Abstract
As of May 2022, there have been more than 400 million cases (including re-infections) of the systemic acute respiratory syndrome-coronavirus 2 (SARS-CoV-2), and nearly 5 million deaths worldwide. Not only has the coronavirus disease 2019 (COVID-19) pandemic been responsible for diagnosis and treatment delays of a wide variety of conditions, and overwhelmed the allocation of healthcare resources, it has impacted the epidemiology and management of cerebrovascular disease. In this narrative review, we summarize the changing paradigms and latest data regarding the complex relationship between COVID-19 and cerebrovascular disease. Paradoxically, although SARS-CoV-2 has been associated with many thrombotic complications—including ischemic stroke—there have been global declines in ischemic stroke and other cerebrovascular diseases. These epidemiologic shifts may be attributed to patient avoidance of healthcare institutions due to fear of contracting the novel human coronavirus, and also related to declines in other transmissible infectious illnesses which may trigger ischemic stroke. Despite the association between SARS-CoV-2 and thrombotic events, there are inconsistent data regarding targeted antithrombotics to prevent venous and arterial events. In addition, we provide recommendations for the conduct of stroke research and clinical trial planning during the ongoing COVID-19 pandemic, and for future healthcare crises.
Keywords: COVID-19, Stroke, Intracranial hemorrhages, Outcomes research, Epidemiology
Introduction
Since the coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization on March 11, 2020, there has been an unprecedented shift in the epidemiology and management of cerebrovascular disease. While COVID-19 screening and contact precautions are now integrated into our treatment pathways, it has taken local and global efforts to transform our experiences into a seamless practice. In addition to the ways this pandemic has altered processes of medical care, COVID-19 has directly and indirectly influenced the epidemiology of cerebrovascular disease with respect to perceived disease incidence (according to global admissions data including comprehensive and primary stroke centers) and outcomes [1,2]. In this narrative review, we summarize the complex and evolving relationship between COVID-19 and cerebrovascular disease.
Impact on stroke epidemiology
Early local reports of the dramatic decline in stroke admissions at the onset of the COVID-19 pandemic have been confirmed on a global level [2]. Declines in ischemic stroke [1], intracerebral hemorrhage (ICH) [2], and subarachnoid hemorrhage admissions [3] have been shown to inverse correlate with the surge in COVID-19 admissions [2,4]. However, declines were observed irrespective of the burden of COVID-19 and the high-, intermediate-, or low-stroke volumes at hospitals [2]. Importantly, the decline in stroke rates have been observed in large observational cohorts of health care institutions, and while they likely reflect a precipitous decline in the true incidence of cerebrovascular disease during the COVID-19 pandemic, we cannot say with certainty that the epidemiology of cerebrovascular disease has been altered by the pandemic. Without population-based cohort data, we cannot know the extent of this misclassification bias. Therefore, any change in the incidence rate of cerebrovascular events described in this narrative review is purely a reflection of the change in new diagnoses made in a health care setting.
There are several hypotheses that may explain the global reduction in the incidence of acute cerebrovascular disease. Zhao et al. [5] reported a 40% decline in hospitalizations due to stroke across 280 centers in China, with a 27% decline in the use of intravenous thrombolysis (IVT) and a 25% decline in the use of endovascular thrombectomy (EVT). The most common reasons patients avoided the hospital were fear of contracting the virus (93.8%) while lack of sufficient public transportation (46.7%) and insufficient first aid knowledge (35.2%) were other barriers observed in this study.
In addition to fear of contracting the virus, the incidence of new acute stroke diagnoses may have declined due to social distancing and other practices (e.g., use of face masks). With this hypothesis, the true incidence rate of stroke may have been unaffected, but those with milder symptoms may have been unaware of their deficits. Indeed, several studies have indicated greater declines in new stroke diagnoses among those with milder symptoms [6,7]. However, none of these studies addressed social factors that may have contributed to the reduction in new stroke admissions.
While many social factors likely contributed to the decline in stroke diagnoses, there is also a biological explanation as to why fewer ischemic strokes have been reported during the first wave of the pandemic—the decline in rate of other transmissible infections. Certainly, the rate of worldwide COVID-19 diagnoses climbed exponentially between December 2019 and May 2020 (with weekly averages exceeding 100,000 new diagnoses by this time); however, the rate of other infections declined precipitously. As a surrogate for transmissible infectious illnesses, influenza has been one of the most widely prevalent and thoroughly studied infection since the COVID-19 pandemic. Rates of influenza, which are typically highest during the winter months, reached an all-time low in the United States shortly after COVID-19 was declared a national emergency on March 1, 2020 [8]. Infections are known to precipitate a systemic inflammatory response, increasing platelet and leukocyte activation [9], ultimately culminating in cardio- and cerebrovascular events. That influenza can trigger acute ischemic stroke is further supported by observational cohort studies which have demonstrated a reduction in the risk of stroke with preceding vaccination [10].
Certainly, one can argue that with increasing rates of COVID-19, the risk of stroke due to systemic inflammation from COVID-19 should also have increased. In spite of our heightened concern for COVID-19 and its many complications, influenza and other transmissible infectious conditions had historically exceeded the systemic acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) on a global scale. One meta-analysis estimated that during recent years, there have been nearly 6 million annual hospitalizations for over 32 million annual lower respiratory infections due to influenza [11]. By May of 2020 when we observed a global plateau in the decline of new strokes [2], only 4 million COVID-19 cases had been confirmed, according to Our World In Data [12]. Therefore, the sharp reductions in influenza and other transmissible infections (despite the rise in SARS-CoV-2) may have partly mediated the temporary decline in new ischemic stroke diagnoses. This decline has now reversed, and as of May 2022, the current rate of new COVID-19 diagnoses is more than 200 million per annum—more than six times the number of annual infections due to influenza.
Impact on stroke outcomes
Several studies have examined the intersections between ischemic stroke, reperfusion therapies, concomitant COVID-19, and their outcomes. While absolute rates of IVT [1] and EVT [2,13] have declined globally, we have no reason to suspect either reperfusion treatment would be less effective in patients with COVID-19. Short-term outcomes among patients treated during the COVID-19 pandemic have been reported poorer across multiple cohort studies; however, most of these did not adjust for SARS-CoV-2 status or address the differential severity of disease among those who were admitted during pandemic months. Much of the difference in poorer stroke-related outcomes may be attributed to the severity of COVID-19 itself. For example, data from Get-With-the-Guidelines-Stroke, including 41,971 patients treated across 458 United States hospitals reported a four-fold higher odds of in-hospital mortality (adjusted odds ratio [OR], 4.34; 95% confidence interval [CI], 3.48 to 5.40) and lower odds of discharge without disability (adjusted OR, 0.65; 95% CI, 0.52 to 0.81) [14]. These results have been validated in a cohort of 54 centers in the Cerner network [15], however, neither model adjusted for IVT.
Stroke reperfusion therapies in COVID-19
The safety of acute IVT and EVT in COVID-19 patients has been an area of active investigation during the pandemic. In the Get-With-the-Guidelines-Stroke database, IVT was not associated with a higher rate of symptomatic ICH among COVID-19 versus non-COVID-19 patients (adjusted OR, 0.79; 95% CI, 0.36 to 1.75) [14]. Independently, investigators querying the Vizient Clinical Data Base (representing 46 states, 166,586 stroke patients) reported ICH (9.6% vs. 6.6%, P<0.001) and subarachnoid hemorrhage (2.8% vs. 2.0%, P=0.01) rates were both nearly 50% higher among stroke patients with COVID-19 versus those without COVID-19 [16]. Thrombolytic and EVT utilization were both lower among COVID-19 patients, so while this is unlikely to have confounded the higher rate of hemorrhagic complications, there was no specific analysis among patients treated with reperfusion therapies. In a separate cohort study of 545 thrombolyzed patients (101 with COVID-19), the CASCADE initiative found no difference in hemorrhagic transformation among stroke patients with versus without COVID-19 who were treated with IVT [17].
ICH and COVID-19
In general, spontaneous ICH is an uncommon complication of COVID-19, with pooled estimates indicating an approximately 0.5% incidence among hospitalized patients [18]. The majority of COVID-19 patients with ICH were anticoagulated prior to the hemorrhage event; however, the incidence rate of ICH exceeds what is typically seen in other medical conditions. Furthermore, the mortality rate in COVID-19 patients with ICH (nearly 50%) is also reflective of the uniqueness and severity of this complication. Endothelial injury likely plays a role in tissue vulnerability and is discussed in ‘Pathophysiology of thrombosis in COVID-19’ below. As a mechanism in primary/spontaneous ICH, endothelial injury from direct viral invasion via the angiotensin converting enzyme receptor may lead to breakdown in the blood-brain barrier and ICH. The considerable systemic inflammation with massive cytokine release may also contribute to this process, and even result in the well-described para-infectious inflammatory condition acute hemorrhagic necrotizing encephalopathy [19]. Coagulopathy is also common in critical illness, and some COVID-19 patients will have a modest reduction in platelet count and/or prolonged prothrombin time [20], as well as marked elevations in tissue plasminogen activator with ex vivo evidence of enhanced clot lysis [21]. The numerous potential mechanisms in which ICH occurs among COVID-19 make it a challenging process to prevent, and to treat.
Pathophysiology of thrombosis in COVID-19
Although there was a transient, global decline in new stroke diagnoses during the first wave of the pandemic, clinicians began to take notice of the association between COVID-19 and thrombotic risk. Some of the earliest reports estimated the risk of stroke among hospitalized patients with COVID-19 between 1% and 5% [1,2,4,22], with a higher risk among more critically ill patients, patients with higher D-dimer levels and other laboratory biomarkers of inflammatory activity [23]. Conversely, the rate of COVID-19 among patients hospitalized with stroke has been reported to range from 1.5% to 3.3% [1,24]. Although the risk of cerebrovascular disease has not been specifically studied among the emerging variants, the omicron variant may have milder severity with a lower risk of hospitalization when compared to the delta [25] and other variants. This warrants further exploration as the potentially milder omicron variant takes foothold around the world.
One of the major mechanisms of COVID-19 coagulopathy pertains to platelet activation. This mechanism following viral infection, which has been termed “thromboinflammation,” is complex and beyond the scope of this review. In essence, multiple simultaneous pathways become activated following SARS-CoV-2 infection, including neutrophil activation, tissue factor expression [26], fibrin deposition, interleukin 6 release [27], matrix metalloproteinase production [28], and others [29], which facilitate thrombus formation [30]. This hematopathology has been implicated in MI, acute ischemic stroke in COVID-19, and other states of systemic inflammation. Levels of circulating soluble P-selectin (which activate platelets) are found to be elevated in patients with severe COVID-19 [31], and are thought to mediate much of the platelet-leukocyte interaction and microthrombi formation in the pulmonary capillary bed and coronary vasculature in these patients. For these reasons—and in the absence of better evidence for antithrombotic treatment in ischemic stroke—conventional antithrombotic regimens are recommended for secondary stroke prevention, with anticoagulation recommended when indicated for other purposes [32].
A second consequence of COVID-19 is endothelial dysfunction, which has been observed histopathologically across many organ systems [33]. Endothelial injury with or without inflammation has been implicated in acute cerebral infarction, ICH, and posterior reversible encephalopathy [34]. Markers of endothelial dysfunction, such as circulating levels of angiopoietin-2 [35], von Willebrand activity [36], and inflammatory cell accumulation within the endothelium [37], have been found in patients with COVID-19, and have been strongly attributed to severity of illness, ICU admission, and early mortality. Intracranial vessel wall enhancement on magnetic resonance imaging (MRI) in patients with acute stroke and multifocal microhemorrhages has been explained by endothelial inflammation in this condition [38]; however, post-mortem data has not shown consistent perivascular inflammatory infiltration.
Thirdly, COVID-19 has been associated with disruptions in the coagulation cascade. This mechanism may explain the disproportionate risk of venous thromboembolism and multifocal pulmonary emboli in patients with COVID-19 and critical illness [39]. Nearly one in five patients who are critically ill from COVID-19 may develop a venous or pulmonary thromboembolism, according to one recent meta-analysis [40]. In a targeted population of noncritically ill patients with COVID-19, many of whom had elevated D-dimer levels, investigators from the trials, Accelerating COVID-19 Therapeutic Interventions and Vaccines 4 ACUTE (ACTIV-4a), Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC), and Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP) reported therapeutic anticoagulation was associated with a significant 1.9% absolute risk reduction in thrombotic events, with a 1.0% absolute increase in major bleeding events [41]. However, the benefit of therapeutic anticoagulation in largely noncritically ill patients with elevated D-dimer was not confirmed in the AntiCoagulaTIon cOroNavirus (ACTION) randomized clinical trial [42]. Furthermore, there was no advantage of therapeutic anticoagulation from the ACTIV-4a, ATTACC, and REMAP-CAP investigation of critically ill patients with COVID-19 [43], nor was there benefit of anticoagulation in the recently completed Intermediate vs. Standard-Dose Prophylactic Anticoagulation in Critically-ill Patients with COVID-19 (INSPIRATION) randomized controlled trial [44].
Coupled with the high risk of thrombotic events in COVID-19 is the relatively high risk of systemic bleeding. In one meta-analysis, an estimated 7.8% of hospitalized patients with COVID-19 (95% CI, 2.6% to 15.3%) experience major bleeding [40]. This risk increases considerably with therapeutic anticoagulation (21.4%), but vastly exceeds what has been reported in other conditions that lead to critical illness [45]. It may be, in part, due to the high risk of major bleeding in COVID-19 that there have been no consistent benefits of therapeutic anticoagulation over routine thromboprophylaxis in hospitalized patients with COVID-19. In addition, the associated multi-organ dysfunction, prolonged use of enteral feeding tube, and requirement for mechanical ventilation among COVID-19 patients with respiratory failure likely contribute to the higher risk of bleeding in this population [46].
Altogether, the risk of venous and arterial thrombotic events are high, but this risk is matched by the equally worrisome risk of major bleeding. Clinical trial and observational cohort data suggest there may be a small benefit of therapeutic anticoagulation earlier in the course of COVID-19 when illness is milder, albeit with a significant risk of major bleeding. It is possible that heparin, due to its pleiotropic mechanisms and anti-inflammatory activity, may be the preferred agent in thromboprophylaxis and therapeutic anticoagulation. However, there remain no randomized clinical trials targeting ischemic stroke prophylaxis or secondary prevention with antithrombotics in COVID-19. Conventional antithrombotic practices, including single or combination antiplatelet strategies (unless anticoagulation is indicated) are recommended until better evidence becomes available [32].
Management paradigms
The surge in COVID-19 cases over the preceding 2 years has tremendously impacted the allocation of healthcare resources, systems of care in cerebrovascular disease [47], and a wide variety of other medical conditions.
Acute reperfusion therapies
Parallel to the decline in stroke admissions was a decline in emergent reperfusion therapy use during the first wave of the COVID-19 pandemic. One early study of 280 centers in China [5] reported a 27% absolute decline in the use of IVT could be attributed in part, to delays for COVID-19 screening (63.0%), as well as febrile patients using stroke examination resources (30.8%), and lack of available medical personnel (15.9%), which the authors attribute to the rising rate of COVID-19 diagnoses exceeding available health care providers.
While there have been declines in absolute numbers of patients treated with reperfusion therapies for acute ischemic stroke, the relative proportion of patients treated with EVT has risen. A recent meta-analysis of 46 observational cohort studies (including 129,491 patients) reported a 24% increase in the odds of EVT during pandemic months when compared to a prior control period [48]. This is likely, at least in part, explained by the higher proportion of patients having more severe strokes at presentation [7], with a 63% higher odds of having a large vessel occlusion [48]. The absolute numbers of new large vessel occlusions do not appear to have changed substantially. However, of total stroke admissions, the relative decline in new mild stroke diagnoses (or patients with milder symptoms avoiding health care institutions) has contributed to a proportional rise in severe strokes due to intracranial occlusion.
Acute stroke treatment throughput
Undertreatment of acute ischemic stroke (and delays in treatment with reperfusion therapies) have been reported elsewhere in the world. Observational data from stroke centers in the United States [14,49] and elsewhere [50,51] have reported small, but significant differences in reperfusion treatment time during the first wave of the pandemic as compared to preceding control periods. While there have been delays in stroke care, there has been a rising interest in simplifying acute stroke triage and expediting acute care [52]. The adoption of tenecteplase as the standard thrombolytic (over alteplase) has been associated with significant reductions in door-to-needle times during the COVID-19 pandemic [53]. Tenecteplase requires less nurse-patient contact and administration maintenance, which can reduce transmission of SARS-CoV-2, and as a single bolus (rather than infusion) may permit faster transfers between primary and endovascular-capable stroke centers [54].
Observational cohort studies have also evaluated the utility of advanced neuroimaging in EVT patient selection. Computed tomography (CT) perfusion and MRI with or without magnetic resonance perfusion may help identify patients likely to benefit the most from EVT, but these modalities can significantly delay endovascular treatment [55]. The BEYOND SWIFT (Bernese-European Registry for Ischemic Stroke Patients Treated Outside Current Guidelines With Neurothrombectomy Devices Using the SOLITAIRE FR With the Intention for Thrombectomy) investigators reported an average EVT delay of 30 minutes when MRI was used over CT, although use of CT in patient selection led to a blunted EVT treatment effect [56]. Importantly, patients selected by CT alone still experienced a higher rate of functional recovery when compared to untreated historic controls with large vessel occlusion [57]. The investigators also concluded in a separate study that EVT for patients with CT- or MRI-based Alberta Stroke Programme Early CT Scale (ASPECTS) scores of 0–5 remains more effective than medical management for patients treated within 6 hours of last known well [58]. In the global CT for Late EndovasculAr Reperfusion (CLEAR) study [59,60], including 1,604 patients treated exclusively in the late window, the use of CT alone was associated with a significant 17 minute reduction in arrival to skin puncture when compared to patients selected by CT perfusion, and a 22 minute reduction in time to skin puncture versus MRI-selected patients (P<0.001). Furthermore, there was no difference in the primary outcome of a favorable 90-day modified Rankin Scale (mRS) shift for patients selected by CT versus CT perfusion (adjusted OR, 0.95; 95% CI, 0.77 to 1.17; P=0.64) or CT versus MRI (adjusted OR, 0.95; 95% CI, 0.80 to 1.13; P=0.55) in multivariable regression.
Peri-procedural sedation during thrombectomy
Among patients with (or suspected of having) COVID-19, it remains unclear whether general anesthesia (GA) or conscious sedation (CS) may be a preferable means of maintaining oxygenation during EVT [61]. In a multicenter study of 458 patients undergoing EVT for large vessel occlusion stroke at the peak of the COVID-19 pandemic, more than half of the patients were intubated prior to EVT, leading to longer door to reperfusion time, higher in-hospital mortality, and lower likelihood of functional independence at discharge [62]. More interestingly, the majority of these sites were not intubating most patients for EVT pre-pandemic, but changed their practice following society recommendations [62].
A meta-analysis from four randomized clinical trials pre-pandemic [63] suggested that GA is preferred over CS, and that GA is associated with a two-fold higher odds of successful recanalization (OR, 2.14; 95% CI, 1.26 to 3.62) and 90-day mRS of 0–2 (OR, 1.71; 95% CI, 1.13 to 2.59). While the included trials were rigorously designed, they were limited to single-center experiences with favorable outcomes of GA reported exclusively among exploratory endpoints. In light of the inconsistent evidence, and particularly lack of significant differences in primary endpoints across the published clinical trials, most academic societies recommend selecting mode of anesthesia based on individual need rather than a standardized practice [47,64].
Primary and secondary prevention strategies
Prioritization of acute care in patients with COVID-19 has led to substantial losses in primary care and long-term secondary prevention of many conditions. Estimates from the United Kingdom suggest that deprioritization of primary care and delays in cancer screening will lead to a 5% to 17% increase in mortality across various solid tumor types, with a cumulative years of life lost totaling approximately 60,000 [65]. Other studies have estimated considerable increases in undiagnosed or suboptimally managed mental health conditions [66], and a number of vascular risk factors [67] including diabetes, hypertension, dyslipidemia, chronic kidney disease, and coronary artery disease. Repurposing and shut down of inpatient rehabilitation centers has contributed to reduction in the number of acute stroke patients being discharged to rehabilitation facilities [68], and more being discharged with greater disability to home [7]. The long-term consequences of these collateral effects of the pandemic may not be appreciated for years, but are likely to lead to greater morbidity and mortality among stroke survivors, and increase costs of care.
Future perspectives
As the COVID-19 pandemic continues to shape our daily practice, it is imperative that we as clinicians and researchers do not underestimate its impact. We should be proactive in ways we can adapt to this disease rather than react to it.
As precautions are recommended to reduce in-person patient-provider contact, clinicians and trialists ought to incorporate remote methods of communication and follow-up, including telemedical care when possible [69]. Telemedicine has a rich history in vascular neurology as an accessible, rapid means of emergent evaluation in patients with suspected acute stroke [70]. It also has been associated with greater use of acute reperfusion therapies, and lower early mortality in stroke [71]. Major limitations of telemedicine are that it may not be practical when imaging or laboratory testing are necessary, when internet or connectivity issues are present, and concerns remain as to reimbursement by some insurance payors [72].
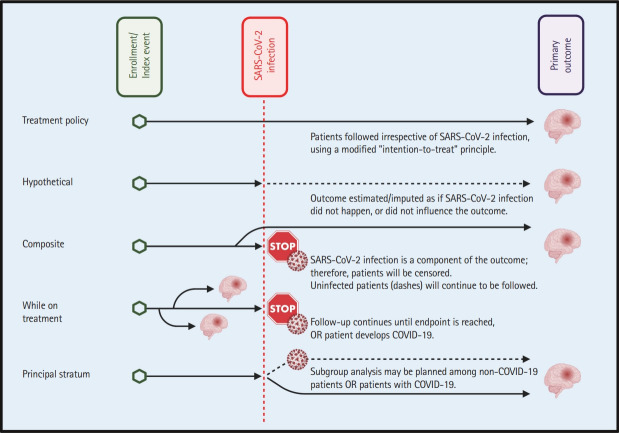
The impact of a pandemic on clinical trials cannot be understated. As summarized in this review, SARS-CoV-2 has established itself as a novel stroke mechanism, altered the global reporting of cerebrovascular events, and changed the way many patients prefer to interact with their health care providers. Furthermore, it is responsible for higher rates of vascular risk factors and protracted cognitive consequences, referred to as the “long-COVID” syndrome (or post-acute sequelae of SARS-CoV-2 [73]). In order to mitigate the collateral effects of a pandemic, some have suggested utilizing the estimands framework when conducting clinical trials and cohort studies [74]. This framework encourages prespecification of strategies to address intercurrent events that can confound randomized clinical trials (Table 1 and Figure 1). Based on the study methodology and primary/secondary outcome events, different approaches may be taken in order to address intercurrent events such as infection with SARS-CoV-2.
Table 1.
Utilization of the estimands framework to address intercurrent events (such as COVID-19 diagnosis in a trial patient)
| Strategy name | Approach | Limitations |
|---|---|---|
| Treatment policy strategy | The trial is largely conducted on the “intention-to-treat” principle. | The outcome must be acquired irrespective of IE (e.g., Mortality would be an acceptable outcome, given that it can be determined in patients with or without COVID-19. However, re-stenosis following angioplasty/stenting at 7 days may not be feasible in some critically ill COVID-19 patients who are too unstable to undergo repeat imaging). |
| Hypothetical strategy | Investigator imputes outcome data based on absence of IE for a given patient. | The outcome(s) may not accurately reflect a response or association with the exposure due to confounding by the IE (e.g., Intracranial hemorrhage risk can be estimated for a patient, assuming they did not develop COVID-19). |
| Composite strategy | The IE can be woven into one (or more) other outcomes into a composite endpoint (e.g., development of COVID-19 or hemorrhagic transformation following recanalization). | This approach is less effective when the composite outcome includes events which do not occur naturally, and when the IE is not anticipated to influence the outcome of interest (e.g., delayed extreme hypertension [systolic blood pressure >180 mm Hg] 90 days after stroke and/or COVID-19). |
| This is most useful when an IE can affect the outcome of interest, and a pre-specified outcome can be selected knowing that the IE can influence it (e.g., 90-Day functional dependence is influenced by COVID-19 status). | ||
| While on treatment strategy | The outcome variable should occur prior to the IE. This is advantageous when there are repeated measures over time (e.g., Serial NIHSS scores may be collected until the day the patient becomes symptomatic of COVID-19, at which point remaining events are censored). | This strategy is less effective when an IE may occur prior to the index or primary outcome event (e.g., Readmission within 30 days may be influenced by COVID-19 status). |
| Principal stratum strategy | This approach involves planned subgroup analysis of patients based on IE. This is particularly useful if the relationship between the exposure and outcome should exist within a particular population (e.g., pre-specification of a subgroup analysis based on patients who never develop COVID-19 during the study period). | Sample size estimates need to account for expected IE rate(s), which may require more funding or follow-up in clinical trials. |
COVID-19, coronavirus disease 2019; IE, intercurrent event; NIHSS, National Institutes of Health Stroke Scale.
Figure 1.
Application of the estimands framework in stroke research during the coronavirus disease 2019 (COVID-19) pandemic. Image generated using biorender.com. SARS-CoV-2, systemic acute respiratory syndrome-coronavirus 2.
As we continue to battle the patient-level and public health consequences of the COVID-19 pandemic, we ought to continuously reappraise our treatment paradigms. Emerging variants of SARS-CoV-2, such as the omicron variant, may be more contagious than the alpha variant; however, they have been associated with less severe systemic illness. Whether these newer variants are associated with similarly heightened thrombotic risk and the “long-COVID” syndrome may be challenging to study, but warrant exploration. Public health awareness regarding COVID-19—as well as its variants and vaccination safety/efficacy—delays in care due to contact precautions and decontamination procedures, and outpatient follow-up using in-person or remote means require constant vigilance in order to reduce the global impact of COVID-19 on stroke patients. The successful implementation of quality improvement studies which target these and other health care objectives should be shared with others to maximize the benefit in our global community.
Acknowledgments
Thanh N. Nguyen reports research support from the Society of Vascular and Interventional Neurology.
Footnotes
Disclosure
James E. Siegler reports speakers bureau (AstraZeneca) and consulting fees (Ceribell), unrelated to the present work. Thanh N. Nguyen reports research support from Medtronic.
References
- 1.Nogueira RG, Qureshi MM, Abdalkader M, Martins SO, Yamagami H, Qiu Z, et al. Global impact of COVID-19 on stroke care and IV thrombolysis. Neurology. 2021;96:e2824–e2838. doi: 10.1212/WNL.0000000000011885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nogueira RG, Abdalkader M, Qureshi MM, Frankel MR, Mansour OY, Yamagami H, et al. Global impact of COVID-19 on stroke care. Int J Stroke. 2021;16:573–584. doi: 10.1177/1747493021991652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen TN, Haussen DC, Qureshi MM, Yamagami H, Fujinaka T, Mansour OY, et al. Decline in subarachnoid haemorrhage volumes associated with the first wave of the COVID-19 pandemic. Stroke Vasc Neurol. 2021;6:542–552. doi: 10.1136/svn-2020-000695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siegler JE, Cardona P, Arenillas JF, Talavera B, Guillen AN, Chavarría-Miranda A, et al. Cerebrovascular events and outcomes in hospitalized patients with COVID-19: the SVIN COVID-19 Multinational Registry. Int J Stroke. 2021;16:437–447. doi: 10.1177/1747493020959216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of COVID-19 on stroke evaluation in the United States. N Engl J Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortega-Gutierrez S, Farooqui M, Zha A, Czap A, Sebaugh J, Desai S, et al. Decline in mild stroke presentations and intravenous thrombolysis during the COVID-19 pandemic: the Society of Vascular and Interventional Neurology Multicenter Collaboration. Clin Neurol Neurosurg. 2021;201:106436. doi: 10.1016/j.clineuro.2020.106436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, et al. Decreased influenza activity during the COVID-19 pandemic: United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Htun P, Fateh-Moghadam S, Tomandl B, Handschu R, Klinger K, Stellos K, et al. Course of platelet activation and plateletleukocyte interaction in cerebrovascular ischemia. Stroke. 2006;37:2283–2287. doi: 10.1161/01.STR.0000236638.75591.61. [DOI] [PubMed] [Google Scholar]
- 10.Lee KR, Bae JH, Hwang IC, Kim KK, Suh HS, Ko KD. Effect of influenza vaccination on risk of stroke: a systematic review and meta-analysis. Neuroepidemiology. 2017;48:103–110. doi: 10.1159/000478017. [DOI] [PubMed] [Google Scholar]
- 11.Lafond KE, Porter RM, Whaley MJ, Suizan Z, Ran Z, Aleem MA, et al. Global burden of influenza-associated lower respiratory tract infections and hospitalizations among adults: a systematic review and meta-analysis. PLoS Med. 2021;18:e1003550. doi: 10.1371/journal.pmed.1003550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Research and data to make progress against the world's largest problems. Our World in Data. https://ourworldindata.org. Accessed April 8, 2022.
- 13.Yavagal DR, Saini V, Inoa V, Gardener HE, Martins SO, Fakey M, et al. International survey of mechanical thrombectomy stroke systems of care during COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021;30:105806. doi: 10.1016/j.jstrokecerebrovasdis.2021.105806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Srivastava PK, Zhang S, Xian Y, Xu H, Rutan C, Alger HM, et al. Acute ischemic stroke in patients with COVID-19: an analysis from get with the guidelines-stroke. Stroke. 2021;52:1826–1829. doi: 10.1161/STROKEAHA.121.034301. [DOI] [PubMed] [Google Scholar]
- 15.Qureshi AI, Baskett WI, Huang W, Shyu D, Myers D, Raju M, et al. Acute ischemic stroke and COVID-19: an analysis of 27676 patients. Stroke. 2021;52:905–912. doi: 10.1161/STROKEAHA.120.031786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Havenon A, Ney JP, Callaghan B, Delic A, Hohmann S, Shippey E, et al. Impact of COVID-19 on outcomes in ischemic stroke patients in the United States. J Stroke Cerebrovasc Dis. 2021;30:105535. doi: 10.1016/j.jstrokecerebrovasdis.2020.105535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sasanejad P, Afshar Hezarkhani L, Arsang-Jang S, Tsivgoulis G, Ghoreishi A, Kristian B, et al. Safety and outcomes of intravenous thrombolytic therapy in ischemic stroke patients with COVID-19: CASCADE Initiative. J Stroke Cerebrovasc Dis. 2021;30:106121. doi: 10.1016/j.jstrokecerebrovasdis.2021.106121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leasure AC, Khan YM, Iyer R, Elkind M, Sansing LH, Falcone GJ, et al. Intracerebral hemorrhage in patients with COVID-19: an analysis from the COVID-19 Cardiovascular Disease Registry. Stroke. 2021;52:e321–e323. doi: 10.1161/STROKEAHA.121.034215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology. 2020;296:E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henry BM, Cheruiyot I, Benoit JL, Lippi G, Prohászka Z, Favaloro EJ, et al. Circulating levels of tissue plasminogen activator and plasminogen activator inhibitor-1 are independent predictors of coronavirus disease 2019 severity: a prospective, observational study. Semin Thromb Hemost. 2021;47:451–455. doi: 10.1055/s-0040-1722308. [DOI] [PubMed] [Google Scholar]
- 22.Bhatia R, Pedapati R, Komakula S, Srivastava M, Vishnubhatla S, Khurana D. Stroke in coronavirus disease 2019: a systematic review. J Stroke. 2020;22:324–335. doi: 10.5853/jos.2020.02264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramos-Araque ME, Siegler JE, Ribo M, Requena M, López C, de Lera M, et al. Stroke etiologies in patients with COVID-19: the SVIN COVID-19 multinational registry. BMC Neurol. 2021;21:43. doi: 10.1186/s12883-021-02075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strambo D, De Marchis GM, Bonati LH, Arnold M, Carrera E, Galletta S, et al. Ischemic stroke in COVID-19 patients: Mechanisms, treatment, and outcomes in a consecutive Swiss Stroke Registry analysis. Eur J Neurol. 2022;29:732–743. doi: 10.1111/ene.15199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolter N, Jassat W, Walaza S, Welch R, Moultrie H, Groome M, et al. Early assessment of the clinical severity of the SARS-CoV-2 Omicron variant in South Africa. bioRxiv. 2021 Dec 21; doi: 10.1101/2021.12.21.21268116. [Preprint]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hottz ED, Azevedo-Quintanilha IG, Palhinha L, Teixeira L, Barreto EA, Pão C, et al. Platelet activation and plateletmonocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020;136:1330–1341. doi: 10.1182/blood.2020007252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan M, Liu Y, Zhou R, Deng X, Li F, Liang K, et al. Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China. Immunology. 2020;160:261–268. doi: 10.1111/imm.13223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Syed F, Li W, Relich RF, Russell PM, Zhang S, Zimmerman MK, et al. Excessive matrix metalloproteinase-1 and hyperactivation of endothelial cells occurred in COVID-19 patients and were associated with the severity of COVID-19. J Infect Dis. 2021;224:60–69. doi: 10.1093/infdis/jiab167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Velavan TP, Meyer CG. Mild versus severe COVID-19: laboratory markers. Int J Infect Dis. 2020;95:304–307. doi: 10.1016/j.ijid.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manne BK, Denorme F, Middleton EA, Portier I, Rowley JW, Stubben C, et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020;136:1317–1329. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yatim N, Boussier J, Chocron R, Hadjadj J, Philippe A, Gendron N, et al. Platelet activation in critically ill COVID-19 patients. Ann Intensive Care. 2021;11:113. doi: 10.1186/s13613-021-00899-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ma A, Kase CS, Shoamanesh A, Abdalkader M, Pikula A, Sathya A, et al. Stroke and thromboprophylaxis in the era of COVID-19. J Stroke Cerebrovasc Dis. 2021;30:105392. doi: 10.1016/j.jstrokecerebrovasdis.2020.105392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bonaventura A, Vecchié A, Dagna L, Martinod K, Dixon DL, Van Tassell BW, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021;21:319–329. doi: 10.1038/s41577-021-00536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lallana S, Chen A, Requena M, Rubiera M, Sanchez A, Siegler JE, et al. Posterior reversible encephalopathy syndrome (PRES) associated with COVID-19. J Clin Neurosci. 2021;88:108–112. doi: 10.1016/j.jocn.2021.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smadja DM, Guerin CL, Chocron R, Yatim N, Boussier J, Gendron N, et al. Angiopoietin-2 as a marker of endothelial activation is a good predictor factor for intensive care unit admission of COVID-19 patients. Angiogenesis. 2020;23:611–620. doi: 10.1007/s10456-020-09730-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McAlpine LS, Zubair AS, Maran I, Chojecka P, Lleva P, Jasne AS, et al. Ischemic stroke, inflammation, and endotheliopathy in COVID-19 patients. Stroke. 2021;52:e233–e238. doi: 10.1161/STROKEAHA.120.031971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keller E, Brandi G, Winklhofer S, Imbach LL, Kirschenbaum D, Frontzek K, et al. Large and small cerebral vessel involvement in severe COVID-19: detailed clinical workup of a case series. Stroke. 2020;51:3719–3722. doi: 10.1161/STROKEAHA.120.031224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020;324:799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiménez D, García-Sanchez A, Rali P, Muriel A, Bikdeli B, Ruiz-Artacho P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Chest. 2021;159:1182–1196. doi: 10.1016/j.chest.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.ATTACC Investigators. ACTIV-4a Investigators. REMAP-CAP Investigators. Lawler PR, Goligher EC, Berger JS, et al. Therapeutic anticoagulation with heparin in noncritically ill patients with COVID-19. N Engl J Med. 2021;385:790–802. doi: 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lopes RD, de Barros E Silva P, Furtado R, Macedo A, Bronhara B, Damiani LP, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet. 2021;397:2253–2263. doi: 10.1016/S0140-6736(21)01203-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.REMAP-CAP Investigators. ACTIV-4a Investigators. ATTACC Investigators. Goligher EC, Bradbury CA, McVerry BJ, et al. Therapeutic anticoagulation with heparin in critically ill patients with COVID-19. N Engl J Med. 2021;385:777–789. doi: 10.1056/NEJMoa2103417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.INSPIRATION Investigators. Sadeghipour P, Talasaz AH, Rashidi F, Sharif-Kashani B, Beigmohammadi MT, et al. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. JAMA. 2021;325:1620–1630. doi: 10.1001/jama.2021.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chatterjee S, Chakraborty A, Weinberg I, Kadakia M, Wilensky RL, Sardar P, et al. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA. 2014;311:2414–2421. doi: 10.1001/jama.2014.5990. [DOI] [PubMed] [Google Scholar]
- 46.Harris SK, Bone RC, Ruth WE. Gastrointestinal hemorrhage in patients in a respiratory intensive care unit. Chest. 1977;72:301–304. doi: 10.1378/chest.72.3.301. [DOI] [PubMed] [Google Scholar]
- 47.Nguyen TN, Abdalkader M, Jovin TG, Nogueira RG, Jadhav AP, Haussen DC, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams. A guidance statement from the Society of Vascular and Interventional Neurology. Stroke. 2020;51:1896–1901. doi: 10.1161/STROKEAHA.120.030100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Katsanos AH, Palaiodimou L, Zand R, Yaghi S, Kamel H, Navi BB, et al. Changes in stroke hospital care during the COVID-19 pandemic: a systematic review and meta-analysis. Stroke. 2021;52:3651–3660. doi: 10.1161/STROKEAHA.121.034601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Siegler JE, Zha AM, Czap AL, Ortega-Gutierrez S, Farooqui M, Liebeskind DS, et al. Influence of the COVID-19 pandemic on treatment times for acute ischemic stroke: the Society of Vascular and Interventional Neurology Multicenter Collaboration. Stroke. 2021;52:40–47. doi: 10.1161/STROKEAHA.120.032789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Plumereau C, Cho TH, Buisson M, Amaz C, Cappucci M, Derex L, et al. Effect of the COVID-19 pandemic on acute stroke reperfusion therapy: data from the Lyon Stroke Center Network. J Neurol. 2021;268:2314–2319. doi: 10.1007/s00415-020-10199-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fuentes B, Alonso de Leciñana M, García-Madrona S, Díaz-Otero F, Aguirre C, Calleja P, et al. Stroke acute management and outcomes during the COVID-19 outbreak: a cohort study from the Madrid Stroke Network. Stroke. 2021;52:552–562. doi: 10.1161/STROKEAHA.120.031769. [DOI] [PubMed] [Google Scholar]
- 52.Chen Y, Nguyen TN, Wellington J, Mofatteh M, Yao W, Hu Z, et al. Shortening door-to-needle time by multidisciplinary collaboration and workflow optimization during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2022;31:106179. doi: 10.1016/j.jstrokecerebrovasdis.2021.106179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hall J, Thon JM, Heslin M, Thau L, Yeager T, Siegal T, et al. Tenecteplase improves door-to-needle time in real-world acute stroke treatment. Stroke Vasc Interv Neurol. 2021;1:e000102. [Google Scholar]
- 54.Warach SJ, Saver JL. Stroke thrombolysis with tenecteplase to reduce emergency department spread of coronavirus disease 2019 and shortages of alteplase. JAMA Neurol. 2020;77:1203–1204. doi: 10.1001/jamaneurol.2020.2396. [DOI] [PubMed] [Google Scholar]
- 55.Meinel TR, Kaesmacher J, Mosimann PJ, Seiffge D, Jung S, Mordasini P, et al. Association of initial imaging modality and futile recanalization after thrombectomy. Neurology. 2020;95:e2331–e2342. doi: 10.1212/WNL.0000000000010614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meinel TR, Kaesmacher J, Fischer U. Author response: association of initial imaging modality and futile recanalization after thrombectomy. Neurology. 2021;96:916–917. doi: 10.1212/WNL.0000000000011900. [DOI] [PubMed] [Google Scholar]
- 57.Siegler JE, Thon JM. Reader response: association of initial imaging modality and futile recanalization after thrombectomy. Neurology. 2021;96:915–916. doi: 10.1212/WNL.0000000000011898. [DOI] [PubMed] [Google Scholar]
- 58.Kaesmacher J, Chaloulos-Iakovidis P, Panos L, Mordasini P, Michel P, Hajdu SD, et al. Mechanical thrombectomy in ischemic stroke patients with Alberta Stroke Program Early Computed Tomography Score 0-5. Stroke. 2019;50:880–888. doi: 10.1161/STROKEAHA.118.023465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nguyen TN, Abdalkader M, Nagel S, Qureshi MM, Ribo M, Caparros F, et al. Noncontrast computed tomography vs computed tomography perfusion or magnetic resonance imaging selection in late presentation of stroke with largevessel occlusion. JAMA Neurol. 2022;79:22–31. doi: 10.1001/jamaneurol.2021.4082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Seker F, Qureshi MM, Möhlenbruch M, Nogueira RG, AbdalKader M, Ribo M, et al. Abstract TMP67: Predictors of unfavourable events despite successful mechanical thrombectomy in the extended window. Stroke. 2022;53(Suppl 1):ATMP67. [Google Scholar]
- 61.Nguyen TN, Nogueira RG, Jovin TG. Response by Nguyen et al to letter regarding article, “Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the society of vascular and interventional neurology”. Stroke. 2020;51:e172–e173. doi: 10.1161/STROKEAHA.120.030629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Al Kasab S, Almallouhi E, Alawieh A, Levitt MR, Jabbour P, Sweid A, et al. International experience of mechanical thrombectomy during the COVID-19 pandemic: insights from STAR and ENRG. J Neurointerv Surg. 2020;12:1039–1044. doi: 10.1136/neurintsurg-2020-016671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Campbell D, Diprose WK, Deng C, Barber PA. General anesthesia versus conscious sedation in endovascular thrombectomy for stroke: a meta-analysis of 4 randomized controlled trials. J Neurosurg Anesthesiol. 2021;33:21–27. doi: 10.1097/ANA.0000000000000646. [DOI] [PubMed] [Google Scholar]
- 64.AHA/ASA Stroke Council Leadership Temporary emergency guidance to US stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: on behalf of the American Heart Association/American Stroke Association Stroke Council Leadership. Stroke. 2020;51:1910–1912. doi: 10.1161/STROKEAHA.120.030023. [DOI] [PubMed] [Google Scholar]
- 65.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Williams R, Jenkins DA, Ashcroft DM, Brown B, Campbell S, Carr MJ, et al. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. Lancet Public Health. 2020;5:e543–e550. doi: 10.1016/S2468-2667(20)30201-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sisó-Almirall A, Kostov B, Sánchez E, Benavent-Àreu J, Paz LG. Impact of the COVID-19 pandemic on primary health care disease incidence rates: 2017 to 2020. Ann Fam Med. 2022;20:63–68. doi: 10.1370/afm.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Thau L, Siegal T, Heslin ME, Rana A, Yu S, Kamen S, et al. Decline in rehab transfers among rehab-eligible stroke patients during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021;30:105857. doi: 10.1016/j.jstrokecerebrovasdis.2021.105857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hatcher-Martin JM, Adams JL, Anderson ER, Bove R, Burrus TM, Chehrenama M, et al. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology. 2020;94:30–38. doi: 10.1212/WNL.0000000000008708. [DOI] [PubMed] [Google Scholar]
- 70.Nam HS, Park E, Heo JH. Facilitating stroke management using modern information technology. J Stroke. 2013;15:135–143. doi: 10.5853/jos.2013.15.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wilcock AD, Schwamm LH, Zubizarreta JR, Zachrison KS, Uscher-Pines L, Richard JV, et al. Reperfusion treatment and stroke outcomes in hospitals with telestroke capacity. JAMA Neurol. 2021;78:527–535. doi: 10.1001/jamaneurol.2021.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Guzik AK, Martin-Schild S, Tadi P, Chapman SN, Al Kasab S, Martini SR, et al. Telestroke across the continuum of care: lessons from the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021;30:105802. doi: 10.1016/j.jstrokecerebrovasdis.2021.105802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moghimi N, Di Napoli M, Biller J, Siegler JE, Shekhar R, McCullough LD, et al. The neurological manifestations of postacute sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021;21:44. doi: 10.1007/s11910-021-01130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yassi N, Hayward KS, Campbell B, Churilov L. Use of the estimand framework to manage the disruptive effects of COVID-19 on stroke clinical trials. Stroke. 2021;52:3739–3747. doi: 10.1161/STROKEAHA.121.036537. [DOI] [PMC free article] [PubMed] [Google Scholar]