Abstract
Management of uncontrolled diabetic (DM) patients has always been a challenge across healthcare settings, but recently we noticed a surge in the number of uncontrolled DM patient in our clinic patients’ population during the COVID19 pandemic. This in part a combination of disruptions to care, delayed or inaccessible care, and poor diet and physical activity. To address this issue, we formed a multidisciplinary Diabetes Initiative Team consisting of attending physicians, residents, clinical pharmacist, nurse manager, care manager, and coordinator, along with supportive staffs in our Internal Medicine Residency clinic. Our aim was to reengage diabetic patients in the outpatient setting and to overcome barriers limiting diabetic care.
Keywords: Multidisciplinary diabetes initiative team, Remote continuous glucometer monitoring, COVID-19 pandemic, HbA1C, Uncontrolled diabetes
1. Introduction
The COVID-19 pandemic has been killing people with uncontrolled diabetes at alarming rates. New researches indicate that uncontrolled diabetics are hospitalized four times longer than non-diabetics patient and are four times as likely to die. New barriers to care due to quarantine and social distancing have caused an influx in number of uncontrolled diabetic patients. To battle this crisis, we developed a multidisciplinary Diabetes Initiative Team to address these barriers and revise care delivery during and beyond the pandemic. We reevaluated our previous protocols and redesigned innovative methods and workflows to reduce these new barriers to patient care. Our aim was to get more patients to reengaged in their health, to decrease the cost of out-of-pocket medications for patients, and to improve diabetic control in high-risk patients measurable by a reduction in percentage of patients with A1c > 9%.
2. Method
The Diabetes Initiative Team identified a cohort of all high-risk diabetics in the Internal Medicine Residency Practice in need of intervention. They include those with A1c >9% and those with no A1c within the past year. We reviewed and identified current processes and potential adverse factors likely to worsen during the pandemic. Then we developed novel protocols and redesigned clinic access to address these barriers to care, including those caused by the pandemic. We implemented telehealth visits so our diabetic patients are able to be seen without worrying about contracting the virus. We created dedicated times for patient to get their POC A1c check by RN Care Manager and Clinical pharmacist to avoid waiting to be seen. We provided nutritional counseling, targeted phone calls to our cohort of uncontrolled diabetics, insulin titration, and Remote Continuous Glucometer Monitoring (RCGM). Bi-weekly meetings were set up to discuss progress towards lowering A1c and identifying barriers to ensure ongoing patient progress and continual quality improvement. We also initiated monthly competition between our clinic firms (staff by an attending physician and three residents: intern, second year, and third year) to highlight which firm would have the greatest A1c reduction in their diabetic patients.
3. Results
Faculty:
Resident:
4. Discussion
The study was based on the diabetic patients in the Internal Medicine Residency clinic managed by attendings and residents. Each attending had a dedicated ‘firm’ where they supervised residents during their three years training. During the beginning of the project, in May of 2020, the clinic had a total of 206 diabetic patients, with 30% of these patients with HbA1c > 9.0. In January 2021, we were able to reduce the number of uncontrolled diabetic population down to 26% (219 total diabetic patients).
The first approach was to try to engage the physicians in identifying diabetic patients among their patient panel and focusing specifically on those who were high risk. There were several trainings conducted on how to assist physicians to run their patients ‘ panel list. The uncontrolled diabetic patients were identified and contacted for follow up appointments and to investigate what challenges or barriers they were having in coming for follow up. Firm meetings were held to discuss the updated progress.
It was noted that, attendings tends to have more effective positive change among their diabetic patients compared to the residents. The attendings were more likely to get their patients to follow up for appointments, which is likely due to their long-established relationship with the patients compared to the residents who are rotating out every 3 years. Residents also have more newly diagnosed diabetic patients after they were admitted for diabetic ketoacidosis. Some of the residents’ patients did not have insurance and found cost of medication challenging making them more likely to be noncompliant with their diet and medication regimen.
Barriers such as medication costs were especially focused on. Our dedicated clinical pharmacist and case manager worked to identify patients who found medication cost challenging. They used multiple resources to find the most reasonable and cost-effective way for patients to afford their medications including use of coupons, changing pharmacy or medication formulary. The CGM was found to be useful to remotely monitor patients and titrate their medications. For patients who did not want to do fingerstick frequently, we were able to obtain some donated continuous glucose monitor for them so that they can check their sugar more frequently. Certain patients were also provided with Flow sheets within the EMR MyChart and trained to use so their medications could be titrated. The case manager also provided nutritional education and support to patients in person and virtually.
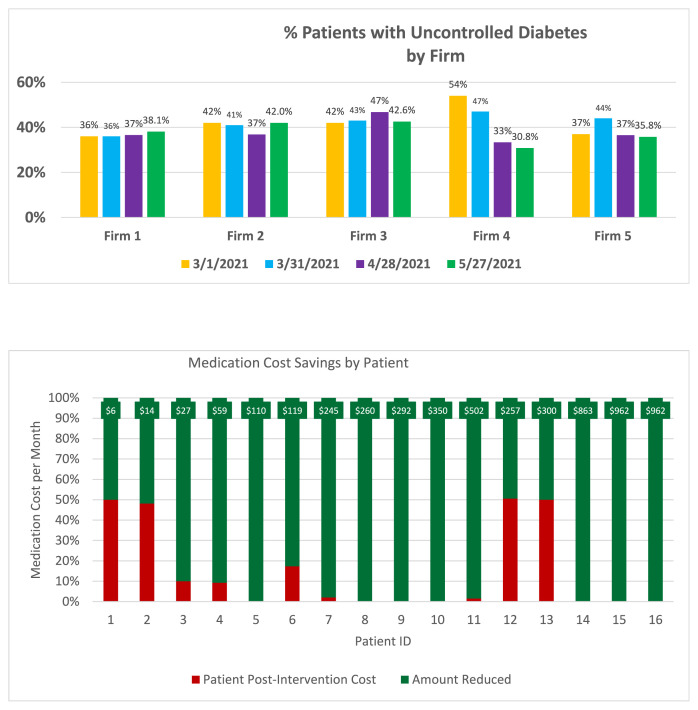
The next step was to further increase engagement and commitment of the providers to the project. Hence, we started a friendly monthly challenge among clinic firms to try to increase motivation for them to keep their diabetic patients at goal. Firm teams with the greatest improvement in diabetes control among their patient populations were identified on a dedicated board in the clinic and awarded with certificate and lunch. This appears to keep the clinic firms more engaged and interested. Firm 4 showed the most decrease in uncontrolled diabetes with decline from 54% of their patient to 30.8%. Firm 1 started off with 36% uncontrolled but increased to 38%. Firm 2 was stable from 42% with moderate decrease but stable at 42%. Similarly Firm 3 averaged to 42%. HbA1C testing hours were extended and flexible to accommodate patient schedules. This enabled us to measure more of our patient A1Cs.
The team was successful based on three key metrics. First, one clinic firm was able to reduce their uncontrolled diabetic patients’ panel by 23% in three months, while we were able to reduce the rate of patients with uncontrolled diabetes by 35% in the attendings’ panel. Second, patients’ median monthly out-of-pocket medication cost decreased from $276 to $4. Finally, the team achieved 100% of the hospital’s annual improvement goal for uncontrolled diabetics in only four months. A control chart indicated the improvement was not due to chance.
There were various reasons why certain firms did not improve compared to the other firms. As an academic center, residents continue to accept new diabetic patients on a continuous basis. One firm might have obtained more newly diagnosed uncontrolled patients compare to the other firms. Other variation might be due to patients’ demographic. Our patients’ population include mixture of ages and races. However, we find that younger patients’ population pose a harder challenge in improving their HbA1c due to non-adherent to medication and follow up rather than medication cost or mobility issue. We did not divide our patients’ panel base on demographic, rather we just based on firm members with a designated attending physician. Therefore, some firms might show improvement while others’ firms either showed no change or increased in percentage of uncontrolled diabetic patients.
5. Conclusion
In conclusion, the aim of the Diabetes Initiative Team was achieved over three months. Patients were more engaged, their out-of-pocket medication costs dropped, and the percentage of uncontrolled diabetics decreased. These results re-energized the Internal Medicine Residency Practice to work towards becoming a nationally recognized center for diabetic care. The study was started in May 2020 and is an ongoing process and continues to evolve. We recognized that diabetes is a chronic disease and like all chronic diseases require continue management. The Internal Medicine Residency Practice is rising to this challenge by adapting the way we deliver care to our patients. We believe that our multidisciplinary approach can be applied to all clinics (both academic and nonacademic). To achieve the goal, it is important to have a dedicated team that is willing to meet biweekly to hold each other accountable. It is also important to have dedicated people (like our clinical pharmacist and RN Care Manager) who would reach out to other pharmacies or companies looking for discounts or alternative versions of the medications for those who cannot afford them. We hope to inspire other resident clinics to implement some of our ideas and perhaps create their own initiative based on their patients’ populations.
Supplementary Information
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.