Abstract
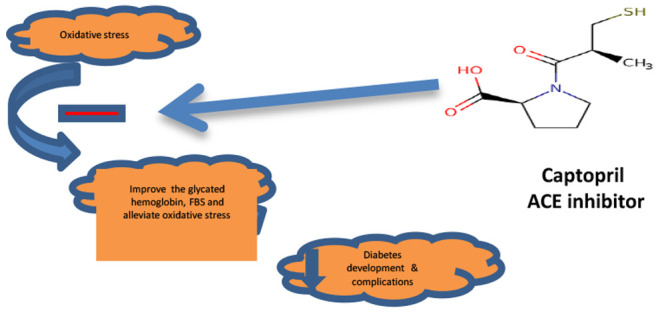
Diabetes mellitus (DM) is believed to promote oxidative stress, which potentially provokes and accelerates complications in conditions such as atherosclerotic cardiovascular, peripheral arterial, and cerebrovascular diseases. In this study, we evaluated the antioxidant therapeutic value of adding an angiotensin-converting enzyme (ACE) inhibitor—a low dose of captopril—as adjunct therapy to the treatment regimen of Type 2 diabetes mellitus (T2DM). Participants were distributed among two different groups: control and treated. T2DM patients in the treated group (group 2) were given a supplement of the ACE inhibitor capotopril, 12.5 mg/day, in addition to standard treatment. All subjects were interviewed for clinical examination. All patients in group 2 were re-examined monthly for 3 months to evaluate FBS, HbA1c, MDA, total GSH, reduced GSH, GSSG, and ox-LDL. All parameters were repeated for patients in group 2 after 1 and 3 months. The study showed improvements in the glycemic and oxidative stress status with the addition of a low dose of captopril—not very prominent but statistically significant. Reduced GSH decreased by 73.6% (P = 0.016) and the TBARS level was decreased by 58.3% (P = 0.018) after 3 months of treatment, while ox-LDL was decreased by 26.4% (P = 0.036) at the end of treatment. In summary, the clinical improvements in the disease indices toward normal levels make the use of low doses of ACE inhibitors as adjunct therapy in T2DM worth pursuing. Thus, investigations directed at preventing or protecting against oxidative damage may open a new window for treatment of diabetes mellitus.
Keywords: diabetes, antioxidant, captopril, atherosclerotic cardiovascular disease, inflammation
Diabetes mellitus (DM) is a metabolic disorder distinguished by chronic hyperglycemia with disturbance of carbohydrate, fat, and protein metabolism resulting from defects in insulin secretion, insulin action, or both.1 Patients with diabetes have increased incidence of atherosclerotic cardiovascular, peripheral arterial, and cerebrovascular diseases.2 The mechanisms by which diabetes accelerates atherosclerosis are not well understood. The risk factors for coronary artery disease (CAD), which is more common in patients with diabetes, are not enough to elucidate this phenomenon.3 Along with the development of hyperglycemia, oxidative stress has been suggested as a potential mechanism for accelerated atherosclerosis.4 The uncontrolled increase in glucose level could stimulate inflammation as well as oxidative stress.5 Oxidative stress and inflammation play major roles in both micro- and macrovascular injury.6 It is suggested that the mitigation of inflammation could lead to alleviation of oxidative stress and decreased cellular damage.5
Oxidative stress is essential in the pathogenesis of cardiovascular disease, stimulating vascular inflammation and promoting inflammatory responses and cytokines.6 Oxidative stress, inflammation, and thrombosis are cofactors that participate in the progression of atherosclerosis.7 Diabetes can upregulate inflammatory markers such as white blood cells, granulocytes, and monocytes, which promote the production of reactive oxygen species (ROS) and eventually result in vascular dysfunction.8
Oxidative damage can result from increased free radical production, insufficient antioxidant potential, or both.9 Free radical production in mammalian cells can be either accidental or deliberate.10 Under normal circumstances, the major source of free radicals in cells is electron leakage from electron transport chains, such as those in mitochondria and in the endoplasmic reticulum.11 The primary biochemical source of ROS in the vasculature appears to be the membrane-associated nicotinamide dinucleotide (phosphate) oxidase enzyme complex (NADH/NAD(P)H).12 Another source of vascular superoxide is the xanthine oxidoreductase enzyme system that catalyzes the oxidation of hypoxanthine to xanthine during purine metabolism.13
The cell injury produced by lipid peroxidation of cell membranes can range from increased permeability to cell lysis and death.9 The generation of ROS in normal cells is under tight homeostatic control to help detoxify ROS.11 Biological antioxidants, including glutathione, α-tocopherol, carotenoids, and ascorbic acid, react with the most oxidant effects. In addition, the oxidant enzymes catalase and glutathione peroxidase detoxify H2O2 by converting it to O2 and H2O.14 However, when ROS levels exceed the antioxidant capacity of a cell, a deleterious condition known as oxidative stress occurs.15 Unchecked, excessive ROS can lead to the destruction of cellular components, including lipids, proteins, and DNA, and ultimately cell death via apoptosis or necrosis.16,17
Glutathione (GSH), the most prevalent cellular thiol, acts as a reducing agent and serves as a reservoir for cystine.18 A dynamic balance is maintained between GSH synthesis, its recycling from oxidized glutathione (GSSG), and its utilization. GSH recycling is catalyzed by glutathione disulfide reductase, which uses reducing equivalents from NADPH to reconvert GSSG to GSH.19 The relative levels of GSH and GSSG are regulated by the activity of two enzymes, glutathione peroxidase and glutathione reductase, within a series of reactions that catalyze reduction of lipid peroxides and/or hydrogen peroxide.18 Under normal conditions, the balance of this reaction series is far in the direction of maintaining cellular GSH in its reduced state. Rapid formation of GSSG can occur in cases of increased production of H2O2 and lipid peroxides and exposure to oxygen radicals.20 GSH is a major antioxidant, playing a role in protection against tissue damage resulting from exposure to an oxidizing environment such as hypoxia, radiation, and photodynamic effect.19
Angiotensin-converting enzyme (ACE) inhibitors block the activation of the renin–angiotensin system in the plasma as well as in the vascular wall.21 It should be noted that ACE inhibitors not only block the conversion of angiotensin I (ANG I) to angiotensin II (ANG II) but also inhibit the degradation of other substances, including bradykinin, substance P, and enkephalins.22 (Bradykinin is apparently responsible for adverse side effects, including cough and angioedema.23) Captopril and other drugs in this class inhibit the converting enzyme peptidyl dipeptidase that hydrolyzes ANG I to ANG II and inactivates bradykinin, a potent vasodilator that works by stimulating release of nitric oxide and prostacyclin.24 The hypotensive activity of captopril probably results from both an inhibitory action on the renin–angiotensin system and a stimulating action on the kallikrein–kinin system.25 ACE inhibitors are proposed to protect against renal vascular injury in diabetes.3 ANG II is a potent stimulator of ROS production in endothelial cells and vascular smooth muscle cells (VSMCs) by stimulating a plasma membrane-bound NAD(P)H oxidase.26,27 ACE inhibitor therapy reduces oxidant stress in the blood vessels. Moreover, captopril and enalapril have been shown to increase endogenous oxidant scavengers (antioxidants) in mouse tissue.28
Oxidation of low-density lipoproteins (LDLs) is a complex process.29 The extent of the changes in the LDL particle induced by oxidation depends on the peroxidation conditions in the LDL bio-environment. Even LDLs subjected to a very mild oxidative stress can acquire important biological properties, including the ability to stimulate the release of chemokines from endothelial cells.30 Oxidation of LDL can be caused by enzymes such as lipooxygenase that are produced by endothelial cells and monocytes/macrophages, which convert polyunsaturated fatty acids into lipid hydroperoxides and then oxidize LDL.31 Oxidized LDL (ox-LDL) may induce vasoconstriction through inhibition of NO production.32 Ox-LDL induces migration of smooth muscle cells by increasing the expression of platelet-derived growth factor (PDGF) by endothelial cells, smooth muscle cells, and macrophages.33 Ox-LDL stimulates platelet adhesion and aggregation by decreasing endothelial production of NO and increasing prostacyclin production.34 The pilot study reported herein is aimed to detect the benefit of adding an ACE inhibitor—a low dose of captopril—and determine their antioxidant activity as adjunct therapy to the treatment regimen of Type 2 diabetes mellitus (T2DM).
Materials and Methods
All participants in the study were recruited from the Diabetes Medical Center at Al-Bayda, Libya. Written informed consent was obtained from the patients before their enrollment in the current study, which adhered to the tenets of the Declaration of Helsinki for research in human subjects. Participants were of the same socio-economic class. Patients with severe renal or hepatic dysfunction and those with malignancies or hormonal disease other than DM were excluded. Participants were distributed among two different groups: Group 1 included 10 non-diabetic, non-obese healthy subjects (4 females and 6 male) with a mean age of 34.4 ± 6 years as control. Group 2 included 10 non-obese, normotensive (non-hypertensive), Type 2 diabetic patients (5 female and 5 male) with a mean age of 52.3 ± 8 years, duration of diabetes 9.7 ± 7 years, with atherosclerotic CAF on standard oral anti-diabetic treatment. Patients in group 2 were given a supplement of the ACE inhibitor captopril, 12.5 mg/day (Farcopril from Pharco Pharmaceuticals).
All patients in group 2 were re-examined monthly for evaluation of prognosis. The duration of follow-ups was 3 months. All subjects were interviewed for clinical examination, and full data sheets were kept for each subject. Coronary heart disease was documented by history, clinical examination, and ECG changes with emphasis on prolongation of the corrected QT interval. Fasting blood sugar was determined by an enzymatic calorimetric method which has been described by Trinder.35 Glycated hemoglobin (HbA1c) was determined by the turbidimetric inhibition immunoassay.
Oxidative stress was assessed by determination of thiobarbituric acid reactive substances (TBARS), calculated as malondialdehyde (MDA).36,37 Total plasma GSH, reduced GSH, and GSSG contents were measured based on an enzymatic method described by Griffith.37
Circulating ox-LDL levels were examined as cardiovascular risk factor, which was determined by using an enzyme immunoassay (EIA) kit (Cat. No. Bl-201932, Biomedica, USA).
All parameters were repeated for patients in group 2 after 1- and 3-month follow-up periods. Data were analyzed using Graphprism version 6 software. Statistical differences were tested using one-way ANOVA. Differences were considered significant at p values ≤0.05, and then Tukey honest significant difference (HSD) analysis was performed to determine whether there were statistically significant differences in the p values.
Results
Glycemic Control
A stepwise decline in plasma glucose was noted with addition of a low dose of captopril, which could be detected even in the first month of the study period; see Table 1, showing 10.3% after 1 month and 22.1% by the end of the follow-up period of 3 months. The same observation also noticed with HbA1C, which decreased by only 3.6% in the first month and by 9.9% after 3 months of treatment with captopril.
Table 1. Parameters of Glycemic Control in Type 2 Diabetic Patients and the Effect of 3 Months Adjunct Treatment with Captoprila.
| control | before treatment | 1 month treatment | 3 months treatment | |
|---|---|---|---|---|
| FBG (mg/dL) | 86.3 ± 9.7 | 197.5 ± 26.3 a | 177.1 ± 18.2 a,b | 153.8 ± 22.9a,b,c |
| (+128.9%) | (+105.2%) | (+78.2%) | ||
| HbA1c(%) | 5.00 ± 0.51 | 6.99 ± 1.08 a | 6.74 ± 1.08 a | 6.30 ± 1.09 a |
| (+39.8%) | (+34.8%) | (+26.0%) |
Data are presented as mean ± SD. Superscript letters indicate significant differences: asignificantly different from control group, bsignificantly different from patient group before treatment, and csignificantly different from patient group after 1 month of treatment, where p < 0.05. Number in parentheses represents percentage deviation from control value.
Oxidative Stress
Diabetes is associated with oxidative stress, which is reflected by increased production of TBARS and disturbance in the balance between reduced GSH and GSSG. At the start of the experiment, the mean plasma levels of TBARS in diabetics were twice as high as those of control subjects; see Table 2. Following the treatment with a low dose of captopril, lipid peroxidation was suppressed, which is represented by decreases in the level of TBARS by 3.7% in the first month and by 18.1% after 3 months (Table 2). The TBARS level decreased from 86.1% after the first month to 58.3% after 3 months of treatment, slowly but steadily declining toward the normal control level. T2DM is associated with a disturbance in GSH metabolism. The total GSH (tGSH) levels were much lower in diabetic than in control subjects. At the start of the study, the mean level of the group treated with a low dose of captopril was 47.5% below the control (Table 2).
Table 2. Parameters of Oxidative Stress in Type 2 Diabetic Patients and the Effect of 3 Months Adjunct Treatment with Captoprila.
| control | before treatment | 1 month treatment | 3 months treatment | |
|---|---|---|---|---|
| TBARS (nmol/mL) | 2.52 ± 0.46 | 4.87 ± 1.21a | 4.69 ± 1.30a | 3.99 ± 1.02a |
| (93.3%) | (+86.1%) | (+58.3%) | ||
| tGSH (nmol/mL) | 2.99 ± 0.48 | 1.57 ± 0.21 a | 1.82 ± 0.38 a | 2.33 ± 0.28 a,b,c |
| (−47.5%) | (−39.1%) | (−22.1%) | ||
| GSH (nmol/mL) | 2.76 ± 0.49 | 0.73 ± 0.13 a | 0.88 ± 0.30 a,b | 1.61 ± 0.28 a,b,c |
| (−73.6%) | (−68.1%) | (−41.7%) | ||
| GSSG (nmol/mL) | 0.12 ± 0.01 | 0.42 ± 0.05 a | 0.40 ± 0.05 a | 0.36 ± 0.04 a,b |
| (+250.0%) | (+233.3%) | (+200.0%) | ||
| GSH/GSSG ratio | 23.9 ± 5.4 | 1.7 ± 0.3 a | 2.6 ± 0.4 a | 4.5 ± 1.1 a,b |
| redox potential (mV) | –139 ± 4.7 | –66 ± 4.0 a | –75 ± 4.2 a,b | –88 ± 4.9 a,b,c |
| (−52.5%) | (−46.0%) | (−36.7%) | ||
| ox-LDL-Ab (mU/mL) | 304.1 ± 61.5 | 457.9 ± 94.5 a | 400.3 ± 76.9 a | 336.9 ± 69.8 b |
| (+50.2%) | (+31.6%) | (+10.8%) |
Data are presented as mean (SD). Superscript letters indicate significant differences: asignificantly different from control group, bsignificantly different from patient group before treatment, and csignificantly different from patient group after 1 month of treatment, where p < 0.05. Number in parentheses represents percentage deviation from control value.
T2DM not only affected tGSH values but also depressed the biologically important reduced GSH levels. The mean baseline value for GSH was substantially reduced by 73.6% in the group treated with captopril; see Table 2. Following 1 month of treatment, mean tGSH increased by 15.9% and was further increased by 48.4% over the baseline value at 3 months. This last value was still 22.1% below the mean control level (Table 2). Reduced GSH also steadily increased as a result of administration of low-dose captopril: increased by 20.5% in the first month and increased by a substantial 120.5% by the end of the follow-up period of 3 months. However, it was still below the mean control value (Table 2). On the other hand, GSSG substantially increased in all diabetic patients. The mean GSSG level in the group treated with a low dose of captopril was higher by 230.0% compared to the control. The elevation in reduced GSH level was accompanied by a decrease in GSSG. After the first month of captopril administration, the GSSG level decreased by more than 5% below the mean starting level, and it reached a statistically significant value of 20% lower by the end of 3 months. According to these results, the GSH/GSSG ratio was greatly perturbed, as it was reduced from 23.9 ± 5.4 down to 1.7 ± 0.3 upon the treatment with captopril, which indicates a great shift in the oxidation/reduction balance toward a more oxidative environment. Such a shift was confirmed by the calculations of the redox potential in these patients.
Confirmation of the presence of an oxidative environment arises from a shift in the redox potential, which changed from a mean value of −139 ± 4.7 mV in the control subjects to −66 ± 4.0 mV at the start of the treatment period, which means a shift of 52.5% toward the oxidative side in the captopril-treated group (Table 2). After 1 month of treatment, the difference was −75 ± 4.2 mV, or 46.0% from control and 13.6% from baseline, going to −88 ± 4.9 mV, or 36.7% difference from control and 33.3% from baseline, after 3 months (Table 2).
The ox-LDL antibodies (Ab) were elevated in the plasma of the diabetic groups compared with the control group. The mean value for the patients at the start of treatment was 50.2% more than for the control group. Addition of low-dose captopril to the treatment regimen caused a decline in ox-LDL-Ab, as the antibodies level decreased by 12.6% and 26.4% by the end of first and third months, respectively. However, although the level was still higher than the mean control value by 10.8%, this difference was statistically significance (Table 2).
Discussion
Diabetes is associated with an increased incidence of macrovascular complications, including CAF and cerebrovascular and peripheral vascular diseases.38 T2DM is associated with a 2- to 4-fold increased risk of coronary heart disease.39 As hyperglycemia is the hallmark of DM, it is logical to find the fasting blood glucose (FBG) levels as well as glycohemoglobin levels higher in the diabetic group with cardiac complications compared to the control group.
The effect of adding a low dose of captopril to the treatment regimen of diabetics was unexpected, as it led to improvement in glycemic status, represented by decreases in the mean FBG and HbA1C levels, not very prominent but statistically significant, probably reflecting a tendency toward better overall improvement in patients’ general health, whole body metabolism, and alleviation of oxidative stress. The results of the present study clearly indicate that there was a definite overproduction of free radicals and excessive exposure of diabetic patients to oxidative stress. The lipid peroxidation index, TBARS, was significantly higher in diabetic patients with CAD than in the control group. These findings are compatible with many reports in the literature.40
Oxidative stress occurs through several pathways. A major mechanism appears to be hyperglycemia-induced intracellular ROS generated by the mitochondrial electron transport chain, which results in increased production of superoxide radicals.41 ROS are continually generated as byproducts of normal cellular respiration, in which electrons are transferred from one molecule to another, yielding free radicals which are highly energetically unstable molecules.42 Hyperglycemia causes increased ROS formation. One mechanism involves the transition-metal-catalyzed autoxidation of free glucose. Through this mechanism, glucose itself initiates the autoxidation reaction and free radical production.43
The increase in free radicals in the present study was coupled with a disturbance in free radical scavengers. We found that GSSG was higher, while the total GSH and reduced GSH were generally lower in the diabetic group than in the control. In addition to the oxidant/antioxidant imbalance, the decreased GSH level in diabetic patients could be influenced by decreased activity of enzymes such as γ-glutamylcysteine synthase and glutathione reductase, possibly because of their glycation by hyperglycemia.44
GSH is essential for maintaining the intracellular redox balance.44 It represents the single largest source of reducing equivalents in the cell and accounts for about 90% of all cellular reducing equivalents.4 Therefore, the depletion of GSH could significantly affect the overall redox potential of the cell. By examining the calculated redox potential in the present study, it becomes clear that the redox potential for subjects with T2DM with CAD shifted to the oxidizing side and the addition of a low dose of captopril partially corrected the balance of GSH/GSSG to restore the reducing potentials, especially after 3 months. Captopril and enalpril have been shown to increase endogenous oxidant scavengers in mouse tissue.45 Decreasing the synthesis and/or blocking the action of ANG II slows the progression of atherosclerosis in diabetic patients,46 which may be due in part to a reduction in the formation of ROS. In addition, ACE inhibition improves insulin sensitivity in those with hypertension and impaired glucose metabolism because of the improvement of blood flow and therefore delivery of insulin and glucose.47 It is believed that ACE inhibitors and angiotensin II receptor blockers (ARBs) act by increasing the delivery of insulin and glucose to the peripheral skeletal muscle through blocking of ANG II, which leads to reduced incidence of diabetes, particularly in high-risk patients.48
The present study has shown alteration in the lipid profile (ox-LDL) in diabetic groups as compared to the healthy control subjects. LDL oxidation plays a key role in atherogenesis.29,49 Oxidative modification of LDL has been implicated as a major factor in the pathogenesis of coronary atherosclerosis.50 It was found that circulating ox-LDL-Ab levels in patients with T2DM were significantly higher than in control subjects. Ox-LDL exerts several biological effects that may contribute to the progression of the atherosclerosis lesion.51 Ox-LDL may also contribute to rapidly progressing atherosclerosis by inducing platelet adhesion, by decreasing the anticoagulant and fibrinolytic capacities of activated endothelium, and by impairing vasodilation.21 Moreover, many studies suggest that ox-LDL stimulates VSMCs and macrophage proliferation and promotes endothelial cytotoxicity.52
Adjunct therapy with a low dose of captopril induced an improvement in the total oxidative stress in patients with T2DM with CAD, which resulted in a significant decrease in ox-LDL. A very encouraging observation in the present study is the favorable response of ox-LDL-Ab levels to ACE inhibitor therapy. The definite and steady decline in ox-LDL-Ab level in T2DM patients with CAD was clear and is indicative of improvement in the atherosclerosis condition. The time factor is also important, as the decline in the level occurred within only 3 months of therapy.
Conclusion
The results obtained from the present study are encouraging. The clinical improvement and the shift in the disease indices toward normal make the use of low doses of ACE inhibitors as adjuvant therapy in Type 2 diabetics with cardiovascular disease worth pursuing. Thus, investigations directed at preventing or protecting against oxidative damage may provide a novel approach for managing a range of cardiovascular disorders associated with Type 2 diabetic patients.
Acknowledgments
We would like to express our gratitude to the Diabetes Medical Centre for their contribution in recruiting of patients, particularly Dr. Randa Hosny for interviewing the patients and doing the required clinical investigations.
The authors declare no competing financial interest.
Dedication
Data underlying the findings described in this Article may be obtained from the corresponding author.
References
- Kerner W.; Bruckel J. Definition, classification and diagnosis of diabetes mellitus. Exp. Clin. Endocrinol. Diabetes 2014, 122 (7), 384–386. 10.1055/s-0034-1366278. [DOI] [PubMed] [Google Scholar]
- Yamamoto S.; Okada Y.; Mori H.; Nishida K.; Uriu K.; Tanaka Y. Type 2 diabetes mellitus complicated by hypertension in Japanese patients: switching treatment from high-dose angiotensin II receptor blockers to losartan plus hydrochlorothiazide. Intern. Med. 2014, 53 (12), 1283–1289. 10.2169/internalmedicine.53.1744. [DOI] [PubMed] [Google Scholar]
- Forrester J. S. Prevention of plaque rupture: a new paradigm of therapy. Ann. Int. Med. 2002, 137 (10), 823–833. 10.7326/0003-4819-137-10-200211190-00012. [DOI] [PubMed] [Google Scholar]
- Dos Santos J. M.; Tewari S.; Mendes R. H. The Role of Oxidative Stress in the Development of Diabetes Mellitus and Its Complications. J. Diabetes Res. 2019, 2019, 4189813. 10.1155/2019/4189813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilgin S.; Kurtkulagi O.; Atak Tel B. M.; Duman T. T.; Kahveci G.; Khalid A.; Aktas G. Does C-reactive protein to serum Albumin Ratio correlate with diabEtic nephropathy in patients with Type 2 dIabetes MEllitus? The CARE TIME study. Prim. Care Diabetes 2021, 15 (6), 1071–1074. 10.1016/j.pcd.2021.08.015. [DOI] [PubMed] [Google Scholar]
- Guzik T. J.; Touyz R. M. Oxidative Stress, Inflammation, and Vascular Aging in Hypertension. Hypertension 2017, 70 (4), 660–667. 10.1161/hypertensionaha.117.07802. [DOI] [PubMed] [Google Scholar]
- Vukicevic P.; Klisic A.; Neskovic V.; Babic L.; Mikic A.; Bogavac-Stanojevic N.; Matkovic M.; Putnik S.; Aleksic N.; Kotur-Stevuljevic J. New Markers of Platelet Activation and Reactivity and Oxidative Stress Parameters in Patients Undergoing Coronary Artery Bypass Grafting. Oxid. Med. Cell. Longev. 2021, 2021, 8915253. 10.1155/2021/8915253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luc K.; Schramm-Luc A.; Guzik T. J.; Mikolajczyk T. P. Oxidative stress and inflammatory markers in prediabetes and diabetes. J. Physiol. Pharmacol. 2019, 70 (6), 2019.6.01. 10.26402/jpp.2019.6.01. [DOI] [PubMed] [Google Scholar]
- Reilly P. M.; Schiller H. J.; Bulkley G. B. Pharmacologic approach to tissue injury mediated by free radicals and other reactive oxygen metabolites. Am. J. Surg 1991, 161 (4), 488–503. 10.1016/0002-9610(91)91120-8. [DOI] [PubMed] [Google Scholar]
- Sureda F. X.; Gabriel C.; Comas J.; Pallas M.; Escubedo E.; Camarasa J.; Camins A. Evaluation of free radical production, mitochondrial membrane potential and cytoplasmic calcium in mammalian neurons by flow cytometry. Brain Res. Brain Res. Protoc. 1999, 4 (3), 280–287. 10.1016/S1385-299X(99)00030-6. [DOI] [PubMed] [Google Scholar]
- Cheeseman K. H.; Slater T. F. An introduction to free radical biochemistry. Br. Med. Bull. 1993, 49 (3), 481–493. 10.1093/oxfordjournals.bmb.a072625. [DOI] [PubMed] [Google Scholar]
- Li J.; Wang C.; Zhang Z. M.; Cheng Y. Q.; Zhou J. The structural basis of an NADP(+)-independent dithiol oxidase in FK228 biosynthesis. Sci. Rep 2014, 4, 4145. 10.1038/srep04145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally J. S.; Davis M. E.; Giddens D. P.; Saha A.; Hwang J.; Dikalov S.; Jo H.; Harrison D. G. Role of xanthine oxidoreductase and NAD(P)H oxidase in endothelial superoxide production in response to oscillatory shear stress. Am. J. Physiol. Heart Circ. Physiol. 2003, 285 (6), H2290–7. 10.1152/ajpheart.00515.2003. [DOI] [PubMed] [Google Scholar]
- Erejuwa O. O.; Sulaiman S. A.; Wahab M. S.; Salam S. K.; Salleh M. S.; Gurtu S. Antioxidant protective effect of glibenclamide and metformin in combination with honey in pancreas of streptozotocin-induced diabetic rats. Int. J. Mol. Sci. 2010, 11 (5), 2056–2066. 10.3390/ijms11052056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reus G. Z.; Dos Santos M. A.; Abelaira H. M.; Titus S. E.; Carlessi A. S.; Matias B. I.; Bruchchen L.; Florentino D.; Vieira A.; Petronilho F.; Ceretta L. B.; Zugno A. I.; Quevedo J. Antioxidant treatment ameliorates experimental diabetes-induced depressive-like behaviour and reduces oxidative stress in brain and pancreas. Diabetes Metab. Res. Rev. 2016, 32 (3), 278–288. 10.1002/dmrr.2732. [DOI] [PubMed] [Google Scholar]
- Kannan K.; Jain S. K. Oxidative stress and apoptosis. Pathophysiology 2000, 7 (3), 153–163. 10.1016/S0928-4680(00)00053-5. [DOI] [PubMed] [Google Scholar]
- Weber K. C.; Honorio K. M.; Bruni A. T.; da Silva A. B. The use of classification methods for modeling the antioxidant activity of flavonoid compounds. J. Mol. Model. 2006, 12 (6), 915–920. 10.1007/s00894-005-0083-x. [DOI] [PubMed] [Google Scholar]
- Anderson M. E. Glutathione and glutathione delivery compounds. Adv. Pharmacol. 1996, 38, 65–78. 10.1016/S1054-3589(08)60979-5. [DOI] [PubMed] [Google Scholar]
- Meister A. Glutathione, ascorbate, and cellular protection. Cancer Res. 1994, 54 (Suppl 7), 1969s–1975s. [PubMed] [Google Scholar]
- Garcia-Gimenez J. L.; Ibanez-Cabellos J. S.; Seco-Cervera M.; Pallardo F. V. Glutathione and cellular redox control in epigenetic regulation. Free Radic. Biol. Med. 2014, 75 (Suppl 1), S3. 10.1016/j.freeradbiomed.2014.10.828. [DOI] [PubMed] [Google Scholar]
- Galle J.; Quaschning T. Angiotensin II and atherosclerosis: relevance for renal disease. Contributions to Nephrology 2001, 135, 235–249. 10.1159/000060170. [DOI] [PubMed] [Google Scholar]
- Kang P. M.; Landau A. J.; Eberhardt R. T.; Frishman W. H. Angiotensin II receptor antagonists: a new approach to blockade of the renin-angiotensin system. Am. Heart J. 1994, 127 (5), 1388–1401. 10.1016/0002-8703(94)90061-2. [DOI] [PubMed] [Google Scholar]
- Haaland K. Angiotensin II receptor antagonists against migraine in pregnancy: fatal outcome. J. Headache Pain 2010, 11 (2), 167–169. 10.1007/s10194-009-0182-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter M. Kallikreins and kinins, an overview: some thoughts old and new. Adv. Exp. Med. Biol. 1983, 156, 13–27. [PubMed] [Google Scholar]
- Margolius H. S.; et al. Kallikreins and kinins. Molecular characteristics and cellular and tissue responses. Diabetes 1996, 45 (Suppl 1), S14–S19. 10.2337/diab.45.1.S14. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Puyol M.; Griera-Merino M.; Perez-Rivero G.; Diez-Marques M. L.; Ruiz-Torres M. P.; Rodriguez-Puyol D. Angiotensin II induces a rapid and transient increase of reactive oxygen species. Antioxid. Redox Signal. 2002, 4 (6), 869–875. 10.1089/152308602762197407. [DOI] [PubMed] [Google Scholar]
- Hanna I. R.; Taniyama Y.; Szocs K.; Rocic P.; Griendling K. K. NAD(P)H oxidase-derived reactive oxygen species as mediators of angiotensin II signaling. Antioxid. Redox Signal. 2002, 4 (6), 899–914. 10.1089/152308602762197443. [DOI] [PubMed] [Google Scholar]
- Bekyarova G. Y.; Ivanova D. G.; Madjova V. H. Molecular mechanisms associating oxidative stress with endothelial dysfunction in the development of various vascular complications in diabetes mellitus. Folia Med. (Plovdiv) 2007, 49 (3-4), 13–19. [PubMed] [Google Scholar]
- Steinberg D.; Parthasarathy S.; Carew T. E.; Khoo J. C.; Witztum J. L.; et al. Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity. N. Engl. J. Med. 1989, 320 (14), 915–924. 10.1056/NEJM198904063201407. [DOI] [PubMed] [Google Scholar]
- Petyaev I. M.; Dovgalevsky P. Y.; Chalyk N. E.; Klochkov V. A.; Kyle N. H. Reduction of elevated lipids and low-density lipoprotein oxidation in serum of individuals with subclinical hypoxia and oxidative stress supplemented with lycosome formulation of docosahexaenoic acid. Food Sci. Nutr. 2019, 7 (4), 1147–1156. 10.1002/fsn3.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harats D.; Shaish A.; George J.; Mulkins M.; Kurihara H.; Levkovitz H.; Sigal E. Overexpression of 15-lipoxygenase in vascular endothelium accelerates early atherosclerosis in LDL receptor-deficient mice. Arterioscler. Thromb. Vasc. Biol. 2000, 20 (9), 2100–2105. 10.1161/01.ATV.20.9.2100. [DOI] [PubMed] [Google Scholar]
- Boulanger C. M.; Tanner F. C.; Bea M. L.; Hahn A. W.; Werner A.; Luscher T. F. Oxidized low density lipoproteins induce mRNA expression and release of endothelin from human and porcine endothelium. Circ. Res. 1992, 70 (6), 1191–1197. 10.1161/01.RES.70.6.1191. [DOI] [PubMed] [Google Scholar]
- Kim J. G.; Taylor W. R.; Parthasarathy S. Demonstration of the presence of lipid peroxide-modified proteins in human atherosclerotic lesions using a novel lipid peroxide-modified anti-peptide antibody. Atherosclerosis 1999, 143 (2), 335–40. 10.1016/S0021-9150(98)00320-7. [DOI] [PubMed] [Google Scholar]
- Kiouptsi K.; Reinhardt C. Contribution of the commensal microbiota to atherosclerosis and arterial thrombosis. Br. J. Pharmacol. 2018, 175 (24), 4439–4449. 10.1111/bph.14483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinder P. Determination of blood glucose using 4-amino phenazone as oxygen acceptor. J. Clin. Pathol. 1969, 22 (2), 246. 10.1136/jcp.22.2.246-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draper H. H.; Hadley M. Malondialdehyde determination as index of lipid peroxidation. Methods Enzymol. 1990, 186, 421–431. 10.1016/0076-6879(90)86135-I. [DOI] [PubMed] [Google Scholar]
- Griffith O. W. Determination of glutathione and glutathione disulfide using glutathione reductase and 2-vinylpyridine. Anal. Biochem. 1980, 106 (1), 207–212. 10.1016/0003-2697(80)90139-6. [DOI] [PubMed] [Google Scholar]
- Bloomgarden Z. T. American Diabetes Association annual meeting, June 2003: gastrointestinal and dietary aspects of diabetes. Diabetes Care 2003, 26 (10), 2941–2946. 10.2337/diacare.26.10.2941. [DOI] [PubMed] [Google Scholar]
- Maxwell S. R.; Lip G. Y. Free radicals and antioxidants in cardiovascular disease. Br. J. Clin. Pharmacology 1997, 44 (4), 307–317. 10.1046/j.1365-2125.1997.t01-1-00594.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadiq I. Z. Free radicals and oxidative stress: signaling mechanisms, redox basis for human diseases, and cell cycle regulation. Curr. Mol. Med. 2021, 10.2174/1566524022666211222161637. [DOI] [PubMed] [Google Scholar]
- Nishikawa T.; Edelstein D.; Du X. L.; Yamagishi S.; Matsumura T.; Kaneda Y.; Yorek M. A.; Beebe D.; Oates P. J.; Hammes H. P.; Giardino I.; Brownlee M. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 2000, 404 (6779), 787–790. 10.1038/35008121. [DOI] [PubMed] [Google Scholar]
- Wolff S. P.; et al. Diabetes mellitus and free radicals. Free radicals, transition metals and oxidative stress in the aetiology of diabetes mellitus and complications. Br. Med. Bull. 1993, 49 (3), 642–652. 10.1093/oxfordjournals.bmb.a072637. [DOI] [PubMed] [Google Scholar]
- McCance D. R.; Dyer D. G.; Dunn J. A.; Bailie K. E.; Thorpe S. R.; Baynes J. W.; Lyons T. J. Maillard reaction products and their relation to complications in insulin-dependent diabetes mellitus. J. Clin. Invest. 1993, 91 (6), 2470–2478. 10.1172/JCI116482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang C.; Sinskey A. J.; Lodish H. F. Oxidized redox state of glutathione in the endoplasmic reticulum. Science 1992, 257 (5076), 1496–1502. 10.1126/science.1523409. [DOI] [PubMed] [Google Scholar]
- de Cavanagh E. M.; Inserra F.; Ferder L.; Fraga C. G. Enalapril and captopril enhance glutathione-dependent antioxidant defenses in mouse tissues. Am. J. Physiol.: Regulatory, integrative and comparative physiology 2000, 278 (3), R572–7. 10.1152/ajpregu.2000.278.3.R572. [DOI] [PubMed] [Google Scholar]
- Munger M. A. Use of Angiotensin receptor blockers in cardiovascular protection: current evidence and future directions. P & T: a peer-reviewed journal for formulary management 2011, 36 (1), 22–40. [PMC free article] [PubMed] [Google Scholar]
- Chan S. M. H.; Lau Y.-S.; Miller A. A.; Ku J. M.; Potocnik S.; Ye J.-M.; Woodman O. L.; Herbert T. P. Angiotensin II Causes β-Cell Dysfunction Through an ER Stress-Induced Proinflammatory Response. Endocrinology 2017, 158 (10), 3162–3173. 10.1210/en.2016-1879. [DOI] [PubMed] [Google Scholar]
- Jandeleit-Dahm K. A.; Tikellis C.; Reid C. M.; Johnston C. I.; Cooper M. E. Why blockade of the renin-angiotensin system reduces the incidence of new-onset diabetes. J. Hypertens. 2005, 23 (3), 463–473. 10.1097/01.hjh.0000160198.05416.72. [DOI] [PubMed] [Google Scholar]
- Navab M.; Berliner J. A.; Watson A. D.; Hama S. Y.; Territo M. C.; Lusis A. J.; Shih D. M.; Van Lenten B. J.; Frank J. S.; Demer L. L.; Edwards P. A.; Fogelman A. M.; et al. The Yin and Yang of oxidation in the development of the fatty streak. A review based on the 1994 George Lyman Duff Memorial Lecture. Arterioscler. Thromb. Vasc. Biol. 1996, 16 (7), 831–842. 10.1161/01.ATV.16.7.831. [DOI] [PubMed] [Google Scholar]
- Yoshida H. Front line of oxidized lipoproteins: role of oxidized lipoproteins in atherogenesis and cardiovascular disease risk. Rinsho Byori 2010, 58 (6), 622–630. [PubMed] [Google Scholar]
- Jialal I.; Devaraj S. The role of oxidized low density lipoprotein in atherogenesis. J. Nutrition 1996, 126 (Suppl 4), 1053S–1057S. 10.1093/jn/126.suppl_4.1053S. [DOI] [PubMed] [Google Scholar]
- Frei B. On the role of vitamin C and other antioxidants in atherogenesis and vascular dysfunction. Proc. Soc. Exp. Biol. Med. 1999, 222 (3), 196–204. 10.1046/j.1525-1373.1999.d01-136.x. [DOI] [PubMed] [Google Scholar]


