SUMMARY
Strabismus is a common disorder in which eyes are not aligned with their optical axis, resulting in an abnormal binocular interaction, thus leading to amblyopia. Accordingly, early detection and diagnosis are mandatory. Despite technology development and constant knowledge growth, the foundations of physiology and the diagnosis of strabismus were set back in the 19th or early 20th century and have not changed since. In this paper, a novel, properly tested and evaluated eye-tracking based method for manifest strabismus diagnosis is presented. The evaluation showed the aforementioned method to have both high sensitivity and specificity in detecting manifest strabismus without the need for a skilled examiner, thus being suitable for population screening and highlighting the need for future research regarding testing of latent strabismus.
Key words: Computer, Eye tracking, Manifest strabismus
Introduction
Strabismus is a disorder in which eyes are not aligned with their optical axis, resulting in abnormal binocular interaction leading to amblyopia. Amblyopia, colloquially a ‘lazy eye’ is regarded as the leading cause of preventable child blindness with the prevalence of 1%-5% and the leading cause of persistent unilateral visual impairment in adulthood (1). Anisometropia is difference in the refractive errors of two eyes, and it is the most common cause of amblyopia in children aged 3-7 years (40%), followed by strabismus (38%), and a combination of these two (24%) (2-5). Other, less common causes of amblyopia include congenital cataract, ptosis, corneal dystrophy, and injury (5). The ideal period for detection of these disorders is before school age. Therefore, ophthalmologists have developed a comprehensive preschool vision screening program, which could become the gold standard (6-8). The gold standards for detecting strabismus are additional tests performed by ophthalmologists, such as cover test variations and alternate prism cover tests (9). They might be unreliable due to interobserver variability with differences in prism diopter because of measurement errors (10). Another approach is a possible screening test that can be performed by a wide range of health professionals, thus being a more cost-effective and less time-consuming way to prevent visual impairments (11). We use monocular visual acuity testing with age-appropriate vision tests (Lea symbol test, etc.), ocular alignment test (cover tests, Hirschberg test, etc.), stereo acuity testing (Lang test), and non-cycloplegic retinoscopy in preschool vision screening protocols (12, 13). Vision screening programs use optotype testing for visual acuity with or without the cover test for strabismus. Handheld autorefractors and photorefractors for detecting amblyopia or amblyogenic factors have entered vision screening protocols (14-17). The American Association of Pediatric Ophthalmology and Strabismus published their recommendations for automated screening (18), but not as the gold standard. Nevertheless, the utility of refraction testing, as explored by Atkinson and Braddick (16) and Atkinson et al. (17), has been reintroduced in clinical practice with the use of novel, handheld photorefractor (19-22). The software that quantifies misalignment from photographs automatically measures ocular deviation (23). Scleral search coil technique was the basis for the evolution of eye movement detection methods (24, 25). Afterwards, electrooculography (26) and SKALAR Iris apparatus (infrared oculography) followed (26-28). Finally, biometric measurements and identification, object recognition, and attention modeling have been developed (29-31). Models of eye alignment detection based on video cameras were at first used for eye tracking purpose in a way of automated eye tracking based systems (31-36). A family member could easily detect large deviations of the eye but not smaller ones, thus leading to the increased percentage of strabismus and affecting amblyopia requiring qualified examiner. While visual acuity testing does not seem to require qualified examiner, the ocular alignment testing does. Our previous work analyzed application possibilities of eye-tracking in medical oculography diagnostics (37). Meanwhile, technology and computers have provided more noninvasive measurements with higher sampling rates and high specificity and sensitivity. In this study, we clinically tested a developed computer-based eye-tracking diagnostic system for strabismus (21).
Materials and Methods
Study design and patients
A clinical study of the Strabiscope system was conducted between June 2017 and June 2019 on subjects randomly selected among patients at the Department of Ophthalmology, Sestre milosrdnice University Hospital Centre in Zagreb, Croatia, providing a representative sample of the population of the Republic of Croatia. The procedures applied were approved by the Sestre milosrdnice University Hospital Center Ethics Committee and in accordance with Helsinki Declaration as of 1975. The study included patients diagnosed with manifest strabismus and orthoptic controls, based on the results of complete ophthalmologic examination. Patients with refractive errors (>+/-7.50 dpt, or cylindrical +/-3.00dpt), amblyopia, other ocular and neurological pathologies were excluded. Complete ophthalmologic examination included visual acuity testing of both near (0.4 m) and far (3 m) (ETDRS optotypes), Lea symbols, Pediatric Eye Near and Distance Charts (Good-Lite, Elgin, USA), cover tests (cover, uncover, alternate cover, and prism cover test), Bagolini, Titmus and fusion test (near and far). According to the cover test, patients were divided into the orthoptic control group and strabismus group, while latent strabismus was excluded (38). The squint angle was measured with prisms. First, two pediatric ophthalmologists performed complete ophthalmologic examination. Then patients were tested with Strabiscope set in eye-tracking apparatus using Tobii EyeX (Tobii AB, Danderyd, Sweden). Since this is an infrared eye tracking device, we minimized additional blinding of patients. Distance between the device and patient was dictated by the device and set to 0.6 m. Cover testing was performed using an occluder acting as a selective wave length filter. In this way, the occluded eye can be observed by an infrared apparatus. The eye-tracking system mimics ophthalmologic examination by using cover test characteristics implemented into a computer based system. First measurement included tracking of both eyes, but later measurements exploited cover test, computer-based, covering one or the other eye, thus exploiting the full range of cover test and their variants (optical occluder being penetrable to infrared light but not to human sight, thus acting as cover test occluder) (Table 1).
Table 1. Description and abbreviations of variables.
| ou-scv | Value of eye deviation angle in degrees after eye tracking of both eyes without eyeglass correction |
|---|---|
| ou-scm | Maximal value of deviation angle in degrees after eye tracking of both eyes without eyeglass correction |
| od-scv | Value of eye deviation in degrees after tracking of the right eye without eyeglass correction while the left eye is covered with the occluder |
| od-scm | Maximal value of eye deviation angle in degrees after tracking of the right eye without eyeglass correction while the left eye is covered with the occluder |
| odcd-scv | Value of eye deviation angle in degrees after eye tracking of the right eye without eyeglass correction while the right eye is covered with the occluder |
| odcd-scm | Maximal value of eye deviation in degrees after eye tracking of the right eye without eyeglass correction while the right eye is covered with the occluder |
| odcs-scv | Value of eye deviation in degrees after eye tracking of the right eye without eyeglass correction while the left eye is covered with the occluder |
| odcs-scm | Maximal value of eye deviation in degrees after eye tracking of the right eye while the left eye is covered with the occluder |
| os-scv | Value of eye deviation in degrees after eye tracking of the left eye without eyeglass correction while the right eye is covered with the occluder |
| os-scm | Maximal value of eye deviation in degrees after eye tracking of the left eye without eyeglass correction while the right eye is covered with the occluder |
| oscs-scv | Value of eye deviation in degrees after eye tracking of the left eye without eyeglass correction while the left eye is covered with the occluder |
| oscs-scm | Maximal value of eye deviation in degrees after eye tracking of the left eye without eyeglass correction while the left eye is covered with the occluder |
| oscd-scv | Value of eye deviation in degrees after eye tracking of the left eye without eyeglass correction while the right eye is covered with the occluder |
| oscd-scm | Maximal value of eye deviation in degrees after eye tracking of the left eye without eyeglass correction while the right eye is covered with the occluder |
Strabiscope
Our system based on our work and presented at the MIPRO 2014 Conference, has the primary purpose of diagnosing and measuring strabismus, therefore we call it Strabiscope (37). The system basic idea is to display a target dot on the screen intended to be gazed by the patient. The system captures 3D and gaze positions of the eye continuously throughout the test. The software further uses these data to calculate parameters for strabismus diagnosis (37). We used the double-Purkinje-image (DPI) eye-tracking system based on the eye-tracking method used by Van Diepen (39). This technique also uses capturing of the reflected light projected on the eye (37, 39, 40). The eye-tracker we used is Tobii EyeX, with a sampling rate of 60 Hz, mounted on a computer screen.
The system hardware setup
The main hardware components necessary for the setup include a 2D display and an eye-tracking device (Fig. 1). The patient sits on a chair with adjustable height, in front of the screen. No chin or headrest is necessary. The head of the patient should be at optimal distance from the eye-tracking device. Optimal distance d depends on the screen size and type of eye-tracking device used in the setup. We calculate optimal distance using the following formula: d=s/tanα.
Fig. 1.
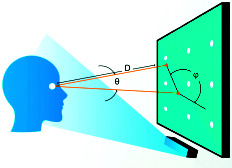
Strabiscope hardware setup and measurement method: real gaze vector (line) and ideal gaze vector (dashed line) are used for calculating deviation (θ) and orientation (φ).
Parameters represent a distance from the bottom center corner of the display area to the upper right/left corner. Optimal gaze angle alpha is a known parameter; its value depends on the type of eye-tracking device.
The measurement method
The system calculates distortion of the eye-viewing angle, described by deviation and orientation. Deviation is the angle between two vectors, real gaze vector and ideal gaze vector, and deviation is calculated from the vectors by the formula shown in Figure 1.The real gaze vector is a vector that describes orientation of the current eye gaze. The eye-tracking device does not explicitly provide the real gaze vector. However, the real gaze vector can be calculated by subtracting the 3D gaze point and the 3D eye position. On the other hand, the ideal gaze vector shows orientation of the gaze if the eyes are healthy. The ideal gaze vector can be computed by subtracting the 3D target point and the 3D eye position. The orientation factor is direction of the deviation, an angle formed by the x-axis vector and screen gaze vector, in positive (counter clockwise) direction. The x-axis vector is horizontal to the display and oriented from left to right. The screen gaze vector connects the target dot with the gaze point in 2D screen coordinates, oriented in the direction of the gaze point.
The eye-tracking sensor records the eye and gaze positions. The system tracks and gathers the positions from both eyes separately and also automatically detects if the eye is right or left, given the eye position is a point in 3D space with values provided in millimeters. The type of 3D coordination system depends on the type of eye-tracking device. Most common is the User Coordinate System (UCS), a millimeter based eye-tracking fixed coordinate system. The origin of the system is at the center of the frontal surface of the eye-tracking device. The x-axis is horizontal and points towards the user’s right side. The y-axis is vertical, and points towards the user up. The z-axis points directly towards the user. The other eye-tracking devices use a 3D coordination system relative to the screen, where the device is mounted. The origin of this system is at the center of the screen. The x- and y-axes are both in the same plane as the display screen. The z-axis is orthogonal to the screen and extends towards the user. The gaze position is a 2D point, represented as a pixel on the screen at which the user gazes. For further calculations, gaze positions need to be converted from a 2D screen coordination system to a 3D coordinate system, the same as used for describing the eye position. The software development kit (SDK) provides additional system configuration parameters. These parameters include the screen physical characteristics such as resolution and dimensions (horizontal and vertical size in millimeters).
The system software design
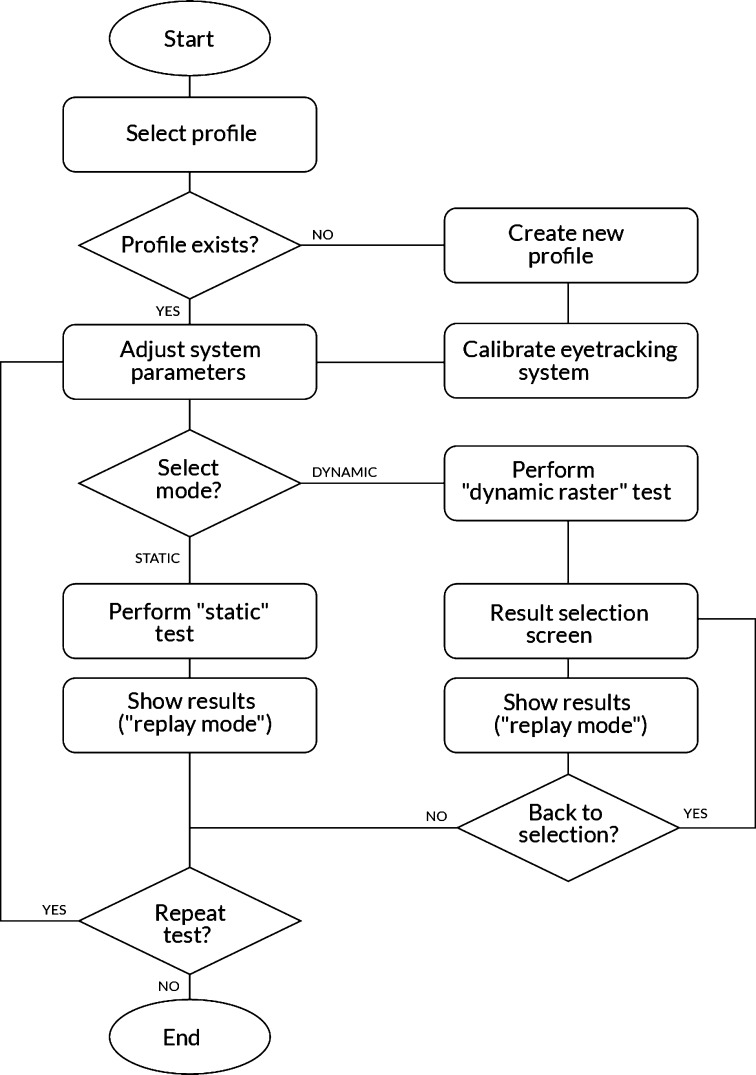
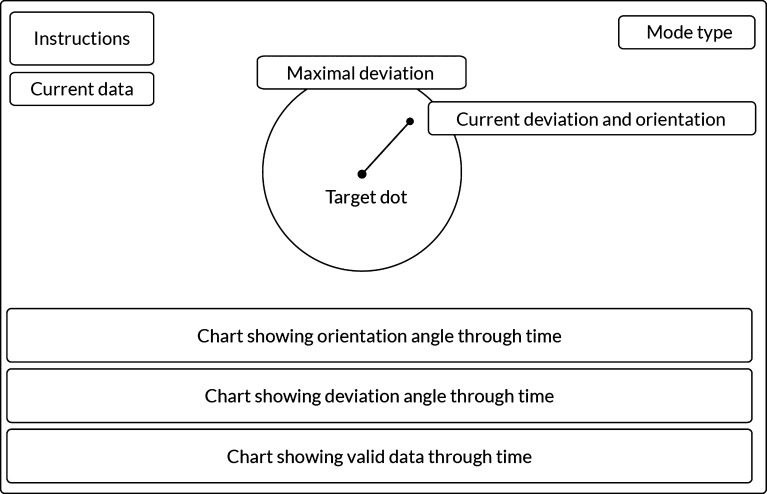
All system software is designed around SDK, acquired with the eye-tracking sensor (Fig. 2). As depicted in Figure 2, the patient’s profile needs to be selected, or created followed by the calibration prior to testing, as reported in our previous work (37). Data shown on the screen are presented numerically and graphically. Deviation and orientation factors are represented numerically as values in degrees and displayed in the upper left section of the screen. Gaze point is shown as a dot on the screen and connected to the central point (target dot), representing a deviation vector. Although all data are acquired and all results calculated, the results are not permanently stored. In addition to the data, all possible controls are also noted and described in the upper left section of the screen. All parameters for measurement can be adjusted to the desired values. After testing, the results are shown on the screen and can be reviewed by the examiner. There is a special module, called ‘replay module’, enabling examiner to get final test results or to replay results for the whole test (Fig. 3). The ‘replay module’ has functions for reviewing collected data. The main function is replay, intended for showing all data in a similar frame rate as original frame rate during data acquisition. The examiner can pause, replay, slow down, or speed it up. The special functionality comes if replay is paused; by selecting time on the timeline, the examiner can browse data interactively. Just below command description the main values are displayed for selected moment. These values include deviation and orientation angle, as well as the exact time of the selected moment expressed in seconds. Central area of the screen demonstrates graphically the currently selected value in time, represented as a vector inside a circle. Size of the vector represents a deviation angle where the circle shows the maximal value of the entire measurement. The direction of the vector (angle between x-axis vector and the vector in counter clockwise direction) represents orientation angle. Bottom section of the screen contains various graphs showing data in time throughout the measurement duration. The timeline track lies on the bottom of this section, which is the bottom of the screen. Currently selected time is represented by a grey track on the white background. The size of the grey track shows time of the currently selected moment compared to the duration of the whole measurement. Just above timeline track, there is a validity track. This track shows if there are valid data for certain period of measurement time or not. Not valid data can be produced if the patient blinks or temporarily changes eye fixation out of the eye-tracking device working area. On the validity track, valid data are presented with green colored track, and not valid with red colored track. Above the validity track, there is a deviation angle graph of the whole measurement and an orientation angle graph. Both deviation and orientation graphs present its value with the width of the blue track. Graphic representations of values are scaled between zero and maximal value of the whole measurement.
Fig. 2.
Strabiscope system workflow: diagram shows all possible states and actions from the start to the end of the system single usage.
Fig. 3.
Graphic interface of the replay mode. The “Instructions”, “Current data”, “Mode type”, “Maximal deviation” and “Current deviation and orientation” parts of the screen contain information in text format. Lower part of the screen shows three different charts graphically representing orientation, deviation and valid data through time.
Statistical analysis
Statistical analysis was performed using SPSS for MS Windows (ver. 20.0, Statistical Package for the Social Sciences; SPSS, Inc., Chicago, USA). The variables included in the analysis were tested according to normal distribution using one sample Kolmogorov-Smirnov test. Differences between the strabismus and control groups were tested using the independent samples T test for each variable. The strength of linear relationship of repeated measurements was tested by Pearson correlation coefficient, and their differences with paired-samples T test, variable after variable, separated in groups. The receiver operating characteristic (ROC) curve was used to define the cut-off value in order to define border values of detecting strabismus with Strabiscope apparatus. The curve plot itself, in a ROC curve, plots the sensitivity against the false-positive rate (i.e., 1 specificity), where each point reflects the values obtained at a different cut-off point value from a continuous measure. The choice of cut-off values is situated at the exact point of the ROC curve where the sum of sensitivity and specificity is the greatest. Calculating of area under the curve (AUC) gives us a summary of discriminative ability among tests, thus an AUC >0.9 is regarded excellent; >0.8-0.9 average; >0.7-0.8 good; >0.6-0.7 average; and<0.6 poor (41). The values of p<0.05 were considered statistically significant.
Results
Out of the 81 included subjects, 41 were previously diagnosed with strabismus and 40 were randomly selected as orthoptic controls. The enrolled patients were aged 5 to 52 years (mean: 16.6; standard deviation (SD): 11.9); there were 22 males and 19 females in the strabismus group, aged 7 to 31 years (mean: 14.9, SD: 6.2), and 11 males and 29 females in the control group. The results of the variable test for normality confirmed normal distribution of all measured values in the control group, whereas some of the strabismus group patients had higher values recorded that led to the slightly left oriented asymmetric distribution, which was medically accepted. Table 2 shows results of the test of differences in the measured values between the strabismus group and control group. In all measurements, participants with strabismus were shown to have higher measured values compared to the control group. Test of difference between the first and second measurement, divided according to groups, showed strong linear dependence set by their correlation and seen by their negligible differences in all of the measurements (Tables 3 and 4).
Table 2. Differences between the groups.
| Variable | Group | n | Mean | SD | t-test | ||
|---|---|---|---|---|---|---|---|
| t | df | p | |||||
| ou-scv1 | Strabismus | 41 | 2.09 | 3.20 | 3.17 | 79 | 0.002 |
| Control | 40 | 0.48 | 0.20 | ||||
| ou-scv2 | Strabismus | 41 | 2.10 | 2.99 | 3.40 | 79 | 0.001 |
| Control | 40 | 0.49 | 0.20 | ||||
| ou-scm1 | Strabismus | 41 | 4.44 | 4.60 | 3.85 | 79 | <0.001 |
| Control | 40 | 1.58 | 0.89 | ||||
| ou-scm2 | Strabismus | 41 | 4.30 | 4.70 | 4.29 | 79 | <0.001 |
| Control | 40 | 1.09 | 0.38 | ||||
| od-scv1 | Strabismus | 39 | 3.19 | 4.19 | 3.38 | 77 | 0.001 |
| Control | 40 | 0.95 | 0.39 | ||||
| od-scv2 | Strabismus | 39 | 3.46 | 4.33 | 3.60 | 77 | 0.001 |
| Control | 40 | 0.98 | 0.43 | ||||
| od-scm1 | Strabismus | 39 | 6.47 | 5.97 | 4.66 | 77 | <0.001 |
| Control | 40 | 2.04 | 0.78 | ||||
| od-scm2 | Strabismus | 39 | 5.97 | 6.23 | 3.87 | 77 | <0.001 |
| Control | 40 | 2.11 | 0.96 | ||||
| odcd-scv1 | Strabismus | 40 | 11.68 | 6.69 | 10.22 | 78 | <0.001 |
| Control | 40 | 0.85 | 0.33 | ||||
| odcd-scv2 | Strabismus | 40 | 11.58 | 6.69 | 10.11 | 78 | <0.001 |
| Control | 40 | 0.88 | 0.41 | ||||
| odcd-scm1 | Strabismus | 40 | 13.72 | 6.59 | 11.15 | 78 | <0.001 |
| Control | 40 | 2.01 | 0.83 | ||||
| odcd-scm2 | Strabismus | 40 | 14.22 | 6.63 | 11.61 | 78 | <0.001 |
| Control | 40 | 1.99 | 0.72 | ||||
| odcs-scv1 | Strabismus | 40 | 1.22 | 0.70 | 2.66 | 78 | 0.009 |
| Control | 40 | 0.87 | 0.43 | ||||
| odcs-scv2 | Strabismus | 40 | 1.27 | 0.94 | 2.42 | 78 | 0.018 |
| Control | 40 | 0.88 | 0.42 | ||||
| odcs-scm1 | Strabismus | 40 | 3.07 | 3.15 | 1.95 | 78 | 0.050 |
| Control | 40 | 2.04 | 1.19 | ||||
| odcs-scm2 | Strabismus | 40 | 3.49 | 3.51 | 2.69 | 78 | 0.009 |
| Control | 40 | 1.96 | 0.79 | ||||
| os-scv1 | Strabismus | 41 | 4.35 | 5.84 | 3.78 | 79 | <0.001 |
| Control | 40 | 0.85 | 0.38 | ||||
| os-scv2 | Strabismus | 41 | 4.15 | 6.03 | 3.45 | 79 | 0.001 |
| Control | 40 | 0.85 | 0.35 | ||||
| os-scm1 | Strabismus | 41 | 6.68 | 6.86 | 4.41 | 79 | <0.001 |
| Control | 40 | 1.87 | 0.75 | ||||
| os-scm2 | Strabismus | 41 | 6.56 | 6.64 | 4.43 | 79 | <0.001 |
| Control | 40 | 1.87 | 0.80 | ||||
| oscs-scv1 | Strabismus | 40 | 12.49 | 6.35 | 11.64 | 78 | <0.001 |
| Control | 40 | 0.79 | 0.34 | ||||
| oscs-scv2 | Strabismus | 40 | 12.40 | 5.95 | 12.35 | 78 | <0.001 |
| Control | 40 | 0.75 | 0.38 | ||||
| oscs-scm1 | Strabismus | 40 | 14.33 | 6.04 | 12.76 | 78 | <0.001 |
| Control | 40 | 1.96 | 1.09 | ||||
| oscs-scm2 | Strabismus | 40 | 14.35 | 5.43 | 14.60 | 78 | <0.001 |
| Control | 40 | 1.73 | 0.67 | ||||
| oscd-scv1 | Strabismus | 41 | 1.07 | 0.72 | 3.08 | 79 | 0.003 |
| Control | 40 | 0.69 | 0.29 | ||||
| oscd-scv2 | Strabismus | 41 | 1.06 | 0.61 | 3.63 | 79 | 0.001 |
| Control | 40 | 0.67 | 0.30 | ||||
| oscd-scm1 | Strabismus | 41 | 3.52 | 4.10 | 2.86 | 79 | 0.005 |
| Control | 40 | 1.63 | 0.76 | ||||
| oscd-scm2 | Strabismus | 41 | 3.47 | 4.25 | 2.97 | 79 | 0.004 |
| Control | 40 | 1.45 | 0.66 | ||||
1 and 2 = first and second measurement; SD = standard deviation
Table 3. Correlations and differences between the first and second measurements in strabismus group.
| Variable | Correlation | Paired difference | |||
|---|---|---|---|---|---|
| n | r | p | Mean | p | |
| ou-scv | 41 | 0.969 | <0.001 | -0.004 | 0.974 |
| ou-scm | 41 | 0.882 | <0.001 | 0.141 | 0.690 |
| od-scv | 39 | 0.988 | <0.001 | -0.265 | 0.019 |
| od-scm | 39 | 0.737 | <0.001 | 0.504 | 0.482 |
| odcd-scv | 40 | 0.985 | <0.001 | 0.097 | 0.598 |
| odcd-scm | 40 | 0.902 | <0.001 | -0.500 | 0.285 |
| odcs-scv | 40 | 0.946 | <0.001 | -0.055 | 0.339 |
| odcs-scm | 40 | 0.906 | <0.001 | -0.417 | 0.084 |
| os-scv | 41 | 0.962 | <0.001 | 0.200 | 0.444 |
| os-scm | 41 | 0.839 | <0.001 | 0.120 | 0.843 |
| oscs-scv | 40 | 0.985 | <0.001 | 0.093 | 0.602 |
| oscs-scm | 40 | 0.976 | <0.001 | -0.018 | 0.937 |
| oscd-scv | 41 | 0.880 | <0.001 | 0.007 | 0.902 |
| oscd-scm | 41 | 0.876 | <0.001 | 0.049 | 0.882 |
Table 4. Correlation and differences between the first and second measurements in control group.
| Variable | Correlation | Paired difference | |||
|---|---|---|---|---|---|
| n | r | p | Mean | p | |
| ou-scv | 40 | 0.848 | <0.001 | -0.003 | 0.842 |
| ou-scm | 40 | 0.290 | 0.069 | 0.490 | 0.001 |
| od-scv | 40 | 0.943 | <0.001 | -0.034 | 0.146 |
| od-scm | 40 | 0.664 | <0.001 | -0.073 | 0.531 |
| odcd-scv | 40 | 0.897 | <0.001 | -0.029 | 0.330 |
| odcd-scm | 40 | 0.511 | 0.001 | 0.025 | 0.839 |
| odcs-scv | 40 | 0.923 | <0.001 | -0.005 | 0.834 |
| odcs-scm | 40 | 0.487 | 0.001 | 0.073 | 0.669 |
| os-scv | 40 | 0.871 | <0.001 | -0.002 | 0.947 |
| os-scm | 40 | 0.572 | <0.001 | -0.002 | 0.982 |
| oscs-scv | 40 | 0.879 | <0.001 | 0.037 | 0.207 |
| oscs-scm | 40 | 0.444 | 0.004 | 0.233 | 0.146 |
| oscd-scv | 40 | 0.798 | <0.001 | 0.021 | 0.478 |
| oscd-scm | 40 | 0.635 | <0.001 | 0.181 | 0.071 |
ROC analysis
The ROC curve illustration was generated for the first and second measurement for the os-csm variable (Fig. 4). Regarding the first measurement with the cut-off value of 1.950, the sensitivity and specificity of the instrument was 82.9% and 62.5%, respectively. Maximum AUC was 0.789 (95% confidence interval (CI), 0.701 to 0.894). In the second measurement, the cut-off value was 2.050, while the sensitivity and specificity was 78.0% and 72.5%, respectively. Maximum AUC was 0.809 (95% CI, 0.713 to 0.904). Thus, the results of the first measurement were considered good, and of the second measurement very good. The ROC curve statistics for all the variables measured are shown in Table 5. According to the results on AUC, it is seen that all measurements could be used for diagnosing strabismus. All the measurements are listed according to their diagnostic capability ranging from average to excellent. For diagnosing strabismus, the greatest certainty was achieved with the odcd and oscs variables, with their AUC values almost 1, and their sensitivity and specificity above 90% and close to 100%, respectively.
Fig. 4.
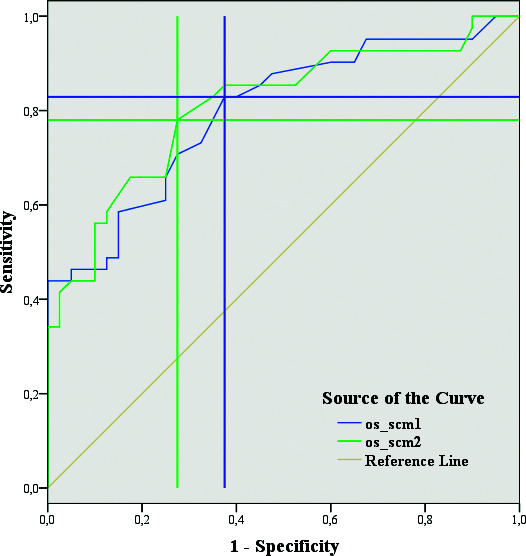
Receiver operating characteristic curve for the first and second measurement of the os-scm variable (maximal value of eye deviation in degrees after eye tracking of the left eye without eyeglass correction while the right eye is covered with the occluder). The chosen points are in the middle of horizontal and vertical line crossing.
Table 5. Receiver operating characteristic curve statistics.
| Variable | AUC | SE | 95% CI | Sensitivity (%) | Specificity (%) | Cut-off value | |
|---|---|---|---|---|---|---|---|
| h1 | h2 | ||||||
| ou-scv1 | 0.780 | 0.053 | 0.676 | 0.884 | 80.5 | 70.0 | 0.505 |
| ou-scv2 | 0.787 | 0.053 | 0.683 | 0.891 | 63.4 | 92.5 | 0.730 |
| ou-scm1 | 0.724 | 0.057 | 0.613 | 0.835 | 75.6 | 65.0 | 1.450 |
| ou-scm2 | 0.827 | 0.049 | 0.732 | 0.923 | 75.6 | 85.0 | 1.350 |
| od-scv1 | 0.713 | 0.062 | 0.593 | 0.834 | 66.7 | 80.0 | 1.050 |
| od-scv2 | 0.706 | 0.064 | 0.582 | 0.831 | 66.7 | 85.0 | 1.385 |
| od-scm1 | 0.792 | 0.051 | 0.691 | 0.893 | 71.8 | 75.0 | 2.400 |
| od-scm2 | 0.752 | 0.055 | 0.645 | 0.858 | 69.2 | 72.5 | 2.250 |
| odcd-scv1 | 0.973 | 0.021 | 0.000 | 1.000 | 92.5 | 100.0 | 2.305 |
| odcd-scv2 | 0.991 | 0.007 | 0.000 | 1.000 | 95.0 | 97.5 | 1.810 |
| odcd-scm1 | 0.969 | 0.023 | 0.000 | 1.000 | 92.5 | 97.5 | 4.050 |
| odcd-scm2 | 0.994 | 0.006 | 0.000 | 1.000 | 97.5 | 100.0 | 3.800 |
| odcs-scv1 | 0.657 | 0.062 | 0.535 | 0.779 | 50.0 | 85.0 | 1.105 |
| odcs-scv2 | 0.654 | 0.063 | 0.531 | 0.778 | 67.5 | 67.5 | 0.915 |
| odcs-scm1 | 0.636 | 0.063 | 0.513 | 0.760 | 67.5 | 67.5 | 1.850 |
| odcs-scm2 | 0.652 | 0.061 | 0.532 | 0.772 | 65.0 | 65.0 | 1.300 |
| os-scv1 | 0.827 | 0.045 | 0.739 | 0.914 | 63.4 | 87.5 | 1.285 |
| os-scv2 | 0.784 | 0.051 | 0.684 | 0.884 | 65.9 | 85.0 | 1.110 |
| os-scm1 | 0.789 | 0.049 | 0.701 | 0.894 | 82.9 | 62.5 | 1.950 |
| os-scm2 | 0.809 | 0.049 | 0.713 | 0.904 | 78.0 | 72.5 | 2.050 |
| oscs-scv1 | 0.998 | 0.002 | 0.000 | 1.000 | 97.5 | 97.5 | 1.730 |
| oscs-scv2 | 0.997 | 0.003 | 0.000 | 1.000 | 97.5 | 97.5 | 1.885 |
| oscs-scm1 | 0.982 | 0.013 | 0.000 | 1.000 | 92.5 | 97.5 | 4.350 |
| oscs-scm2 | 0.989 | 0.011 | 0.000 | 1.000 | 97.5 | 100.0 | 3.950 |
| oscd-scv1 | 0.694 | 0.059 | 0.579 | 0.809 | 82.9 | 55.0 | 0.605 |
| oscd-scv2 | 0.726 | 0.055 | 0.618 | 0.835 | 97.6 | 35.0 | 0.495 |
| oscd-scm1 | 0.727 | 0.056 | 0.618 | 0.836 | 43.9 | 90.0 | 2.450 |
| oscd-scm2 | 0.784 | 0.050 | 0.687 | 0.882 | 68.3 | 72.5 | 1.550 |
1 and 2 = first and second measurement; AUC = area under the curve; SE = standard error; 95% CI = 95% confidence interval; variables described in Table 1
Discussion
This study results demonstrated the effectiveness of diagnosing manifest strabismus with a computer-based eye-tracking system in children and adults, compared to the standard ophthalmologic examination. Comparison of the results of standard ophthalmologic examination with cover test and those achieved by using a computer-based measurement showed a strong positive correlation. A higher AUC was found using ROC curve analysis for the odcd and oscs variables having AUC values almost 1 and their sensitivity and specificity above 90% and close to 100%, respectively. The included patients were either control subjects, where strabismus was excluded through standard ophthalmic examination, or manifest strabismic patients diagnosed by the same ophthalmic examination. The results showed highest sensitivity and specificity in those variables, which, according to the standardized evident strabismus testing with cover/uncover test, as expected, highlighted eye misalignment or eye movement itself (42-45). Strabismus could easily be misdiagnosed in children if the angles are small, or in intermittent esodeviation. More than that, there is a need for an objective test being accurate and effective enough for screening purposes (46-48). Based on our previous work on the possible use of computer-based technology, we have envisaged the possibility of testing manifest strabismus patients and comparing the results with manual ones in the control group. The computer-based measurements showed an excellent correlation with manual measurements. Accurate assessment of the strabismus angle, using a prism and cover tests, requires a skilled examiner. The strabismus angle is an essential criterion for the choice of surgical procedure. The measurement results are often subject to variations, resulting in repeated testing to obtain high-quality data (3). The measurements in the office settings and at home, in an everyday situation, could be helpful. Some of the small angle intermittent esotropia patients could progress to constant (in several months) esotropia patients, while other misdiagnosed patients could develop amblyopia (9, 10, 49). Detecting strabismus by using manual methods, including the gold standard prism/cover tests and Krimsky test, are strongly dependent on the expertise of a skilled professional, as well as on their ability to estimate ocular misalignment (50). It is a known fact that the interobserver variability fluctuates for the prism cover test, but both Hirschberg and Krimsky test are even more prone to having less accurate results (9, 10). The surrounding elements and patient health, anxiety, attention, and age affect several factors necessary for adequate results (51, 52). In our study, a computer-based system using the eye-tracking method showed good diagnostic accuracy on detecting strabismus. With a computer-based eye-tracker, the testing becomes a noninvasive and simple procedure, measuring ocular alignment and ocular movement. The ocular filter and eye-tracking device used, coupled with a simple computer are inexpensive tools. These coupled with additional software offer the possibility of application in clinical practice (37).
Our present study, though, had several limitations, primarily regarding patient selection. We looked at manifest strabismus and excluded latent strabismus because we designed the study to test the functionality of the device first. We will include the latent type of strabismus in our next study. Secondly, a small number of young participants highlighted the need for further studies enrolling children aged 4-6 years in the screening population (18). Nevertheless, strabismus was confirmed in all included patients, stressing the sensitivity and specificity of the eye-tracking. Having in mind the potential amblyogenic effect of strabismus, the eye-tracker passed the initial test in children with an angle of >8 prism diopter (18). Statistical analysis showed complete overlapping of the manual and computer-based eye misalignment measurements. The former was done by a skilled professional, and the latter by a resident. To conclude, a computer-based eye-tracker device using additional filters as eye occluders does not require a skilled examiner. Yet, it offers the possibility of detecting strabismus even in young children, having the potential for use in screening.
Conclusion
According to the results of our study, an eye-tracking based computer system using selective wavelength occluder can detect manifest strabismus with high sensitivity and specificity, without a skilled examiner. There was a strong positive correlation between the manual measurement results and those done by the eye-tracking system. Therefore, this method could be a reliable tool for screening strabismus. Further research should test the system in diagnosing latent strabismus.
References
- 1.Attebo K, Mitchell P, Cumming R, Smith W, Jolly N, Sparkes R. Prevalence and causes of amblyopia in an adult popula-tion. Ophthalmology. 1998;105:154–9. 10.1016/S0161-6420(98)91862-0 [DOI] [PubMed] [Google Scholar]
- 2.Assaf AA. The sensitive period: transfer of fixation after occlusion for strabismic amblyopia. Br J Ophthalmol. 1982;66:64–70. 10.1136/bjo.66.1.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Von Noorden GK. Binocluar vision and ocular motility. 4th edn. St. Louis: Mosby; 1990. [Google Scholar]
- 4.Simons K. Preschool vision screening rationale, methodology and outcome. Surv Ophthalmol. 1996;41:3–30. 10.1016/S0039-6257(97)81990-X [DOI] [PubMed] [Google Scholar]
- 5.Pediatric Eye Disease Investigator Group . A randomized trial of atropine versus patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–78. 10.1001/archopht.120.3.268 [DOI] [PubMed] [Google Scholar]
- 6.Flynn JT, Woodruff G, Thompson JR, Hiscox F, Feuer W, Schiffma J, et al. The therapy of amblyopia: an analysis comparing the results of amblyopia therapy utilizing two pooled data sets. Trans Am Ophthalmol Soc. 1999;97:373–90. [PMC free article] [PubMed] [Google Scholar]
- 7.Fulton AB, Mayer DL. Esotropic children with amblyopia: effects of patching on acuity. Graefes Arch Clin Exp Ophthalmol. 1988;226:309–12. 10.1007/BF02172956 [DOI] [PubMed] [Google Scholar]
- 8.Schmucker C, Grosselfinger R, Riemsma R, Antes G, Lange S, Lagreze W, et al. Diagnostic accuracy of vision screening tests for the detection of amblyopia and its risk factors: a systematic review. Graefes Arch Clin Exp Ophthalmol. 2009;247:1441–54. 10.1007/s00417-009-1150-2 [DOI] [PubMed] [Google Scholar]
- 9.Choi BC. Slopes of a receiver operating characteristics curve and likelihood ratios for a diagnostic test. Am J Epidemiol. 1998;148:1127–32. 10.1093/oxfordjournals.aje.a009592 [DOI] [PubMed] [Google Scholar]
- 10.Pediatric Eye Disease Investigator Group . Interobserver reliability of the prism and alternate cover test in children with esotropia. Arch Ophthalmol. 2009;127:59–65. 10.1001/archophthalmol.2008.548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Association for Pediatric Ophthalmology and Strabismus . Eye care for the children of America. J Pediatr Ophthalmol Strabismus. 1991;28:64–7. 10.3928/0191-3913-19910301-03 [DOI] [PubMed] [Google Scholar]
- 12.Hartmann EE, Dobson V, Hainline L, Marsh-Tootle W, Quinn GE, Ruttum MS, et al. Preschool vision screening summary of a task force report. Pediatrics. 2000;106:1105–16. 10.1542/peds.106.5.1105 [DOI] [PubMed] [Google Scholar]
- 13.Ciner EB, Dobson V, Schmidt PP, Allen D, Cyert L, Maguire M, et al. A survey of vision screening policy of preschool children in the United States. Surv Ophthalmol. 1999;43:445–57. 10.1016/S0039-6257(99)00021-1 [DOI] [PubMed] [Google Scholar]
- 14.Pesudovs K, Weisinger SH. A comparison of autorefractor performance. Optom Vis Sci. 2004;81:554–8. 10.1097/00006324-200407000-00018 [DOI] [PubMed] [Google Scholar]
- 15.Choi M, Weiss S, Schaeffel F, Seidemann A, Howland HC, Wilhelm B, et al. Laboratory clinical and kindergarten test of a new eccentric infrared photorefractor (Powerrefractor). Optom Vis Sci. 2000;77:537–48. 10.1097/00006324-200010000-00008 [DOI] [PubMed] [Google Scholar]
- 16.Atkinson J, Braddick O. The use of isotropic photorefraction for vision screening in infants. Acta Ophthalmol Suppl. 1983;157:36–45. 10.1111/j.1755-3768.1983.tb03929.x [DOI] [PubMed] [Google Scholar]
- 17.Atkinson J, Braddick O, Robier B, Anker S, Ehrlich D, King J, et al. Two infant vision screening programmes: prediction and prevention of strabismus and amblyopia from photo- and videorefractive screening. Eye (Lond). 1996;10:189–98. 10.1038/eye.1996.46 [DOI] [PubMed] [Google Scholar]
- 18.Donahue SP, Arthur B, Neely DE, Arnold RW, Silbert D, Ruben JB, et al. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013;17:4–8. 10.1016/j.jaapos.2012.09.012 [DOI] [PubMed] [Google Scholar]
- 19.Peterseim MM, Papa CE, Wilson ME, Davidson JD, Shtessel M, Husain M, et al. The effectiveness of the spot vision screener in detecting amblyopia risk factors. J AAPOS. 2014;18(6):539–42. 10.1016/j.jaapos.2014.07.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arana Mendez M, Arguello L, Martinez J, Salas Vaargas M, Alvarado Rodriguez AM, Papa CE, et al. Evaluation of the spot vision screener in young children in Costa Rica. J AAPOS. 2015;19:441–4. 10.1016/j.jaapos.2015.08.002 [DOI] [PubMed] [Google Scholar]
- 21.Marzolf AL, Peterseim MM, Forcina BD, Papa C, Wilson ME, Cheeseman EW, et al. Use of the spot vision screener for patients with developmnetal disability. J AAPOS. 2017;21:313–5.e1. 10.1016/j.jaapos.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 22.Forcina BD, Peterseim MM, Wilson ME, Cheeseman EW, Feldman S, Marzolf AL, et al. Performance of the spot vision screeners in children younger than 3 years of age. Am J Ophthalmol. 2017;178:79–83. 10.1016/j.ajo.2017.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang HK, Han SB, Hwang JM, Kim YJ, Jeong CB, Kim KG. Assessment of binocular alignment using the three-dimensional strabismus photo analyzer. Br J Ophthalmol. 2012;96:78–82. 10.1136/bjophthalmol-2011-300305 [DOI] [PubMed] [Google Scholar]
- 24.Houben MM, Goumans J, van der Steen J. Recording three dimensional eye movements: scleral search coil versus video oculography. Invest Ophthalmol Vis Sci. 2006;47:179–87. 101167/iovs.05-0234 10.1167/iovs.05-0234 [DOI] [PubMed] [Google Scholar]
- 25.Crawford JD, Ceylan MZ, Kher EM, Guitton D. Three-dimensional eye-head coordination during gaze saccades in the primate. J Neurophysiol. 1999;81:1760–82. 10.1152/jn.1999.81.4.1760 [DOI] [PubMed] [Google Scholar]
- 26.Knapp RB, Hake LE, Lusted HS. Method and apparatus for eye tracking for convergence and strabismus measurement. U.S. Patent 5491492, 1996.
- 27.Ciuffreda KJ, Tannen B. Eye Movement Basics for the Clinician. St. Louis: Mosby; 1995. [Google Scholar]
- 28.Young LR, Sheena D. Eye-movement measurement techniques. Am Psychol. 1975;30:315–30. 10.1037/0003-066X.30.3.315 [DOI] [PubMed] [Google Scholar]
- 29.Kim S, Lombardino LJ, Cowles W, Altmann LJ. Investigating graph comprehension in students with dyslexia: an eye tracking study. Res Dev Disabil. 2014;35:1609–22. 10.1016/j.ridd.2014.03.043 [DOI] [PubMed] [Google Scholar]
- 30.Orlosky J, Itoh Y, Ranchet M, Kiyokawa K, Morgan J, Devos H. Emulation of physician tasks in eye-tracked virtual reality for remote diagnosis of neurodegenerative disease. IEEE Trans Vis Comput Graph. 2017;23:1302–11. 10.1109/TVCG.2017.2657018 [DOI] [PubMed] [Google Scholar]
- 31.Atam S, Khan A, Khiyal MSH. Design and implementation of human computer interface tracking system based on multiple eye features. J Theor Appl Inf Technol. 2009;9:155-61. https:// 10.13140/2.1.3647.0403 10.13140/2.1.3647.0403 [DOI]
- 32.Morimoto C, Mimica M. Eye gaze tracking techniques for interactive application. Comput Vis Image Underst. 2005;98:4–24. 10.1016/j.cviu.2004.07.010 [DOI] [Google Scholar]
- 33.Reulen JP, Marcus JT, Kopps D, de Vries FR, Tiessinga G, Boshuizen K, et al. Precise recording of eye movement: the IRIS technique. Part 1. Med Biol Eng Comput. 1988;26:20–6. 10.1007/BF02441823 [DOI] [PubMed] [Google Scholar]
- 34.Guyton DL, Moss A, Simons K. Automated measurement of strabismic deviation using a remote haploscope and an infrared television-based eyetracker. Trans Am Ophthalmol Soc. 1987;85:320–31. [PMC free article] [PubMed] [Google Scholar]
- 35.Schiavi C, Orciuolo M. Automated measurement of strabismic deviation. Curr Opin Ophthalmol. 1992;3:731–4. 10.1097/00055735-199212000-00002 [DOI] [PubMed] [Google Scholar]
- 36.Model D, Eizenman M. An automated Hirschberg test for infants. IEEE Trans Biomed Eng. 2011;58:103–9. 10.1109/TBME.2010.2085000 [DOI] [PubMed] [Google Scholar]
- 37.Grubišić I, Grbeša I, Lipić T, Skala K, Zrinšćak O, Iveković R, et al. Natural eye gaze computer interaction for medical oculography diagnosis: current status and future prospects. MIPRO 2014: Proceedings of the 37th International Convention on Information and Communication Technology, Electronics and Microelectronics 2014; 421-5. 10.1109/MIPRO.2014.6859603 10.1109/MIPRO.2014.6859603 [DOI] [Google Scholar]
- 38.Pediatric Eye Disease Investigator group . Interobserver reliability of the prism and alternate cover test in children with esotropia. Arch Ophthalmol. 2009;127:59–65. 10.1001/archophthalmol.2008.548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Diepen PMJ. New data-acqusition software for Leuven dual-PC controlled Purkinje eye-tracking system. Psych Rep. 1998;246. [Google Scholar]
- 40.Van Rensbergen J, De Troy A. A reference for Leuven dual-PC controlled Purkinje eye-tracking system. Psych Rep. 1993;145. [Google Scholar]
- 41.Choi BC. Slopes of a receiver operating characteristic curve and likelihood ratios for diagnostic test. Am J Epidemiol. 1998;148:1127–32. 10.1093/oxfordjournals.aje.a009592 [DOI] [PubMed] [Google Scholar]
- 42.Gamble JD. Identifying deviations by the cover test. Opt J Rev Optom. 1950. August 15;87(16):31. [PubMed] [Google Scholar]
- 43.McKean HE, Wirtschafter JD, Marx D. Bias of the cover test in the diagnosis of alternating tropia. Ann Ophthalmol. 1976;8:435–7. [PubMed] [Google Scholar]
- 44.Romano PE. Individual case photogrammetric calibration of the Hirschberg Ratio (HR) for corneal light reflection test strabometry. Binocul Vis Strabismus Q. 2006;21:45–6. [PubMed] [Google Scholar]
- 45.Scott AB. Editorial: Strabismus – beyond the cover test. Invest Ophthalmol. 1973;12:719–20. [PubMed] [Google Scholar]
- 46.Williams C, Harrad RA, Harvey I, Sparrow JM, ALSPAC Study Team . Screening for amblyopia in preschool children: results of a population-based, randomised controlled trial. ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. Ophthalmic Epidemiol. 2001;8:279–95. 10.1080/09286586.2001.11644257 [DOI] [PubMed] [Google Scholar]
- 47.Gräf M, Alhammouri Q, Vieregge C, Lorenz B. The Bruckner transillumination test: limited detection of small-angle esotropia. Ophthalmology. 2011;118:2504–9. 10.1016/j.ophtha.2011.05.016 [DOI] [PubMed] [Google Scholar]
- 48.Han S, Kim US. Symptom based diagnosis of infant under one year in outpatient clinic. Korean J Ophthalmol. 2014;28:241–5. 10.3341/kjo.2014.28.3.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fu VL, Stager DR, Birch EE. Progression of intermittent small-angle and variable esotropia in infancy. Invest Ophthalmol Vis Sci. 2007;48:661–4. 10.1167/iovs.06-0717 [DOI] [PubMed] [Google Scholar]
- 50.Hrynchak PK, Herriot C, Irving EL. Comparison of alternate cover test reliability at near in non-strabismus between experienced and novice examiners. Ophthalmic Physiol Opt. 2010;30:304–9. 10.1111/j.1475-1313.2010.00723.x [DOI] [PubMed] [Google Scholar]
- 51.Von Noorden GK. Binocular vision and ocular motility: theory and management of strabismus. St. Louis: Mosby; 1990. [Google Scholar]
- 52.Yang HK, Hwang JM. The effect of target size and accommodation on the distant angle of deviation in intermittent exotropia. Am J Ophthalmol. 2011;151:907–13.e1. 10.1016/j.ajo.2010.11.021 [DOI] [PubMed] [Google Scholar]