Abstract
The experience of patients who choose observation or surgery for kidney stones has not been well established. We compared these patients using qualitative interviews, the Wisconsin Quality of Life questionnaire (WISQOL), and the Cambridge Renal Stone Patient Reported Outcome Measure (CReSP). Adult patients with upper tract urinary calculi for whom observation or intervention were options underwent qualitative interviews at baseline and at 2 months. WISQOL and CReSP were administered at baseline, and at 6–16 weeks post operatively if surgery was selected. Comparisons in patient experiences and quality of life measures were performed between groups. Among 15 patients who opted for surgery and 10 patients who opted for observation, we identified major themes in patient experiences related to context, health care episodes, patient responses, and perceived outcomes. A conceptual framework for the domains of patient experience during kidney stone disease was developed, which can be used by clinicians and patients to shape discussion. Baseline standardized WISQOL and CReSP scores were comparable between groups. In the surgery group, both WISQOL and CReSP scores improved after surgery (WISQOL 58 to 83, higher is better, p = 0.003; CReSP 31 to 23, lower is better, p = 0.009). Patients who underwent surgery for kidney stones reported improvements in quality of life after treatment via WISQOL and CReSP. A conceptual framework was developed for the patient experience of kidney stones which provides a common language for patients and clinicians.
Keywords: Nephrolithiasis, Urolithiasis, Quality of life, Patient reported outcome measures, Qualitative research
Introduction
Patients with kidney stones often must choose between surgical intervention or observation [1, 2]. Decision-making between these options traditionally relies on disease-specific considerations including likelihood of stone-free status and the potential for complications [3–5].
Patient experiences and patient reported outcome measures have been increasingly recognized as important factors in treatment decisions [6–8]. Emerging data show the utility of validated quantitative instruments in demonstrating changes in health-reported quality of life (QoL) before and after treatment [9–12]. Many previous studies rely on general QoL instruments that are not specific to kidney stones, such as the Short Form 36 questionnaire (SF-36) [13]. Furthermore, there is a paucity of data within the context of decision-making for surgical intervention versus observation. Patient experiences and QoL may be different between these two treatment options, especially in cases where traditional outcome metrics do not show a clear advantage for one course of action. Previous investigators have developed QoL instruments for patients with kidney stones, such as the Wisconsin Quality of Life score (WISQOL) and the Cambridge Renal Stone Patient Reported Outcome Metric (CReSP) [14, 15]. Qualitative interviewing of patients living with kidney stone disease provides an assessment of the patient experience at a single time point, [14] and an opportunity for in depth examination of the patient perspective in their own words.
We build on previous work by comparing the QoL of patients who choose between intervention or observation for upper tract urinary calculi. Specifically, we developed a conceptual framework for the experience of kidney stone disease and identified themes among patients using temporally separated qualitative interviews. Furthermore, we compared self-reported QoL for patients undergoing surgery or observation for upper tract urinary calculi using previously validated measures. These findings aim to provide a better understanding of the patient experience in kidney stone management to help guide decision making for clinicians and patients.
Methods
Patient population
With Institutional Review Board approval, patients who were offered observation or surgical intervention for upper tract urinary calculi were recruited between December 2019 and March 2020. Recruitment was from a convenience sample of patients meeting the following criteria: (1) diagnosis of upper urinary tract stones; (2) new patient status to the clinic; (3) adult > 18 years of age; (4) decision-making discussion occurring for surgical intervention and observation. Exclusion criteria were non-English speaking status as the interviews and qualitative coding were conducted in English. Informed consent was obtained. Patient demographics were collected. Total stone surface area was calculated as the sum of the axial surface areas [16].
Patient interviews
All participants completed semi-structured interviews at baseline and at 6–16 weeks after the initial interview. For patients undergoing surgical intervention, each assessment occurred before and after intervention. Interviews were conducted by telephone by a trained interviewer, namely author KB who holds an MA in Psychology and over 10 years of qualitative research experience. This was further overseen by author DGS, PhD who is the director of Vanderbilt Qualitative Research Core. Open-ended scripted questions were asked using an interview guide that included questions related to (1) experiences with kidney stones; (2) decision to have surgery or to observe their stone(s); (3) concerns about future kidney stone experiences; (4) symptom management; (5) prevention methods; (6) barriers to maintaining positive change; and (7) symptom improvement. These kidney-stone specific questions were developed by collaboration between the co-authors and the Vanderbilt Qualitative research core, based on previous qualitative research experience, with an aim to stimulate open-ended discussion [17]. After setting the stage by inquiring about time of first kidney stone diagnosis, initial open-ended questions designed to elicit broad responses were posed. These included “What was it like when you found out you had kidney stones?” and “How did you choose between getting that surgery versus observing the stones?” Follow-up questions were asked to encourage discussion. All interviews were audio recorded and transcribed verbatim.
Measures of quality of life
All participants completed assessment of QoL, health literacy and decisional conflict at baseline. QoL was evaluated with WISQOL [18] and CRESP [14]. A decisional conflict screen was assessed using the SURE decisional conflict form [19]. Which is a four item screening tool to assess patient conviction in a given medical decision. Participants also completed the Brief Health Literacy Screen (BHLS) [20]. These data were managed using REDCap (Research Electronic Data Capture) [21]. For patients who underwent surgery, the QoL instruments were completed a second time at 6–16 weeks during the post-operative visit. For those who underwent observation, we were unable to complete follow up QoL instruments in that timeframe due to logistical barriers associated with a lack of follow up appointment in the required timeframe.
Data analysis
Descriptive statistics were provided for all participants. Participants who selected observation were compared to those who selected surgical management. QoL, health literacy and decisional conflict were compared using a two-tailed t-test for comparison with p < 0.05 considered significant. Among those who underwent surgical management, differences in baseline and follow up scores were explored with paired, two-tailed t-tests.
Important themes were identified from qualitative interviews to gain insight into patient perspectives and reasons for electing observation or surgical management. A hierarchical coding system was developed and refined using the interview guide and a preliminary review of the transcripts. Definitions and rules were created and applied to categories within which themes were organized, using the conceptual framework developed in (Fig. 1) during coding. Using an iterative inductive/deductive methodology [22, 23] key themes were identified and organized to summarize the response data from interviews. Experienced coders each reviewed four transcripts. Coding of each transcript was compared, and discrepancies resolved by discussion. After reaching consensus, remaining transcripts were divided and coded independently. Each statement was treated as a separate quote and assigned up to eight different codes. The coded transcripts were combined and sorted by code. Coded transcripts were managed using Microsoft Excel 2016 templates and processed and sorted using SPSS version 26.0.
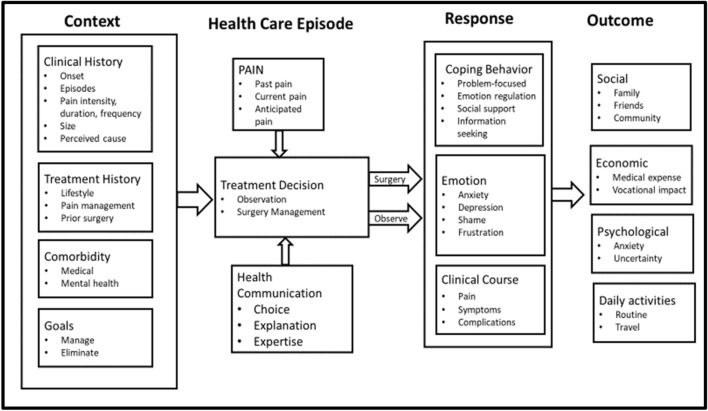
Fig. 1.
Impact of kidney stones on quality of life: a conceptual framework. Each bullet point represents a theme extracted from qualitative patient interviews about their kidney stone experience. Themes are organized into a framework of four columns which represent the decision process and its outcomes
Finally, we explored differences in themes for patient groups who were at risk of lower functioning or lower resilience. These patient groups were evaluated as we suspected they would have a higher chance of expressing negative emotions or confusion in their qualitative interview themes. We identified these patients by those with the lowest scores on the WISQOL emotional domain, and low to intermediate health literacy scores using the BHLS. We compared themes from their qualitative interviews to high functioning patients in these domains. Contrasts were made between themes with high and low expression in each group.
Results
Thirty patients were enrolled, and 25 participants completed at least one interview. Five patients who did not complete any interviews were excluded from subsequent analyses. Twenty-two participants completed both interviews, including 13 from the surgery group and 9 from the observation group. Three participants completed only the first interview (2 surgery, 1 observation). Of those three, the two surgery patients had their surgery delayed due to COVID-19.
Demographics for participants in each group can be found in (Table 1). The mean age was 54 years, with a range of 23 to 72 years. Almost half (44%) are female and the majority (92%) were non-Hispanic White. Overall, 40% of patients opted for observation and 60% opted for intervention. The median stone surface area was 40 mm2 for the observational group, and 107 mm2 for the interventional group (p = 0.13). There were significantly more women in the observational group compared to the surgery group (70 vs 27%, p = 0.049). A stone was present in the ureter in 12% of cases and hydronephrosis was present in 28% of the overall cohort. Neither presence of hydronephrosis nor baseline presence of symptoms were detected as different between groups. The mean health literacy score was identical in both surgery and observation groups at baseline (13, range 8–15).
Table 1.
Baseline demographic characteristics of participants who elected observation or surgery for kidney stones
| Characteristic | Observation | Surgery | p-value |
|---|---|---|---|
| Participants (n) | 10 | 15 | N/A |
| Age (mean years, range) | 52 (28–68) | 56 (23–72) | 0.5 |
| Sex | |||
| Male | 3 (30%) | 11 (73%) | |
| Female | 7 (70%) | 4 (27%) | 0.049* |
| Race | |||
| White non-Hispanic | 10 (100%) | 13 (87%) | |
| Asian, American Indian/Alaska Native | 0 (0%) | 1 (7%) | |
| Black or African American | 0 (0%) | 1 (7%) | 1 |
| BMI (kg/m2, median and range) | 32 (26–39) | 31 (19–53) | 0.78 |
| History of stones | |||
| Yes | 7 (70%) | 9 (60%) | |
| No | 3 (30%) | 6 (40%) | 0.69 |
| Family history of stones | |||
| Yes | 2 (20%) | 3 (20%) | |
| No | 8 (80%) | 12 (80%) | 1 |
| Previous stone surgery(ies) | |||
| None | 6 | 9 | N/A |
| SWL | 2 | 4 | |
| URS | 4 | 5 | |
| PCNL | 1 | 0 | |
| Stone laterality | |||
| Right | 2 (22%) | 4 (27%) | |
| Left | 1 (11%) | 4 (27%) | |
| Bilateral | 6 (67%) | 7 (47%) | 0.74 |
| Stone location | |||
| Upper pole | 3 | 6 | |
| Middle pole | 8 | 5 | |
| Lower Pole | 6 | 10 | |
| Renal pelvis | 1 | 5 | |
| Ureter | 2 | 1 | N/A |
| Median total stone surface area (mm2, range) | 40 (24–57) | 107 (52–176) | 0.13 |
| Hydronephrosis at enrollment | |||
| Present | 2 (20%) | 5 (33%) | |
| Absent | 8 (80%) | 10 (67%) | 0.66 |
| Symptoms present | |||
| Yes | 7 (78%) | 11 (79%) | |
| No | 2 (22%) | 3 (21%) | 1 |
| Initial treatment plan decision | |||
| Observation | 10 (100%) | 0 (0%) | |
| SWL | 0 (0%) | 1 (7%) | |
| URS | 0 (0%) | 10 (67%) | |
| PCNL | 0 (0%) | 4 (27%) | N/A |
SWL shockwave lithotripsy, URS ureteroscopy, PCNL percutaneous nephrolithotomy
* Statistically significant (p < 0.05)
Patient interview data
Major themes identified from patient interviews included (1) kidney stone medical history; (2) communication with provider; (3) QoL impacts; (4) emotion and cognition; (5) coping and acceptance; (6) treatment experience/decision; (7) management/prevention of symptoms; (8) COVID-19 perception and experience; (9) suggestions for an improved experience; (10) future medical expectations; and (11) changes in perception/experiences. All themes saturated.
The conceptual framework in (Fig. 1) organizes the major themes into four categories: context, health care episode, response, and outcome. This conceptual framework was developed to integrate themes into a holistic understanding of the patient experience. Stone-free status was not a major theme voiced by patients. Rather, the outcome-related themes focused on day-to-day functioning and impact on life. Representative patient quotes from selected patient themes can be found in (Table 2).
Table 2.
Selected patient experiences among identified themes from qualitative interviews
| Themes | Quote | |
|---|---|---|
| Context | ||
| Clinical History | “Oh, I've had kidney stones for six years.” (Surgery) | |
| ““The very first time I had one was in 1994. I think January, a long time ago. And I'd never had any other problems after that” (Surgery) | ||
| Treatment History | “They told me to give up certain types of tea, and tomato-based products.” (Surgery) | |
| “I did have surgery. They called it the basket surgery at that time.” (Surgery) | ||
| Comorbidity | “When I was diagnosed with prostate cancer two years ago, and it was so bad it would have killed me had they not given me the procedures that they did […] I just didn't realize that this kidney stone could be like this” (Surgery) | |
| “You get kidney stones. They also found cysts on my kidneys and they also found something on my thyroid. Is this the beginning of the end?” (Surgery) | ||
| Goals | “I think there will always be a little bit of anxiety that more stones may form, because I know I'm at significant increased risk of future stones forming now that I've had one”(Surgery) | |
| “I hope to just get all the kidney stones out of there and with the condition going away that it won't come back” (Surgery) | ||
| Health care episode | ||
| Observation | “Right now we've decided to just watch that one. It's not causing any problems, and I don't really think it's going to cause any problems” (Observation) | |
| Surgery | “I was told it hurts worse when you pass them through, you know what I mean? You really hurt when it's coming through, I mean. So, I mean, am I scared about having it done? Yes, ma'am, I'm terrified” (Surgery) | |
| Health Communication | “We wrote down pros and cons and I think I talked to maybe 12 people about this situation and it all boiled down to let's just wait, because he sounds like he knows what he's talking about. Why don't we just lean on his decision?” (Observation) | |
| “if you're sitting there and someone tells you, ‘If we do procedure A, we may have to do it again and it can be somewhat painful in having to pass these stones, blah, blah, blah’. And then they say, ‘But if we do procedure B, we can most likely get it out, you'll be done with it.’ I mean, what would you do, right?” (Surgery) | ||
| Pain | “I couldn't get off of the bed it was hurting that bad, to go get in the car” (Surgery) | |
| “Well, I, if any time when you have a new pain, you're trying to figure out what the cause of it is and it made me you fearful what's going to happen next?” (Surgery) | ||
| Response | ||
| Coping behaviour | “You get a loop in your head it just goes round and round about something and it's like, Oh my God, this thing is 11 mm. That's pretty big. What are they going to do to get it?” (Surgery) | |
| “What have I done? Am I doing something? Eating wrong or drinking something wrong or something to cause this” (Surgery) | ||
| Emotion | “I would be really happy one day and the next day I'd be really down and just depending on how much sleep I'd actually get because of them being there” (Surgery) | |
| Clinical course | “On the days when it hurts really bad or Tylenol. On the days that it hurts just kind of sort of, it's there, I try not to take anything”(Surgery) | |
| “I think I'm getting an infection again, and if they could have went ahead and done it, I don't think that would have been a problem” (Surgery) | ||
| Outcome | ||
| Social | “But then when it started interfering in my life people started to notice things. Up to that point you can really just hide it”(Surgery) | |
| Economic | “Well I had finally scheduled an appointment with a urologist and I went and they recommended having the lithotripsy which I was scheduled to do over a year ago. But couldn't make it work out with the insurance and the money” (Surgery) | |
| Psychological | “it was constant anxiety, and that has played a huge part into the remainder of the anxiety in my system to this day. And why very shortly after that, I think it was maybe a year, year and a half after that, I actually went to the doctor and was put on anxiety medication.” (Surgery) | |
| “I don't really know what to expect, so that's kind of got me a little scared”(Surgery) | ||
| Daily activities | “I had to be the only one in the class that had to just stay sitting […] it felt like I was an outlier for that” (Surgery) | |
| “I've got a lot of trips planned and things going on. And so a little frustrating just sitting and waiting, hoping that everything will work out” (Surgery) | ||
Observation = patient selected observation; Surgery = patient selected surgery
Quality of life instruments
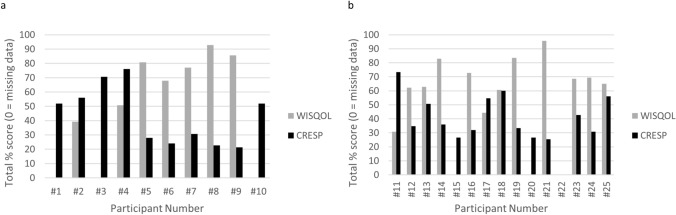
The total WISQOL scores in the observation group had a mean of 63 compared to 58 for the intervention group (Table 3). Baseline QoL scores for surgery and observational groups were not statistically different (Table 3, Fig. 2). The total WISQOL scores improved significantly after surgery (mean 58 to 83, p = 0.003; higher is better, mean change 36 with standard deviation 33). Multiple domains within WISQOL all also improved, including social functioning, emotional functioning, stone-related impact, and overall vitality. The CReSP total score improved significantly after surgery (31 to 23, p = 0.009; lower is better, mean change − 7.4 with standard deviation 7.5). The most notable improvements occurred in pain (mean improvement 3.9), work related activities (mean improvement 1.5) and anxiety domains (mean improvement 1.5). There was one participant in each group at baseline who had decisional conflict according to the SURE score [19]. One participant in the observational group changed from having decisional conflict to not having decisional conflict at the follow-up questionnaire. This participant expressed satisfaction at the follow-up interview: “Well, really everything's went good. I mean, I hurt some at times, but there's no big changes.”
Table 3.
Responses to standardized surveys for observational group, and for interventional group before and after surgery
| Questionnaire | Observational group | Interventional group before surgery | p-value (observational vs interventional) | Interventional group after surgery | p-value (before vs after surgery) |
|---|---|---|---|---|---|
| N = 10 | N = 15 | ||||
| WISQOL (mean, range) | |||||
| Total score | 63 (24–91) | 58 (13–95) | 0.66 | 83 (39–100) | 0.003* |
| Social functioning | 61 (19–100) | 73 (19–100) | 86 (31–100) | ||
| Emotional functioning | 44 (11–82) | 55 (4–86) | 82 (36–100) | ||
| Stone impact | 49 (3–88) | 52 (9–100) | 78 (38–100) | ||
| Vitality | 64 (58–92) | 60 (8–100) | 76 (8–100) | ||
| CRESP (mean, range) | |||||
| Total score | 33 (16–57) | 31 (19–55) | 0.84 | 23 (13–35) | 0.009* |
| Pain score | 10 (3–19) | 10 (6–19) | 5 (3–12) | ||
| Urinary score | 2 (1–4) | 2 (1–3) | 1 (1–2) | ||
| GIT score | 2 (1–4) | 2 (1–4) | 1 (1–3) | ||
| Work/activities score | 8 (3–12) | 7 (4–12) | 5 (3–12) | ||
| Anxiety score | 8 (4–17) | 7 (4–12) | 5 (4–12) | ||
| Diet score | 3 (2–7) | 3 (2–7) | 4 (2–7) | ||
| Decisional conflict | |||||
| Yes | 1 (10%) | 1 (7%) | 1 | 0 (0%) | NS |
| No | 9 (90%) | 14 (93%) | 11 (100%) | ||
| BHLS score | 13 (11–15) | 13 (11–15) | 0.84 | 13 (8–15) | NS |
WISQOL Wisconsin Stone Quality of Life Questionnaire, CRESP Cambridge Renal Stone Patient Reported Outcome Measure, GIT gastrointestinal tract, BHLS brief health literacy screen
* Statistically significant (p < 0.05)
Fig. 2.
Baseline WISQOL (grey) and CRESP (black) scores for each individual participant. a Participants #1–10 represent observational group b #11–25 represent surgical group. Participants with no bars have missing data. Scores were standardized as a percentage of total possible score for ease for ease of visual comparison
Qualitative-quantitative assessment
Thematic expression and QoL instruments were assessed. Groups were selected who were suspected to be at risk of lower functioning or lower resilience as these were suspected to have an impact on health-related decisions and delivery. First, patients with low to intermediate BHLS scores (average score 11 or lower [24], n = 4) were compared to patients with high BHLS scores (average score 15, n = 8). The lower BHLS group spoke about other medical history, about their pain, about prescription medications, and about other strategies to assess their problems. The higher BHLS group spoke about embarrassment, competing priorities, and COVID19.
A comparison was then performed between patients with higher and lower scores on the emotional domain of the WISQOL instrument (highest 4 scores, mean 87 vs lowest 4 scores, mean 16). Patients with low emotional domain WISQOL scores spoke about the future and about negative changes associated with stone disease. They also spoke about comorbid conditions, non-kidney procedures, other causes of kidney stones, family history, uncertainty and about observation. The patients with high emotional domain WISQOL scores spoke about past symptoms, religion, pain, surgery, and dietary modifications.
Discussion
This study improves understanding of the patient experience for surgical treatment or observation for upper tract calculi. The voice of the patient was directly applied through qualitative interviews to develop a new framework to inform shared decision processes of care for treatment options in kidney stone disease.
Our results illustrate the richness of patient responses within the framework of decision-making (Fig. 1). This framework may help clinicians and researchers understand the context from which patients enter their encounter, their major concerns during their healthcare encounter, their responses, and the outcomes of most individual importance. The themes identified in the conceptual framework may be important for treatment outcomes, willingness to adopt dietary and medication interventions, and adherence to these preventative therapies. Providers can use this framework to guide discussion and address otherwise unspoken issues that affect patient decision-making. As each clinician has different focuses and practice patterns, we invite a review of the themes in (Fig. 1) and clinician self-evaluation of their typical encounter questions. This may identify “blind spots” in domains that are systematically omitted from discussion, and encourage a positive evolution in patient interaction and counselling. This self-evaluation is especially important given evidence that stone treatment recommendations vary systematically among urologists based on practice patterns including rural vs urban location and year of training [25]. Furthermore, this framework could be distributed to patients to empower understanding and naming of their own healthcare experiences. For example, patients with severe past kidney stone pain are more likely to choose ureteroscopy over shockwave lithotripsy or observation [26]. This framework can be used to build clinical support tools and educational resources for patients and clinicians. The framework also helps to expand the definition of success into all the relevant patient-expressed outcomes in addition to surgical stone-free rates. Of interest is that regret as a specific entity did not emerge as a saturated theme in our framework. Rather, themes in which regret could be expressed, such as “coping behavior” and “emotions” were saturated.
Using QoL instruments specific for kidney stone patients (WISQOL and CReSP), we found an improvement in scores for patients who selected surgery over observation. Baseline scores were similar to the patients who chose observation. Previous studies have in general found improvements in QoL for patients after treatment compared to before treatment for kidney stones [10–12]. However, most of these studies used general QoL instruments such as the SF-36 rather than stone-specific instruments. Changes in QoL varied with different patient populations and treatments. For lower pole or calyceal calculi undergoing PCNL, QoL improved in fewer than half of the patients, with statistical significance reached in only 2 of the 7 domains of SF-36 [11]. In another study, patients who underwent retrograde ureteroscopy or ESWL both had statistically significant improvements in all four domains of WISQOL [12]. It is notable that in our study, only one patient (7%) selected SWL despite stone-free status not being a major theme voiced by patients. This is below the 36.7% utilization of SWL for stone intervention in the United States [27], and may indicate either a lack of interest in this modality in this patient group, an influence of the provider on the choice by the patient, or a combination of both. We did not detect a difference in stone surface area between the observation and intervention groups in this study (40 vs 107 mm2, p = 0.13). However, this may be because of a lack of power from the small sample size. The absolute difference between groups suggests that this could be a contributing factor to the QoL improvement seen in the surgery group.
This study builds on the literature by evaluating QoL changes in kidney stone patients who underwent surgery, but who also had the option of observation. Patient experience after choosing treatment for prostate cancer, such as treatment regret [28, 29], is well established and impacts health related QoL. The effects of treatment choice on patients for kidney stones is not well understood. In our study, patients who selected surgery for kidney stone disease had significant improvements in health-related QoL according to both WISQOL and CReSP. There was also moderate concordance between these instruments at baseline. This shows that in general, patients who make the decision for intervention benefit from a QoL perspective. Of note, symptoms or presence of hydronephrosis did not appear to have an impact on decision making, as there was no difference in these between surgery and observation groups.
We identified two groups thought to require special focus and analyzed themes extracted from interviews. The first group was patients with lower baseline emotional domain WISQOL scores. Lower emotional function using other QoL instruments has been linked to lower resilience to health challenges [30]. Patients with lower emotional domain scores spoke about uncertainty, about negative changes associated with stone disease, and about observation for their kidney stones. This finding reinforces that patients may have preconceived opinions influenced by their outlook. Knowing that patients with low emotional functioning may prefer observation may help providers understand and tailor decision making discussions to suit patient needs.
The second group of patients whose themes were analyzed were those with lower BHLS scores, who represent a vulnerable patient population with challenges in engaging with healthcare. Lower health literacy has been linked to reduced preference by patients for involvement in decision making [31] and increased decisional conflict with respect to elective surgery [32]. We hypothesized that patients with lower BHLS scores may have unique challenges in kidney stone treatment decision making. In this study, low to intermediate BHLS patients specifically spoke about pain and prescription medications. Clinicians may wish to include extra counseling on the multi-modal pain regimens that will be used for these patients. The importance of this is suggested by previous work from our group showing that kidney stone patients with lower health literacy scores were more likely to develop new chronic opioid use after ureteroscopy [33]. Overall, addressing the needs, spoke or unspoken, of patients as described by our framework may further help personalize the decision-making process.
This study has several limitations. This study is at a single center, with English speaking patients and a small cohort size which may limit generalizability. We were not logistically able to collect follow up QoL instruments for the observational group, which may have provided comparative insight into changes in their QoL. We did not detect a difference in baseline QoL instruments between surgery and observation groups, however, there could differences between these groups not detected by these instruments. Our findings may not apply to other kidney stone patient populations, as it is expected that patient perceptions and expectations vary across region, culture, and health care system. Differences in stone surface area and symptoms at baseline were not statistically significant in this small sample size. However, this may be due to a lack of power. In addition, there were significantly more women in the observational group compared to the interventional group, so sex-based differences could have been detected in interviews or QoL instruments, which are known to have an impact on health-related QoL. Further engagement with the diverse population of kidney stone formers is required to uncover their unique experiences.
Conclusions
In this single center, mixed-methods, prospective observational study, qualitative interviews yielded an experiential framework which can consulted by clinicians and patients alike as a common language to understand and discuss the patient experience of kidney stone disease. Patients had improved QoL scores after selecting surgery according to WISQOL and CReSP questionnaires.
Acknowledgements
The project described was supported by a grant from the Vanderbilt Center for Effective Health Communication. It was also supported by CTSA award No. UL1TR000445 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Abbreviations
- CReSP
Cambridge Renal Stone Patient Reported Outcome Measure
- BHLS
Brief Health Literacy Screen
- REDCap
Research Electronic Data Capture
- SF-36
Short Form 36 questionnaire
- WISQOL
Wisconsin Quality of Life questionnaire
- QoL
Quality of life
Author contributions
All authors certify that they had substantial contributions to the manuscript, including conception/data acquisition/analysis; drafting/critical revision of the work; final approval of the work; agreement of accountability of the work.
Declarations
Conflict of interest
The authors have no relevant conflicts of interest to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Connor M. Forbes, Email: connor.forbes@vumc.org
Kemberlee Bonnet, Email: kemberlee.bonnet@vanderbilt.edu.
Tracy Bryant, Email: tracy.bryant@vumc.org.
David G. Schlundt, Email: david.schlundt@vanderbilt.edu
Kerri L. Cavanaugh, Email: kerri.cavanaugh@vumc.org
Ryan S. Hsi, Email: ryan.hsi@vumc.org
References
- 1.Zumstein V, Betschart P, Abt D, Schmid HP, Panje CM, Putora PM. Surgical management of urolithiasis - a systematic analysis of available guidelines. BMC Urol. 2018;18(1):25. doi: 10.1186/s12894-018-0332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, et al. Surgical management of stones: American urological association/endourological society guideline PART I. J Urol. 2016;196(4):1153–1160. doi: 10.1016/j.juro.2016.05.090. [DOI] [PubMed] [Google Scholar]
- 3.Jin L, Yang B, Zhou Z, Li N. Comparative efficacy on flexible ureteroscopy lithotripsy and miniaturized percutaneous nephrolithotomy for the treatment of medium-sized lower-pole renal calculi. J Endourol. 2019;33(11):914–919. doi: 10.1089/end.2019.0504. [DOI] [PubMed] [Google Scholar]
- 4.Sener NC, Bas O, Sener E, Zengin K, Ozturk U, Altunkol A, et al. Asymptomatic lower pole small renal stones: shock wave lithotripsy, flexible ureteroscopy, or observation? A prospective randomized trial. Urology. 2015;85(1):33–37. doi: 10.1016/j.urology.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 5.Keeley FX, Jr, Tilling K, Elves A, Menezes P, Wills M, Rao N, et al. Preliminary results of a randomized controlled trial of prophylactic shock wave lithotripsy for small asymptomatic renal calyceal stones. BJU Int. 2001;87(1):1–8. doi: 10.1046/j.1464-410x.2001.00781.x. [DOI] [PubMed] [Google Scholar]
- 6.Mehmi A, Jones P, Somani BK. Current status and role of patient-reported outcome measures (PROMs) in endourology. Urology. 2020 doi: 10.1016/j.urology.2020.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Raja A, Wood F, Joshi HB. The impact of urinary stone disease and their treatment on patients' quality of life: a qualitative study. Urolithiasis. 2020;48(3):227–234. doi: 10.1007/s00240-019-01142-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Serna J, Talwar R, Ziemba JB. Health-related quality of life in renal stone formers: are we improving? Curr Opin Urol. 2020;30(2):190–195. doi: 10.1097/mou.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 9.Sahin C, Cetinel AC, Eryildirim B, Tuncer M, Faydaci G, Sarica K. Stone size and quality of life: a critical evaluation after extracorporeal shock wave lithotripsy. Archivio italiano di urologia, andrologia: organo ufficiale [di] Societa italiana di ecografia urologica e nefrologica. 2015;87(3):227–232. doi: 10.4081/aiua.2015.3.227. [DOI] [PubMed] [Google Scholar]
- 10.Pérez-Fentes DA, Gude F, Blanco B, Freire CG. Percutaneous nephrolithotomy: short- and long-term effects on health-related quality of life. J Endourol. 2015;29(1):13–17. doi: 10.1089/end.2014.0081. [DOI] [PubMed] [Google Scholar]
- 11.Staios D, Andrews HO, Shaik T, Buchholz NN. Quality of life after percutaneous nephrolithotomy for caliceal diverticulum and secluded lower-pole renal stones. J Endourol. 2007;21(5):515–519. doi: 10.1089/end.2006.0432. [DOI] [PubMed] [Google Scholar]
- 12.Jan S, Igor S, Viera S, Vladimir S, Jan L. Is health-related quality of life of patients after single-use flexible ureteroscopy superior to extracorporeal shock wave lithotripsy? A randomised prospective study. Urolithiasis. 2020 doi: 10.1007/s00240-020-01224-4. [DOI] [PubMed] [Google Scholar]
- 13.Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ (Clinical research ed) 1993;306(6890):1437–1440. doi: 10.1136/bmj.306.6890.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ragab M, Baldin N, Collie J, Tran MGB, Al-Hayek S, P KS, et al. Qualitative exploration of the renal stone patients' experience and development of the renal stone-specific patient-reported outcome measure. BJU Int. 2020;125(1):123–132. doi: 10.1111/bju.14873. [DOI] [PubMed] [Google Scholar]
- 15.Penniston KL, Antonelli JA, Viprakasit DP, Averch TD, Sivalingam S, Sur RL, et al. Validation and reliability of the Wisconsin Stone Quality of Life Questionnaire. J Urol. 2017;197(5):1280–1288. doi: 10.1016/j.juro.2016.11.097. [DOI] [PubMed] [Google Scholar]
- 16.Ito H, Kawahara T, Terao H, Ogawa T, Yao M, Kubota Y, et al. Evaluation of preoperative measurement of stone surface area as a predictor of stone-free status after combined ureteroscopy with holmium laser lithotripsy: a single-center experience. J Endourol. 2013;27(6):715–721. doi: 10.1089/end.2012.0548. [DOI] [PubMed] [Google Scholar]
- 17.McKernan LC, Bonnet KR, Finn MTM, Williams DA, Bruehl S, Reynolds WS, et al. Qualitative analysis of treatment needs in interstitial cystitis/bladder pain syndrome: implications for intervention. Can J Pain. 2020;4(1):181–198. doi: 10.1080/24740527.2020.1785854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Penniston KL, Nakada SY. Development of an instrument to assess the health related quality of life of kidney stone formers. J Urol. 2013;189(3):921–930. doi: 10.1016/j.juro.2012.08.247. [DOI] [PubMed] [Google Scholar]
- 19.Légaré F, Kearing S, Clay K, Gagnon S, D'Amours D, Rousseau M, et al. Are you SURE? Assessing patient decisional conflict with a 4-item screening test. Canadian family physician Medecin de famille canadien. 2010;56(8):e308–e314. [PMC free article] [PubMed] [Google Scholar]
- 20.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azungah T. Qualitative research: deductive and inductive approaches to data analysis. Qual Res J. 2018;18(4):383. doi: 10.1108/QRJ-D-18-00035. [DOI] [Google Scholar]
- 23.Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80–92. doi: 10.1177/160940690600500107. [DOI] [Google Scholar]
- 24.Wright JP, Edwards GC, Goggins K, Tiwari V, Maiga A, Moses K, et al. Association of health literacy with postoperative outcomes in patients undergoing major abdominal surgery. JAMA Surg. 2018;153(2):137–142. doi: 10.1001/jamasurg.2017.3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skenazy J, Ercole B, Lee C, Best S, Fallon E, Monga M. Nephrolithiasis: "scope," shock or scalpel? J Endourol. 2005;19(1):45–49. doi: 10.1089/end.2005.19.45. [DOI] [PubMed] [Google Scholar]
- 26.Omar M, Tarplin S, Brown R, Sivalingam S, Monga M. Shared decision making: why do patients choose ureteroscopy? Urolithiasis. 2016;44(2):167–172. doi: 10.1007/s00240-015-0806-0. [DOI] [PubMed] [Google Scholar]
- 27.Metzler IS, Holt S, Harper JD. Surgical trends in nephrolithiasis: increasing de novo renal access by urologists for percutaneous nephrolithotomy. J Endourol. 2021;35(6):769–774. doi: 10.1089/end.2020.0888. [DOI] [PubMed] [Google Scholar]
- 28.Hurwitz LM, Cullen J, Kim DJ, Elsamanoudi S, Hudak J, Colston M, et al. Longitudinal regret after treatment for low- and intermediate-risk prostate cancer. Cancer. 2017;123(21):4252–4258. doi: 10.1002/cncr.30841. [DOI] [PubMed] [Google Scholar]
- 29.van Stam MA, Aaronson NK, Bosch J, Kieffer JM, der Voort V, van Zyp JRN, Tillier CN, et al. Patient-reported outcomes following treatment of localised prostate cancer and their association with regret about treatment choices. Eur Urol Oncol. 2020;3(1):21–31. doi: 10.1016/j.euo.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz CE, Michael W, Rapkin BD. Resilience to health challenges is related to different ways of thinking: mediators of physical and emotional quality of life in a heterogeneous rare-disease cohort. Qual Life Res: an Int J of Qual of Life Asp of Treat, Care and Rehabilit. 2017;26(11):3075–3088. doi: 10.1007/s11136-017-1633-2. [DOI] [PubMed] [Google Scholar]
- 31.Seo J, Goodman MS, Politi M, Blanchard M, Kaphingst KA. Effect of health literacy on decision-making preferences among medically underserved patients. Med Decis Making: an Int J of the Soc for Med Decis Mak. 2016;36(4):550–556. doi: 10.1177/0272989x16632197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Oliveira GS, Jr Errea M, Bialek J, Kendall MC, Mccarthy RJ. The impact of health literacy on shared decision making before elective surgery: a propensity matched case control analysis. BMC Health Serv Res. 2018;18(1):958. doi: 10.1186/s12913-018-3755-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nimmagadda N, Kang C, Miller N, Herrell D, Hsi R. Impact of health literacy on ureteroscopy outcomes among kidney stone patients. J Urol. 2020;203(4S):e1052–e1053. [Google Scholar]