Abstract
X‐ray regulations and room design methodology vary widely across Canada. The Canadian Organization of Medical Physicists (COMP) conducted a survey in 2016/2017 to provide a useful snapshot of existing variations in rules and methodologies for human patient medical imaging facilities. Some jurisdictions no longer have radiation safety regulatory requirements and COMP is concerned that lack of regulatory oversight might erode safe practices. Harmonized standards will facilitate oversight that will ensure continued attention is given to public safety and to control workplace exposure. COMP encourages all Canadian jurisdictions to adopt the dose limits and constraints outlined in Health Canada Safety Code 35 with the codicil that the design standards be updated to those outlined in NCRP 147 and BIR 2012.
Keywords: diagnostic radiology, medical imaging, occupational dose, radiation safety, shielding
1. INTRODUCTION
Radiation use in Canada is regulated by the Canadian Nuclear Safety Commission (CNSC) and Federal, Territorial, and Provincial governments. Radionuclides, above published exemption amounts, fall under the exclusive jurisdiction of the CNSC. The CNSC issues licenses for the manufacture, acquisition, and use of radionuclides and the standards are uniformly applied across the country. The situation is different for x‐ray‐emitting devices with energies below 1 MeV. Federal agencies authorize the sale, lease, and importation of x‐ray devices, but it is the jurisdiction of the Provinces and Territories to regulate the installation and use of medical x‐ray imaging equipment. Consequently, permitted uses, occupational dose constraints and limits, and shielding design of x‐ray facilities vary across the country. As many jurisdictions are attempting to reduce the legislative burden of radiation safety regulations, the Canadian Organization of Medical Physicists (COMP) conducted a survey in 2016/2017 to provide a useful snapshot of existing variations in rules and methodologies for human patient medical imaging facilities in order to assist jurisdictions to harmonize approaches.
2. BACKGROUND
Canada has adopted the guidelines of the International Commission on Radiological Protection (ICRP) on occupational dose limits for radiation. Starting with the publication of ICRP 261 in 1977, estimates were given of the radiation sensitivities of various organs and tissues (wt ), and the whole‐body dose was considered as the sum of doses to all organs and tissues each weighted for their radiation sensitivities. Publication ICRP 60 (1991)2 improved upon ICRP 26 with better data on radiation sensitivities. Equivalent dose (HR ) was defined as the absorbed dose multiplied by a radiation weighting factor (wR ) related to relative biological effect of a given type of primary radiation. For x‐ray photons of concern here, wR = 1. Effective Dose (E) was defined as the sum of the equivalent dose to each organ or tissue weighted by the relevant radiation sensitivity. ICRP 103 (2007),3 using new data, further refined the tissue sensitivities. The tissue weighting factors from the different ICRP reports are compared in Table 1 and it is noteworthy that these weighting factors change over time as the understanding of the effects of radiation on human biology improves.
Table 1.
Tissue Weighing Factors (wt ) from ICRP26, ICRP60, and ICRP103. The definition and handling of doses to Remainder tissues changed after ICRP26. Remainder tissues for ICRP103 are as follows: adrenals, extrathoracic region, gall bladder, heart, kidneys, lymphatic nodes, muscle, oral mucosa, pancreas, prostate, small intestine, spleen, thymus, and uterus/cervix.
| Tissue or organ | wt | ||
|---|---|---|---|
| ICRP26 (1977) | ICRP60 (1991) | ICRP103 (2007) | |
| Gonads | 0.25 | 0.20 | 0.08 |
| Bone Marrow | 0.12 | 0.12 | 0.12 |
| Colon | – | 0.12 | 0.12 |
| Lung | 0.12 | 0.12 | 0.12 |
| Stomach | – | 0.12 | 0.12 |
| Breast | 0.15 | 0.05 | 0.12 |
| Bladder | – | 0.05 | 0.04 |
| Liver | – | 0.05 | 0.04 |
| Esophagus | – | 0.05 | 0.04 |
| Thyroid | 0.03 | 0.05 | 0.04 |
| Skin | – | 0.01 | 0.01 |
| Bone Surface | 0.03 | 0.01 | 0.01 |
| Brain | – | – | 0.01 |
| Salivary glands | – | – | 0.01 |
| Remainder | 0.30 | 0.05 | 0.12 |
At the time of publication for ICRP 103, the occupational limit for eyes was under review, and ICRP 118 was subsequently published recommending a lower limit for the eyes.4 The recommended stochastic dose limits from ICRP 60, 103, and 118 are shown in Table 2.
Table 2.
Occupational and nonmedical stochastic dose limits from ICRP 60 103, and 118 for planned exposure situations.
| Person | Dose limits | ||
|---|---|---|---|
| ICRP 60 (1991) | ICRP 103 (2007) | ICRP 118 (2012) | |
| Radiation worker (effective dose) | 20 mSv/yr — 5 yr average and not exceeding 50 mSv in one year | 20 mSv/yr—5 yr average and not exceeding 50 mSv in 1 yr | – |
| Pregnant radiation worker | 2 mSv for duration of pregnancy once declared (equivalent dose to the surface of the abdomen) | 1 mSv for duration of pregnancy once declared (effective dose to the fetus) | – |
| Hands and feet of radiation worker (equivalent dose) | 500 mSv/yr (localized exposure) | 500 mSv/yr (averaged over 1 cm2 area of exposed skin) | – |
| Eyes (equivalent dose for occupational worker) | 150 mSv/yr | 150 mSv/yr | 20 mSv/yr— 5 yr average and not exceeding 50 mSv in 1 yr |
| Members of the public (effective dose) | 1 mSv/yr | 1 mSv/yr | – |
2.1. Dose constraints, diagnostic reference levels, and dose limits
A dose constraint is a restriction on the prospective doses to individuals that may result from a defined source of radiation, providing a basic level of protection for a population from planned exposure situations. The dose constraint is often chosen as a level of dose and do not apply to medical diagnosis or treatment. Diagnostic reference levels are similar to dose constraints, but are intended for medical exposure situations. An example of a dose constraint is shielding adjacent spaces of an x‐ray room to planned occupational dose levels. And an example of a diagnostic reference level is the 75th percentile of a distribution of dose indicator values used for a specific patient population for a given diagnostic exam. A dose limit is used for the occupational exposure of individuals, and is a limit of exposure from all occupational sources. Two examples of dose limits are full body exposure limits for radiation workers and eye exposure limits mostly of concern in fluoroscopy guided interventional (FGI) procedures. In both cases, if the annual dose limit is exceeded the individual should be prevented from receiving further occupational exposures for a year. Dose limits do not apply to patients.
2.2. Optimization
The dose limits in Table 2 were set at the limit of unacceptability in ICRP 60, where it was recommended that occupational exposure be kept as low as reasonably achievable (ALARA), taking social and economic considerations into account, in order to avoid exceeding these limits. These values were retained in ICRP 103. In the USA National Council on Radiation Protection & Measurements (NCRP) report 147 it was recommended that the shielding design constraint should be 5 mSv per year for radiation workers and 1 mSv for the general public.5
In the United Kingdom (UK), the National Radiological Protection board recommends that for optimization purposes the dose constraint should not exceed 30 % of the dose limit.6 This recommendation is in line with ICRP, which also recommends an occupational dose constraint of ≤20 mSv/yr.3 From personnel dosimetry it was found that the average dose to UK radiology technologists was 0.06 mSv/yr. As a result, the annual dose constraint of 0.3 mSv was adopted for workers in the shielding design of x‐ray facilities, as this dose constraint was already being met.6
2.3. Radiation shielding design
NCRP 49, published in 1976,7 was the main guide to x‐ray shielding in North America until the publication of NCRP 147 in 2004. NCRP 49 was essentially the same as NCRP 348 first published in 1970. In the late 1980s, NCRP 49 came under a lot of criticism for lacking important information and being overly conservative, including9:
No information on modalities such as computed tomography (CT), mammography, and digital imaging.
Attenuation data were not applicable to three phase or constant potential generators.
Typical mAs workloads were no longer valid due to the use of newer high speed rare‐earth film/screens.
The use factors and occupancy factors appeared to be unrealistically high.
Shielding was specified using half‐value‐layers (HVLs) of Pb or concrete required to attenuate scattered and primary radiation to designed levels, and the requirement to “add‐one‐HVL” was considered overly‐conservative.
The requirement to cover screws or nails with Pb tabs was questioned.
Funding and other issues, however, hampered the publication of a new shielding guide until 2004. The shielding design recommendations of NCRP 147 addressed most of the shortcomings of NCRP 49 listed above. Instead of a formulaic approach to the calculation of primary, scatter, and leakage radiation, NCRP 147 lists actual field measurements for typical radiological examinations. Extensive attenuation data are given which can easily be incorporated in a spreadsheet or other software. Workload data are also taken from actual surveys across the USA. One paper that compared shielding design using NCRP 49 and NCRP 147 showed that NCRP 49 methodology overestimated the required thickness of Pb by up to 50%.10
NCRP 147 is not without criticism, however, including concerns about tertiary radiation scattered from the ceilings of CT and angiography rooms into control areas.11 For high workload rooms the dose to staff in adjacent rooms can exceed several mSv/yr.11
The British Institute of Radiology’s (BIR) Radiation Shielding for Diagnostic x‐rays published in 200012 and updated in 20126 uses a different approach to shielding calculation compared to the NCRP. Primary barriers are calculated assuming a standard dose is required at the detector whether this be film, computed radiography, or direct digital radiography. Scattered radiation barriers for radiography and FGI systems are calculated using a formula relating scattered dose to the tube voltage and dose indicator Kerma Area Product. Scatter in CT rooms is calculated from the dose indicator Dose Length Product for studies performed in the room. The 2012 version of the guide also covers tertiary scatter from ceilings and labyrinths. It is of interest that leakage radiation was considered a prominent type of radiation in NCRP 49 but is in fact completely ignored in the BIR publications.
In federal workplaces, Health Canada Safety Codes play an important role in radiation safety. Overall, federal departments are regulated by the Canada Labour Code (CLC) which includes requirements addressing workplace health and safety. More explicitly, promulgated under the CLC, the Canada Occupational Health and Safety Regulations (COHSR) set out the requirements of an employer, where a device that is capable of producing and emitting energy in the form of ionizing or nonionizing radiation is used in the workplace. Under the COHSR regulations, the requirement to implement prescribed safety codes (and safety standards) is outlined (Section 10.26, Note 1). Thus, Health Canada Safety Codes are primarily for the instruction and guidance of persons employed by federally regulated employers, or those under the jurisdiction of the CLC, and they are not themselves regulations, they are guidance documents; however, they can and do become a regulatory requirement when incorporated by reference into other regulations or acts — federal, provincial, or territorial.
Safety Code (SC) 20A13 was first published in 1976. Safety Code 20A was mainly concerned with safety procedures for the installation, use, and control of x‐ray equipment. It had limited sections on the x‐ray output parameters. Only film processor quality control was defined in any detail.
Safety Code 35 (2008)14 is a vast improvement on the former Code, and COMP endorses the provincial and territorial adoption of this code into jurisdictional regulations and accreditation agencies.15 Safety Code 35 includes comprehensive safety requirements for the installation, use, and control of all x‐ray equipment (except mammography equipment covered in SC 36,16 dentistry equipment covered in SC 30,17 and bone mineral density equipment). There is increased emphasis on patient dose and much of SC 35 is concerned with quality control (QC) of digital imaging systems. Unfortunately, although SC 35 explicitly states that radiation shielding should be designed using the methods of NCRP 147, an Appendix has a summary of NCRP 49 which was retained from SC20A at the request of some provincial radiation protection authorities for their reference.
3. MATERIALS AND METHODS
3.1. How the survey was conducted
The Canadian Organization of Medical Physicists endeavored to capture existing rules and methodologies for human patient medical imaging facilities. Participants from the COMP Imaging Committee, and their contacts representing every Province and Territory, were invited to provide information on the regulations governing the use of x‐rays, as well as related dose limits and constraints. The survey was performed in November 2016 and includes human patient medical imaging facilities only, and excludes installations within penitentiaries (Correctional Services Canada), Department of National Defence, First Nations and Inuit Health Branch and other federally regulated facilities.
3.2. Health Canada national dose registry data
Radiography occupational dose information was provided by Health Canada's National Dose Registry for the years 1990–2016, broken down by province and territory. Health Canada has published a report containing these data for Medical and other job sectors.18
4. RESULTS AND DISCUSSION
4.1. Regulations in each province/territory
Table 3 provides a summary of the provincial and territorial acts and regulations. All provinces and territories have x‐ray Acts and/or Regulations in place except New Brunswick, Nova Scotia, and Prince Edward Island. In New Brunswick the Radiological Health Protection Act was repealed in 2007. In Prince Edward Island The Radiation Safety Regulations were revoked on August 1, 2016, which COMP strongly opposed.19
Table 3.
Provincial and territorial acts and regulations.
| Province or territory | Regulations regarding radiation safety |
|---|---|
| Alberta | Radiation Protection Regulations (2003) under the Radiation Protection Act http://work.alberta.ca/occupational-health-safety/radiation-legislation.html |
| British Columbia | WorkSafeBC, College of Physician and Surgeon’s Diagnostic Accreditation Program. WorkSafeBC is obliged under their Regulations to enforce all Health Canada Safety Codes. https://www.worksafebc.com/en/law-policy/occupational-health-safety/searchable-ohs-regulation/ohs-regulation/part-07-noise-vibration-radiation-and-temperature; https://www.cpsbc.ca/programs/dap |
| Manitoba | The Radiation Protection Act. Regulations being drafted https://web2.gov.mb.ca/bills/40-4/b037e.php |
| New Brunswick | No regulations |
| Newfoundland and Labrador | Radiation Health and Safety Regulations under the Radiation Health and Safety Act (2003) |
| Northwest Territories and Nunavut | Occupational Health & Safety regulations, Part 23, Sections 339‐363 |
| Nova Scotia | No regulations |
| Ontario | Healing Arts Radiation Protection Act, Ontario Regulation 543 and Regulation 861‐90 under the Occupation Health and Safety Act for workers |
| Prince Edward Island | No regulations |
| Quebec |
Loi sur la santé publique Loi sur les services de santé et services sociaux Loi et Règlement sur les laboratoires médicaux, la conservation d’organes et les tissus et la disposition des cadavres Loi sur la santé et la sécurité du travail (RLRQ, chapitre S‐2.1) et son Règlement d’application. |
| Saskatchewan | The Saskatchewan Employment Act and The Radiation Health and Safety Regulations, 2005. |
| Yukon | Yukon Occupational Health and Safety Act. |
In most provinces and territories, x‐rays are regulated under Labour or Health legislation and implementation and/or enforcement is performed by the provincial/territorial occupational health and safety departments, such as WorkSafeBC in British Columbia and Ministry of Labour Relations and Workplace Safety in Saskatchewan, for examples. In Manitoba x‐ray Inspectors have a letter of appointment from Minister of Health.
4.2. Dose limits
As shown in Table 4, many jurisdictions use the annual dose limits from SC 20A; that is, 50 mSv for x‐ray workers, 1 mSv for the public, and 4 mSv for the remainder of a pregnancy following declaration. A few provinces have adopted the more recent 20 mSv for radiation workers from SC 35, and some jurisdictions have no limits due to the lack of regulations. For jurisdictions without regulations, institutions or authorities usually set their own limits as best practice, but there is a risk they might not.
Table 4.
Provincial and territorial breakdown of dose limits.
| Province or territory | Dose limits | ||
|---|---|---|---|
| X‐ray Worker (mSv/yr) | General public (msv/yr) | Pregnant worker (mSv) c | |
| Alberta | 50a | 1 | 4 |
| British Columbia | 20 | 1 | 4 |
| Manitoba | 20 | 1 | 4 |
| New Brunswick | NA | NA | NA |
| Newfoundland and Labrador | 50 | 5 | 5 |
| Northwest Territories and Nunavut | 50a | 1 | 4 |
| Nova Scotia | 20 | 1 | 4 |
| Ontario | 50 | 1b | 5 |
| Prince Edward Island | NA | NA | NA |
| Quebec | 50a | 1 | 4d |
| Saskatchewan | 50a | 1 | 4 |
| Yukon | NA | NA | NA |
NA = not available.
With an additional 5‐yr cumulative dose limit of 100 mSv.
5 mSv for other workers (non‐x‐ray).
For the remainder of the pregnancy.
Could be 2 mSv or lower depending on the designated regional occupational health physician.
4.3. Shielding of x‐ray facilities
No two provinces or territories have the same standards for the shielding of x‐ray facilities, as shown in Table 5. The responsibility for designing and subsequently verifying shielding installation varies widely, from being the responsibility of the owner (e.g., private clinics in Alberta), to a dedicated radiation protection group within government or the health care sector (e.g., CancerCare Manitoba). In some jurisdictions design templates are available (e.g., from the Radiation Safety Unit in Saskatchewan and the Centre for Disease Control in British Columbia, although the British Columbia entity no longer provides this service) and for rooms that do not satisfy the template criteria, other experts, such as those listed in Table 5 are used.
Table 5.
Shielding design personnel by province and territory for radiological x‐ray, fluoroscopy, and computed tomography (CT) rooms.
| Province or territory | Allowed to perform shielding design | Approves shielding design | Visual inspection required? | Scatter survey required after construction complete? |
|---|---|---|---|---|
| Alberta | Not Regulated | N/A | Yes. By ARPA inspector who did not design the room shielding | Yes. By an ARPA inspector who did not design the room shielding |
| Alberta Health Services | Medical physicists who are also Authorized Radiation Protection Agency (ARPA) inspectors | N/A | Yes. By ARPA inspector who did not design the room shielding | Yes. By an ARPA inspector who did not design the room shielding |
| British Columbia | “trained individuals with current in‐depth knowledge of structural shielding design” Note9 | Not applicable | No | Yes |
| Manitoba | Radiation Protection Officers (with appointment as x‐ray Inspector)/Radiation Safety specialist | CCMB Radiation Protection Group ‐ Radiation Protection Officers (with appointment as X‐ray Inspector)/ designated CCMB Health Physicist or CCMB Medical Imaging Physicist | Yes (photo record kept) |
No Sometimes performed in special circumstances |
| New Brunswick | Not regulated. Usually performed by medical physicist hired on contract | Not regulated. Usually performed by medical physicist hired on contract | No | No |
| Newfoundland and Labrador | Manufacturer, Medical Physicist, Engineer, etc | Compliance and Regulatory Affairs Officers, Occupational Health and Safety, Service NL | No | Yes |
| Northwest Territories and Nunavut | None specified | Chief safety Officer | No | No |
| Nova Scotia | Performed by Medical Physicist, not regulated | Typically Medical Physicist, not regulated | No | No |
| Ontario | Qualification not specified but in practice by someone approved by the Radiation Protection Service of Ontario | X‐ray Inspection Service via BCEP | No | No |
| Prince Edward Island | Medical Physicist | Medical Physicist | Yes | Yes |
| Quebec | Engineer; if necessary with the help of a qualified physicist |
Private facilities: Laboratoire de Santé Publique du Québec (LSPQ) Public Facilities: no mandate; this falls the under engineer responsibilities when they stamp and seal a design |
Private facilities: Yes Public Facilities: Yes |
Private facilities: Yes, with report to LSPQ Public Facilities: Yes |
| Saskatchewan | Shielding Consultant if requirements outlined in shielding manual can’t be met | Radiation Safety Unit | No | No |
| Yukon | Not specified | X‐ray inspector on behalf of Director | Yes | No |
In some jurisdictions shielding designs falls under the purview of engineers. Engineers Canada publishes national guidelines on the practice of engineering in Canada, with input from all provincial and territorial associations, which may be adopted in part, in whole, or not at all by engineering regulators in Canada. This organization defines the practice of engineering as “any act of planning, designing, composing, evaluating, advising, reporting, directing or supervising, or managing any of the foregoing, that requires the application of engineering principles and that concerns the safeguarding of life, health, property, economic interests, the public welfare or the environment.” Note 2 This definition is circular, defining engineering as applying engineering principles (although the French pages are more specific Note 3). Alberta, Note 4 and Newfoundland and Labrador, Note 5 more specifically define the practice of engineering as “the principles of mathematics, chemistry, physics or any related applied subject” and Prince Edward Island has similar wording, Note 6 whereas Quebec considers the field of practice to include works using “processes of applied chemistry or physics.” Note 7 In practice, most jurisdictions do not formally require an engineer’s oversight for a shielding design, with the exception of Quebec and Ontario. As part of any engineering design work, field reviews are required, which include visual inspections and scatter surveys in Table 5. Consequently, with regards to Table 6, an engineer is not obligated to use only specific design documents permitted by regulations or accreditation agencies, but are expected to use any and all methodologies that would be considered good practice and obvious to peers performing similar design work.
Table 6.
Presently allowed shielding design methodologies.
| Province or territory | NCRP 49 (1976) | BIR (2000) | NCRP 147 (2004) | BIR (2012) | Other (list)/notes |
|---|---|---|---|---|---|
| Alberta | X | X | |||
| British Columbia | X | X | BC Centre for Disease Control has some standard templates that can be used. | ||
| Manitoba | X | X | |||
| New Brunswick | Unregulated | ||||
| Newfoundland and Labrador | X | X | CNSC GD‐ 52 used in part for PET/CT and SPECT/CT | ||
| Northwest Territories and Nunavut | Not regulated but recommended NCRP 147 | ||||
| Nova Scotia | Unregulated. Nova Scotia Health Authority uses NCRP 147 | ||||
| Ontario | X | Health Canada Safety Code 20A | |||
| Prince Edward Island | Unregulated. Health PEI uses NCRP 147 | ||||
| Quebec | X | X | X | X | Safety Codes 30 and 35 |
| Saskatchewan | X | X | The Government of SK has some standard templates that can be used in their Shielding Manual. | ||
| Yukon | “Recommended Safety Procedures for Installation and Use” published by the Department of National Health and Welfare. Generally, employers voluntarily comply with current industry best practice |
As shown in Table 6, for all provinces with regulations, except Ontario, NCRP147 is identified as the main source of information for the design of x‐ray shielding. In Ontario, assuming a radiographic detector has a certain Pb equivalency as suggested by NCRP 147 has to be approved by the x‐ray inspection service. Many provinces also use BIR2000 and BIR2012 which also provide information on dental, BMD, SPECT/CT, and PET/CT installations. The x‐ray Inspection Service (XRIS) of the Ontario Ministry of Health and Long Term Care has advised that room shielding calculation should use the methodology specified in Safety Code 20A, even though the preamble of Safety Code 35 clearly indicates that it replaces the former code. However, there are two exceptions to this recommendation:
For the recommended dose limits of ionizing radiation, XRIS is not following the limits published in SC20A (1999 printing), instead the limits published in the 1981 version are followed.
Figure 2 of SC20A, which plots the attenuation in concrete of x‐rays generated at 50 to 300 kVp, has a typographical error in the labeling of the x‐axis where the thickness of concrete should be in centimeters instead of millimeters.
Figure 2.
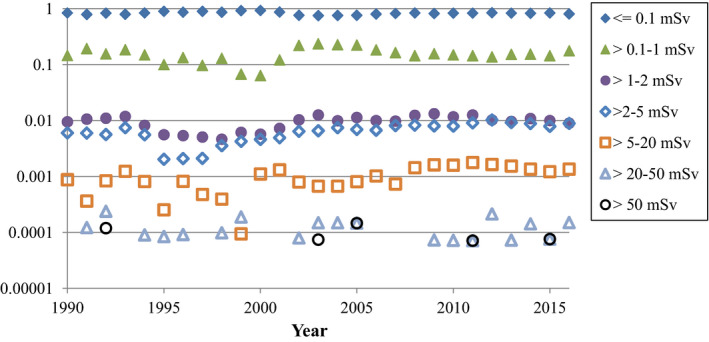
Fraction of Canadian radiography workers receiving different ranges of annual occupational dose. Note the log scale on the y‐axis. Years where there were zero workers for a specific range are not shown on the log scale graph.
In the time since the survey was conducted, the province of Ontario has repealed the Healing Arts and Protection (HARP) Act with the Oversight of Health Facilities and Devices Act as part of Bill 160, Strengthening Quality and Accountability for Patients Act.20 At the time of writing, the Medical Radiation and Imaging Technology Act (2017) is in the consolidation period and not yet in force. Note 8 The Canadian Organization of Medical Physicists strongly supported the modernization of the Ontario Healing Arts Radiation Protection Act21 and contributed as a stakeholder in the Health Quality Ontario report on this topic.22
There is a wide range of annual dose constraints used for the design of shielding, as shown in Table 7. For x‐ray workers, where there are regulations, the range is 1 to 50 mSv, and the range for the General Public is 1 to 5 mSv. It is also interesting to note that the constraints and dose limits (Table 4) are often different. An appropriate and conservative approach, and one recommended by the authors of this paper who perform shielding design, is to set a shielding design goal of 1 mSv for all cases, allowing future use of adjacent spaces to change without the need to change shielding, for example, if an office fully occupied by a radiation worker becomes office space for a nonradiation worker (general public).
Table 7.
Dose Constraints used in the different provinces and territories for radiation protection shielding.
| Province or territory | Dose constraints | |
|---|---|---|
| X‐ray worker (mSv/y) | General public (mSv/y) | |
| Alberta | 20 | 1 |
| Alberta Health Services | 1 | 1 |
| British Columbia | 1 | 1 |
| Manitoba | 1 | 1 |
| Newfoundland and Labrador | 20 | 2 |
| New Brunswick | NA | NA |
| Northwest Territories and Nunavut | 50 | 1 |
| Nova Scotia | 5 | 1 |
| Ontario | 50 | 5 |
| Prince Edward Island | NA | NA |
| Health PEI | 20 | 1 |
| Quebec | 1a | 1a |
| Saskatchewan | 20 | 1 |
| Yukon | 50 | NA |
Not directly indicated but explicitly implied by good practice in an engineering sense.
4.4. Radiographer occupational exposures 1990–2016
The average and median annual occupational dose for radiographic technologists in Canada are shown in Fig. 1. The average value for 2016 is approximately 0.10 mSv/yr and the median value is zero. Technologists working in FGI procedures, who typically experience higher occupational exposures, were not separated from technologists exclusively working in general radiography. The Canadian average is slightly higher than the UK radiographer average value of 0.06 mSv/yr.6 It appears that the BIR recommendations to use a dose constraint of 30% of the dose limit (or 0.3 mSv) would also be applicable to Canadian practice, since this constraint level is already achieved, especially considering the measured values reported here include staff who are exposed to workplace radiation without protection from structural shielding, including technologists who work in FGI procedures.
Figure 1.
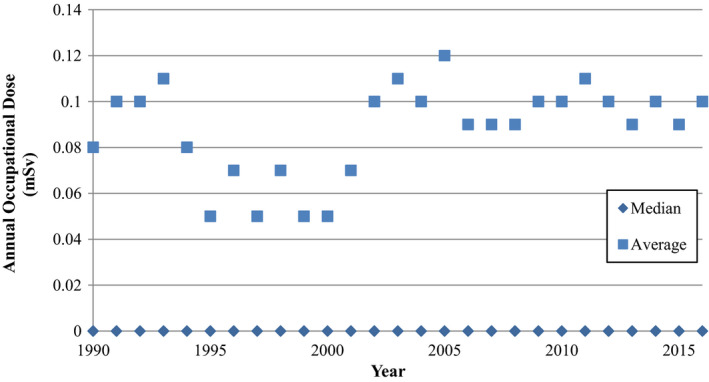
Average and median annual occupational dose for radiographers in Canada. All median values are zero.
A breakdown of radiographer occupation exposure by different dose ranges is shown in Fig. 2. The vast majority of workers receive doses below detectability on their badges (represented as <=0.1 mSv on the graph, although newer badges with technology that measures 0.01–0.1 mSv are also included here). The total number of workers whose doses are reported here are 8000 in 1990, increasing to 13 300 by 2016.
While not apparent in the Figures, it is the experience of the authors that general medical imaging technologists rarely register a reading on their dosimeters. In contrast, FGI workers occasionally experience small doses. It is also noteworthy that some nonzero badge readings reported to Health Canada are not accurate in terms of actual staff occupational exposure. For example, if a radiographer has an anomalous reading exceeding 0.25 mSv/quarter on their badge, most jurisdictions will perform an investigation as to the cause. Sometimes the cause is not explained and such higher readings never show up again with that worker. However, since most jurisdictions allow 20 mSv/yr for radiation workers, if the investigators deem it unlikely that the worker's badge readings will exceed this limit for a year even with a high erroneous badge reading, they do not bother issuing a correction to the National Dose Registry. Similar high readings can also be a result of accidental workplace exposure to a group of badges, and again, the investigators might not correct the National Dose Registry records if not doing so has no repercussions to the site or staff member.
An interesting discovery arising from the author correspondence for this work is that some facilities issue a single badge to FGI staff that is to be worn on top of the apron, which is common practice in the United States23, 24 but uncommon in Canada and not the practice suggested by SC35.14 The ICRP recommends two dosimeters be worn—one above the apron at neck level and one under the protective apron for FGI work.25 The NCRP recommends both practices but does not recommend a single dosimeter under the apron for FGI work.24 For one set of facilities in Canada where they issue a single badge to FGI workers to be worn on top of the apron, we confirmed that from 2008 to 2016, the collar badge readings are being reported as whole‐body readings (occupational dose) with the National Dose Registry. Such practice can routinely result in badge readings exceeding 20 mSv while the true occupational dose is a fraction of this. We verified that at least some of the high “occupational dose” readings in Fig. 2 are not representative of actual occupational dose received by radiography workers.
Another interesting finding is that badging practices vary across Canada. Many jurisdictions require all general duty x‐ray staff to wear a badge in order to demonstrate their workplace exposure does not exceed regulatory limits. In some jurisdictions, since the aforementioned approach showed these staff always received less workplace exposure than what is allowed for the general public (1 mSv/yr), not all staff are routinely badged. A single or handful of full time employees wear dosimeters in order to ensure compliance with dose limits, whereas the rest of the staff wears the dosimeter for the first 6 months and if their workplace exposure is well below 1 mSv/yr they are no longer issued a dosimeter unless the staff member requests it. In such jurisdictions staff working in FGI work still wear dosimeters as do general duty pregnant staff.
Box plot distributions of average occupational dose from 1990 to 2016 by province/territory are shown in Fig. 3, and all median values for each year were reported as zero. However, the true value is more accurately reported as <0.1 mSv, since the minimum reporting values for different badge technologies is 0.1 and 0.01 mSv, and measurements less than these values are reported as zero to Canada’s National Dosimetry Registry.
Figure 3.
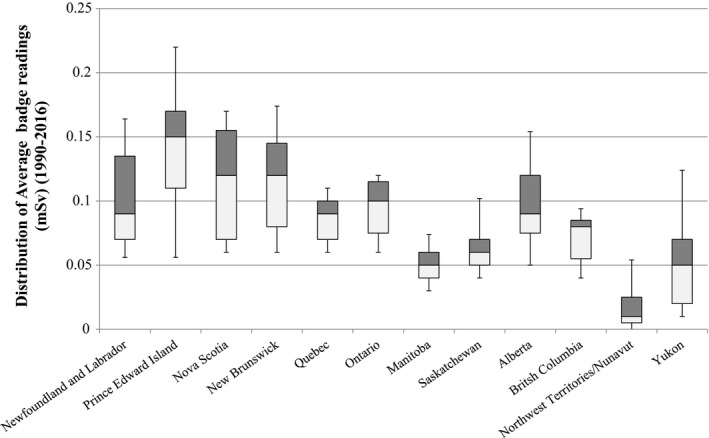
Distribution of average occupational dose badge readings by province/territory for 1990–2016. Box and whisker plot shown with central horizontal line representing the median value, the upper and lower limits of the box are the 25th and 75th percentiles, and the extent of the whiskers are the 10th and 90th percentiles.
At the time of writing, Newfoundland and Labrador is presently reviewing their radiation safety legislations and the supporting regulations, whereas Ontario and Manitoba are in the final stages of their processes. Ontario’s higher shielding specifications are based on SC 20A which follows NCRP49 requirements, and Pesianian et al have shown thicker Pb would be specified for shielding designs based on NCRP49 when compared to NCRP14710 at greater economic expense. In Newfoundland and Labrador, while not specified in the current regulations, the Minister is referencing Safety Code 35 for inspection standards and exposure limits. There is no explicit distinction between diagnostic x‐ray personnel and nuclear medicine personnel in terms of permissible exposure, but the latter of course are monitored under the CSNC regulations. In practice, it is the experience of these authors that x‐ray radiation workers rarely exceed an occupational exposure of 1 mSv/yr, whereas a nuclear medicine radiation worker has a much higher probability of doing so.
5. CONCLUSIONS
In the interests of public safety and to control workplace exposure, it would be useful for different jurisdictions in Canada to adopt a harmonized approach, by implementing uniform dose limits and constraints outlined in Safety Code 35 with the codicil that the design standards are updated to those outlined in NCRP 147 and BIR 2012.
Conflict of Interest
All authors have no conflict of interest to declare.
Acknowledgments
The authors thank Monika Kumala, Narine Martel, Graeme Wardlaw, Richard Smith, and Gary Hughes.
Notes
http://laws.justice.gc.ca/eng/regulations/SOR-86-304/page-26.html#h-126 (accessed 2018.12.18)
https://engineerscanada.ca/publications/public-guideline-on-the-practice-of-engineering-in-canada#-defining-the-engineering-profession (accessed 2019.04.02, last updated 2012.02)
https://engineerscanada.ca/fr/definition-de-lexercice-de-la-profession-dingenieur (accessed 2019.04.02, last updated 2016.04.30)
http://www.qp.alberta.ca/documents/Acts/E11.pdf (accessed 2018.12.18, last updated 2015.04.30)
https://www.assembly.nl.ca/legislation/sr/annualstatutes/2008/e12-1.c08.htm (accessed 2018.12.18, last updated 2008.12.18)
https://www.princeedwardisland.ca/sites/default/files/legislation/E-08-1-Engineering%20Profession%20Act.pdf (accessed 2018.12.18, last updated 2018.06.12)
http://legisquebec.gouv.qc.ca/en/ShowDoc/cs/I-9 (accessed 2018.12.18, last updated 2016.01.28)
https://www.ontario.ca/laws/statute/17m25 (accessed 2019.04.02, last updated 2017.12.12).
Diagnostic Accreditation Program of British Columbia. Accreditation standards 2014 – Diagnostic Imaging. Standard RS6.1.5.
REFERENCES
- 1. International Commission on Radiological Protection . ICRP publication 26: recommendations of the international commission on radiological protection. Ann ICRP. 1977;1-80. [DOI] [PubMed] [Google Scholar]
- 2. International Commission on Radiological Protection . ICRP publication 60: 1990 recommendations of the international commission on radiological protection. Ann ICRP. 1991;21:1–201. [PubMed] [Google Scholar]
- 3. International Commission on Radiological Protection . ICRP publication 103: the 2007 recommendations of the international commission on radiological protection. Ann ICRP. 2007;37:1–332. [DOI] [PubMed] [Google Scholar]
- 4. International Commission on Radiological Protection . ICRP publication 118: ICRP statement on tissue reactions/early and late effects of radiation in normal tissues and organs – threshold doses for tissue reactions in a radiation protection context. Ann ICRP. 2012;41:1–322. [DOI] [PubMed] [Google Scholar]
- 5. National Council on Radiation Protection and Measurements . NCRP Report 147: Structural Shielding Design for Medical X‐ray Imaging Facilities; 2004.
- 6. Sutton DG, Martin CJ, Williams JR. Radiation Shielding for Diagnostic Radiology, 2nd edn. London: British Institute of Radiology; 2012. [Google Scholar]
- 7. National Council on Radiation Protection and Measurements . NCRP Report 49: Structural Shielding Design and Evaluation for Medical Use of X‐Rays and Gamma‐Rays up to 10 MeV; 1976.
- 8. National Council on Radiation Protection and Measurements . NCRP Report 34: Medical X‐Ray and Gamma‐Ray Protection for Energies up to 10 MeV—Structural Shielding Design and Evaluation; 1970.
- 9. Archer BR. History of the shielding of diagnostic x‐ray facilities. Health Phys. 1995;69:750–758. [DOI] [PubMed] [Google Scholar]
- 10. Pesianian I, Mesbahi A, Shafaee A. Shielding evaluation of a typical radiography department: a comparison between NCRP reports No.49 and 147. Iran J Radiat Res. 2009;6:183–8. [Google Scholar]
- 11. Martin CJ, Sutton DG, Magee J, McVey S, Williams JR, Peet D. Derivation of factors for estimating the scatter of diagnostic x‐rays from walls and ceiling slabs. J Radiol Prot. 2012;32:373–396. [DOI] [PubMed] [Google Scholar]
- 12. Sutton DG, Williams JR. Radiation Shielding for Diagnostic X‐rays: Report of a joint BIR/IPEM Working Party. London, England: British Institute of Radiology; 2000. [Google Scholar]
- 13. Health Canada . Safety Code 20A: X‐ray Equipment in Medical Diagnosis Part A: Recommended Safety Procedures for Installation and Use. Canada: Minister of Health Canada; 1999.
- 14. Health Canada . Safety Code 35: Radiation Protection in Radiology ‐ Large Facilities. Canada: Minister of Health Canada; 2008.
- 15. Canadian Organization of Medical Physicists . Position Statement: Safety Code 35 [updated December 10, 2013‐July 9, 2019]. Available from http://www.comp-ocpm.ca/download.php?xml:id=379
- 16. Health Canada . Safety Code 36: Radiation Protection and Quality Standards in Mammography: Ministry of Health Canada; 2013.
- 17. Health Canada . Safety Code 30: Radiation Protection in Dentistry: Ministry of Health Canada; 2000.
- 18. Health Canada . 2017 Report on Occupational Radiation Exposures in Canada: Minister of Health, Canada; 2018.
- 19. Canadian Organization of Medical Physicists . Response to the Repeal of PEI’s Public Health Act Radiation Safety Regulations [updated 2016July 9, 2019]. Available from http://www.comp-ocpm.ca/download.php?xml:id=1097.
- 20. Bill 160: An Act to amend, repeal and enact various Acts in the interest of strengthening quality and accountability for patients; 2017.
- 21. Canadian Organization of Medical Physicists . COMP Comment on the HARP Act Renewal Process [updated October 9, 2015‐July 9, 2019]. Available from http://www.comp-ocpm.ca/download.php?xml:id=735
- 22. Health Quality Ontario . Report and Recommendations on Modernizing Ontario's Radiation Protection Legislation. Ontario, Canada; 2016.
- 23. National Council on Radiation Protection and Measurements . NCRP Report 122: Use of Personal Monitors to Estimate Effective Dose Equivalent and Effective Dose to Workers for External Exposure to Low‐LET Radiation; 1995.
- 24. National Council on Radiation Protection and Measurements . NCRP Report 168: Radiation Dose Management for Fluoroscopically‐Guided Interventional Medical Procedures; 2012.
- 25. López PO, Dauer L, Loose R, et al. ICRP Publication 139: occupational radiological protection in interventional procedures. Ann ICRP. 2018;47:1–118. [DOI] [PubMed] [Google Scholar]


