Abstract
Background:
To evaluate the clinical and radiological outcomes of aseptic revision of total knee arthroplasty (TKA) using the Vanguard 360 Revision Knee System with the hybrid cementation technique.
Methods:
Between January 2014 and October 2016, nineteen aseptic revision TKAs were carried out with the Vanguard 360 Revision Knee System (Zimmer-Biomet, Warsaw, IN, USA) performed by two different surgeons. The patients were evaluated clinically and radiographically at one, six, and twelve months after surgery and yearly thereafter. Functional outcomes were assessed according to the range of motion (ROM), knee society knee score (KSKS) and knee society function score (KSFS). Radiological evaluations were performed using the hip-knee-ankle angle (HKA), weight-bearing anteroposterior view, latero-lateral view, Rosenberg x-rays of the knee and skyline patellar x-rays. A triple-phase technetium bone scan was performed on all the patients complaining of knee pain after one year from surgery.
Results:
Clinical and radiological results including KSKS, KSFS, ROM and HKA angle improved after revision of TKA with a statistically significant difference (p<0.05). There were seven revisions of the CCK prosthesis due to persistent pain.
Conclusion:
Patients who underwent revision of TKA using the Vanguard 360 with the hybrid cementation technique had a failure rate of 36.8% at a mean time of 29 months due to aseptic loosening. Further studies are required to analyse the role of cementation in detail to prevent this complication.
Key Words: Hybrid cementation, Knee revision, Vanguard 360
Introduction
The primary goal of revision of total knee arthroplasty (TKA) is to obtain a stable and functional prosthesis. This can be achieved by different types of implants such as posterior-stabilized (PS), constrained condylar knee (CCK), and fully constrained rotating-hinge knee (RHK) prostheses according to the bone stock and ligament stability (1,2).
In case of revision of an unicompartmental knee arthroplasty (UKA) or a TKA with valid collateral ligaments, a standard PS implant might be used. A CCK prosthesis is considered if one or both collateral ligaments are deficient. In case of deficiency in both collateral ligaments and/or an important loss of bone stock, an RHK implant is generally preferred (1,2).
According to the literature, the outcomes after revision of TKA are less encouraging than those after primary TKA with failure rates of 11% – 60% being reported in series with a relatively short follow-up (3,4). The reasons for these poor results are numerous, including poor bone stock, high infection rate, extensor mechanism failure, malalignment, and ligament instability (1-4).
In last few years, the Vanguard 360 Knee Revision System (Zimmer-Biomet, Warsaw, IN, USA) was developed for revision of TKAs. It is the second generation of the Vanguard Super Stabilized Knee (SSK, Zimmer-Biomet, Warsaw, IN, USA) with a right and left femoral component, modular stem extensions for both femoral and tibial components, more off-set options, and a new locking mechanism for the tibial polyethylene insert (5).
The purpose of this study is to evaluate the clinical and radiological outcomes of revision of TKA using the Vanguard 360 Knee Revision System. Since this is a relatively new type of implant that was introduced in the United States in May 2011, the literature on this implant is scarce with only one available report (6)
Materials and Methods
Between January 2014 and October 2016, nineteen aseptic revisions of TKAs were carried out by two different surgeons, out of which 17 of them were by Surgeon 1 and 2 of them by Surgeon 2, using the Vanguard 360 Revision Knee System.
The indications for using this prosthesis were similar to those described by Insall et al. (7): deficient medial or lateral collateral ligament with intact extensor mechanism, absent posterior cruciate ligament, and moderate bone loss. In these cases, the prosthesis should have a weight-bearing intramedullary stem to transfer stress lines to the cortical bone. General data is summarised in Table 1.
Table 1.
General data, date of first and second revision, type of implant are described
| Patient | Sex | Age | BMI | ASA grade | Side | 1 implant | 2 implant | Time between 1 and 2 revision |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 74 | 33.3 | II | Left | Vanguard 360 | LCCK | 24 months |
| 2 | F | 68 | 29.4 | II | Left | Vanguard 360 | ||
| 3 | F | 69 | 31.1 | II | Right | Vanguard 360 | LCCK | 42 months |
| 4 | F | 73 | 27.3 | II | Left | Vanguard 360 | LCCK | 16 months |
| 5 | F | 58 | 24.3 | II | Left | Vanguard 360 | LCCK | 34 months |
| 6 | M | 69 | 28.7 | II | Left | Vanguard 360 | ||
| 7 | F | 71 | 31.2 | II | Right | Vanguard 360 | ||
| 8 | F | 73 | 35.5 | II | Left | Vanguard 360 | ||
| 9 | F | 74 | 31.2 | II | Right | Vanguard 360 | ||
| 10 | F | 76 | 26.5 | II | Left | Vanguard 360 | ||
| 11 | F | 66 | 29.7 | II | Right | Vanguard 360 | ||
| 12 | M | 79 | 33 | II | Right | Vanguard 360 | ||
| 13 | F | 68 | 37.2 | III | Right | Vanguard 360 | LCCK | 15 months |
| 14 | F | 76 | 31.8 | II | Left | Vanguard 360 | ||
| 15 | F | 76 | 38.5 | III | Right | Vanguard 360 | LCCK | 43 months |
| 16 | F | 67 | 32.8 | II | Left | Vanguard 360 | ||
| 17 | M | 65 | 37.1 | II | Left | Vanguard 360 | ||
| 18 | M | 66 | 30.1 | II | Left | Vanguard 360 | ||
| 19 | F | 61 | 28.3 | II | Right | Vanguard 360 | LCCK | 32 months |
In case of suspected infection, in addition to routine blood tests, including white blood cells, ESR, and C-reactive protein, a joint fluid sampling and scintigraphy with labeled leukocytes were performed. In no case were there any signs of infection.
The patients were evaluated clinically and with x-rays at one, six and twelve months after surgery and yearly thereafter. The functional outcomes were assessed according to the range of motion (ROM), knee society knee score (KSKS), and knee society function score (KSFS) (8). The clinical results were rated as excellent (80–100 points), good (70–79 points), fair (60–69 points), or poor (less than 60 points).
Knee ROM was assessed using a standard longarm goniometer to measure flexion and extension. Measurements were performed as reported by Hancock et al. (9).
Radiological evaluations were performed using the hip-knee-ankle angle (HKA), weight-bearing anteroposterior view, latero-lateral view, Rosenberg x-rays of the knee and skyline patellar x-rays. An independent observer, who was not involved in the study, assessed the radiographs for the alignment of the limb, position of the components, and presence and location of all radiolucent lines (RLL) at the cement-bone interface according to the knee society guidelines (10). A triple-phase technetium bone scan was performed on all the patients complaining of knee pain one year after the surgery. All the patients signed informed consent forms to be included in the study.
Surgical technique
Prophylactic antibiotic with two grams of cephazolin was administered 30 minutes before skin incision. All the cases were performed without a tourniquet. All surgical procedures were performed with patients in supine position under the influence of spinal anesthesia. A longitudinal skin incision was performed on the previous scar. A medial parapatellar arthrotomy was performed and where it was necessary the approach was lengthened both proximally and distally to have a full vision of the joint; after scar tissue excision and prosthesis were removed, bone defects were evaluated to choose the appropriate augments if necessary. All the implants were fixed using the hybrid technique: cement fixation of the femoral or tibial metaphysis and the femoral or tibial cut surface, but press-fit fixation of the femoral or tibial component stem; a femoral and tibial modular stem was used in all the cases with appropriate augments to fill bony defects, and obtain restoration of the joint line and, consequently, good stability. Cemented splined stems, which were double-flanged stems in 14 femurs and six tibias (the design varied according to the stem diameter) as opposed to grit blast or smooth stems were used in all cases. Routine closure was performed over a close-suction drain, which was removed 24 hours postoperatively. 750mg of tranexamic acid, peri-articular as previously published, was administered intravenously in all the patients (except those with contraindications) before skin incision, after 3 hours, and intraoperatively (11).
Rehabilitation protocol
Rehabilitation using a continuous passive motion machine and physical therapy was performed six hours after surgery. Able patients started to walk six hours after surgery with partial weight-bearing (30%) using two crutches for the first 30 days, followed by progressive weight-bearing. In other cases, they started from the day after surgery. Rivaroxaban was administered at a dose of 10 mg per day for 35 days after surgery for thromboembolism prophylaxis (12).
Statistical analysis
All the data was checked for normality with the use of the Shapiro-Wilk W test. Comparisons between the preoperative and postoperative data were done with paired T-test for normal distribution and Wilcoxon test for skewed data. A value of p < 0.05 was considered to be significant. Kaplan-Meier curves were used in the analysis of rate of survival of the prostheses.
Results
The average follow-up time for the Vanguard 360 implant was 33.6 months. The clinical and radiological outcomes of Vanguard 360 implant, including KSKS, KSFS, ROM, and HKA angle, improved after revision of TKA with a statistically significant difference (p<0.05). The average KSKS improved from 41 to 76 when the range improved from 31–53 to 52–83 and the average KSFS improved from 39 to 65 when the range improved from 30–48 to 53–72, at the last follow-up. Four patients had an excellent result (80–100), seven patients had a good result (70–79), five had a fair result (60–69), and two had a poor result (less than 60). The average range of motion improved from 87 (range 76–93) to 98 (range 92–110). The overall limb alignment improved from an average of 2.3° varus to 1° varus when the range improved from 9° varus–7° valgus to 8° varus–3.5° valgus, at the last follow-up. The radiolucency was relatively common: eight knees (or 42 %) had at least 1 mm radiolucency around the femoral (7) (4 for zone 4; 3 for zone 1) and tibial (4) (2 for zone 3; 1 for zone 1; 1 for zone 2) stem [Figure 1]. Four of these femoral stems were double-flanged; regarding the tibia, 2 were double flanged. No RLLs were located at the patellar component.
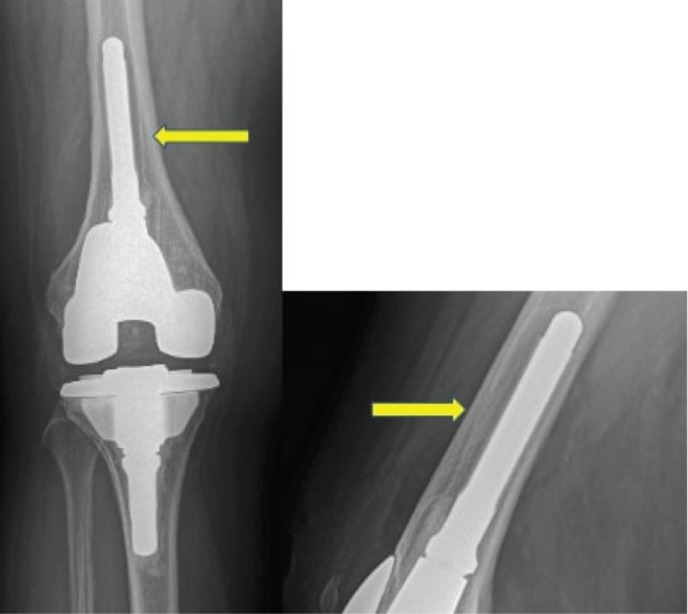
Figure 1.
Antero-posterior and latero-lateral x-ray views of Vanguard 360 Knee Revision System. The arrows indicate radiolucent lines around the femoral stem
Seven revisions of the CCK prosthesis were conducted due to persistent pain (6 by Surgeon 1 and 1 by Surgeon 2). All the revisions were performed using the legacy constrained condylar knee (LCCK) (Zimmer-Biomet, Warsaw, IN, USA). The average time for the second revision was 29 months (range of 15–43 months). All the revised patients were female with an average age of 71.4 years (range of 61–80) and an average BMI of 31.4 (range of 24.3–38.5). Two of these patients (in cases 1 and 19) were operated in another hospital and one of them received a patellar replacement before our revision, but without a symptom relief. Case 5 underwent a revision of the femoral component with another Vanguard 360 modular component before the final revision with LCCK. All these patients underwent a triple-phase technetium bone scan which showed bone hyperactivity of femoral component in four of them and tibial component in two of them while one patient reported hyperactivity of both tibial and femoral components. In all the cases, RLLs were visible. In all the seven cases, the blood tests, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), were within normal range and the intraoperatively taken tissue samples were negative for cultures.
After the second revision with LCCK, the clinical results and ROM of the seven patients improved significantly (p < 0.05): KSKS improved from 37 to 74 when the range improved from 33–45 to 68–80, KSFS improved from 35 to 68 when the range improved from 33–42 to 62–71, and ROM improved from 81° to 95°when the range improved from 70°–84° to 90°–103°. At the radiological evaluation, the HKA had an average of 1.5° varus with a range of 3° varus–1.5° valgus. No radiolucency was observed around the femoral and tibial components at the last follow-up. Prosthesis removal was considered as the implant endpoint for any reason. The implant survival rate of the Vanguard 360 system at short-term follow-up, which is an average of 36 months, was 63%.
No complications regarding the use of Rivaroxaban were reported in our cohort.
Discussion
The most important finding of this study was that the patients who underwent aseptic revision of TKA using the Vanguard 360 revision system had a revision rate of 36.8% at an average rate of 29 months. The functional evaluation using KSKS and KSFS showed a statistically significant improvement concerning preoperative analysis; the RLLs were similar to those reported in other studies, but the failure rate was higher than in other reports (13-16).
The reported clinical outcomes of revision of TKA performed with CCK are conflicting. The range of failure rates is 11–60% according to recent literature (13-16). The poor results have been attributed to several factors such as reduced bone stock, extensor mechanism problems, ligament instability or soft tissue incompetence, progressive RLLs, and higher rates of infection. On the other hand, Insall and Dethmers (17) reported good and excellent results in 89% of their 72 revisions of TKAs, whereas Goldberg et al. (18) reported only 46% of good or excellent results in their 59 revisions of TKAs. Some authors (13-16,19) found high rates of extensor mechanism problems: for example, Stuart et al. (19) reported these problems as the cause for reoperation in 41% of the 60 cases of revisions of TKAs.
We found only one paper that dealt with the functional results of Vanguard 360 Knee Revision System: Morris et al. (2013) (6) where the results of 101 consecutive revisions of TKAs reporting a survival rate of 96% at the short-term follow-up (1 year) were presented. They did not specifically mention the fixation technique; 1 aseptic loosening and 3 infections were reported as the causes for implant failures. Four RLLs were described in the femoral and tibial components. Regarding the Vanguard SSK revision system, we found three papers in the English literature: in 2009, Peters et al. (20) reported outcomes of 184 revisions of TKAs using Maxim and Vanguard SSK systems (Zimmer-Biomet, Warsaw, IN, USA) where all the cases were performed with cement fixation of the metaphysis and press-fit cementless fixation of the fluted titanium stem. They reported 15 failures due to aseptic loosening in 2 cases and infection in 13 cases. In 2016, Lackey et al. (21) reported the outcomes of 297 primary cases and revisions of TKAs using the Vanguard SSK system; they did not mention the fixation technique. In this case, the survival rate at 4.8 years was 92.6%. In 2017, Crawford et al. (22) presented the results of 278 revisions of TKAs performed with the Vanguard SSK. They used the hybrid fixation technique in most of the cases, for 91% of femoral components and 93% of tibial components. They had 13 revisions for aseptic loosening, out of which, only 1 femoral stem was fully cemented whereas all the other femoral and tibial stems were press-fit with only cement in the metaphysis.
One of the most studied CCK revision systems is the LCCK (Zimmer-Biomet). Some authors (23-28) reported good results: Kim et al. (24) reported that in 114 cases of revisions of TKAs, KSKS improved from 35 to 90 points and KSFS improved from 16 to 64 points; Lee et al. (25) reported that in 79 cases of revisions of TKAs, KSKS improved from 48.3 to 88.8 and KSFS improved from 36.9 to 73.4. Ye et al. (26) reported 92% of good or excellent results with a follow-up of 5.5 years in a group of primary cases and revisions of TKAs using CCK. The survival rate ranged between 88.5% and 100% [Table 2].
Table 2.
Literature review of recent series on CCK-type implants
| Author | Cases | Follow-up (years) | KSKS (mean) | KSFS (mean) | Survival rate | Causes of failure (implant removal) | Type of prosthesis | HKA (mean, °) | Radiolucent lines > 1 mm |
|---|---|---|---|---|---|---|---|---|---|
| Nakano et al. (23) | 41 | 4.1 | 82.9 | 79.2 | 97.5% | 1 infection | LCCK | 174.9 | Not reported |
| Kim YH et al. (21) | 114 | 7.2 | 90 | 64 | 96% | 3 aseptic loosening and 2 infections | LCCK | 174.5 | 4% |
| Lee JK et al. (22) | 79 | 5.3 | 88.8 | 73.4 | 93% | 4 infections and 1 aseptic loosening | LCCK | 174 | 41% |
| Hwang SC et al. (20) | 15 | 2.4 | 81 | 85 | 100% | None | LCCK | 176.9 | 18% |
| Cholewinski et al. (33) | 43 | 11 | 90 | 61 | 88.5 % | 2 infections and 1 instability | LCCK | 179.5 | 50% |
| Kwon KT et al. (34) | 18 | 6.7 | 84.8 | 63.6 | 94.5% | 1 infection | LCCK | 5 valgus | 27.8% |
| Ye CY et al. (24) | 47 | 5.5 | 80 | 85 | 95% | 2 infections | LCCK | Not reported | 4% |
| Morris MJ et al. (12) | 101 | 1 | 78 | 48.4 | 96% | 1 aseptic loosening, 3 infections | Vanguard 360 | Not reported | 4% |
| Peters CL et al. (17) | 184 | 4 | 85 | 82 | 92% | 2 aseptic loosening and 13 infections | Maxim and Vanguard SSK | Not reported | 7% |
| Lackey WG et al. (18) | 297 | 4.8 | 77.4 | 66.3 | 92.6% | 12 infections, 3 aseptic loosening, 7 other causes | Vanguard SSK | Not reported | Not reported |
| Crawford DA et al. (19) | 278 | 6 | 78.6 | 54.5 | 84% | 25 aseptic loosening, 10 infections | Vanguard SSK | Not reported | 3.9% |
| Current study | 19 | 2.7 | 76 | 65 | 63.1% | 7 aseptic loosening | Vanguard 360 | 179 | 42% |
The RLLs on the radiographs represent one of the main features in knee arthroplasty failure and can be the first sign of initial implant loosening and failure. Several studies have reported that RLLs occur more often after revision than after primary TKA. Rosenberg et al. (10) found 60% of RLLs in a series of 36 patients; Kim et al. (24) presented a series of 114 knees where 31% of RLLs around the tibial component and 18% around the femoral component were identified. In other studies, the occurrence of RLLs was reported to range from 36% to 72% after revision of TKA with the use of various implants (27-29).
Implant fixation techniques can be classified into three types according to cement application over the prosthesis: full cementation technique, hybrid technique (cement fixation of the femoral or tibial metaphysis, and the femoral or tibial cut surface but press-fit fixation of the femoral or tibial component stem), and surface cementation technique. Full cementation has the advantage of immediate and secure fixation with a disadvantage of difficulty to remove the cement in case of revision. According to Cawley et al. (30), the full cementation technique reduces bone stress over the baseplate and decreases the possibility of aseptic loosening of tibial component. Mumme et al. (31) suggested full cementation for large bone defects or osteoporosis. Whaley et al. (32) reported excellent results and a high survival rate with the full cementation technique in revision of TKAs with CCK. On the other hand, Greene et al. (33) and Sah et al. (34) achieved good results while using hybrid cementation techniques in revision of TKAs using CCK, which is very useful in case of implant re-revision. Cemented stems increase the area of cement fixation to the host bone, but their removal can be very difficult. All the implants in this study were fixed with the hybrid cementation technique (35-37) since avoiding cement in the femoral or tibial canal makes re-revision easier to perform. Controversy still exists regarding the fixation method and whether the entire portion of the stem should be cemented or not.
If we consider prosthesis removal as implant failure, our results are poorer compared to the CCK literature. Table 2 shows the survival rates of LCCK—the most used and studied CCK prosthesis. In most cases, the causes for implant failure were infections in which case the long-term follow-up survival rate ranges from 85% to 100%. In this study, we included only patients that reported failure due to aseptic loosening. During surgery, no cases of implant instability were recorded. If it is assumed that one of the possible cause of failure was the hybrid cementation technique then we advocate the full cementation technique for this kind of prosthesis.
There are some limitations to this study. Firstly, a retrospective and non-comparative design was used. Secondly, the study included a small cohort of patients which might be insufficient for assessing clinical and radiological results. However, due to the relatively rare indication and high failure rate in this small cohort, we believe that the series contains important data on this relatively new implant system.
Patients who underwent revision of TKA using the Vanguard 360 with the hybrid cementation technique had a failure rate of 36.8% at a mean time of 29 months due to aseptic loosening. Further studies are required to analyse the role of cementation in detail to prevent this complication. We advocate other studies to compare our results and to find a relationship among cementation technique, stem type and dimension, and bone quality in the case of osteoporosis.
References
- 1.Ghasemi SA, Rashidi S, Rasouli MR, Parvizi J. Staged Bilateral Total Knee Arthroplasty: When Should the Second Knee be Replaced? Arch Bone Jt Surg. 2021;9(6):633–640. doi: 10.22038/abjs.2021.49007.2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lei PF, Hu RY, Hu YH. Bone Defects in Revision Total Knee Arthroplasty and Management. Orthop Surg. 2019;11(1):15–24. doi: 10.1111/os.12425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tarazi JM, Chen Z, Scuderi GR, Mont MA. The Epidemiology of Revision Total Knee Arthroplasty. J Knee Surg. 2021;34(13):1396–1401. doi: 10.1055/s-0041-1735282. [DOI] [PubMed] [Google Scholar]
- 4.Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD. Annual revision rates of partial versus total knee arthroplasty: A comparative meta-analysis. Knee. 2017;24(2):179–190. doi: 10.1016/j.knee.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Kolich MT, Adams JB, Morris MJ, Hurst JM, Berend KR, Lombardi AV Jr, Crawford DA. Mid-Term Clinical Outcomes and Survivorship of a Second-Generation Modular Revision Knee System. Surg Technol Int. 2021;38:460–466. [PubMed] [Google Scholar]
- 6.Morris MJ, Berend KR, Adams JB, Lombardi Jr. Early Results of a Modular Revision System in Total Knee Arthroplasty. JISRF Reconstructive Review. 2013;3(3):27. doi: 10.1016/j.arth.2017.03.076. [DOI] [PubMed] [Google Scholar]
- 7.Insall JN. Revision of total knee replacement. Instr Course Lect. 1986;35:290–296. [PubMed] [Google Scholar]
- 8.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;(248):13–14. [PubMed] [Google Scholar]
- 9.Hancock GE, Hepworth T, Wembridge K. Accuracy and reliability of knee goniometry methods. J Exp Orthop. 2018;5(1):46. doi: 10.1186/s40634-018-0161-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR. Development of a Modern Knee Society Radiographic Evaluation System and Methodology for Total Knee Arthroplasty. J Arthroplasty. 2015 Dec;30(12):2311–2314. doi: 10.1016/j.arth.2015.05.049. [DOI] [PubMed] [Google Scholar]
- 11.Pinsornsak P, Rojanavijitkul S, Chumchuen S. Peri-articular tranexamic acid injection in total knee arthroplasty: a randomized controlled trial. BMC Musculoskelet Disord. 2016;17:313. doi: 10.1186/s12891-016-1176-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manista GC, Batko BD, Sexton AC, Edmiston TA, Courtney PM, Hannon CP, et al. Anticoagulation in Revision Total Joint Arthroplasty: A Retrospective Review of 1917 Cases. Orthopedics. 2019;42(6):323–329. doi: 10.3928/01477447-20190906-02. [DOI] [PubMed] [Google Scholar]
- 13.Hermans K, Vandenneucker H, Truijen J, Oosterbosch J, Bellemans J. Hinged versus CCK revision arthroplasty for the stiff total knee. Knee. 2019;26(1):222–227. doi: 10.1016/j.knee.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Tsai SW, Chen CF, Wu PK, Chen CM, Chen WM. Revision Total Knee Arthroplasty Using a Constrained Condylar Knee Prosthesis Combined with a Posterior Stabilized Articular Surface. J Knee Surg. 2018;31(2):197–201. doi: 10.1055/s-0037-1603337. [DOI] [PubMed] [Google Scholar]
- 15.Barnoud W, Schmidt A, Swan J, Sappey-Marinier E, Batailler C, Servien E, Lustig S. Condylar constrained knee prosthesis and rotating hinge prosthesis for revision total knee arthroplasty for mechanical failure have not the same indications and same results. SICOT J. 2021;7:45. doi: 10.1051/sicotj/2021046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Badawy M, Fenstad AM, Furnes O. Primary constrained and hinged total knee arthroplasty: 2- and 5-year revision risk compared with unconstrained total knee arthroplasty: a report on 401 cases from the Norwegian Arthroplasty Register 1994-2017. Acta Orthop. 2019;90(5):467–472. doi: 10.1080/17453674.2019.1627638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Insall JN, Dethmers DA. Revision of total knee arthroplasty. Clin Orthop Relat Res. 1982;(170):123–130. [PubMed] [Google Scholar]
- 18.Goldberg VM, Figgie MP, Figgie HE 3rd, Sobel M. The results of revision total knee arthroplasty. Clin Orthop Relat Res. 1988;(226):86–92. [PubMed] [Google Scholar]
- 19.Stuart MJ, Larson JE, Morrey BF. Reoperation after condylar revision total knee arthroplasty. Clin Orthop Relat Res. 1993;(286):168–173. [PubMed] [Google Scholar]
- 20.Peters CL, Erickson JA, Gililland JM. Clinical and radiographic results of 184 consecutive revision total knee arthroplasties placed with modular cementless stems. J Arthroplasty. 2009;24(6 Suppl):48–53. doi: 10.1016/j.arth.2009.04.033. [DOI] [PubMed] [Google Scholar]
- 21.Lackey WG, Ritter MA, Berend ME, Malinzak RA, Faris PM, Meding JB. Midterm Results of the Vanguard SSK Revision Total Knee Arthroplasty System. Orthopedics. 2016;39(5):e833–7. doi: 10.3928/01477447-20160509-02. [DOI] [PubMed] [Google Scholar]
- 22.Crawford DA, Berend KR, Morris MJ, Adams JB, Lombardi AV Jr. Results of a Modular Revision System in Total Knee Arthroplasty. J Arthroplasty. 2017;32(9):2792–2798. doi: 10.1016/j.arth.2017.03.076. [DOI] [PubMed] [Google Scholar]
- 23.Hwang SC, Kong JY, Nam DC, Kim DH, Park HB, Jeong ST, et al. Revision total knee arthroplasty with a cemented posterior stabilized, condylar constrained or fully constrained prosthesis: a minimum 2-year follow-up analysis. Clin Orthop Surg. 2010;2(2):112–120. doi: 10.4055/cios.2010.2.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim YH, Park JW, Kim JS, Oh HK. Long-Term Clinical Outcomes and Survivorship of Revision Total Knee Arthroplasty with Use of a Constrained Condylar Knee Prosthesis. J Arthroplasty. 2015;30(10):1804–1809. doi: 10.1016/j.arth.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 25.Lee JK, Kim SJ, Choi CH, Chung HK. Revision total knee arthroplasty using a constrained condylar knee prosthesis in conjunction with a posterior stabilized articular polyethylene. J Arthroplasty. 2013;28(4):566–569. doi: 10.1016/j.arth.2012.07.017. [DOI] [PubMed] [Google Scholar]
- 26.Ye CY, Xue DT, Jiang S, He RX. Results of a Second-generation Constrained Condylar Prosthesis in Complex Primary and Revision Total Knee Arthroplasty: A Mean 5 5-Year Follow-up. Chin Med J (Engl). 2016;129(11):1334–1339. doi: 10.4103/0366-6999.182845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mow CS, Wiedel JD. Revision total knee arthroplasty using the porous-coated anatomic revision prosthesis: six-to twelve-year results. The Journal of arthroplasty. 1998;13(6):681–686. doi: 10.1016/s0883-5403(98)80013-2. [DOI] [PubMed] [Google Scholar]
- 28.Nakano N, Matsumoto T, Muratsu H, Ishida K, Kuroda R, Kurosaka M. Revision total knee arthroplasty using the modern constrained condylar knee prosthesis. Acta ortopedica brasileira. 2016;24:304–308. doi: 10.1590/1413-785220162406146213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takahashi Y, Gustilo RB. Nonconstrained implants in revision total knee arthroplasty. Clin Orthop Relat Res. 1994;(309):156–162. [PubMed] [Google Scholar]
- 30.Cawley DT, Kelly N, Simpkin A, Shannon FJ, McGarry JP. Full and surface tibial cementation in total knee arthroplasty: a biomechanical investigation of stress distribution and remodeling in the tibia. Clin Biomech (Bristol, Avon). 2012;27(4):390–397. doi: 10.1016/j.clinbiomech.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 31.Mumme T, Marx R, Qunaibi M, Niethard FU, Wirtz DC. Oberflächenkonditionierung für eine verbesserte Uberlebenswahrscheinlichkeit von Knieprothesen: Komplett- vs Oberflächenzementiertechnik der Tibiakomponente [Surface pretreatment for prolonged survival of cemented tibial prosthesis components: full- vs surface-cementation technique] Biomed Tech (Berl). 2006;51(2):95–102. doi: 10.1515/BMT.2006.017. [DOI] [PubMed] [Google Scholar]
- 32.Whaley AL, Trousdale RT, Rand JA, Hanssen AD. Cemented long-stem revision total knee arthroplasty. J Arthroplasty. 2003;18(5):592–599. doi: 10.1016/s0883-5403(03)00200-6. [DOI] [PubMed] [Google Scholar]
- 33.Greene JW, Reynolds SM, Stimac JD, Malkani AL, Massini MA. Midterm results of hybrid cement technique in revision total knee arthroplasty. J Arthroplasty. 2013;28(4):570–574. doi: 10.1016/j.arth.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 34.Sah AP, Shukla S, Della Valle CJ, Rosenberg AG, Paprosky WG. Modified hybrid stem fixation in revision TKA is durable at 2 to 10 years. Clin Orthop Relat Res. 2011;469(3):839–846. doi: 10.1007/s11999-010-1569-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gofton WT, Tsigaras H, Butler RA, Patterson JJ, Barrack RL, Rorabeck CH. Revision total knee arthroplasty: fixation with modular stems. Clin Orthop Relat Res. 2002;(404):158–168. [PubMed] [Google Scholar]
- 36.Cholewinski P, Putman S, Vasseur L, Migaud H, Duhamel A, Behal H, et al. Long-term outcomes of primary constrained condylar knee arthroplasty. Orthop Traumatol Surg Res. 2015;101(4):449–54. doi: 10.1016/j.otsr.2015.01.020. [DOI] [PubMed] [Google Scholar]
- 37.Kwon KT, Han KY, Lee WS, Kim DH. Full Cementation in Revision Total Knee Arthroplasty Using a Constrained Condylar Knee Prosthesis with an Average 7-Year Follow-up. Knee Surg Relat Res. 2017;29(4):282–287. doi: 10.5792/ksrr.17.101. [DOI] [PMC free article] [PubMed] [Google Scholar]