Abstract
Background:
Justice-involved youth report high rates of substance use and related problems that are associated with treatment needs; however, data on screening and linkage to treatment within the justice system is lacking. To further inform the juvenile justice behavioral health cascade of care, this study examined factors associated with identified problematic substance use and treatment referral using two screening tools.
Method:
As part of a family court intake process, 348 justice-involved youth received two screening measures, the MAYSI-2 alcohol/drug use subscale and the CRAFFT. Both tools are designed to indicate early warning signs of substance use problems and signal referral for further clinical evaluation or treatment. Chart review analysis examined whether demographic variables (sex & race), severity of use, and type of substance used were associated with positive screens on either or both measures and subsequent treatment referral.
Results:
Half (51.2%) of youth were identified as having problematic substance use (a positive screen) on at least one of the screeners. Overall, 38.5% positively screened on the CRAFFT with only 0.3% positively screening on just the MAYSI-2 alcohol/drug scale. Cannabis only users were less likely to positively screen on the MAYSI-2 compared to youth who reported use of both alcohol and cannabis. Positively screening on one versus both screeners was not associated with referral, yet many (28%) who positively screened were not referred for services.
Conclusions:
The CRAFFT may be more accurate at identifying youth specifically at risk for problematic cannabis use compared to the MAYSI-2 alcohol/drug subscale. Regardless of tool used, treatment referral was low, highlighting the need for accurate identification of treatment needs of substance-using, justice-involved youth. Interventions to facilitate referrals for youth with problematic substance use are needed.
Keywords: Juvenile justice, Adolescents, Alcohol, Cannabis, Substance use screening
1. Introduction
Youth involved in the justice system have elevated rates of trauma, behavioral disorders (e.g., Conduct Disorder), and other mental health disorders (e.g., Depression & Anxiety) compared to the general adolescent population (Teplin et al., 2002). Justice-involved youth also have increased levels of alcohol and drug related problems, including substance use disorders (SUDs; Chassin et al., 2009; Dembo et al, 1997; Rossow et al, 1999). Substance misuse is the most commonly identified problem reported in the juvenile justice system, with many adolescents presenting with drug related charges or entering the system with problematic use (Teplin et al., 2002). Substance misuse is also linked to increased recidivism and more severe criminal offenses (Aalsma et al., 2015; Colins et al., 2011; Kopak and Proctor, 2016). To address the complex needs of this population, programs aimed at diverting youth from detention have been implemented through various specialty court processing (e.g., Family Court) as an alternative to more formal court hearings. Although little research has been done in this area, diverted youth appear to have similar rates of substance use and other risky behaviors (e.g., sexual risk behaviors) to non-diverted youth (those who went through formal court processing; Tolou-Shams et al., 2007, 2008).
Implementing the use of screening tools in juvenile justice settings to help identify youth with problem drinking or drug use and referring them into treatment may be one way to mitigate the high prevalence of SUDs in this population (Aalsma et al., 2019; Belenko et al., 2017). Initial contact with the justice system provides a unique opportunity to identify substance misuse and link and engage these youth in treatment, thereby preventing continued contact with the justice system. Despite the benefit of identifying substance misuse and connecting to appropriate care, few adolescents that screen positive for potential substance misuse are further evaluated or connected to treatment services (Chassin, 2008). Furthermore, gender and racial disparities in access to available substance use care and treatment use are evident among justice involved youth (Dembo et al., 1995; Feldstein Ewing et al., 2011; Spinney et al., 2016). Given these disparities and high rates of substance misuse in this population, it is imperative to examine the utility of different substance use screeners in identifying problematic substance use, associated individual factors and subsequent treatment referral.
One widely used adolescent behavioral health screening tool in juvenile justice settings that includes a subscale for drug and alcohol screening is the Massachusetts Youth Screening Instrument-Version 2 (MAYSI-2; Grisso et al., 2012). Another tool, the CRAFFT (Mitchell et al., 2014), is commonly used in primary care settings to assess substance use. Although both tools are designed to indicate early warning signs of substance use problems and signal referral for further clinical evaluation or treatment (Grisso et al., 2001, Grisso et al., 2012, Knight et al., 2003), some evidence suggests that the MAYSI-2 Alcohol/Drug use subscale may not always identify youth in need of intervention (Grisso et al., 2012; Wasserman et al., 2004). To the authors knowledge, no studies have yet to examine the combined utility of these two measures to identify problematic substance use and the subsequent influence of identification on treatment referral among justice-involved youth. Findings could further inform the juvenile justice behavioral health cascade of care model and improve substance use screening and referral procedures for juvenile justice staff and clinicians (Becan et al., 2020).
2. Materials and method
2.1. Participants and procedures
As part of a family court diversionary program (i.e., diverted from formal court hearings), intake staff implemented mental health and substance use screening as part of intake proceedings. Staff guided youths to a private space to complete paper and pencil measures. Variables were entered into a database for the purpose of program improvement. The database was subsequently de-identified and exported into SPSS for analyses. Over approximately a 1-year period, intake staff conducted these screens with 891 youth ranging from 12 to 18 years old. Due to implementation roll-out procedures, a subset of youth (N = 348) received both the MAYSI-2 and the CRAFFT and comprised the chart review subsample for the current study1. The institutional review board approved this study as a de-identified dataset and authorized a waiver of informed consent.
3. Measures
3.1. Demographics information
Data were collected on sex, age, race and ethnicity.
Massachusetts Youth Screening Instrument—Second Version (MAYSI-2) (Alcohol/Drug Use Subscale).
The MAYSI-2 is a 52-item self-report inventory used as a mental health screening tool administered by juvenile justice personnel (Grisso and Romaine, 2006). The Alcohol/Drug Use subscale was used in this study, which assesses the frequency and pervasiveness of substance use and is comprised of 8 items (e.g., “Have you used alcohol or drugs to help you feel better?”; “Have you been drunk or high at school?”). The “yes” responses are summed for each question. The MAYSI-2 has been found to be a valid and reliable mental health screening tool for juvenile justice youth (Grisso et al., 2012).
3.2. CRAFFT screening tool
The CRAFFT is a 6-item tool designed to screen for likelihood of alcohol and other drug use disorders for children and has demonstrated strong sensitivity and specificity in predicting DSM-V SUD diagnosis (Mitchell et al., 2014). Each “yes” response is recorded and used to determine the severity of the youths’ substance use.
3.3. Referral status
A scoring protocol was developed as a guideline for intake workers to respond when scores fell in the caution or warning range on the screeners. Referral options included initiating a new referral to a community behavioral health provider, maintaining current treatment services (if relevant), and/or not referring to treatment. A referral variable was created that divided youth into three groups: 1) those not referred for treatment services; 2) those referred; and 3) those already in treatment and not referred for additional services.
3.4. Type of referral
Intake workers charted whether they referred youth to treatment services for mental health, alcohol and drug or co-occurring (mental health and substance use) needs.
3.5. Data analytic plan
First, demographic and descriptive statistics on the outcome variables were calculated (see Table 1). Rates of positive screening by youth on the CRAFFT and MAYSI-2 separately as well as on both assessments were examined to identify differences among each tool in identifying problematic substance use. A positive screen on either measure was indicative of problematic substance use and determined by a score of 2 or higher on the CRAFFT and a score of 4 or higher on the MAYSI-2. Analyses examining factors associated with referral to treatment excluded youth who reported already receiving treatment. Next, a series of logistic regressions and analyses of covariates (ANCOVAs) were conducted to examine 1) whether demographic variables (sex & race) and type or severity of substance use were associated with a positive screen on either measure; and 2) the relationship between a positive screen and subsequent treatment referral2.
Table 1.
Demographic and Descriptive Statistics for outcome variables for total sample and by substance use positive screen status.
| Total Sample N = 348 | Positively Screened† N = 178 | CRAFFT Only Positive Screens N = 134 | CRAFFT & MAYSI-2 Subscale Positive ScreensN = 43 | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Variables | N | Mean (SD)/% | N | Mean (SD)/% | N | Mean (SD)/% | N | Mean (SD)/% |
|
| ||||||||
| Age | 348 | 15.68 (1.27) | 178 | 15.66 (1.22) | 134 | 15.50 (1.21) | 43 | 16.16 (1.11) |
| Gender | 347 | 178 | 134 | 43 | ||||
| Male | 233 | 67.1% | 121 | 68.0% | 95 | 70.9% | 25 | 58.1% |
| Female | 114 | 32.9% | 57 | 32.0% | 39 | 29.1% | 18 | 41.9% |
| Race | 339 | 173 | 132 | 40 | ||||
| White | 175 | 51.6% | 101 | 58.4% | 77 | 58.3% | 23 | 57.5% |
| Black | 39 | 11.5% | 20 | 11.6% | 17 | 12.9% | 3 | 7.5% |
| Latino/Hispanic | 59 | 17.4% | 25 | 14.5% | 18 | 13.6% | 7 | 17.5% |
| Multi-Racial | 45 | 13.3% | 17 | 9.8% | 15 | 11.4% | 2 | 5.0% |
| Other | 21 | 6.2% | 10 | 5.8% | 5 | 3.8% | 5 | 12.5% |
| Referral Status | 348 | 178 | 134 | 43 | ||||
| No referral | 128 | 36.8% | 35 | 19.7% | 29 | 21.6% | 5 | 11.6% |
| Referral | 120 | 34.5% | 81 | 45.5% | 62 | 46.3% | 19 | 44.2% |
| Already in Treatment | 100 | 28.7% | 62 | 34.8% | 43 | 32.1% | 19 | 44.2% |
| Referral Typea | 119 | 81 | 62 | 19 | ||||
| Mental Health | 73 | 61.3% | 43 | 53.1% | 33 | 53.2% | 10 | 52.6% |
| Substance Use | 39 | 32.8% | 32 | 39.5% | 25 | 40.3% | 7 | 36.8% |
| Co-occurring | 7 | 5.9% | 6 | 7.4% | 4 | 6.5% | 2 | 10.5% |
| Substance Use | 347 | 177 | 133 | 43 | ||||
| No substance Use | 1 | 0.30% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Cannabis Only | 184 | 53.0% | 78 | 44.1% | 73 | 54.9% | 5 | 11.6% |
| Alcohol Only | 33 | 9.5% | 4 | 2.3% | 4 | 3.0% | 0 | 0.00% |
| Co-use | 129 | 37.2% | 95 | 53.7% | 56 | 42.1% | 38 | 88.4% |
Note. Because only 1 youth positively screened on just the MAYSI-2 alcohol/drug use scale, a separate column displaying demographic and descriptive data specifically for positive screens on just the MAYSI-2 alcohol/drug use subscale was not included in the table.
indicates all participants who positively screened for problematic substance use (including the 1 participant who positively screened on just the MAYSI-2 alcohol/drug use subscale).
only includes participants who were referred for treatment in each group. Co-use = concurrent use of both alcohol and cannabis.
4. Results
4.1. Descriptive statistics
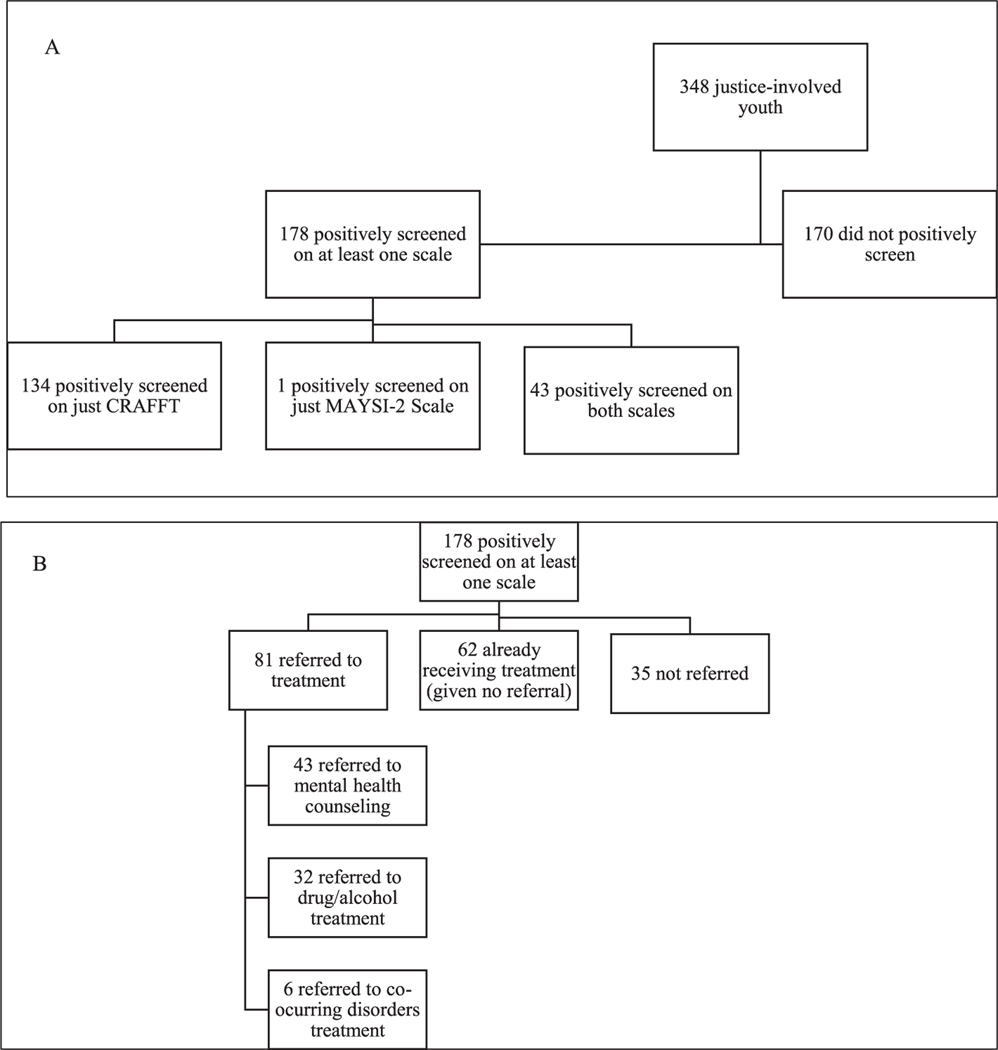
The majority of the 348 youth were male (67.1%) and self-identified as White (51.6%), Latinx (17.4%), Multi-racial (13.3%), and Black (11.5%) with an average age of 15.68 (SD = 1.27). Regarding past year substance use, the majority of youth (53.7%) reported using both alcohol and cannabis, 44.1% reported only using cannabis, and 2.3% of youth reporting just alcohol use. Approximately 51.2% (n = 178) positively screened on at least one of the two substance use screeners. Of those who positively screened, only 0.3% (n = 1) screened positive on just the MAYSI-2 alcohol/drug scale with 38.5% (n = 134) positively screening on just the CRAFFT. A total of 12.4% (n = 43) of youth positively screened on both the CRAFFT and the MAYSI-2 alcohol/drug scales. Hence, most youth (all but 1) who were identified as at-risk for problematic substance use by the MAYSI-2 alcohol/drug use subscale, also positively screened on the CRAFFT. However, 134 youth were identified as at-risk for problematic substance use by the CRAFFT but were not identified as at-risk by the MAYSI-2 alcohol/drug use subscale (See Fig. 1).
Fig. 1.
Panel A depicts the participant flow of positive screens. Panel B depicts the participant flow of treatment referral for youth who positively screened for problematic substance use.
Of the 178 youth who positively screened on at least one screener, 45.5% were referred to treatment, 34.8% were already receiving treatment and given no additional referral, and 19.7% were not referred. Of the youth who positively screened and were not already receiving treatment, only 28% were referred to substance use treatment services (See Fig. 1).
5. MAYSI-2 and CRAFFT screening analyses
5.1. Demographic and substance use severity differences in positive assessment screens
Because only 1 participant positively screened on just the MAYSI-2 alcohol/drug subscale, analyses examining demographic and substance use severity associations of positive screens by screening measure could only compare youth who screened positive on both tools versus those who screened positive on just the CRAFFT. Logistic regression analyses demonstrated that sex, race and ethnicity were not positively associated with positively screening (p > .05) on just the CRAFFT versus both screeners. However, ANCOVA analyses controlling for sex, race and ethnicity, demonstrated that youth who positively screened on both screeners demonstrated significantly higher total scores on the CRAFFT and the MAYSI-2 alcohol/drug use subscale compared to youth who only positively screen on just the CRAFFT (ps < 0.0001). Additional logistic regression analysis examining substance use severity indicated that youth who reported past year co-use of alcohol and cannabis had 10.17 times greater odds of positively screening on both the MAYSI-2 and CRAFFT compared to youth using cannabis alone (p < .0001; CI = 3.52–29.42; See Table 2)3.
Table 2.
Logistic regression models examining demographics and substance use associations of positively screening on the MAYSI-2 and CRAFFT.
| Variable | 95% CI | ||||
|---|---|---|---|---|---|
|
|
|||||
| B | OR | Lower | Upper | P | |
|
| |||||
| Step 1 | |||||
| Gender† | − 0.30 | 0.74 | 0.33 | 1.68 | 0.473 |
| Race | 0.329 | ||||
| White | ref | ref | ref | ref | |
| Black | −0.36 | 0.70 | 0.16 | 3.13 | 0.642 |
| Latino/Hispanic | −0.73 | 0.48 | 0.16 | 1.49 | 0.203 |
| Multi-Racial | 0.15 | 1.17 | 0.21 | 6.30 | 0.861 |
| Other | −1.47 | 0.23 | 0.05 | 1.10 | 0.066 |
| Step 2 | |||||
| Substance Usea | 2.32 | 10.17 | 3.52 | 29.42 | 0.000* |
Note. OR = odds ratio; CI = confidence interval.
Females were coded as 1.
Co-use of both alcohol and cannabis was coded as 1 and use of just cannabis was coded as 0. Flagging on both the MAYSI-2 and the CRAFFT was coded as 1 and flagging on just the CRAFFT was coded as 0.
p ≤ 0.001.
5.2. Treatment referral analyses
After controlling for sex, race and ethnicity, positively screening on just the CRAFFT versus both screeners was not associated with treatment referral (p > .05). Hence, youth identified as at-risk for substance use by both screening tools were no more likely to be referred to treatment than youth who positively screened on just the CRAFFT. Similarly, in youth that were referred to treatment, positively screening on the CRAFFT only versus both screeners was not associated with type of treatment referred to (Mental Health vs. Alcohol and Drug services)4.
6. Discussion
The current study examined the ability of two different substance use screening measures to identify justice-involved youth in need of substance use treatment services, identify demographic and substance use severity factors associated with positive screens and subsequent treatment referral rates by court staff. Results suggest the CRAFFT may be more accurate at identifying justice involved youth at risk for problematic substance use compared to the MAYSI-2 alcohol/drug scale. This may be especially true for youth who only use cannabis. Specifically, findings indicate that youth who reported only using cannabis in the past year were less likely to positively screen on the MAYSI-2 alcohol/ drug use subscale compared to youth who reported past year use of both alcohol and cannabis. In other words, youth reporting just using cannabis in the past year were more likely to be categorized as at-risk for problematic substance use by the CRAFFT (but not the MAYSI-2) compared to those using both substances. Neither sex, race nor ethnicity was associated with a positive screen on either measure. Positively screening on one versus both screeners did not influence treatment referral rates, but of those who positively screened for problematic substance use and were not already receiving treatment, only about 28% were referred for substance use treatment services.
These findings are somewhat consistent with prior work acknowledging the limitation of the MAYSI-2 alcohol and drug subscale to accurately identify youth in need of intervention (Grisso et al., 2012). While this limitation has often been attributed to youth being hesitant to disclose substance use in a court setting, our findings suggest an alternative explanation. Despite some item level overlap between these two screening tools (e.g., Getting into trouble and/or forgetting what happened while using alcohol or drugs), the MAYSI-2 substance use subscale may have a higher threshold for positive screens compared to the CRAFFT. For example, the MAYSI-2 requires endorsement of a greater number of substance-related consequences within a shorter time period to generate a positive screen compared to the CRAFFT. Hence the MAYSI-2 may be assessing more diagnostic criteria rather than general behaviors that represent problematic substance use, resulting in a certain missed subset of substance using youth.
There may be some risk in using the MAYSI-2 substance use scale as the sole substance use screener in juvenile justice settings (especially for diverted youth) in that adolescents who are heavily using cannabis and might benefit from intervention are not being identified for services. Approximately 40% of youth were identified as at-risk for problematic substance use by the CRAFFT, but not the MAYSI-2 Alcohol/Drug Use subscale. This has implications for adolescents who are screening positive for substance misuse early on and could benefit from early intervention to offset future use and legal difficulties. Not capturing cannabis-only users is concerning because cannabis is the most commonly reported illicit substance used among justice-involved youth (Grigorenko et al., 2015; Racz et al., 2016). Of the adolescents involved in the court system that meet criteria for an SUD, the majority are diagnosed with cannabis use disorder (CUD; Tolou-Shams et al., 2014). While the CRAFFT is commonly used in primary care settings, our findings highlight the utility of its use in juvenile justice settings as well.
This study has several relevant limitations. Data were collected at one family court in the Northeastern United States and may be not generalizable to other juvenile justice populations. Furthermore, because this was conducted in a court setting, youth may have been hesitant to provide honest answers regarding their substance use. Further, only 4 youth reported just using alcohol so analyses were unable to examine the likelihood of alcohol only or non-cannabis using youth to positively screen on either measure. Future work should examine these associations with a more inclusive range of substance using youth. Similarly, these analyses were conducted solely with diverted youth. Future work should examine the combined utility of these two screening tools with non-diverted youth. Data were collected via a retrospective chart review so future work may want to prospectively examine substance use screening and referral procedures, as well as subsequent treatment attendance in this population. Finally, due to implementation procedures, only a subset of youth included in this chart review received both the CRAFFT and the MAYSI-2.
Despite these limitations, study findings have important clinical implications for substance use screening and referral procedures in juvenile justice settings. Our results highlight the importance of using both the CRAFFT and the MAYSI-2 when screening for substance use risk in juvenile justice settings. The MAYSI-2 has utility in identifying youth at risk for a variety of mental health concerns, it may not be as accurate as the CRAFFT in identifying cannabis-only using youth, although more research in this area is warranted. Approximately 20% of youth who positively screened on at least one measure were ultimately not referred to any treatment. Of those who were not already receiving treatment, only 28% were referred to substance use treatment services. Hence, a subset of youth at-risk for (or already are) engaging in problematic substance use behaviors are not being identified or referred to appropriate treatment services. This is concerning as unidentified and untreated substance use is related to the development of substance use disorders and reoffending (Hoeve et al., 2014; Schubert et al., 2011). This lack of referral could in part be explained by a dearth of substance use treatment available in the community (Funk et al., 2020; Mericle et al., 2015). Despite youth positively screening, intake staff may be unsure of where to refer youth for further evaluation and ultimately just refer for mental health services or do not refer at all. Alternatively, individuals responsible for the initial screening may lack the requisite clinical background to navigate the appropriate next steps for substance using youth. Hence, there may be a need for increased workforce development and learning system models that provide training and supervision in screening procedures for justice staff (Sheidow et al., 2020; Viglione et al., 2020). Further, improving coordination between juvenile justice departments and private sector service providers may enhance the successful implementation of substance use screening and referral outcomes. Utilizing decision-making and progress-monitoring process- improvement plans may also help to identify and address gaps in services and implement practice improvement strategies (Becan et al., 2020).
Acknowledgments
This research was supported by K23 MH111606 (Kemp) and K24DA046569 (Tolou-Shams). Ali Yurasek’s contribution to the manuscript was supported by National Institute on Drug Abuse (NIDA) grant K23 DA046565–01. NIMH and NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
My coauthors and I do not have any interests that might be interpreted as influencing the research. The paper contains original material and is not currently in press, published or submitted elsewhere for publication. All authors have contributed significantly to the manuscript and have agreed to the submission of the manuscript in this form.
7. Funding sources
This research was supported by K23 MH111606 (Kemp) and K24DA046569 (Tolou-Shams). Ali Yurasek’s contribution to the manuscript was supported by National Institute on Drug Abuse (NIDA) grant K23 DA046565–01. NIMH and NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
As part of the original implementation roll-out plan, the addition of the CRAFFT as part of intake proceedings was implemented after the MAYSI-2 resulting in a reduced sample size. The 348 youth who received both the MAYSI-2 and CRAFFT screeners were significantly older and more likely to be male compared to youth who were screened with just the MAYSI-2.
Primary analyses were also conducted controlling for additional mental health positive screens on the MAYSI-2. Inclusion of this covariate did not alter the pattern of results.
Only 4 youth reported not using cannabis (and just using alcohol), therefor substance use analyses did not include alcohol only users or non-cannabis users.
Because only 6 youth were referred to Co-Occurring Disorder services, it was not included in the treatment referral outcome variable for this analysis.
References
- Aalsma MC, White LM, Lau KS, Perkins A, Monahan P, & Grisso T. (2015). Behavioral health care needs, detention-based care, and criminal recidivism at community reentry from juvenile detention: A Multisite survival curve analysis. American Journal of Public Health, 105(7), 1372–1378. 10.2105/AJPH.2014.302529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aalsma MC, Dir AL, Zapolski TCB, Hulvershorn LA, Monahan PO, Saldana L, et al. (2019). Implementing risk stratification to the treatment of adolescent substance use among youth involved in the juvenile justice system: Protocol of a hybrid type I trial. Addiction Science and Clinical Practice, 14(1). 10.1186/s13722-019-0161-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becan JE, Fisher JH, Johnson ID, Bartkowski JP, Seaver R, Gardner SK, et al. (2020). Improving substance use services for juvenile justice-involved youth: Complexity of process improvement plans in a large scale multi-site study. Administration and Policy in Mental Health and Mental Health Services Research, 47(4), 501–514. 10.1007/s10488-019-01007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belenko S, Knight D, Wasserman GA, Dennis ML, Wiley T, Taxman FS, et al. (2017). The juvenile justice behavioral health services cascade: A new framework for measuring unmet substance use treatment services needs among adolescent offenders. Journal of Substance Abuse Treatment, 74, 80–91. 10.1016/j.jsat.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L. (2008). Juvenile justice and substance use. The Future of Children, 18(2), 165–183. 10.1353/foc.0.0017. [DOI] [PubMed] [Google Scholar]
- Chassin A L Hussong I. Beltran RM Lerner L. Steinberg Handbook of Adolescent Psychology John Wiley & Sons, Inc. Hoboken, NJ, USA: 10.1002/9780470479193.adlpsy001022. [DOI] [Google Scholar]
- Colins O, Vermeiren R, Vahl P, Markus M, Broekaert E, & Doreleijers T. (2011). Psychiatric disorder in detained male adolescents as risk factor for serious recidivism. The Canadian Journal of Psychiatry, 56(1), 44–50. 10.1002/9781118133880.hop211016. [DOI] [PubMed] [Google Scholar]
- Dembo R, Pacheco K, Schmeidler J, Fisher L, & Cooper S. (1997). Drug use and delinquent behavior among high risk youth. Journal of Child and Adolescent Substance Abuse, 6(2), 1–23. 10.1300/J029v06n02_01. [DOI] [Google Scholar]
- Dembo R, Schmeidler J, Chin Sue C, Borden P, & Manning D. (1995). Journal of Correctional Health Care, 2, 191–216. [Google Scholar]
- Hoeve M, McReynolds LS, & Wasserman GA (2014). Service referrals for juvenile justice youths: Associations with psychiatric disorder and recidivism. Administration and Policy in Mental Health and Mental Health Services Research, 41, 379–389. [DOI] [PubMed] [Google Scholar]
- Feldstein Ewing SW, Venner KL, Mead HK, & Bryan AD (2011). Exploring racial/ethnic differences in substance use: A preliminary theory-based investigation with juvenile justice-involved youth. BMC Pediatrics, 11, 71. 10.1186/1471-2431-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk R, Knudsen HK, McReynolds LS, Bartkowski JP, Elkington KS, Steele EH, et al. (2020). Substance use prevention services in juvenile justice and behavioral health: Results from a national survey. Health & Justice, 8(1). 10.1186/s40352-020-00114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigorenko EL, Edwards L, & Chapman J. (2015). Cannabis use among juvenile detainees: Typology, frequency and association. Criminal Behavior and Mental Health, 25(1), 54–65. 10.1002/cbm.v25.110.1002/cbm.1913. [DOI] [PubMed] [Google Scholar]
- Grisso T. and Riggs Romaine CL (2012). Forensic Evaluation in Delinquency Cases. Handbook of Psychology, Second Edition (eds Weiner I. and Otto RK). 359–380. [Google Scholar]
- Grisso T, Barnum R, Fletcher KE, Cauffman E, & Peuschold D. (2001). Massachusetts Youth Screening Instrument for mental health needs of juvenile justice youths. Journal of the American Academy of Child and Adolescent Psychiatry, 40 (5), 541–548. 10.1097/00004583-200105000-00013. [DOI] [PubMed] [Google Scholar]
- Grisso T, Fusco S, Paiva-Salisbury M, Perrauot R, Williams V, & Barnum R. (2012). The Massachusetts Youth Screening Instrument-Version 2 (MAYSI-2): Comprehensive research review. Worcester: University of Massachusetts Medical School. [Google Scholar]
- Knight JR, Sherritt L, Harris SK, Gates EC, & Chang G. (2003). Validity of brief alcohol screening tests among adolescents: A comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcoholism, Clinical and Experimental research, 27(1), 67–73. 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- Kopak AM, & Proctor SL (2016). Acute and chronic effects of substance use as predictors of criminal offense types among juvenile offenders. Journal of Juvenile Justice, 5, 50–64. [Google Scholar]
- Mericle AA, Arria AM, Meyers K, Cacciola J, Winters KC, & Kirby K. (2015). National trends in adolescent substance use disorders and treatment availability: 2003–2010. Journal of Child & Adolescent Substance Abuse, 24(5), 255–263. 10.1080/1067828X.2013.829008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SG, Kelly SM, Gryczynski J, Myers CP, O’Grady KE, Kirk AS, et al. (2014). The CRAFFT cut-points and DSM-5 criteria for alcohol and other drugs: A reevaluation and reexamination. Substance Abuse, 35(4), 376–380. 10.1080/08897077.2014.936992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert CA, Mulvey EP, & Glasheen C. (2011). Influence of mental health and substance use problems and criminogenic risk on outcomes in serious juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry, 50(9), 925–937. [DOI] [PubMed] [Google Scholar]
- Spinney E, Yeide M, Feyerherm W, Cohen M, Stephenson R, & Thomas C. (2016). Racial disparities in referrals to mental health and substance abuse services from the juvenile justice system: A review of the literature. Journal of Crime and Justice, 39(1), 153–173. 10.1080/0735648X.2015.1133492. [DOI] [Google Scholar]
- Racz SJ, Saha S, Trent M, Adger H, Bradshaw CP, Goldweber A, et al. (2016). Polysubstance use among minority adolescent males incarcerated for serious offenses. Child Youth Care Forum, 45(2), 205–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossow I, Pape H, & Wichstrom L. (1999). Young, wet & wild? Associations between alcohol intoxication and violent behaviour in adolescence. Addiction, 94, 1017–1031. 10.1046/j.1360-0443.1999.94710177.x. [DOI] [PubMed] [Google Scholar]
- Sheidow AJ, McCart MR, Chapman JE, & Drazdowski TK (2020). Capacity of juvenile probation officers in low-resourced, rural settings to deliver an evidence- based substance use intervention to adolescents. Psychology of Addictive Behaviors, 34 (1), 76–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, & Mericle AA (2002). Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 59 (12), 1133–1143. 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolou-Shams M, Brown LK, Gordon G, & Fernandez I. (2007). Arrest history as an indicator of adolescent/ young adult substance use and HIV risk. Drug and Alcohol Dependence, 88(1), 87–90. [DOI] [PubMed] [Google Scholar]
- Tolou-Shams M, Brown LK, Houck C, & Lescano CM (2008). The association between depressive symptoms, substance use, and HIV risk among youth with an arrest history. Journal of Studies on Alcohol and Drugs, 69(1), 58–64. [DOI] [PubMed] [Google Scholar]
- Tolou-Shams M, Rizzo CJ, Conrad SM, Johnson S, Oliveira C, & Brown LK (2014). Predictors of detention among juveniles referred for a court clinic forensic evaluation. The Journal of the American Academy of Psychiatry and the Law, 42(1), 56–65. [PMC free article] [PubMed] [Google Scholar]
- Viglione J, Alward LM, & Sheppard DL (2020). Staff Training Aimed at Reducing Rearrest: Probation officer attitudes and experiences. European Journal of Probation, Epub ahead of print. [Google Scholar]
- Wasserman G, Vilhauer J, McReynolds L, Shoai R, & John R. (2004). Mental health screening in the juvenile justice system: A comparison between the Voice-DISC-IV and the MAYSI-2. Journal for Juvenile Justice Services, 19, 7–17. [Google Scholar]