdominal pregnancy: the localisation of the ectopic pregnancy in the abdominal side of the fallopian tube with the presence of a gestational sac with embryo floating in the peritoneal cavity (C2).
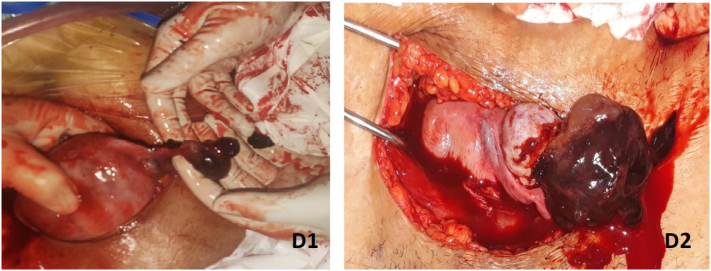
Fig. D.
Intraoperative finding of ectopic pregnancy in the left ampular tube associated with large hemoperitoneum.
Table 1.
Summary of clinical features of the five cases.
| Profile | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Age (years) | 40 | 38 | 36 | 28 | 32 |
| Parity | 5 | 2 | 0 | 0 | 3 |
| Pathological medical or surgical history | No | 2 cesarean sections | 2 spontaneous miscarriage | Repeated genital infections | No |
| Contraception | Micro-progestative pills | Intra-uterine contraceptive device | No | No | No |
| Smoking exposition | No | Passive exposition | Active exposition | Active exposition | Passive exposition |
| History of ectopic pregnancy | No | No | No | Right ectopic pregnancy 6 months ago treated with methotrexate | No |
| Induced or spontaneous pregnancy | Spontaneous | Spontaneous | Citrate clomiphene induced pregnancy | Spontaneous | Spontaneous |
| Interval between beginning of symptoms and diagnostic (days) | 10 | 23 | 7 | 12 | 15 |
| Symptoms at the admission | |||||
| Acute pelvic pain | Yes (left iliac fossa) | Yes (left iliac fossa) | Yes (left iliac fossa) | Yes (right iliac fossa) | Yes (left iliac fossa) |
| Menstruation's delay (days) | 66 | 60 | 70 | 52 | 72 |
| Hemodynamic perturbations | Vascular collapse | Vascular collapse | Vascular collapse | Vascular collapse | Vascular collapse |
| Cutaneous-mucosal paleness | Yes | Yes | Yes | Yes | Yes |
| Peritoneal irritation signs | Yes | Yes | Yes | Yes | Yes |
| Uterin bleeding | No | Minimal | No | Minimal | Minimal |
Table 2.
Summary of sonographic (suspubic and transvaginal) and biological features of the five cases.
| Profile | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Sonographic parameters | |||||
| Intrauterine pregnancy | Active intrauterine pregnancy of 7 weeks and 5 days of gestation according to Crown-rump length (CRL) (Fig. A) |
Active intrauterine pregnancy of 7 weeks and 6 days of gestation according to CRL | Active intra uterine pregnancy of 9 weeks of gestation according to CRL (Fig. B) |
Intrauterine gestational sac without any embryological structure according to 5 weeks of gestation. | Active intrauterine pregnancy of 9 weeks and 2 days of gestation according to CRL. |
| Ectopic pregnancy | Left uterine hematosalpinx measuring 45 mm without any embryo structure (Fig. A) | Left uterine hematosalpinx measuring 60 mm without any embryo structure | Left uterine Ectopic pregnancy with an embryo of 9 weeks according to CRL with heart beating. (Fig. B) | Right uterine heterogenous adnexal mass measuring 6 cm corresponding to hematosalpinx | Left uterine adnexal mass with an ectopic pregnancy of 8 weeks according to CRL. Cardiac activity was presented. |
| Hemoperitoneum | Large | Large | Large | Large | Large |
| Biological parameters | |||||
| Hemoglobin (g/dl) | 6.9 | 8.1 | 5.4 | 5,2 | 8,7 |
| Platelets (ele/mm3) | 308,000 | 156,000 | 203,000 | 120,000 | 150,000 |
| Hematocrit (%) | 20 | 28 | 29.1 | 18 | 25 |
| Prothrombin level (%) | 60 | 90 | 79 | 52 | 71 |
| Creatinine (g/dl) | 4,8 | 5,6 | 14 | 17 | 12 |
Table 3.
Summary of management features of the five cases.
| Profile | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Anesthetic management | |||||
| Anesthesia mode | General | ALR | General | General | General |
| Red blood cells | 2 | No | 3 | 3 | 1 |
| Transfusion (unit) | |||||
| ICU admission | No | No | Yes (1 day) | Yes (3 days) | No |
| Surgical approach | Laparotomy (vascular collapse) | Laparotomy (vascular collapse) | Laparotomy (vascular collapse) | Laparotomy (hemorrhagic choc) | Laparotomy (vascular collapse) |
| Intra-operative finding | |||||
| Hemoperitoneum (ml) | 1000 ml | 600 ml | 1000 ml | 1500 ml | 700 ml |
| Localisation of the ectopic pregnancy | Ruptured ectopic pregnancy in left ampular fallopian tube (Fig. D1) | Ruptured ectopic pregnancy in left ampular fallopian tube | Abdominal ectopic pregnancy with trophoblastic implantation in the abdominal side of the left ampular fallopian tube an intact gestational sac with embryo floating in intraperitoneal cavity. (Fig. C) | Ruptured ectopic pregnancy in right isthmic fallopian tube | Ruptured ectopic pregnancy in left ampular fallopian tube (Fig. D2) |
| Anatomical conditions of the fallopian tube | Damaged | Damaged | Trophoblastic invasion of the fallopian tube (hemorrhagic dissection) | Damaged | Damaged |
| Predisposing anatomical cause | No | Multiple peritoneal adhesions | No | Multiple peritoneal adhesions (chlamydia infection sequels). | No |
| Treatment | Left salpingectomy | Left salpingectomy | Left salpingectomy | Right salpingectomy | Left salpingectomy |
Table 4.
Summary of post-operative management and evolution features of the five cases.
| Profile | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Post-operative management | Vaginal progesterone 800 mg/day | Vaginal progesterone 800 mg/day | Vaginal progesterone 800 mg/day | No vaginal progesterone | Systematic vaginal progesterone 800 mg/day (4 weeks) |
| Evolution | Normal evolution of the IUP | Abortion 1 week later | Normal evolution of the IUP | Spontaneous miscarriage 2 days later | Normal evolution of the IUP. |
3. Clinical discussion
Heterotopic pregnancy is a rare form of twin pregnancy, defined by the coexistence of an ectopic and intrauterine pregnancy. It was described for the first time by DUVERNET at 1708 [4].
The frequency was increased with the avenement of assisted reproductive techniques (ART), especially the frequency of use of ovulation inducer. The incidence is estimated at 1/30000 when associated with spontaneous pregnancy, above 1/100 when associated with in vitro fertilization, and 1/900 when using clomiphene citrate [5], [6], [7].
In 2021, the frequency of this pathology in our maternity was about 10% of all ectopic pregnancies (52 cases). One of them was induced with clomiphene citrate.
The mechanical or functional fallopian tube factors are the same ones for the ectopic pregnancies (endometriosis, peritoneal adhesions, infections, pelvic inflammation…). Multiple embryo transfers in ART techniques are also associated with high risk of heterotopic pregnancies [8].
The diagnosis of heterotopic pregnancy remains one of the greatest challenges of the gynecological emergencies. It is often delayed due to the early visualization of an intrauterine sac, that confused the physician, with late detection of adnexal abnormalities. Also the clinical symptoms are often related to an ongoing abortion.
The most common symptoms include abdominal pain, vaginal bleeding, peritoneal irritation and uterine enlargement, making the diagnostic easier [9], [10]. Otherwise, the symptoms can be misleading when we had isolated abdominal pain associated with intrauterine pregnancy. This situation is very dangerous, and the evolution can be towards to rupture of the ectopic pregnancy or even maternal shock.
In our five cases, diagnosis was delayed at minimal 7 days, after symptoms declaration, going to 23 days. All of them was diagnosed at advanced stage with vascular collapse.
The diagnostic is based on suprapubic and transvaginal ultrasound by specifying the presence and the vitality of the intrauterine pregnancy and the site of the ectopic pregnancy. Although, the sensitivity of ultrasound can vary from 26.3% to 92.4% [11].
Often, the presence of an intrauterine pregnancy leads to difficulties of interpretation, especially in the youngest pregnancies that can make confusion to inexperimented physician. In 2 cases the adnexal mass was interpreted as an ruptured hemorrhagic cyst.
The echographic signs that allow to confirm the diagnosis are the presence of intrauterine gestational sac associated with heterogenous adnexal mass corresponding to hematosalpinx or the visualization of latero-uterine mass surrounded by an echogenic trophoblastic halo, sometimes containing an embryon. The presence of hemoperitoneum supports the diagnostic [12], [13].
In the above reported clinical cases, both intrauterine and ectopic pregnancies were visualized by ultrasound, 3 with hematosalpinx and 2 with evolutive ectopic pregnancies with embryo outside the uterine cavity. Hemoperitoneum was large in 4 cases.
The treatment of heterotopic pregnancies consists of interventing as early as possible on the ectopic pregnancy, respect the intrauterine one, preserve patient fertility, and avoid the recurrence.
Laparoscopy should be performed as the first line treatment, especially in case of uncertain diagnosis [14]. It has the advantage of avoiding the risk of uterine manipulation to preserve the intrauterine pregnancy, compared to laparotomy, which can cause uterine irritability and postoperative spontaneous abortion.
Urgent Laparotomy is recommended in cases of hemodynamic instability or large hemoperitoneum like in our cases. Manipulation of the uterus should be minimal [15].
Salpingectomy was performed in all our cases because of anatomical damage following the rupture in 4 of them and the deep implantation of the trophoblast in the case of the abdominal pregnancy.
For asymptomatic, hemodynamically stable patients and no evolutive ectopic pregnancy, expectant management can be suggested Intra-muscular injection of Methotrexate maybe an alternative only if the intrauterine pregnancy is not progressive [16].
A progestin therapy can be associated to avoid post-operative abortion. A 800 mg of Micronized progesterone was administered to four of our patients with intrauterine active pregnancies. One of them had spontaneous abortion 1 week later versus 3 with evolutive pregnancies. We report a second spontaneous abortion in our series without any hormonal treatment, but the evolution of the pregnancy was uncertain.
The prognosis of the Heterotopic pregnancy depends on the early diagnoses and treatment [17]. Precisely treated, 30 to 75% of intrauterine pregnancies progress to term [18].
The complications are the result of late diagnosis, they are often hemorrhagic. In our cases, all of our patients had a severe anemia, 4 of them was transfused with red cell blood, 2 had elevated creatinine level and was admitted in intensive care unit.
Take away points:
-
1-
The exam of adnexa must be systematic in the first sonographic exam for pregnancy in all patients.
-
2-
Detailed history and physical examination are importance to explore all risk factors related to heterotopic pregnancy
-
3-
The presence of intra uterine pregnancy doesn't make optional the exam of adnex, especially if the patient reports symptoms or ectopic pregnancy risk factors.
-
4-
The delayed diagnoses limit the possibility of conservative treatment and can be responsible of secondary infertility.
4. Conclusion
The frequency of heterotopic pregnancy has increased in recent years, with the emergence of medically assisted procreation. The diagnosis is often difficult.
The presence of any symptoms or ectopic pregnancies risk factors, associated with intrauterine pregnancy must lead the physician to miniciously screen of the adnexa to research any abnormalities.
The standard treatment is conservative surgery, preferably by laparoscopy. However, treatment by laparotomy is not uncommon.
Through these case reports, we brought to light the importance correlation of the clinical symptoms, and all risk factors in order to make the diagnosis as early as possible.
Patient consent
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patients.
Ethical approval
I declare on my honor that the ethical approval has been exempted by my establishment.
Funding
None.
Author contribution
Lamrissi Amine: Corresponding author writing the paper and operating surgeon
Antaky Redouane: writing the paper and operating surgeon
Mourabbih mariam: writing the paper
Jalal Mohamed: study concept
Fichtali Karima: study concept
Bouhya Said: correction of the paper and operating surgeon.
Guarantor
Dr. Lamrissi Amine.
Registration of research studies
researchregistry2464.
Declaration of competing interest
The authors declare having no conflicts of interest for this article.
References
- 1.Siraj S.H.M., Wee-Stekly W.W., Chern B.S.M. Heterotopic pregnancy in a natural conception cycle presenting as acute abdomen: a case report and literature review. Gynecol. Minim. Invas. Ther. 2014;3:100–102. [Google Scholar]
- 2.Mihmanli V., Kilickaya A., Cetinkaya N., et al. Spontaneousheterotopicpregnancy presenting with hemoperitoneum. J. Emerg. Med. 2016;50:44–46. doi: 10.1016/j.jemermed.2015.02.050. [DOI] [PubMed] [Google Scholar]
- 3.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 4.DA Bright FB Gaupp. Heterotopic pregnancy; a reevaluation. J Am Board Fam Practice; 3: 125-8. [PubMed]
- 5.Bataille P., Reynard A., Ducarme G. Spontaneous heterotopic triplets–a review of literature. J. Gynecol. Obstet. Hum. Reprod. 2017;46(8):657–659. doi: 10.1016/j.jogoh.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Bambara M., Dao B., Toure B., Ouedraogo B., Koalaga P.A., Kone B. Grossesses hétérotopiques: à propos de trois cas. Louvain Med. 2002;121(8):383–387. [Google Scholar]
- 7.Ooki S. Estimation of the contribution of assisted and non-assisted reproductive technology fertility treatments to multiple birthsur ding the past 30 years in Japan: 1979–2008. Twin Res.Hum. Genet. 2011;14:476–483. doi: 10.1375/twin.14.5.476. [DOI] [PubMed] [Google Scholar]
- 8.Ooki S. Estimation of the contribution of assisted and non-assisted reproductive technology fertility treatments to multiple birthsur ding the past 30 years in Japan: 1979–2008. Twin Res.Hum. Genet. 2011;14:476–483. doi: 10.1375/twin.14.5.476. [DOI] [PubMed] [Google Scholar]
- 9.Barrenetxea G., Barinaga-Rementeria L., Lopez de Larruzea A., Agirregoikoa J.A., Mandiola M., Carbonero K. Heterotopic pregnancy: two cases and a comparative review. Fertil. Steril. 2007;87(2):417. doi: 10.1016/j.fertnstert.2006.05.085. [DOI] [PubMed] [Google Scholar]
- 10.Ciebiera Michal, Slabuszewska-Jozwiak Aneta, Zareba Kornelia. 2018 Dec 31. Heterotopic pregnancy – how easily you can go wrong in diagnosing? A case study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li X.H., Ouyang Y., Lu G.X. Value of transvaginal sonography in diagnosing heterotopic pregnancy after in-vitro fertilization with embryo transfer. Ultrasound Obstet. Gynecol. 2013;41:563–569. doi: 10.1002/uog.12341. [DOI] [PubMed] [Google Scholar]
- 12.Ousehal A., Mamouchi H., Ghazli M., Kadiri R. Grossesse hétérotopique: intérêt de l'échographie sus pubienne (à propos d'un cas) J. Radiol. 2001;82(7):851–853. [PubMed] [Google Scholar]
- 13.Li X.H., Ouyang Y., Lu G.X. Value of transvaginal sonography in diagnosing heterotopic pregnancy after in-vitro fertilization with embryo transfer. Ultrasound Obstet. Gynecol. 2013;41:563–569. doi: 10.1002/uog.12341. [DOI] [PubMed] [Google Scholar]
- 14.Sefroui O., Azyer M., Babahabib A., Kaanane F., Matar N. Pregnancy in rudimentary uterine horn: diagnosis and therapeutic difficulties. Gynecol. Obstet. Tertil. 2004;32(4):308–310. doi: 10.1016/j.gyobfe.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 15.J.-B. Li L.-Z. Kong J.-B. Yang G. Niu L. Fan J.-Z. Huang S Chen Management of Heterotopic Pregnancy: Experience From 1 Tertiary Medical Center Medicine Observational study. [DOI] [PMC free article] [PubMed]
- 16.Morelli A., Ratozz P., Fleischer A. Diagnosis and treatement of intra-uterine pregnancy associated with tubal pregnancy. Minerva Gynecol. 1994;46(9):517. [Google Scholar]
- 17.Habana A., Dokras A., Giraldo J., Jones E.E. Cornual heterotopic pregnancy: contemporary management options. Am. J. Obstet. Gynecol. 2000;182:1264–1270. doi: 10.1067/mob.2000.103620. [DOI] [PubMed] [Google Scholar]
- 18.Bornstein E., Berg R., Santos R., Monteagudo A., Timor-Tritsch I.E. Term singleton pregnancy after conservative management of a complicated triplet gestation including a heterotopic corneal monochorionic twin pair. J. Ultrasound Med. 2011;30(6):865–867. doi: 10.7863/jum.2011.30.6.865. [DOI] [PubMed] [Google Scholar]