Summary:
Community leaders collaborated with human-centered design practitioners and academic researchers to co-develop a community health worker (CHW) training program for delivering community-based hearing care to fellow older adults. When implemented by CHWs, clients’ communication function improved comparably with outcomes following professional interventions. Community-based models offer opportunities to advance hearing health.
Keywords: Hearing loss, presbycusis, community health worker, health equity, health disparities, aural rehabilitation, human-centered design, social design, community engagement, community-delivered hearing care, older adults, healthy aging
Age-related hearing loss is highly prevalent and independently associated with multiple adverse outcomes, including incident dementia and accelerated cognitive decline.1,2 However, relatively few older adults receive treatment. The overall rate of hearing aid use remains low in the United States (estimated 14–33% of total candidates) and disparities are observed across low socioeconomic and racial/ethnic minority groups, with rates of hearing aid use among minority older adults approximately half of that observed among non-Hispanic White counterparts.1,3,4 Recent national calls for action to address hearing health disparities as a public health priority include recommendations for expanding the accessibility and affordability of care through community-based delivery models that incorporate task sharing, such as community health worker (CHW) models.1
Hearing aids are predominantly acquired through clinic-based settings and are associated with high out-of-pocket costs.1,4 With the anticipation of over-the-counter (OTC) hearing aids entering the consumer market in 2021,5 hearing care delivery models that connect older adults, particularly at-risk populations, to needed technology are critical. We describe a first-in-kind curriculum developed through transdisciplinary collaboration to train older adult lay community members as interventionists to deliver hearing care with OTC technology.
HEARS: A Community-Delivered Hearing Care Program
The Hearing Health Equity through Accessible Research and Solutions (HEARS) program is a theory-driven hearing care intervention designed to be delivered by trained CHWs that targets traditional barriers in accessing clinic-based hearing care.6 Clients audiometrically screened for hearing loss through remote tablet-based technology7 receive a personalized program across two days (totaling an estimated 2–2.5 hours) within their community settings. The program incorporates education around goal setting for clients, such as improving ability to follow spoken conversations. Clients also receive an introduction to age-related hearing loss and lessons on applying communication strategies to address situational listening challenges. Finally, the CHW provides instruction and support for appropriately using an OTC amplification device that a client selects following a brief orientation.6
The program is delivered by trained CHWs who follow a structured series of program manuals.6 Each manual, along with features of the CHW training program, were developed following several guiding principles (Box 1), including human-centered design (HCD) (Figure 1).8 The ultimate goal was to develop program materials that are accessible and usable by older adults, both the CHWs and clients.9
Box 1. DESIGN PRINCIPLES FOR ENHANCING ACCESSIBILITY BY OLDER ADULTS.
Hierarchy: The most important information should be dominant visually for effi cient page orientation
Each page should host limited tasks/concepts to avoid cognitive overload
Limit excessive texts and elements to support selective attention
Layout: Use clean and consistent layouts to avoid overwhelming the audience who are learning new content
Print page titles in the same location throughout, except on the main cover and subcover pages
A table of contents in the beginning helps prepare the audience’s expectations accordingly
Subcover pages signal a shift in topics and help orient the audience for processing content effi ciently
Maximize the use of white space for visual breaks; this minimizes risks of cognitive overload
Iconography: Designs familiar in styles such as those seen in public places convey information effi ciently
Curved lines and edges are less harsh visually and promote a more casual, inviting, and relaxed setting
Use symbol icons throughout to help navigate the audience’s attention and support procedural memory
Font: Use large font sizes (14 point and above) for visual accessibility
Use 90% black color to maintain high contrast against white backgrounds while avoiding the jarring visual effect of 100% black
Select a font that is sans-serif with simple curved lines, which promotes a friendly and casual setting
Bold letters in titles help draw attention first; use bolded texts for accentuating vital information, but avoid distracting the audience through overuse
Avoid capitalizing all letters, which creates a perception of yelling, except in logos or to highlight important points
Crowded texts may be overwhelming and cultivate anxiety; allow significant white space between lines of texts for “visual breaks”
Colors: Avoid yellow, green, and blue in close proximity as differentiating these become more difficult in age
Increasing color contrasts between texts, graphics, and background provide better visual accessibility
Colors should be at mid-tone; over-saturation may distract and fatigue the eyes and under-saturation may lead to eye strain
Warmer colors with longer wavelengths, such as yellows, oranges, and reds, offer higher contrast against white and black backgrounds; apply colors judiciously and consider that yellow tones for texts can be difficult to read and that red tones may be alarming and distracting
Test color choices with the target audience as emotional connotations are subjective and vary across demographics
Figure 1.
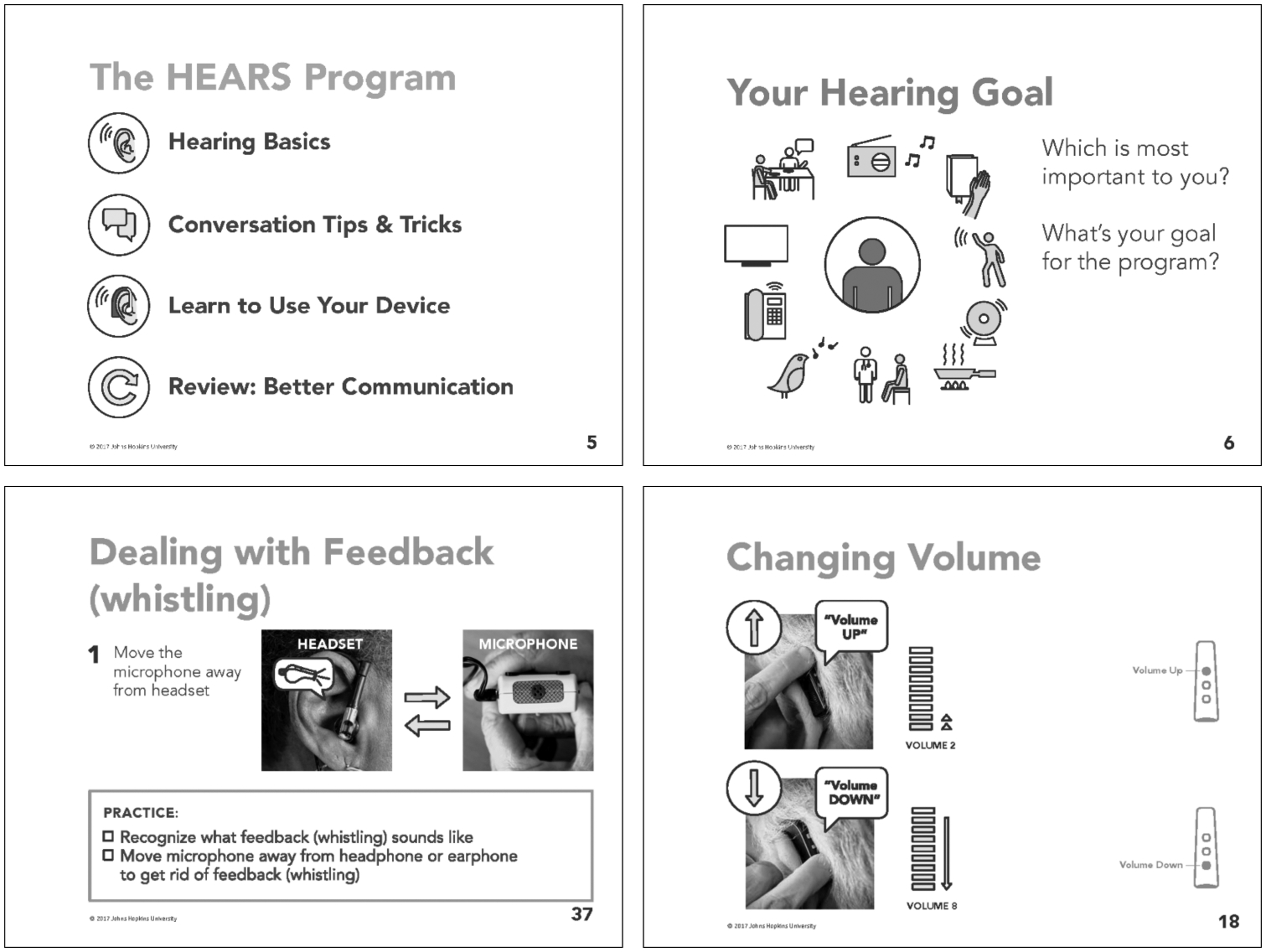
Examples of HEARS Program Manual Pages
Note:
HEARS materials are professionally printed single-sided in selected colors through following the principles described in Box 1, including community involvement. Manuals are either spiral-bound or saddle stitched for ease in use during program delivery.
Guiding Design Principles
Community engagement.
We incorporated community engagement and human-centered design methodologies8,10,11 to guide the development and enhance the acceptability of the training program. We approached the training program development and interactions with our partners through upholding multi-lateral learning between CHW trainees, housing staff, academic team members, and HCD practitioners.11 The HEARS audiologist met with staff and resident leaders weekly at one of the residential sites to co-develop the CHW training curriculum, engage in training activities, and discuss fidelity monitoring plans.
Human-centered design.
Emerging from roots in “design thinking,” human-centered design (HCD) is a qualitative approach for discovering innovative and viable solutions to problems through an iterative process of prototyping and testing ideas (Box 2).8,12 Human-centered design involves collaboration across stakeholders, particularly target users and beneficiaries, while considering realistic constraints.13 As a systematic methodology, HCD has origins beginning in the early 1980s and it was popularized by the business sector for creating consumer-driven commodities in the 1990s.8,13 Health care and public health initiatives have since begun leveraging HCD to tackle projects such as optimizing hospital shift change protocols, health risk assessment strategies, as well as the design and implementation of public health programs targeting social determinants of health.8,13–16
Box 2. HUMAN-CENTERED DESIGN PROCESS.
1. Frame & Plan
Organize and learn from existing research (including scientific data) that are associated with the problem.
Facilitate discussions around key research to understand the problem more intimately and to appropriately plan project engagements.
2. Research
Strive to understand the culture and context of the problem by learning about the people involved.
Talk to, observe, and actively learn from project stakeholders to identify relevant needs and assets to support and leverage.
3. Synthesize
Compile research observations and lessons learned and search for common themes.
Embrace the unexpected as they come, including insights, ideas, and inspiration.
Find appropriate opportunities through collaborations for intervention.
4. Ideate
Brainstorm as many ideas as possible and defer judgement (no bad ideas during drafting phases!).
Generate ideas visually, creatively, and share openly.
Focus on bigger concepts, not results.
Document the creative process and routinely refine ideas along the way.
5. Prototype
Create tangible representations of ideas.
Prototype with target people to check assumptions, lower risks, align expectations across all stakeholders, and uncover potential issues early.
6. Implement & Iterate
Test, iterate, and develop prototypes centered on local contexts.
Document and gather feedback for informing the development of strategies and interventions for feasibility, acceptability, sustainability, and target effectiveness.
Note:
Source: Adapted from Center for Social Design, Maryland Institute College of Art (MICA); Baltimore, MD (2021). Available at: https://www.mica.edu/research-center-for-social-design/process/
Human-centered design practitioners incorporate empathy, or a deeper consideration of people’s needs and their experiences using a product, into their drafting process with the goal of creating user-friendly results.12,13,16 From the business perspective, HCD aims to improve satisfaction with products given the multiple refinements guided by a deeper understanding of consumers’ needs.8,14,16 Application of HCD to public health initiatives may similarly facilitate greater acceptability and, ultimately, sustainability by valuing community partnerships.10,16
The HCD process also promotes divergent thinking as an essential component in the creation and testing of novel ideas, which often requires a team with diverse backgrounds.8,16 This approach complements principles of community engagement as it frames lived experiences as expertise, involving community partners as co-creators.10,11,16 The HEARS program benefits from collaboration with HCD practitioners from the Center for Social Design at the Maryland Institute College of Art (MICA) along with academics from multiple disciplines including audiology, gerontology, nursing, and otolaryngology. The program’s mission to target a public health disparity compliments the specialty of social design, which targets effecting positive social change through the HCD process (https://www.mica.edu/research/center-for-social-design/).
Developing and Testing a CHW Training Program
Project goal.
The HEARS program was developed to be delivered by trained para-professionals, including CHWs, and an initial pilot study was previously delivered by a single trained professional interventionist.6 The goal of the project described here was to develop a CHW training program for preparing lay individuals to promote the value of hearing health, deliver the HEARS program, and become certified HEARS interventionists.
Context and collaborators.
The development of the HEARS CHW training program incorporated community interests and representation through partnerships with local leaders. The relationship built upon existing collaborations that began in 2013, when the HEARS program was initially conceived, developed, and piloted. The community advisory board (CAB) formed in 2013 continued throughout this project and remains active today. The CAB consists of representatives from affordable older adult housing organizations in the Baltimore area, including Weinberg Senior Living and Catholic Charities, city officials from the local Area Agency on Aging (AAA), building Service Coordinators who advocate for residents, resident leaders from participating buildings, and representatives from HASA, a local nonprofit organization providing hearing care services. In addition to CAB meetings, the academic team and HCD practitioners sought out regular ad-hoc consultation with community representatives during the development of program materials, delivery plans, and program evaluation.
Program CHWs and clients.
Volunteer residents serving as CHW trainees (n=6) were recruited based on nominations from housing staff who identified trusted community leaders as potential trainees. The CHWs’ clients (n=14) were recruited through a building-wide information session. All clients were community-dwelling residents from the same independent housing network as the CHWs, Weinberg Senior Living. See Table 1 for demographic details. Clients had the option of inviting a communication partner (e.g., spouse/partner, adult child) to join their sessions with the CHWs. Through consultation with the CAB, volunteers serving as CHWs were offered monthly remunerations for their time during the course of the program development and implementation. The plan was approved by the Johns Hopkins School of Medicine’s Institutional Review Board and all volunteers provided consent for participating. Pre- and three-month post-intervention self-reported assessments were gathered from clients to assess the CHW training program’s preliminary impact.
Table 1.
VOLUNTEER CHARACTERISTICS
| Demographics | Volunteers |
|---|---|
| Age (years), median (IQR) | 71.5 (66.6–78.5) |
| Female sex, n (%) | 12 (60) |
| Race/ethnicity, n (%) | |
| Non-Hispanic Black or African American | 15 (75) |
| Non-Hispanic White or Caucasian | 3 (15) |
| Hispanic and/or Latinx | 1 (5) |
| Other | 1 (5) |
| Highest level of education completed, n (%) | |
| Less than high school | 5 (25) |
| High school graduate or GED | 4 (20) |
| Greater than high school | 11 (55) |
| Annual income, n (%) | |
| Less than $25,000 | 18 (90) |
| More than $25,000 | 2 (10) |
| Lived alone, n (%) | 20 (100) |
Program site.
Weinberg Senior Living is a nonprofit older adult community housing network nested within a local faith-based organization, Comprehensive Housing Assistance, Inc. (CHAI).
A training program for CHW-delivered hearing care.
Curriculum development.
We first developed a training framework to support a high-quality, high-fidelity delivery of the HEARS intervention by CHWs. The HEARS audiologist prototyped classroom modules based on adaptations of the Gallaudet University Peer Mentoring Training Program.17 The original program from Gallaudet University is a hybrid online/campus-based certificate program designed to prepare adults with hearing loss to work alongside clinical professionals in aural rehabilitation by providing informal support, mentoring, and coaching to other adults with hearing loss.17 With input from the CHW trainees and housing staff, we assessed the relevancy and appropriateness of the training program’s format and content based on a thorough review of the HEARS intervention.6 Our team co-identified the interpersonal skills needed to serve as an effective CHW for the target client population and efforts also focused on ensuring printed materials were written at or below a 6th–7th grade reading level. The curriculum was refined from an initial prototype comprising 14 weekly modules (1.5 hours each) to eight weekly modules (2 hours each) (Box 3).
Box 3. HEARS COMMUNITY HEALTH WORKER TRAINING MODULES.
| Prototype Structure | Final Structure |
|---|---|
14 sessions (1.5 hours each)
|
8 sessions (2 hours each)
|
CHW trainee evaluation and certification.
The HEARS audiologist assessed the acceptability of the CHW training program, specifically the module structures, learning activities, approaches for evaluation, and participation policies with CHW trainees and community partners. Trainees demonstrated content and technical competencies through supervised practical exercises evaluated through a structured rubric assessing levels of independence, comfort, and appropriateness of delivery. Based on the evaluation, successful trainees interested in proceeding earned a certificate to serve as a CHW interventionist (HEARS Teacher) who delivers the HEARS program or as a support personnel (HEARS Promoter) who serves as a community liaison for referrals and program operations. We certified two HEARS Teachers who met training benchmarks and two HEARS Promoters from the first cohort. Two CHW trainees chose not to complete the training due to conflicting priorities.
Monitoring program fidelity.
Fidelity monitoring protocols for CHWs delivering the HEARS program were co-developed with community input, including procedures for audio recording a subset of interventions for evaluation purposes. We established monthly group meetings following certification with CHWs for opportunities to provide booster trainings and technical support as needed, continuing education, and team building activities. Additionally, CHWs received remote support through weekly case reviews by phone with the audiologist to preserve the personal dynamics between CHWs and clients. The communication plan (i.e., monthly meetings and weekly phone calls) was intended to enhance training program feasibility and intervention quality, safety, and acceptability. All interventions were delivered in reserved community spaces within the residential building. One client invited a communication partner to join and all other clients had one-on-one sessions with their CHW.
CHW training program evaluation.
To evaluate the CHW training program’s preliminary impact, we assessed HEARS clients’ three-month post-intervention outcomes. A team of two trained data collectors recorded survey data through standardized interviews with printed questionnaire cards that also reflected the design principles detailed in Box 1. Self-reported outcomes included communication function (Hearing Handicap Inventory for the Elderly-screening version, HHIE-S18) and a program evaluation from all clients who completed their three-month follow-up (n=9). All clients (9/9) indicated at least some benefit from the CHW-delivered HEARS program and felt more connected with others. A majority shared that they met personal communication goals through the program (88.9%, 8/9) and that HEARS enabled them to feel less frustrated by communication difficulties (88.9%, 8/9). A majority indicated that the program was instrumental in learning how to use an OTC amplification device (77.8%, 7/9). Furthermore, all clients shared that the CHW was the most useful aspect of the program and all would highly recommend the program to others (9/9). The median change in communication function as measured by the HHIE-S was −8 (IQR: 21) over three-months, indicating improvements in communication function. This compares to both the previous HEARS pilot that was also measured over three months, and professionally-delivered care with hearing aids.6 (Figure 2)
Figure 2.
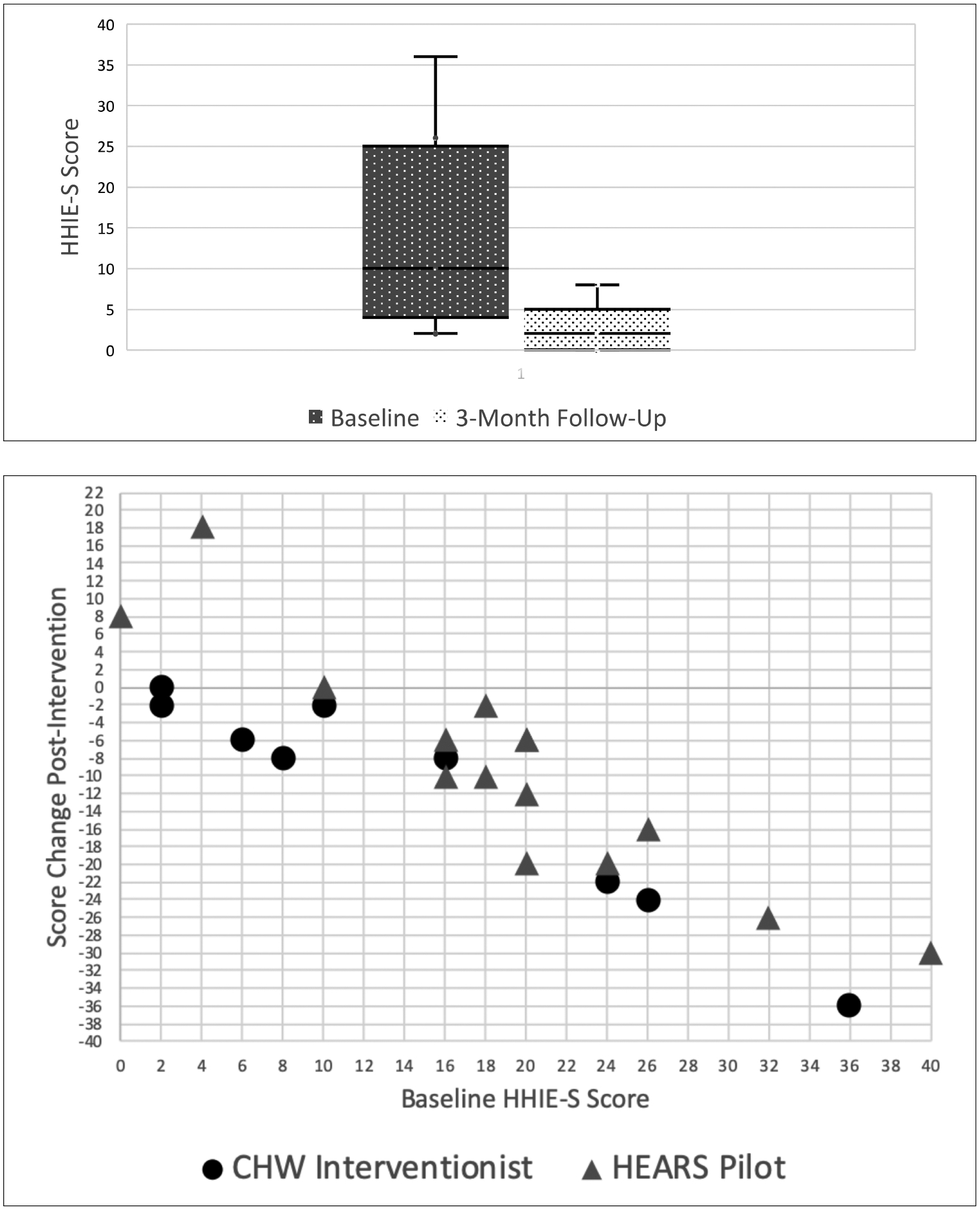
HEARS Client Hearing Handicap
Note:
TOP: Baseline self-reported hearing handicap scores (Hearing Handicap Inventory for the Elderly, Screening Version; HHIE-S) versus 3-months post-intervention scores. A score of ≥10 represents where follow-up hearing care is recommended.18 BOTTOM: Higher baseline HHIE-S scores generally yielded greater reductions (improvements) in self-reported hearing handicap following the HEARS intervention. Group median change in HHIE-S is −8 (IQR: 21) and −10 (IQR: 18) as delivered by CHW interventionist and the HEARS pilot’s professional interventionist,6 respectively.
Future directions.
Building from the initial CHW training program, HEARS is currently undergoing a randomized controlled trial (NCT03442296) based in over 10 community sites throughout Baltimore and includes eight trained older adults as CHWs. We continue to foster local partnerships with community organizations through an active CAB. Our collaboration with HCD practitioners enables design adaptations to setting-specific challenges such as client recruitment. The HEARS program has been adapted and tested at multiple sites nationally and internationally.19–21 Access HEARS, a separate nonprofit organization with national-and state-level funding, focuses on building a sustainable and scalable model of community-delivered hearing care and serves as an important agent in transitioning pilot programs into practice.
Given the growing number of pilot programs that leverage community resources to provide accessible hearing care, targeting local- and national-level policies is critical to support ongoing implementation and dissemination.19 Policies must focus on sustainability through the development of reimbursement mechanisms. Other priority policy areas include defining scope of practice, standardizing training curricula, and regulating certification processes for CHWs providing hearing care to ensure quality and safety.19
Conclusion.
There is growing recognition of the need to address hearing loss among older adults as a national and global public health imperative.1,22 Options to obtain hearing care in the United States are generally limited to those with enough resources and clinic-based models often fail to provide adequate access.1 A community-based program that trains CHWs, specifically older adult peer mentors, is feasible, acceptable, demonstrates preliminary improvements in outcomes, and represents a critical avenue for advancing task-sharing in hearing care as a public health approach to age-related hearing loss.19 With the coming expansion of OTC hearing aids, community-delivered, evidence-based models, such as HEARS, are needed to advance hearing health equity.
Acknowledgments
MICA social design team members were integral collaborators during the human-centered design process, particularly Becky Slogeris, Jen Sullivan, and Smile Indias.
Staff members of Weinberg Senior Living provided invaluable assistance throughout the project.
- This project was supported in part by funding from the following:
- NIH NIA P30AG048773 (FRL)
- NIH NIDCD R21DC015062/R33 (CLN, FRL)
- NIH NIA K23AG059900 (CLN)
- Eleanor Schwartz Charitable Foundation (FRL)
- Cochlear Center for Hearing and Public Health at the Johns Hopkins Bloomberg School of Public Health
CLN and FRL report being board members for the nonprofit, Access HEARS
FRL reports being a consultant for Cochlear, Ltd. and Boehringer Ingelheim; and receives speaking honoraria from Amplifon and Cochlear, Ltd.
References
- 1.National Academies of Sciences, Engineering, and Medicine. Hearing health care for adults: priorities for improving access and affordability. Washington, DC: The National Academies Press, 2016. 10.17226/23446 [DOI] [PubMed] [Google Scholar]
- 2.Deal JA, Betz J, Yaffe K, et al. Hearing impairment and incident dementia and cognitive decline in older adults: The health ABC study. J Gerontol A Biol Sci Med Sci. 2017. May;72(5):703–9. 10.1093/gerona/glw069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mamo SK, Nieman CL, Lin FR. Prevalence of untreated hearing loss by income among older adults in the United States. J Health Care Poor Underserved. 2016. Nov;27(4):1812–8. https://doiorg/10.1353/hpu.2016.0164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nieman CL, Marrone N, Szanton SL, et al. Racial/ethnic and socioeconomic disparities in hearing health care among older Americans. J Aging Health. 2016. Feb;28(1):68–94. Epub 2015 May 7. 10.1177/0898264315585505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warren E. S.670—115th Congress (2017–2018): Over-the-Counter Hearing Aid Act of 2017. 2017.
- 6.Nieman CL, Marrone N, Mamo SK, et al. The Baltimore HEARS Pilot Study: an affordable, accessible, community-delivered hearing care intervention. Gerontologist. 2017. Nov;57(6):1173–86. 10.1093/geront/gnw153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Th ompson GP, Sladen DP, Borst BJH, et al. Accuracy of a tablet audiometer for measuring behavioral hearing thresholds in a clinical population. Otolaryngol Head Neck Surg. 2015. Nov;153(5):838–42. Epub 2015 Jul 16. 10.1177/0194599815593737 [DOI] [PubMed] [Google Scholar]
- 8.Brown T, Wyatt J. Design thinking for social innovation. Stanford, CA: Stanford Social Innovation Review, 2010. Available at: https://ssir.org/articles/entry/design_thinking_for_social_innovation. [Google Scholar]
- 9.Fisk AD, Czaja SJ, Rogers WA, et al. Designing for older adults: principles and creative human factors approaches. 2nd ed. Boca Raton, FL: CRC Press, 2009. [Google Scholar]
- 10.Chen E, Leos C, Kowitt SD, et al. Enhancing community-based participatory research through human-centered design strategies. Health Promot Pract. 2020. Jan;21(1):37–48. Epub 2019 May 25. 10.1177/1524839919850557 [DOI] [PubMed] [Google Scholar]
- 11.Suen JJ, Marrone N, Han H-R, et al. Translating public health practices: community-based approaches for addressing hearing health care disparities. Semin Hear. 2019;40(1):37–48. Epub 2019 Feb 5. 10.1055/s-0038-1676782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matheson GO, Pacione C, Shultz RK, et al. Leveraging human-centered design in chronic disease prevention. Am J Prev Med. 2015. Apr;48(4):472–9. Epub 2015 Feb 18. 10.1016/j.amepre.2014.10.014 [DOI] [PubMed] [Google Scholar]
- 13.Roberts JP, Fisher TR, Trowbridge MJ, et al. A design thinking framework for health-care management and innovation. Healthc (Amst). 2016. Mar;4(1):11–4. Epub 2016 Jan 14. 10.1016/j.hjdsi.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 14.Brown T Design Th inking. Harv Bus Rev. 2008. Jun;86(6):84–92, 141. [PubMed] [Google Scholar]
- 15.Harte R, Quinlan LR, Glynn L, et al. Human-centered design study: enhancing the usability of a mobile phone app in an integrated falls risk detection system for use by older adult users. JMIR Mhealth Uhealth. 2017. May 30;5(5):e71. 10.2196/mhealth.7046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vechakul J, Shrimali BP, Sandhu JS. Human-centered design as an approach for place-based innovation in public health: a case study from Oakland, California. Matern Child Health J. 2015. Dec;19(12):2552–9. 10.1007/s10995-015-1787-x [DOI] [PubMed] [Google Scholar]
- 17.Bally SJ, Bakke MH. A Peer Mentor Training Program for Aural Rehabilitation. Trends Amplif. 2007. Jun;11(2):125–31. 10.1177/1084713807301587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ventry I, Weinstein B. Identification of elderly people with hearing problems. ASHA. 1983. Jul;25(7):37–42. [PubMed] [Google Scholar]
- 19.Suen JJ, Bhatnagar K, Emmett SD, et al. Hearing care across the life course provided in the community. Bull World Health Organ. 2019. Oct 1;97:681–90. Epub 2019 Aug 20. 10.2471/BLT.18.227371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.A Canadian first: community-based affordable hearing care. North York, ON: Baycrest, 2018. Available at: https://www.baycrest.org/Baycrest-Pages/News-Media/News/Clinical-Programs-Nursing/A-Canadian-First-Community-Based-Affordable-Heari. [Google Scholar]
- 21.Mester I An audiologist’s quest to empower seniors through hearing. Toronto, ON: Centre for Aging + Brain Health Innovation, 2017. Available at: https://www.cabhi.com/news/an-audiologists-quest-to-empower-seniors-through-hearing/. [Google Scholar]
- 22.Davis A, McMahon CM, Pichora-Fuller KM, et al. Aging and hearing health: the life-course approach. Gerontologist. 2016. Apr;56 Suppl 2(Suppl 2):S256–67. 10.1093/geront/gnw033 [DOI] [PMC free article] [PubMed] [Google Scholar]


