Abstract
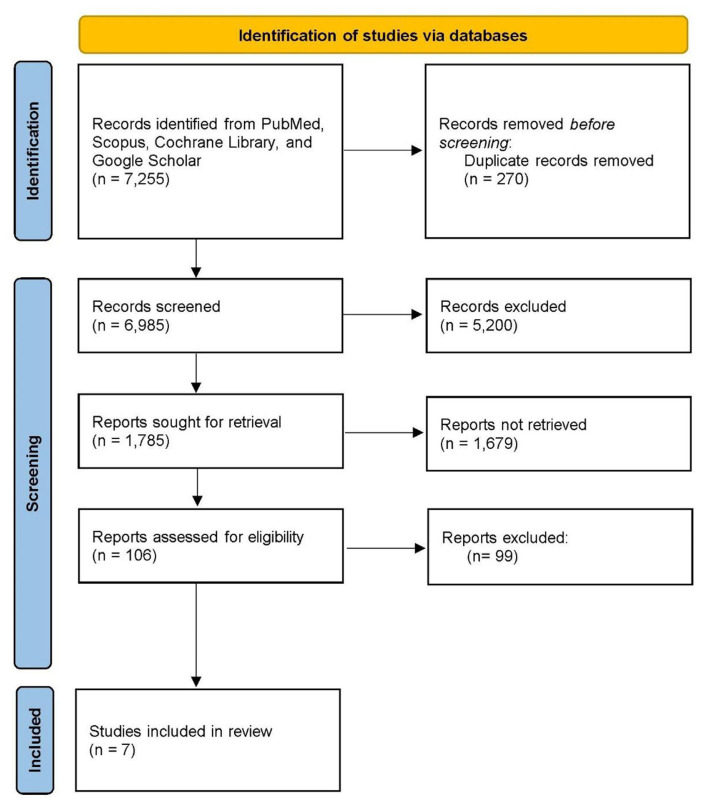
Electronic cigarettes have grown in popularity due to natural curiosity, novel flavors, and advertising as both a means to aid smoking cessation and a “safe” smoking option. There is a substantial body of research on the harmful physical health effects of vaping, but there are relatively few studies on its mental health effects, particularly in adolescents 10–21 years of age. The purpose of this review is to examine the negative effects of vaping on mental health, in particular depression and suicidality. Using the databases PubMed, Scopus, Cochrane Library, and the search engine Google Scholar, we focused on observational studies looking into association between vaping, depression and suicidality. We found 7255 studies; after removing duplicates and other irrelevant articles, 106 articles were left. After reviewing the abstracts and titles, 99 citations were manually removed, 7 studies were included in the final review. Suicide attempts were significantly higher among e-cigarette users compared to non-users. E-cigarette use was associated with depression, suicidal ideation and suicide attempt. Suicide attempts were significantly higher among e-cigarette users compared to non-users. It is critical to raise awareness about the association between electronic cigarettes and adolescent mental health.
Keywords: Vaping, Electronic cigarettes, Mental health, Depression, Suicidality
1. Introduction
Vaping devices, also known as electronic nicotine delivery systems, are used to inhale vapors containing nicotine and other potentially harmful substances.1 These devices, more commonly known as e-cigarettes (electronic cigarettes), were introduced to primarily assist adult smokers in quitting the use of combustible tobacco cigarettes.1 Vape pens, e-hookahs, pod mods, and tanks are some other names for these devices. These are battery-powered devices containing a proprietary liquid that is heated into an aerosol that users inhale.2 The cartridges’ liquid commonly contains propylene glycol or glycerol, nicotine, tetrahydrocannabinol, or flavoring chemicals. Volatile organic products, heavy metals (nickel and lead), Diethylene glycol, acrolein, and diacetyl are also harmful ingredients.2
The use of e-cigarettes among adolescents is on the rise. According to the 2019 National Youth Tobacco Survey more than 5 million middle and high school students used e-cigarettes in 2019.3 Some of the reasons for the significant increase in adolescent vaping include 1) misconceptions about the safety of e-cigarettes, 2) lower prices than traditional cigarettes, 3) a variety of flavors such as fruits and candy, and 4) social or peer pressure.4 Eight out of every ten users preferred flavored e-cigarettes, with menthol being the most popular flavor.3
Vaping has been shown to have numerous harmful effects on the physical and mental health of individuals. E-cigarette or Vaping use Associated Lung Injury (EVALI) was first identified in 2019.5 A total of 2807 EVALI hospitalized cases, or deaths have been reported since February 2020.2 Additionally, nicotine (one of the components of E-cigarettes) use in adolescents has been shown to cause severe impairment to the growing brain leading to cognitive and psychiatric issues6 like depression, anxiety, violence, other substance abuse, and suicidality. 7 Because of the growing public health crisis and health consequences, the Food and Drug Administration (FDA) recommended a ban on most flavored vaping cartridges and pods in 2020.4 To protect youth from the harmful side effects of vaping, the minimum age for purchasing tobacco-containing products was raised from 18 to 21 years old.4
This review aims to present comprehensive evidence from the literature on the association of e-cigarette use and mental health outcomes particularly depression and suicidality. We hope to raise awareness among adolescents, their parents, teachers, healthcare providers, and the entire community and subsequently decrease the incidence of mental health disorders associated with the use of EC through various public health measures.
2. Methods
We use the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement 2020.8 A review of white literature was conducted using the electronic databases PubMed, Scopus, the Cochrane library, and for grey literature Google Scholar was utilized, with a focus on studies on E-cigarettes and their mental health consequences. The review included observational studies that looked at the impact of vaping on adolescent mental health, particularly depression and suicidality. This review included studies published in the previous 5 years up until April 30, 2021, examining the impact of vaping on adolescent mental health. Search terms included: Vaping OR Electronic cigarettes OR E-cigarettes AND Depression AND Suicidality. Two authors (SJ and SU) blindly screened all articles obtained from the search using titles and abstracts to identify relevant articles for full-text consideration. Disagreements were resolved through discussion, and a consensus was reached. On the initial search, we found 7255 articles in the literature; after removing duplicates and other irrelevant articles, we were left with 106 articles. 99 citations were manually removed after reviewing the abstracts and titles. The final review included 7 studies in total (see Fig. 1).
Fig. 1.
PRISMA flowchart.
3. Results
The characteristics of included studies are listed in Table 1. Synthesis of key findings is presented below.
Table 1.
Characteristics of included studies. EC = Electronic Cigarettes; CC: Combustible cigarettes; F= Female; M = Male; N/A: Not available; YRBS - Youth Risk Behavior Survey, MTF -, RCADS - Revised Children’s Anxiety and Depression Scale, MDQ - Mood Disorder Questionnaire, DTS - Distress Tolerance Scale, CASI - Childhood Anxiety Sensitivity Index, SHAPS - Snaith-Hamilton Pleasure Scale, TCI - Temperament and Character Inventory Impulsivity Scale, UPPS-P - Positive and Negative Urgency Subscales, EATQ - The Early Adolescent Temperament Questionnaire-R-Inhibitory Control Scale, DAST - Drug Abuse Screening Test-Adolescent Version, CAST - Cannabis Abuse Screening Test, RAPI - Rutgers Alcohol Problem Index.
| Author | Country | Age (years) | Sample Size (n) | Gender (female) | Ethnicity | Data collection frequency | Outcomes | Measure of Outcome |
|---|---|---|---|---|---|---|---|---|
| Tram Pham, 2019 | Canada | >12 | 53,050 | 50.7% | NA | NA | Depression, Suicide attempts and thoughts. | Depressive symptoms were assessed using the 9-item Patient Health Questionnaire (PHQ-9) |
| Chadi et al., 2019 | USA | 14–18 | 26,821 | 51.3% | Whites = 44.8% African Americans = 14.5% Hispanics = 29.4% All others = 11.3% |
60% | Suicidal ideation and depressive symptoms | Youth Risk Behavior Survey (YRBS) |
| Kim et al., 2019 | Korea | 14.5–17.3 | 5405 | 18.9% | NA | Once | Suicidal ideation, suicidal plans, suicidal attempts, serious attempts | 12th Korea Youth Risk Behavior Web-based Survey (KYRBWS-XII) |
| Lee et al., 2019 | Korea | 13–18 | 62,276 | 49.3% | NA | 95.8% | Depression, suicidal Ideation, suicide planning, and suicide attempt | 2017 Korean Youth Risk Behavior Web-based Survey (KYRBWS), |
| Lechner et al., 2017 | USA | 13.7–14.5 | 2460 | 53% | NA | Baseline, 6 months, 12 m | Depression | 20-item Center for Epidemiologic Studies – Depression Scale (CES-D) |
| Jee et al., 2016 | South Korea | 12–18 | 11,313 | 24.6% | NA | NA | Sadness and hopelessness, suicidal plans and suicide attempts, suicidal ideation | 2015 Korea Youth Risk Behavior Web-based Survey (KYRBS) |
| Leventhal et al., 2016 | USA | 13.7–14.5 | 3310 | F = 53.4% | NA | Once | Major depression | YRBS survey, RCADS, MDQ, DTS, CASI, SHAPS, TCI Impulsivity Scale, UPPS-P, EATQ-R Inhibitory Control Scale, DAST, CAST, RAPI |
3.1. Depression
Five of the seven studies included depression as a primary outcome. Lechner et al. (2017), discovered that continued use of electronic cigarettes (EC) with or without concurrent use of CC worsened depressive symptoms, resulting in a deterioration of the individual’s mental health.9 Lechner and colleagues showed a bidirectional relationship between EC use and depression and noticed that adolescents who were depressed were more likely to initiate EC use and dual-use than non-users. They found that the past 30-day frequency of EC use was positively associated with depressive symptoms at the final follow-up. The authors suggested a longer follow-up period to observe depressive symptoms. These findings were reinforced by many other studies (i.e., Lee & Lee, 2019; Chadi et al., 2019 and Jee, 2016), all of whom reported finding higher levels of depression in EC users.10–12 Female EC users, as compared to males, were found to have a greater risk of mental health issues, including depression and suicide ideation.10,11,13
Leventhal et al. (2016) reported higher internalizing outcomes of depression in EC only users compared to non-users.14 However, these outcomes were lower compared to CC only or dual users (p < 0.0001).14 Also, the prevalence of mental health issues including depression, anhedonia was found to be higher in EC users compared to non-users.14 The risk of developing depression or anxiety was higher in dual users and CC users compared to adolescents who only used ECs.14 Pham et al. (2020) examined the prevalence of depression, suicidal ideation, and attempts among various age groups, genders, education, employment, geographical region, income, and relationship status.10 In the age group 12–18 years, the prevalence of depressive symptoms was 9.1% and the prevalence of serious suicidal ideation/attempts was 3.2%. Adverse mental health impact was more prominent in dual users. Smoking status and gender were identified as important modifiers for the association between EC use and mental health.
3.2. Suicidality
Chadi et al. (2019), described in their study, the link between single or dual-use EC and depressive symptoms and suicidality in high school students (n = 26,821) using the risk behavior survey.11 They reported 9.1% of exclusive EC users (vs non-use) were associated with suicidal ideation (AOR = 1.23, 95% CI: 1.03–1.47) and depressive symptoms (AOR = 1.37, 95% CI: 1.19–1.57).11 30.7% of participants reported experiencing depressive symptoms for more than 2 weeks and 17.3% reported seriously considering attempting suicide in the past year.11 EC only and dual EC and marijuana users reported more depressive symptoms and suicidality compared to non-users.11 In addition, Jee (2016) explored the comparison between the use of e-cigarettes and psychological and emotional health indicators in Korean youth smokers by using the data from the 2015 Korean youth risk behavior web bases survey.12 They reported higher rates of sadness and hopelessness, suicidal plans, and suicide attempts among the past-12-month EC users (compared to non-users).12 Males were more adversely affected than females, mostly used EC in high school, 10% started using EC because of curiosity and would buy these from friends or seniors at school.12
The results were consistent with another study where Kim & Kim (2019) who reported higher suicidal ideation (AOR = 1.58, 95% CI: 1.31–1.89, p < 0.05), suicidal plans (AOR = 2.44, 95% CI: 1.94–3.08, p < 0.05), suicidal attempts (AOR = 2.44, 95% CI: 1.85–3.22, p < 0.05), and serious attempts (AOR = 3.09, 95% CI: 1.51–6.32, p < 0.05) among the past 30-day EC users (versus non-users).15 However, as compared to the above-mentioned study Kim & Kim (2019) reported that most high school EC users were females, had very high or low socioeconomic status and very high or low school performance, making the user profiles and associated factors bimodal in distribution; had very high or low subjective health status, reported greater awareness about depression, lifetime drinking and habitual drug use.15
3.3. Depression and suicidality
Some studies analyzed both depression and suicide as their primary outcomes. Lee & Lee (2019) found that male adolescents, who were EC-only users had a higher suicide attempt prevalence of 5.9%, whereas female adolescents showed the prevalence of suicide planning of 16.8% and suicide attempt of 14.3%.10 Male dual users showed the highest prevalence in the depression of 34.2%, suicidal ideation of 16.1%, and suicide planning of 7.0%.10 Female dual users showed the highest prevalence in the depression of 53.2% and suicidal ideation of 29.4% (53.2% and 29.4%, respectively).10 EC only users compared to non-EC or CC users were associated with depression, suicidal ideation, suicide planning, and suicide attempt. EC current users compared to non-EC or CC users were associated with depression, suicidal ideation, suicide planning, and suicide attempt. The adjusted Odds Ratio (AOR) for suicide plans and attempts were much higher in female than male EC users. Alternatively, Leventhal et al. (2016) described lower levels of internalizing symptoms (depression, GAD, panic disorder, social phobia, OCD) in EC users compared to CC and dual users.14 Overall, it was found that adolescents who used ECs were more likely to consider attempting suicide and had a higher-than-average number of suicide attempts.11–13,15
4. Discussion
There has been an alarming increase in the popularity and usage of e-cigarettes among adolescents 10–21 years of age. In addition to the detrimental physical effects, e-cigarettes have been found to have a negative impact on mental health among this age group. EC is advertised in attractive packaging with a variety of unique flavors, which entices curious adolescents who want to try nicotine and smoking products. The use of EC has been particularly promoted by social media fads in which ‘influencers’ encourage teenagers to use e-cigarettes in the belief that it is safe and socially acceptable. The risk of EC use is greater in adolescents with impulsive personality traits as they tend to initiate EC at an earlier age and use them more often.16
At present, there are more than 30 annual vaping conventions in the US; vape clubs tend to hold national and local conventions with upwards of thousands of attendees at each event. This is of drastic concern to public health and healthcare workers due to the emerging vaping culture and its connection to adverse mental health outcomes.17 Flavors such as “captain crunch berries” and “cookies and cream” appeal to audiences in middle and high school that have a high rate of e-cigarette update.17
A systematic thematic analysis of 808 e-cigarette/vaping-related videos in TikTok that is a video sharing service presented a synthesis of likes, themes, and categories of the users.18 The study found that the shortlisted videos were viewed around 1.5 billion times; moreover, 63% of the videos depicted vaping in a positive manner. The themes in the videos included 52% being comedic, 20% showing vaping tricks, 20% targeting nicotine and addiction, 16% being creative in nature, and only 11% had a warning.18
The findings illustrate the vaping and e-cigarette postings are available without age restrictions in TikTok, a video-sharing platform that is popular among adolescents; effective disclaimers and age restrictions ought to be imposed by public health professionals to reduce exposure to positive vaping portrayals.18
There is compelling evidence from published data that there is a higher incidence of depression in adolescent users of ECs than in those who do not use these products.9–12 Adolescents who have pre-existing depression or depressive symptoms are more likely to begin using ECs, suggesting a bidirectional relationship between depression and EC use.9 An association between suicidality and e-cigarette use has been observed in adolescents, with increased suicide ideation, suicide planning, and suicidal attempts. A higher rate of suicidality has been observed among dual users.10 Lee and Lee examine the relationship between suicidality and depression among Korean adolescents from the 2017 Korean Youth Risk Behavior Web-based Survey. Including a total of 62,276 students, significant differences were found among users where dual (EC and CC) users had a higher prevalence of suicidality and depression for both current and lifetime users. Whereas, EC only users had higher levels of suicidality and depression compared to non-users. Among female adolescents, CC-only and EC-only users, and dual users had a higher prevalence of suicidality and depression as compared to male adolescents. 10,13 Lee and Lee’s study was the first to assess the associations of suicidality and depression to CC and EC use using a nationally representative Korean adolescent sample. The findings suggest that there is an urgent need for the intervention and evaluation of e-cigarette use by healthcare professionals to provide smoking cessation programs for users.10,14 This relationship suggests that while exclusive use of ECs is associated with unfavorable psychological outcomes, its use by current or lifetime conventional smokers can lead to a greater exacerbation of existing symptoms of mental illnesses.
Due to the increase in the use of EC and its impact on mental health, multiple policy changes have been implemented in the United States to mitigate the public health threat. These include increasing the minimum age to buy nicotine-based products including e-cigarettes to 21 years of age, and a ban on the sale of disposable and cartridge-based e-cigarettes with mint, candy, and fruit flavors.19 Also, the use of packaging with highly identifiable logos or cartoon characters has been deemed illegal. However, menthol and tobacco-flavored e-cigarettes and ENDS like open tank vaping systems can still be sold and concerns have been raised that this might lead to teenagers switching to menthol or tobacco flavored pods or even switch to more dangerous and addictive substances. Eliminating the EC from the market might lead to a relapse amongst people who have quit smoking. This could result in a hazardous rise in health issues associated with smoking traditional cigarettes. The implementation warrants new innovative preventive strategies.20,21
The most important prevention strategy is educating the youth about the development of potential mental health effects or deterioration of pre-existing conditions that can result from using EC. A program like “The Real Cost”, an excellent example, was launched by the FDA in 2014 to educate youth on the dangers of tobacco use. The program aggressively prioritized spreading awareness about e-cigarettes to dispel the misconception that e-cigarettes are harmless. Similar campaigns at schools and colleges may help reduce the use of EC and prevent the negative impact on the mental health of adolescents.
Outreach programs via social media can be an effective way to propagate awareness. Primary care physicians including pediatricians should screen the youth on the usage of EC along with the recommended alcohol and drug screens during preventive healthcare visits. The youth must be encouraged to quit the use of vaping devices to avoid dependence on nicotine as a coping strategy. Resources on the symptoms of dependence and withdrawal should be shared with them. Potential breakthrough responses by primary care physicians may be offering insurance discounts for those with negative nicotine testing, conducted regularly. It may also be beneficial for healthcare professionals to receive additional training in motivational interviewing to facilitate change among the population that wishes to quit e-cigarettes.
4.1. Strengths and limitations
Our study is unique as it focuses mainly on the adolescent age group (10–21 years) which is the more vulnerable age group. We included studies carried out in different parts of the world to get a broader perspective on this issue. The main limitation was the restricted number of studies showing the effect of vaping on adolescent mental health. In the included studies, we did not take into account any pre-existing mental health conditions in adolescents to prevent confounding. Another limitation was that we did not consider the frequency of e-cigarette use or the concentration of nicotine because some of the studies had limited data in this regard.
5. Conclusion
This review finds that e-cigarette adolescents are more likely to have mental health problems such as depression and suicidality. The combination of conventional and electronic cigarettes exacerbates these conditions. Also, females develop higher adverse effects on mental health as a result of vaping. To further understand the mechanisms which lead to mental illness in E-cigarette users, more research needs to be done. Although the FDA has taken commendable steps to restrict adolescent access to E-cigarettes, more work needs to be done to identify and close loopholes. We anticipate our review findings to be a critical piece of information for healthcare professionals and public health practitioners.
List of abbreviations
- AOR
Adjusted odds ratio
- CC
Combustible cigarettes
- CI
Confidence interval
- EC
Electronic cigarettes
- EVALI
E-cigarette or vaping use associated lung injury
- FDA
Food and drug administration
Footnotes
Funding
No funding was obtained.
Conflict of interest
All authors declare no conflict of interest.
References
- 1. Arane K, Goldman RD. Electronic cigarettes and adolescents. Can Fam Phys. 2016 Nov;62(11):897–898. [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Outbreak of Lung Injury associated with the use of E-cigarette, or vaping, products. 2020. Retrieved April 22, 2021 from https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
- 3.CDC. Youth e-cigarette use is down, but 3.6 million still use e-cigarettes. 2020. Retrieved April 20, 2021 from https://www.cdc.gov/media/releases/2020/p0909-youth-e-cigarette-use-down.html.
- 4. Jones K, Salzman GA. The vaping epidemic in adolescents. Mo Med. 2020;117(1):56. [PMC free article] [PubMed] [Google Scholar]
- 5. Aberegg SK, Cirulis MM, Maddock SD, et al. Clinical, bronchoscopic, and imaging findings of e-cigarette, or vaping, product use–associated Lung Injury among patients treated at an academic medical center. JAMA Netw Open. 2020;3(11):e2019176–e2019176. doi: 10.1001/jamanetworkopen.2020.19176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC. Quick facts on the risks of E-cigarettes for kids, teens, and young adults. 2021. Retrieved April 16, 2021 from https://www.cdc.gov/tobacco/basic_information/e-cigarettes/Quick-Facts-on-the-Risks-of-E-cigarettes-for-Kids-Teens-and-Young-Adults.html.
- 7. Demissie Z, Jones SE, Clayton HB, King BA. Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics. 2017;139(2) doi: 10.1542/peds.2016-2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews BMJ 2021. 372 n71 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents. Prev Med. 2017;96:73. doi: 10.1016/j.ypmed.2016.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee Y, Lee K-S. Association of depression and suicidality with electronic and conventional cigarette use in South Korean adolescents. Subst Use Misuse. 2019;54(6):934–943. doi: 10.1080/10826084.2018.1552301. [DOI] [PubMed] [Google Scholar]
- 11. Chadi N, Li G, Cerda N, Weitzman ER. Depressive symptoms and suicidality in adolescents using e-cigarettes and marijuana: a secondary data analysis from the Youth Risk Behavior Survey. J Addiction Med. 2019;13(5):362–365. doi: 10.1097/ADM.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 12. Jee Y-J. Comparison of emotional and psychological indicators according to the presence or absence of the use of electronic cigarettes among Korea youth smokers. Int Infor Inst (Tokyo) 2016;19(10A):4525. [Google Scholar]
- 13. Pham T, Williams JV, Bhattarai A, Dores AK, Isherwood LJ, Patten SB. Electronic cigarette use and mental health: a Canadian population-based study. J Affect Disord. 2020;260:646–652. doi: 10.1016/j.jad.2019.09.026. [DOI] [PubMed] [Google Scholar]
- 14. Leventhal AM, Strong DR, Sussman S, et al. Psychiatric comorbidity in adolescent electronic and conventional cigarette use. J Psychiatr Res. 2016;73:71–78. doi: 10.1016/j.jpsychires.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim J, Kim K. Electronic cigarette use and suicidal behaviors among adolescents. J Publ Health. 2019;43(2):274–280. doi: 10.1093/pubmed/fdz086. [DOI] [PubMed] [Google Scholar]
- 16. Bold KW, Morean ME, Kong G, et al. Early age of e-cigarette use onset mediates the association between impulsivity and e-cigarette use frequency in youth. Drug Alcohol Depend. 2017;181:146–151. doi: 10.1016/j.drugalcdep.2017.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jarmul S, Aherrera A, Rule AM, Olmedo P, Chen R, Navas-Acien A. Lost in E-cigarette clouds: a culture on the rise Am J Publ Health 2017. 107 2 265 266 10.2105/AJPH.2016.303463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sun T, Lim CCW, Chung J, et al. Vaping on TikTok: a systematic thematic analysis [published online ahead of print, 2021 Jul 26] Tobac Control. 2021 doi: 10.1136/tobaccocontrol-2021-056619.tobaccocontrol-2021-056619. [DOI] [PubMed] [Google Scholar]
- 19.FDA. FDA finalizes enforcement policy on unauthorized flavored cartridge-based e-cigarettes that appeal to children, including fruit and mint. 2020. Retrieved May 02, 2021 from https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children.
- 20. Adriaens K, Van Gucht D, Declerck P, Baeyens F. Effectiveness of the electronic cigarette: an eight-week Flemish study with six-month follow-up on smoking reduction, craving and experienced benefits and complaints. Int J Environ Res Publ Health. 2014;11(11):11220–11248. doi: 10.3390/ijerph111111220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sarfraz Z, Sarfraz A, Sarfraz M, Pandav K, Michel G. Ripple collision of three epidemics: vaping, opioid use, and COVID-19. Addict Health. 2021;13(4):277–278. doi: 10.22122/ahj.v13i4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]