Posttraumatic pneumonectomy is a highly morbid and lethal event.
Central Message.
Posttraumatic pneumonectomy is a highly morbid and lethal event. Postoperative use of venovenous ECMO and serial washouts for a contaminated pleural space is an effective treatment strategy.
See Commentary on page 280.
Posttraumatic pneumonectomy is a rare event that carries extremely high morbidity and mortality.1, 2, 3 The optimal management for posttraumatic pneumonectomy is not well delineated, given the uncommon circumstances.4,5 This case had added complexity with involvement of the complex tracheal reconstruction and introduction of contaminated soil into the mediastinum and pleural space due to the traumatic nature of the injury. In the setting of a pneumonectomy, a contaminated pleural space, in and of itself, is a known deadly complication, with mortality rates ranging from 25% to 50%.6, 7, 8 Serial washouts and packing with iodinated gauze have been described for management of non–trauma-related early and late postpneumonectomy empyema.9,10 A contaminated pleural space in an already highly fatal situation with multiorgan trauma secondary to a motor vehicle crash (MVC) elevates the complexity of the situation. The ability to control a traumatically contaminated space allows for ongoing trauma care including patient mobilization to aid recovery.
Pulmonary contusions and acute respiratory distress syndrome (ARDS) are well-known problems following an MVC.11, 12, 13 However, after an emergent pneumonectomy, pulmonary contusions and ARDS of the remaining lung can be disastrous, where ARDS after pneumonectomy carries a mortality rate of 47% to 56%.14, 15, 16 Venovenous extracorporeal membrane oxygenation (V-V ECMO) has been used in the settings of ARDS,17,18 traumatic lung injury,19,20 and complex tracheal reconstruction21,22 as a bridge to recovery; this case involved all 3.
Case Description
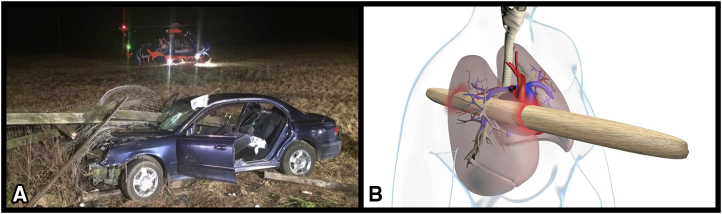
University of Florida, UF Health Shands, and patient written informed consent and authorization to use and disclose deidentified health information for publication and educational purposes was obtained (institutional review board #202000163, approval date February 19, 2020). The patient was a 14-year-old, restrained driver of a single-car motor vehicle crash into a horse farm fence at highway speed resulting in penetrating thoracic trauma with impalement of a wooden fence board via a right parasternal entry site and right paraspinal exit site (Figure 1). The patient had a prolonged extrication time over 1 hour due to her impalement injury and arrived to the emergency department with the wooden fence through-and-through her chest such that she could not lay flat, a Glasgow Coma Scale of 14, blood pressure 150/110 mm Hg, heart rate 142, temperature 33.8 °C, and oxygen saturation of 88% on a nonrebreather mask. She was subsequently intubated and resuscitated in the trauma bay, which improved her oxygen saturations and tachycardia. She was then brought emergently to the operating room for the traumatic thoracic injury. She did not undergo any imaging or chest tube placement in the emergency department for fear of delaying definitive care and/or disrupting the injuries already present.
Figure 1.
A, Image at the scene of the car shown with the fence through the windshield. B, Graphical depiction of injury with the anterior red highlighted area on the skin depicting the right parasternal entry site and posterior red highlighted area depicting the right paraspinal exit site. The impalement was just lateral to the heart.
Once in the operation room (Video 1), the patient was positioned with a bump on the right side due to an inability to lay flat secondary to the fence protruding through her back wound. The fence piece was from a horse farm, and inspection of the wood revealed animal hair, soil, and mold (Figure 2, A). In addition, her shirt had to be cut around the fence, and part of her shirt could also be seen passing through her chest and exiting the back. A preoperative plan entailed a right thoracotomy with the option for a clamshell extension, if needed. Additional preparation involved a left groin cutdown for emergent access to the femoral vessels in the case that cardiopulmonary bypass was required.
Figure 2.
A, Traumatic impalement injury with right parasternal entry site and right paraspinal exit site. B, Surgical image status post right thoracotomy and right middle and lower lobectomy, before removal of the foreign body. C, Surgical image showing cross-table ventilation for complex tracheoplasty.
After right anterolateral thoracotomy, a large volume air leak was noted, but no active bleeding. The anesthesiologists completed a flexible fiberoptic bronchoscopy and it appeared the right mainstem was compressed and unable to be visualized, and subsequently the endotracheal tube was advanced into the left mainstem in preparation for further surgical exploration. There were small fragments of the wooden shards from the fence freely inside her chest cavity, as well as fragments of cloth from the patient's shirt. The pericardium was noted to be torn by the impalement, but the heart was without injury. The pericardium was further opened to have access to the intrapericardial pulmonary artery and veins for vascular control. Right middle and lower lobectomies were performed promptly, as they both appeared to have been transected away from the hilum by the wooden piece and were no longer attached secondary to the traumatic injury. We then noted that the right upper lobe was severely congested. Before removal of the foreign body, vascular clamps and staplers were made available. Cardiac anesthesia, perfusionist, trauma surgeon, cardiac surgeon, thoracic surgeon, cardiothoracic surgery scrub technicians, and circulators coordinated the removal of the foreign body (Figure 2, B). The video accompanying this article shows the active removal of the fence and additional intraoperative images.
After removal of the foreign body, the right superior pulmonary vein was noted to have already been transected and sealed by the fence board, which is why it was so congested in appearance. As the right upper lobe appeared infarcted, an expeditious right upper lobectomy was then performed. Now with full visualization, the source of the air leak could be identified. The right main stem bronchus was three-fourths detached from the carina with an associated inferior carinal injury. The residual right mainstem was debrided to healthy tissue while cross field ventilation was used (Figure 2, C). The right mainstem remnant was used a cartilaginous flap onto the carinal injury and sutured in placed. An intercostal muscle flap was placed to protect the complex tracheal reconstruction.
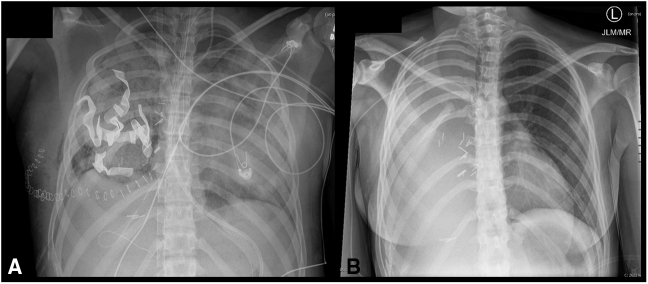
At the conclusion of the operation, the patient was placed on V-V ECMO for a multitude of reasons. First, the patient was status post-MVC with prolonged extrication who required large-volume resuscitation with crystalloid and 4 units of packed red bloods cells, as well as having severe pulmonary contusions of the remaining lung. These combined contributed to postoperative hypoxia. Second, for protection of the complex tracheal reconstruction, it was felt that low positive end-expiratory pressure would be ideal for healing of the tracheal wound. She underwent right internal jugular vein and right femoral venous cannulation with an 18-Fr cannula in the internal jugular vein and 25-Fr cannula in the groin. At our institution, we preferentially use 2 separate venous cannulas, as we have anecdotally had had some trouble with flows using a single-catheter VV-ECMO cannula. Her postoperative radiograph is seen in Figure 3, A. This image shows a closed chest with gauze packing in right chest space, chest tube in place, V-V ECMO cannulas in the superior vena cava and inferior vena cava, and a left lung with severe pulmonary contusions and volume overload. We also considered placing the patient on venoarterial ECMO (V-A ECMO), assuming that she might experience postpneumonectomy right heart strain. Due to relative stability of her hemodynamics postoperatively, we elected to pursue V-V ECMO to decrease the need for anticoagulation that is needed for V-A ECMO in this trauma patient.
Figure 3.
A, Postoperative image showing povidone–iodine-soaked gauze packing in right chest space with chest tube in place within the sponges and closed chest with staples. In addition, venovenous extracorporeal membrane oxygenation cannulas can be seen in the superior vena cava and inferior vena cava. The left lung is noted to have severe pulmonary contusions and volume overload after large volume resuscitation and postpneumonectomy. B, Follow-up chest radiograph image as an outpatient showing normalized left lung and right pneumonectomy site that is appropriately fluid-filled.
Not surprisingly, transthoracic echocardiogram on postoperative day 1 revealed a severely dilated right ventricle with depressed right ventricular systolic function. The patient was extubated on postinjury day 3 and ambulated daily in the intensive care unit with support from the intensive care unit providers, nurses, and physical/occupational therapy. By postinjury day 6, her echocardiogram exhibited some recovery with now a moderately dilated right ventricle and improved systolic function while on a milrinone drip. Her right ventricular size and function had normalized on the echocardiogram obtained on postinjury day 16 on no support. Ultimately, she was decannulated from ECMO 25 days after her injury. Figure 3, B, shows her chest radiograph after discharge.
The impalement from the fence not only caused significant direct injury to the patient's lung, but additionally it introduced gross contamination into the pleural space. The dirty fence went through-and-through the patient's body, and pieces of her shirt were also noted inside the chest cavity as well. The fence was from a horse farm, and upon direct inspection of the wood was noted animal hair, soil, and mold. Small shards of the fence were inside the chest cavity as well. For management of her severely contaminated pleural space, the patient required 6 washouts and debridements with iodine–povidone- soaked gauze packs, and broad-spectrum antibiotic and fungal coverage. This approach has been described by Schneiter and colleagues9,10 for postpneumonectomy empyema, and was adapted for use in this traumatic setting. The patient underwent reopening of the closed thoracotomy incision, debridement of the pleural cavity, irrigation, and packing with diluted povidone–iodine:normal saline (1:10)-soaked gauze sponges. The chest is then fully closed, and the pleural tube is then placed on suction. The pleural tube is surrounded by the gauze, which applies a negative pressure wound therapy to the pleural space via suction on the gauze (Figure 3, A). This process is repeated every 48 to 72 hours until the chest cavity is macroscopically clean. By macroscopically clean, in our case meant there were no longer deposits of gelatinous or fibrinous material on the gauze, foul smell, or green coloration to the sponges as there had been in previous washouts.
Finally, the chest cavity was obliterated with antibiotic solution and the thoracotomy incision definitively closed. The final closing of her chest was accomplished on postinjury day 20. She was maintained on V-V ECMO throughout the process of the serial washouts to preserve the tracheal repair even during intubation for the debridements. She was discharged postinjury day 63 and made a full recovery. The patient is now 3 years status post-MVC and pneumonectomy doing well as an outpatient. She was positive for the severe acute respiratory syndrome coronavirus 2 (coronavirus disease 2019) in December 2020, received remdesivir, and made a full uneventful recovery.
Discussion
Posttraumatic pneumonectomy is a rare event with potential for high morbidity and mortality. Pneumonectomy alone carries a high risk, but the additive risk of injuries from a high-speed MVC elevates the hazards for recovery. Although lung-sparing techniques are associated with improved outcomes compared with anatomic resection for severe lung injuries,23 this case required an emergent completion pneumonectomy with carinal reconstruction due to the location of the injury. The addition of the complex tracheal intervention and the grossly contaminated pleural space creates a potentially lethal situation. We had placed the patient on V-V ECMO after the completion of the operation, but looking back, could have placed the patient on V-V ECMO before tracheal reconstruction. In addition, her eventual normalization of right heart function confirmed our decision to not use V-A ECMO, although it was certainly considered at the time.
Serial washouts and packing with iodine solution of the pleural space until resolution of gross contamination has been previously described for management of non–trauma-related early and late postpneumonectomy empyema.9,10 The ability to control a traumatically contaminated space in this manner allowed for furthering of the ongoing trauma. The alternative would have been open packing and long-term wound-healing issues. The ability to temporarily close the pleural space after each wash out allowed for physical therapy and occupational therapy to advance the patient's recovery.
Furthermore, use of V-V ECMO for the enhancement in the patient's recovery was paramount. V-V ECMO allowed for early extubation and offered protection of the remaining lung and tracheal reconstruction by minimizing the positive pressure ventilation. While cannulated on ECMO, the critical care team, nursing, and therapy continued to mobilize the patient and walk the intensive care unit hallways. Ambulation in an ECMO patient takes extraordinary support and buy-in from all parties involved. This complex case highlights the importance of teamwork and highly specialized, advanced, multidisciplinary care. Overall, this dramatic case demonstrates the valuable use of V-V ECMO support after traumatic injury and complex tracheal reconstruction, as well as the confirms that serial washouts with iodine-soaked gauze for a contaminated pleural space can be an effective treatment strategy.
Acknowledgments
We acknowledge the entire staff of UF Health, including the first responders, emergency and trauma services, the operating room staff and perfusion, critical care teams, and therapy services, and special thanks to Carlos Campos for graphic design.
Footnotes
Funded by the Department of Surgery, Division of Thoracic and Cardiovascular Surgery, University of Florida, Gainesville, Fla.
Drs Freeman and Pipkin contributed equally to this article.
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
Case presentation of thoracic impalement secondary to MVC versus fence with subsequent injuries identified, complex repair undertaken, V-V ECMO support, and management of contaminated pleural space. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00120-1/fulltext.
References
- 1.Homo R., Grigorian A., Lekawa M., Dolich M., Kuza C., Doben A., et al. Outcomes after pneumonectomy versus limited lung resection in adults with traumatic lung injury. Updates Surg. 2020;72:547–553. doi: 10.1007/s13304-020-00727-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matsushima K., Aiolfi A., Park C., Rosen D., Strumwasser A., Benjamin E., et al. Surgical outcomes after trauma pneumonectomy. J Trauma Acute Care Surg. 2017;82:927–932. doi: 10.1097/TA.0000000000001416. [DOI] [PubMed] [Google Scholar]
- 3.Stewart K., Urschel J., Nakai S., Gelfand E., Hamilton S. Pulmonary resection for lung trauma. Ann Thorac Surg. 1997;63:1587–1588. doi: 10.1016/s0003-4975(97)00442-6. [DOI] [PubMed] [Google Scholar]
- 4.Martin M., McDonald J., Mullenix P., Steele S., Demetriades D. Operative management and outcomes of traumatic lung resection. J Am Coll Surg. 2006;203:336–344. doi: 10.1016/j.jamcollsurg.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Huh J., Wall M., Estrera A., Solero E., Mattox K. Surgical management of traumatic pulmonary injury. Am J Surg. 2003;186:620–624. doi: 10.1016/j.amjsurg.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Wong P., Goldstraw P. Post-pneumonectomy empyema. Eur J Cardiothorac Surg. 1994;8:345–349. doi: 10.1016/1010-7940(94)90027-2. [DOI] [PubMed] [Google Scholar]
- 7.Ng C., Wan S., Lee T., Wan I., Arifi A., Yim A. Post-pneumonectomy empyema: current management strategies. ANZ J Surg. 2005;75:597–602. doi: 10.1111/j.1445-2197.2005.03417.x. [DOI] [PubMed] [Google Scholar]
- 8.Clark J.M., Cooke T., Brown L.M. Management of complications after lung resection: prolonged air leak and bronchopleural fistula. Thorac Surg Clin. 2020;30:347–358. doi: 10.1016/j.thorsurg.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schneiter D., Cassina P., Korom S., Inci I., Al-Abdullatief M., Dutly A., et al. Accelerated treatment for early and late postpneumonectomy empyema. Ann Thorac Surg. 2001;72:1668–1672. doi: 10.1016/s0003-4975(01)03083-1. [DOI] [PubMed] [Google Scholar]
- 10.Schneiter D., Grodzki T., Lardinois D., Kestenholz P., Wojcik J., Kubisa B., et al. Accelerated treatment of postpneumonectomy empyema: a binational long-term study. J Thorac Cardiovasc Surg. 2008;136:179–185. doi: 10.1016/j.jtcvs.2008.01.036. [DOI] [PubMed] [Google Scholar]
- 11.Cohn S.M., Dubose J.J. Pulmonary contusion: an update on recent advances in clinical management. World J Surg. 2010;34:1959–1970. doi: 10.1007/s00268-010-0599-9. [DOI] [PubMed] [Google Scholar]
- 12.Sutyak J.P., Wohltmann C.D., Larson J. Pulmonary contusions and critical care management in thoracic trauma. Thorac Surg Clin. 2007;17:11–23. doi: 10.1016/j.thorsurg.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Daurat A., Millet I., Roustan J.P., Maury C., Taourel P., Jaber S., et al. Thoracic Trauma Severity score on admission allows to determine the risk of delayed ARDS in trauma patients with pulmonary contusion. Injury. 2016;47:147–153. doi: 10.1016/j.injury.2015.08.031. [DOI] [PubMed] [Google Scholar]
- 14.Peretti M., Hervochon R., Loi M., Blanc K., Roche N., Alifano M. Predictors of post-pneumonectomy respiratory failure and ARDS: usefulness of normalized pulmonary artery diameter. Intensive Care Med. 2018;44:1357–1359. doi: 10.1007/s00134-018-5206-9. [DOI] [PubMed] [Google Scholar]
- 15.Blanc K., Zaimi R., Dechartres A., Lefebvre A., Janet-Vandroux A., Hamelin-Canny E., et al. Early acute respiratory distress syndrome after pneumonectomy: presentation, management, and short-and long-term outcomes. J Thorac Cardiovasc Surg. 2018;156:1706–1714. doi: 10.1016/j.jtcvs.2018.06.021. [DOI] [PubMed] [Google Scholar]
- 16.Blanc K., Dechartres A., Zaimi R., Lefebvre A., Janet-Vendroux A., Fournel L., et al. Patients experiencing early acute respiratory failure have high postoperative mortality after pneumonectomy. J Thorac Cardiovasc Surg. 2018;156:2368–2376. doi: 10.1016/j.jtcvs.2018.08.113. [DOI] [PubMed] [Google Scholar]
- 17.Combes A., Hajaga D., Capellier G., Demoule A., Lavoue S., Guervilly C., et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 18.Brodie D., Bacchetta M. Extracorporeal membrane oxygenation for ARDS in Adults. N Engl J Med. 2011;365:1905–1914. doi: 10.1056/NEJMct1103720. [DOI] [PubMed] [Google Scholar]
- 19.Robba C., Ortu A., Bilotta F., Lombardo A., Sekhon M., Gallo F., et al. Extracorporeal membrane oxygenation for adult respiratory distress syndrome in trauma patients: a case series and systematic literature review. J Trauma Acute Care Surg. 2017;82:165–173. doi: 10.1097/TA.0000000000001276. [DOI] [PubMed] [Google Scholar]
- 20.Guirand D., Okoye O., Schmidt B., Mansfield N., Aden J., Martin R., et al. Venovenous extracorporeal life support improves survival in adult trauma patients with acute hypoxemic respiratory failure: a multicenter retrospective cohort study. J Trauma Acute Care Surg. 2014;76:1275–1281. doi: 10.1097/TA.0000000000000213. [DOI] [PubMed] [Google Scholar]
- 21.Qiu Y., Chen Q., Wu W., Zhang S., Tang M., Chen Y., et al. Extracorporeal membrane oxygenation (ECMO)-assisted intratracheal tumor resection and carina reconstruction: a safer and more effective technique for resection and reconstruction. Thorac Cancer. 2019;10:1297–1302. doi: 10.1111/1759-7714.13007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lei J., Su K., Li X., Zhou Y., Han Y., Juang L., et al. ECMO-assisted carinal resection and reconstruction after left pneumonectomy. J Cardiothorac Surg. 2010;5:89. doi: 10.1186/1749-8090-5-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cothren C., Moor E.E., Biffl W.L., Franciose R.J., Offner P.J., Burch J.M. Lung-sparing techniques are associated with improved outcome compared with anatomic resection for severe Lung Injuries. J Trauma. 2002;53:483–487. doi: 10.1097/00005373-200209000-00015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Case presentation of thoracic impalement secondary to MVC versus fence with subsequent injuries identified, complex repair undertaken, V-V ECMO support, and management of contaminated pleural space. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00120-1/fulltext.