ABSTRACT
Aim
To understand the awareness of the willingness to be vaccinated and influencing factors of the new coronavirus vaccine (neo-crown vaccine) among medical personnel in North China and to provide a theoretical basis and application guidelines for the feasibility of coronavirus vaccination by medical personnel to guide the public to actively be vaccinated by taking initiative and obtaining a coronavirus vaccination as soon as possible.
Methods
From April 2021 to June 2021, medical staff in North China were selected to complete an online questionnaire survey using Questionnaire Star to analyze the willingness rate to be vaccinated with the new coronavirus vaccine, and the influencing factors were analyzed using binary logistic regression.
Results
Among 621 respondents, 85.7% were willing to be vaccinated after the launch of the new vaccine. In the questionnaire, respondents were asked to answer questions such as “Do you think it is better to receive as few vaccines as possible at the same time?,” “If I get the new coronavirus vaccine, I may have serious side effects.,” “The new coronavirus vaccine is safe.,” “Specifically, for the new coronavirus vaccine, do you think it is safe?,” and “Specifically, for the new coronavirus vaccine, do you think it is easy to administer?.” These beliefs have an important influence on the vaccination of medical staff with the new coronavirus vaccine in Northern China (OR = 1.610,95% CI: 1.055 ~ 2.456; OR = 1.715,95% CI: 1.164 ~ 2.526; OR = 0.401, 95% CI: 0.212 ~ 0.760; OR = 0.352,95% CI: 0.147 ~ 0.843; OR = 3.688,95% CI: 1.281 ~ 10.502, respectively; All P values < .05).
Conclusions
Medical staff have a high willingness to be vaccinated with the new coronavirus vaccine, which plays a positive role in the publicity of the vaccine.
KEYWORDS: New coronavirus vaccine, willingness to vaccinate, influencing factors, medical personnel
1. Introduction
Coronavirus disease 2019 (COVID-19) is an acute respiratory disease with rapid transmission, high pathogenicity and high mortality caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 was reported in more than 136 million patients in April 2021. Over 2 million patients have died from COVID-19.1 It is not only a major global public health emergency but also has a great negative impact on the economy and social lives of people worldwide. Although China has taken effective measures to control COVID-19, the risk of spread in some areas is still high, especially by asymptomatic individuals, who have a significant impact on the spread of COVID-19.2 At the same time, there is an ever-present risk of breakthrough infection with the new delta (δ) coronavirus variant strain from India. Vaccination has always been the most effective way to prevent infectious diseases. For COVID-19, which may coexist with humans for a long time, the development of the new coronavirus vaccine is particularly important. At the same time, the safety and effectiveness of the new coronavirus vaccine are the key factors affecting the epidemic prevention of the new coronavirus.3 At present, nearly 200 kinds of COVID-19 vaccines are in the preclinical research stage, and more than 90 kinds are in the clinical research stage. Three inactivated vaccines, one adenovirus vector vaccine and one recombinant protein vaccine in China have been urgently approved for marketing for population vaccination.4 Studies have shown that people’s knowledge of the disease affects their self-management and compliance with interventions, thus influencing the general population’s vaccination behavior.5 Therefore, novel coronavirus pneumonia and the new coronavirus vaccine are important factors that determine the current popularity of the new coronavirus vaccine. The population is aware of COVID-19, new coronavirus pneumonia and new coronavirus vaccines. In China, although the new coronavirus vaccine was fully launched in April 2021, the understanding of medical staff regarding the new coronavirus vaccine is still unclear. The high cognition of medical staff on the new coronavirus vaccine is of great significance for the prevention of breakthrough infections. Therefore, it is necessary to understand current medical staff’s understanding of COVID-19 and the new coronavirus vaccine and to guide medical staff to actively inoculate with it. This study took medical staff in North China as the research object and conducted an online questionnaire survey in April 2021 to understand the willingness of the medical staff to vaccinate with the new coronavirus vaccine and potential influencing factors to provide a basis for the further promotion of the vaccination plan for the new coronavirus vaccine and its specific implementation.
2. Materials and methods
2.1. Survey sample
The survey sample was from Inner Mongolia, Beijing and Hebei, and included current medical workers aged 18 to 60 years. A total of 663 people were surveyed, with 621 valid questionnaires returned and a response rate of 93.67%. Participants with missing main information and incomplete responses were excluded. Based on the formula n = (Z(1-α/2)/δ)2p(1-p) for the required sample size for the cross-sectional survey and the vaccination rate of P ≈ 80% obtained in a previous study,α = 0.05, and the absolute tolerance error forδ = 5%, Z(1-α/2) = 1.96; for this survey, the design effect Deff = 2, and considering the 20% missing visit rate, the minimum required sample size was calculated as 590 people.
2.2. Survey content
The survey included general information about medical personnel in North China (age, usual residence, sex, ethnicity, education, marital status, annual household income, smoking status, alcohol consumption, whether they had received nucleic acid testing for the novel coronavirus and nucleic acid testing results), understanding of new coronavirus pneumonia, understanding of the new vaccine without vaccination, and awareness of the new coronavirus vaccine. The specific survey questions are shown in Appendix.
2.3. Survey method
The study from a national multi-center study at Peking Union Medical College, and we only selected the northern China.The questionnaire was designed with reference to the literature and in accordance with the actual situation and was presurveyed after expert discussion. The results of the presurvey showed that the Cronbach’s α coefficient of the full questionnaire was 0.737. The Kaiser–Meyer–Olkin coefficient was 0.925. This indicates that the internal consistency and validity of the questionnaire was good. The questionnaire was revised, refined and finalized after the presurvey. Using the convenience sampling method and online survey, the questionnaire was designed through “Questionnaire Star” software, a two-dimensional code was generated, and the questionnaire was released to the medical staff in North China. The staff voluntarily participated in the online questionnaire survey.
2.4. Data analysis
The collected questionnaires were collated for information, and those with missing entries greater than 20% were excluded. SPSS 20.0 software was used to build a database and to statistically analyze indicators such as the proportion willing to be vaccinated. Factors influencing willingness to be vaccinated were first analyzed as independent variables using a 2-test for one-way analysis, and then binary logistic regression analysis was conducted to determine the independent factors. The test level was α = 0.05.
3. Results
3.1. Basic characteristics of the survey respondents
A total of 621 respondents were included, most of whom were women, accounting for 71.5%; Participants aged 18–30, 31–50 and ≥ 51 years accounted for 20.9%, 68.3% and 10.8%, respectively. Most of them lived in cities and towns, accounting for 97.7%, and most had a college degree or bachelor degree or above, accounting for 98.3%. Regarding marital status, most of the participants were married, accounting for 81.3%. The annual income was mostly 100000 yuan or less, accounting for 66.8%. The majority of participants were nonsmokers, accounting for 88.6%; nondrinkers accounted for 84.9%. Most of the participants had been tested for novel coronavirus nucleic acids, accounting for 90.3%. All participants nucleic acid test results were negative. The results are shown in Table 1.
Table 1.
Respondents’ general information
| Demographic characteristics | Total (n = 621) |
(%) | |
|---|---|---|---|
| Age (years) | 18 ~ 30 | 130 | 20.9 |
| 31 ~ 50 | 424 | 68.3 | |
| ≥51 | 67 | 10.8 | |
| Residence | Countryside | 14 | 2.3 |
| Towns | 607 | 97.7 | |
| Sex | Male | 177 | 28.5 |
| Female | 444 | 71.5 | |
| Ethnicity | Han Chinese | 534 | 86.0 |
| Other | 87 | 14.0 | |
| Education Level | Senior High School and below | 11 | 1.8 |
| Bachelor’s degree or college | 409 | 65.9 | |
| Postgraduate and above | 201 | 32.4 | |
| Marital status | Unmarried | 98 | 15.8 |
| Married | 505 | 81.3 | |
| Divorced or widowed | 18 | 2.9 | |
| Annual household income (yuan) | 100,000 and below | 415 | 66.8 |
| 110,000-3–50,000 | 195 | 31.4 | |
| >350,000 | 11 | 1.8 | |
| Smoking status | Yes | 71 | 11.4 |
| No | 550 | 88.6 | |
| Drinking status | Yes | 94 | 15.1 |
| No | 527 | 84.9 | |
| Q1 | Yes | 561 | 90.3 |
| No | 60 | 9.7 | |
| Q2 | Negative | 561 | 90.3 |
| Not tested | 60 | 9.7 | |
| Positive | 0 | 0.0 | |
3.2. Willingness to receive the new coronavirus vaccine
After the launch of the new coronavirus vaccine, the total number of medical staff in North China was 621, of which 532 (85.7%) were willing to receive or make an appointment to receive the new coronavirus vaccine; 89 (14.3%) staff members were unwilling to receive the new coronavirus vaccine.
3.3. Factors influencing willingness to be vaccinated
3.3.1. Univariate analysis
Univariate analysis showed that in the questionnaire, respondents were asked to answer questions such as “place of usual residence”; “whether I have been tested for novel coronavirus nucleic acids”; “nucleic acid test results”; “If I get the new coronavirus pneumonia, is it considered a high risk to my health.”; “If I do not get the new coronavirus vaccine, I have a high risk of getting the new coronavirus pneumonia.”; “If I do not get the new coronavirus vaccine, I will always be at risk of getting the new coronavirus pneumonia.”; “If I get the new coronavirus vaccine, my risk of getting the new coronavirus pneumonia will be reduced.”; “If everyone gets the new coronavirus vaccine, the prevalence of new coronavirus pneumonia can be reduced.”; “If I get the new coronavirus vaccine, my risk of getting the new coronavirus pneumonia will be reduced.”; “If I get the novel coronavirus, I may pass it on to family and friends who may contract the novel coronavirus.”; “If I get the novel coronavirus, I have a greater risk of dying.”; “I think getting the novel coronavirus vaccine will prevent the spread of the new coronavirus pneumonia to family members and relatives.”; “I think that vaccination with the new coronavirus vaccine will prevent financial and labor losses due to the new coronavirus.”; “I think the new coronavirus vaccination will instead cause me to the develop the new coronavirus pneumonia.”; “I believe that the outbreak in China is under control, so there is no longer a need for the new coronavirus vaccine.”; “Do you think that the new crown vaccination will prevent the new coronavirus pneumonia (which is a very serious disease)?”; “Do you think it is better to get immunity by having the new coronavirus pneumonia than by getting the new coronavirus vaccine?”; “Do you think it is better to receive as few vaccinations as possible at the same time?”; “I could have serious side effects if I get the vaccine.”; “The new coronavirus vaccine is necessary to protect our health.”; “The new coronavirus vaccine is good for preventing the new coronavirus pneumonia.”; “The new coronavirus vaccine is safe.”; “If I do not get the new coronavirus vaccine, I may get the new coronavirus pneumonia and cause others to contract it.”; “Specifically, for the new coronavirus vaccine, do you think it is necessary to get the new coronavirus vaccine?”; “Specifically, for the new coronavirus vaccine, do you think it is important?”; “Specifically, for the new coronavirus vaccine, do you think it is safe?”; “Specifically, for the new coronavirus vaccine, do you believe that it is effective?”; and “Specifically, for the new coronavirus vaccine, do you find the new coronavirus vaccine easy to administer?.” These were significant factors influencing the survey respondents’ willingness to be vaccinated after the launch of the new coronavirus vaccine (all P values < .05). The results are shown in Tables 2 and 3 .
Table 2.
Intentions of survey respondents to receive the new coronavirus vaccine
| Variables | Yes |
No |
χ2-value | P value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Age (years) | 18 ~ 30 | 111 | 20.9 | 19 | 21.3 | 2.928 | .231 |
| 31 ~ 50 | 359 | 67.5 | 65 | 73.0 | |||
| ≥51 | 62 | 11.7 | 5 | 5.6 | |||
| Residence | Countryside | 9 | 1.7 | 5 | 5.6 | 5.334 | .021 |
| Towns | 523 | 98.3 | 84 | 94.4 | |||
| Sex | Male | 156 | 29.3 | 21 | 23.6 | 1.227 | .268 |
| Female | 376 | 70.7 | 68 | 76.4 | |||
| Ethnicity | Han Chinese | 456 | 85.7 | 78 | 87.6 | 0.235 | .628 |
| Other | 76 | 14.3 | 11 | 12.4 | |||
| Education Level | Senior High School and below | 9 | 1.7 | 2 | 2.2 | 0.243 | .886 |
| Bachelor’s degree or college | 352 | 66.2 | 57 | 64.0 | |||
| Postgraduate and above | 171 | 32.1 | 30 | 33.7 | |||
| Marital status | Unmarried | 81 | 15.2 | 17 | 19.1 | 0.989 | .610 |
| Married | 436 | 82.0 | 69 | 77.5 | |||
| Divorced or widowed | 15 | 2.8 | 3 | 3.4 | |||
| Annual household income (yuan) | 100,000 and below | 347 | 65.2 | 68 | 76.4 | 5.282 | .071 |
| 110,000-350,000 | 174 | 32.7 | 21 | 23.6 | |||
| >350,000 | 11 | 2.1 | 0 | 0.0 | |||
| Smoking status | Yes | 62 | 11.7 | 9 | 10.1 | 0.179 | .672 |
| No | 470 | 88.3 | 80 | 89.9 | |||
| Drinking status | Yes | 80 | 15.0 | 14 | 15.7 | 0.028 | .866 |
| No | 452 | 85.0 | 75 | 84.3 | |||
| Q1 | Yes | 487 | 91.5 | 74 | 83.1 | 6.157 | .013 |
| No | 45 | 8.5 | 15 | 16.9 | |||
| Q2 | Negative | 487 | 91.5 | 74 | 83.1 | 6.157 | .013 |
| Not tested | 45 | 8.5 | 15 | 16.9 | |||
| Q3 | Yes | 418 | 78.6 | 63 | 70.8 | 2.646 | .104 |
| No | 114 | 21.4 | 26 | 29.2 | |||
| Q4 | Yes | 490 | 92.1 | 75 | 84.3 | 5.706 | .017 |
| No | 42 | 7.9 | 14 | 15.7 | |||
Table 3.
Analysis of vaccine-related perceptions among survey respondents and their willingness to receive the new coronavirus vaccine [n (%)]
| Variables | Disagree | Uncertainty | Agree | χ2-value | P value | |
|---|---|---|---|---|---|---|
| Awareness of unvaccinated/infected COVID-19: | ||||||
| Q5 | Yes | 77 (14.5) | 165 (31.0) | 290 (54.5) | 14.962 | .001 |
| No | 21 (23.6) | 39 (43.8) | 29 (32.6) | |||
| Q6 | Yes | 94 (17.7) | 153 (28.8) | 285 (53.6) | 9.476 | .009 |
| No | 22 (24.7) | 35 (39.3) | 32 (36.0) | |||
| Q7 | Yes | 37 (7.0) | 95 (17.9) | 400 (75.2) | 29.134 | .000 |
| No | 13 (14.6) | 34 (38.2) | 42 (47.2) | |||
| Q8 | Yes | 32 (6.0) | 81 (15.2) | 419 (78.8) | 34.908 | .000 |
| No | 8 (9.0) | 36 (40.4) | 45 (50.6) | |||
| Q9 | Yes | 217 (40.8) | 239 (44.9) | 76 (14.3) | 1.128 | .569 |
| No | 31 (34.8) | 44 (49.4) | 14 (15.7) | |||
| Q10 | Yes | 134 (25.2) | 206 (38.7) | 192 (36.1) | 2.922 | .232 |
| No | 19 (21.3) | 43 (48.3) | 27 (30.3) | |||
| Q11 | Yes | 56 (10.5) | 94 (17.7) | 382 (71.8) | 10.172 | .006 |
| No | 14 (15.7) | 26 (29.2) | 49 (55.1) | |||
| Q12 | Yes | 92 (17.3) | 135 (25.4) | 305 (57.3) | 8.797 | .012 |
| No | 22 (24.7) | 31 (34.8) | 36 (40.4) | |||
| In the perception of vaccination with the new coronavirus vaccine: | ||||||
| Q13 | Yes | 28 (5.3) | 85 (16.0) | 419 (78.8) | 35.236 | .000 |
| No | 9 (10.1) | 36 (40.4) | 44 (49.4) | |||
| Q14 | Yes | 31 (5.8) | 85 (16.0) | 416 (78.2) | 26.955 | .000 |
| No | 14 (15.7) | 28 (31.5) | 47 (52.8) | |||
| Q15 | Yes | 383 (72.0) | 87 (16.4) | 62 (11.7) | 35.405 | .000 |
| No | 39 (43.8) | 38 (42.7) | 12 (13.5) | |||
| Q16 | Yes | 405 (76.1) | 67 (12.6) | 60 (11.3) | 20.318 | .000 |
| No | 50 (56.2) | 27 (30.3) | 12 (13.5) | |||
| Q17 | Yes | 57 (10.7) | 78 (14.7) | 397 (74.6) | 39.888 | .000 |
| No | 12 (13.5) | 37 (41.6) | 40 (44.9) | |||
| Q18 | Yes | 288 (54.1) | 150 (28.2) | 94 (17.7) | 23.867 | .000 |
| No | 25 (28.1) | 46 (51.7) | 18 (20.2) | |||
| Q19 | Yes | 140 (26.3) | 176 (33.1) | 216 (40.6) | 8.004 | .018 |
| No | 14 (15.7) | 42 (47.2) | 33 (37.1) | |||
| Q20 | Yes | 295 (55.5) | 162 (30.5) | 75 (14.1) | 33.519 | .000 |
| No | 20 (22.5) | 45 (50.6) | 24 (27.0) | |||
| Q21 | Yes | 26 (4.9) | 79 (14.8) | 427 (80.3) | 21.500 | .000 |
| No | 5 (5.6) | 31 (34.8) | 53 (59.6) | |||
| Q22 | Yes | 21 (3.9) | 96 (18.0) | 415 (78.0) | 38.317 | .000 |
| No | 4 (4.5) | 42 (47.2) | 43 (48.3) | |||
| Q23 | Yes | 16 (3.0) | 114 (21.4) | 402 (75.6) | 54.058 | .000 |
| No | 8 (9.0) | 48 (53.9) | 33 (37.1) | |||
| Q24 | Yes | 53 (10.0) | 124 (23.3) | 355 (66.7) | 18.033 | .000 |
| No | 10 (11.2) | 39 (43.8) | 40 (44.9) | |||
| Q25 | Yes | 16 (3.0) | 64 (12.0) | 452 (85.0) | 70.433 | .000 |
| No | 5 (5.6) | 42 (47.2) | 42 (47.2) | |||
| Q26 | Yes | 11 (2.1) | 61 (11.5) | 460 (86.5) | 61.197 | .000 |
| No | 6 (6.7) | 37 (41.6) | 46 (51.7) | |||
| Q27 | Yes | 9 (1.7) | 86 (16.2) | 437 (82.1) | 80.506 | .000 |
| No | 6 (6.7) | 49 (55.1) | 34 (38.2) | |||
| Q28 | Yes | 10 (1.9) | 80 (15.0) | 442 (83.1) | 74.496 | .000 |
| No | 6 (6.7) | 46 (51.7) | 37 (41.6) | |||
| Q29 | Yes | 10 (1.9) | 71 (13.3) | 451 (84.8) | 43.182 | .000 |
| No | 4 (4.5) | 36 (40.4) | 49 (55.1) | |||
3.3.2. Binary logistic regression analysis
With the willingness to receive the new coronavirus vaccine as the dependent variable and the factors influencing the willingness to receive the new coronavirus vaccine as the independent variables (Table 4 for the assignment table).The variables that were significant in the univariate analysis were included in the binary logistic regression analysis, and included the following survey questions: “Do you think it is better to receive as few vaccines as possible at the same time?”; “If I get the new coronavirus vaccine, I may have serious side effects.”; “The new coronavirus vaccine is safe.”; “Specifically, for the new coronavirus vaccine, do you think it is safe?”; and “Specifically, for the new coronavirus vaccine, do you think it is easy to administer?.” They had an important influence on the vaccination of medical staff with the new coronavirus vaccine in Northern China (OR = 1.610,95% CI: 1.055 ~ 2.456; OR = 1.715, 95% CI: 1.164 ~ 2.526; OR = 0.401,95% CI: 0.212 ~ 0.760; OR = 0.352, 95% CI: 0.147 ~ 0.843; OR = 3.688, 95% CI: 1.281 ~ 10.502; All P values < .05). The results are shown in Table 5.
Table 4.
Assignment table for each variable
| Variable | Assignment |
|---|---|
| Age (years) | 1 = 18–30; 2 = 31–50; 3 = ≥51 |
| Residence | 1 = Countryside; 2 = Towns |
| Sex | 1 = Male; 2 = Female |
| Ethnicity | 1 = Han Chinese; 2 = Other |
| Education Level | 1 = Senior High School and below 2 = Bachelor’s degree or college 3 = Postgraduate and above |
| Marriage status | 1 = Unmarried; 2 = Married 3 = Divorced or widowed |
| Annual household income (yuan) | 1 = 100,000 and below; 2 = 110,000-350,000; 3 = >350,000 |
| Smoking status | 1 = Yes; 2 = No |
| Drinking status | 1 = Yes; 2 = No |
| Q1 | 1 = Yes; 2 = No |
| Q2 | 1 = Positive; 2 = Negative; 3 = Not tested |
| Q3-Q4 | 1 = Yes; 2 = No |
| Q5-Q29 | 1 = Disagree; 2 = Uncertainty; 3 = Agree |
| Q30 | 1 = Yes; 2 = No |
Table 5.
Binary logistic regression models of the factors influencing willingness to receive the new coronavirus vaccine
| Variables | β | Sx | Waldχ2 | P value | OR (95% CI) |
|---|---|---|---|---|---|
| Residence | −1.044 | 0.701 | 2.215 | .137 | 0.352 (0.089 ~ 1.392) |
| Q1 | 0.025 | 0.405 | 0.004 | .950 | 1.026 (0.464 ~ 2.268) |
| Q4 | 0.369 | 0.418 | 0.778 | .378 | 1.446 (0.637 ~ 3.281) |
| Awareness of unvaccinated/infected COVID-19: | |||||
| Q5 | −0.117 | 0.237 | 0.245 | .621 | 0.889 (0.559 ~ 1.415) |
| Q6 | −0.122 | 0.224 | 0.298 | .585 | 0.885 (0.571 ~ 1.372) |
| Q7 | −0.357 | 0.324 | 1.215 | .270 | 0.700 (0.371 ~ 1.320) |
| Q8 | 0.348 | 0.370 | 0.883 | .347 | 1.416 (0.685 ~ 2.925) |
| Q11 | 0.298 | 0.282 | 1.116 | .291 | 1.347 (0.775 ~ 2.343) |
| Q12 | −0.289 | 0.235 | 1.513 | .219 | 0.749 (0.472 ~ 1.187) |
| The perceptions of vaccination with the new coronavirus vaccine: | |||||
| Q13 | −0.010 | 0.331 | 0.001 | .976 | 0.990 (0.518 ~ 1.893) |
| Q14 | −0.572 | 0.300 | 3.636 | .057 | 0.564 (0.313 ~ 1.016) |
| Q15 | 0.331 | 0.245 | 1.821 | .177 | 1.392 (0.861 ~ 2.249) |
| Q16 | 0.028 | 0.244 | 0.013 | .910 | 1.028 (0.638 ~ 1.657) |
| Q17 | −0.137 | 0.239 | 0.330 | .566 | 0.872 (0.546 ~ 1.393) |
| Q18 | 0.294 | 0.200 | 2.160 | .142 | 1.342 (0.907 ~ 1.986) |
| Q19 | 0.476 | 0.216 | 4.878 | .027 | 1.610 (1.055 ~ 2.456) |
| Q20 | 0.539 | 0.198 | 7.455 | .006 | 1.715 (1.164 ~ 2.526) |
| Q21 | 0.520 | 0.406 | 1.642 | .200 | 1.682 (0.759 ~ 3.727) |
| Q22 | 0.031 | 0.392 | 0.006 | .939 | 1.032 (0.479 ~ 2.223) |
| Q23 | −0.914 | 0.326 | 7.850 | .005 | 0.401 (0.212 ~ 0.760) |
| Q24 | 0.271 | 0.275 | 0.966 | .326 | 1.311 (0.764 ~ 2.249) |
| Q25 | −0.545 | 0.408 | 1.780 | .182 | 0.580 (0.260 ~ 1.291) |
| Q26 | −0.427 | 0.513 | 0.691 | .406 | 0.653 (0.239 ~ 1.784) |
| Q27 | −1.044 | 0.446 | 5.493 | .019 | 0.352 (0.147 ~ 0.843) |
| Q28 | −0.452 | 0.487 | 0.861 | .353 | 0.636 (0.245 ~ 1.653) |
| Q29 | 1.300 | 0.537 | 5.867 | .015 | 3.688 (1.281 ~ 10.502) |
4. Discussion
This survey showed that 85.7% of the medical personnel in northern China were willing to receive the new coronavirus vaccine after its launch, which is higher than a survey that investigated willingness to receive the new coronavirus vaccine among the general population in China in May 2020, in which 83.5% were willing to receive the new coronavirus vaccine,6 which was significantly higher than the following findings. In December 2020, Solís Arce et al. found that an average of 64.6% of individuals were willing to receive the new coronavirus vaccine and only an average of 30.4% were willing to receive the new coronavirus vaccine among the general population in Russia.7 A survey by Harapan et al. in April 2020 found that 78.3% of individuals in Indonesia were willing for willing to receive the new coronavirus vaccine;8 a survey by Detoc et al. in April 2020 found that approximately 77.6% of the general population in France definitely or probably agreed to receive the new coronavirus vaccine;9 and an analysis conducted by Dror et al. in April 2020 of the willingness of the general Australian population to receive the new coronavirus vaccine showed that 85.8% were willing to receive the new coronavirus vaccine, similar to the results of this study.10 The results suggest that the willingness of medical personnel to be vaccinated is higher in northern China, partly because of the in-depth knowledge of medical personnel about the clinical manifestations of the new coronavirus pneumonia and the data on the development of the new coronavirus vaccine, and partly because of the better results that have been achieved in the prevention of the new coronavirus and the promotion of the use of the new coronavirus vaccine. One of the most important factors influencing vaccination against the new coronavirus is government action. The government and health community should strengthen the positive publicity of the new coronavirus vaccine and correct the negative reports it in a timely manner, and in addition to the traditional media, the government should also make use of the internet to vigorously publicize the positive effects of the new coronavirus vaccine and the relevant data on vaccination through various media channels such as Sina, Google and short video apps to increase the willingness of medical staff to receive the vaccine and to further guide the public’s willingness to receive it. A study of the 2021 U.S. Health Care Workers New Coronavirus Vaccination Survey showed that 57.5% were interested in receiving the new coronavirus vaccine, with 80.4% of this group being physicians and medical scientists, as health care workers are often a reliable source of vaccine information and their vaccination may have a positive impact on the population.11
This survey also found that the important influencing factors for medical professionals in North China to receive the new coronavirus vaccine were as follows: “Do you think it is better to receive as few vaccines as possible at the same time?”; “If I get the new coronavirus vaccine, I may have serious side effects.”; “The new coronavirus vaccine is safe.”; “Specifically, for the new coronavirus vaccine, do you think it is safe?”; and “Specifically, for the new coronavirus vaccine, do you think the it is easy to administer?.” From this, we can see that the safety of the vaccine and the ease of administration are the main reasons for the willingness of medical staff to receive the vaccine. The safety of the new coronavirus vaccine was the main reason for the high willingness of medical staff to receive the vaccine, and doubts about the safety of the vaccine were consistent with the findings of Sheikh and Karpiński’s study. The main concern about the safety of the vaccine is the unexplained illnesses that occur after vaccination,12 and Karpiński found that Grimballi syndrome and allergic reactions were common side effects of the vaccine, with Grimballi syndrome being the most serious side effect.13 The workload of medical staff has increased significantly during the new coronavirus epidemic, and their work is stressful. A retrospective survey analysis showed that the prevalence of anxiety among doctors and nurses was 26.1%;14 therefore, the convenience and rapidity of vaccination became another major reason for the high willingness of medical staff to be vaccinated. Currently, the new coronavirus epidemic is still a global pandemic, and although the epidemic has been effectively controlled in China, the immunity acquired by the population due to new coronavirus infection is low, and it is important to build a joint immunity barrier against the new coronavirus through vaccination against it.15 Therefore, the national promotion of new coronavirus vaccination occupies a key position in the prevention and control of the current epidemic. In recent years, there have been numerous questions about the safety and efficacy of vaccines, which have affected public confidence in vaccines for disease prevention.16,17 Therefore, the establishment of sound vaccine regulatory laws and standardized vaccination practices are key to the effective promotion of the new coronavirus vaccine.
This survey has certain limitations. Due to this is a cross-sectional study, bias is inevitable.The study adopted convenience sampling instead of random sampling, which may affect the representativeness of the study sample. The network questionnaire survey was a self-report method, which leads to information bias. With the continuous development of global COVID-19 and the deepening of new coronavirus vaccine research, we need to constantly investigate and study the willingness of medical staff to be vaccinated at different times.
In conclusion, the new coronavirus vaccine will be a key public health strategy to reduce the burden of disease caused by COVID-19. Our study provides insights into the acceptability of a new coronavirus vaccine, and the results suggest that health workers in northern China are overwhelmingly willing to be vaccinated. As the vaccine development process continues, the safety and ease of administration of the vaccine will also be greatly enhanced.
Supplementary Material
Acknowledgments
We thank all the individuals who generously shared their time and materials for this study. We thank the clinicians who contributed to the data collection and preparation.
Appendix. Question numbers
| Number | Question |
|---|---|
| Q1 | Have you been tested for novel coronavirus nucleic acids? |
| Q2 | What were the results of your nucleic acid test? |
| Q3 | Do you consider COVID-19 to be a major health problem affecting the population? |
| Q4 | If you have contracted COVID-19, do you think it was a significant risk to your health? |
| Q5 | If I have not received the new coronavirus vaccine, the possibility of contracting new coronavirus pneumonia is high. |
| Q6 | If I am not vaccinated against the new coronavirus, I will always be at risk of contracting COVID-19. |
| Q7 | If I get the new coronavirus vaccine, my risk of developing the new coronavirus pneumonia is reduced. |
| Q8 | The new coronavirus pneumonia epidemic can be reduced if all people are vaccinated against the new coronavirus. |
| Q9 | If I get the new coronavirus, I will die. |
| Q10 | If I get the new coronavirus, I could die. |
| Q11 | If I get the novel coronavirus, I may pass it on to family and friends who may get the new coronavirus. |
| Q12 | If I get the novel coronavirus, I am at greater risk of death. |
| Q13 | I believe that vaccination against COVID-19 can prevent the spread of COVID-19 to family members and relatives. |
| Q14 | I believe that vaccination against the new coronavirus can prevent economic and labor losses due to the new coronavirus pneumonia. |
| Q15 | I think the new coronavirus vaccine will cause me to develop COVID-19 instead. |
| Q16 | I think the outbreak is under control in China, so there is no need for the new coronavirus vaccine. |
| Q17 | Do you think that the new coronavirus vaccine will prevent new coronavirus pneumonia (which is a very serious disease)? |
| Q18 | Do you think it is better to get immunity from COVID-19 than from the new coronavirus vaccine? |
| Q19 | Do you think the fewer vaccinations you receive at the same time, the better? |
| Q20 | I may have serious side effects if I get the new coronavirus vaccine. |
| Q21 | The new coronavirus vaccine is necessary to protect our health. |
| Q22 | The new coronavirus vaccine provides good protection against the novel coronavirus pneumonia. |
| Q23 | The new coronavirus vaccine is safe. |
| Q24 | If I am not vaccinated against COVID-19, I may develop COVID-19 and cause others to contract the disease. |
| Q25 | Specifically, for the new coronavirus vaccine, do you think it is necessary? |
| Q26 | Specifically, in relation to the new coronavirus vaccine, do you think it is important? |
| Q27 | Specifically, for the new coronavirus vaccine, do you consider it to be safe? |
| Q28 | Specifically, for the new coronavirus vaccine, do you think it is effective? |
| Q29 | Specifically, for the new coronavirus vaccine, do you think it is easy to get it? |
| Q30 | Would you be willing to receive or make an appointment to receive the new coronavirus vaccine if it becomes available? |
Funding Statement
This study was supported by the Asian Regional Special Cooperation Fund of the National Health Commission of the People’s Republic of China.
Supplemental data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2031775.
Disclosure statement
No potential conflict of interest was reported by the author(s).
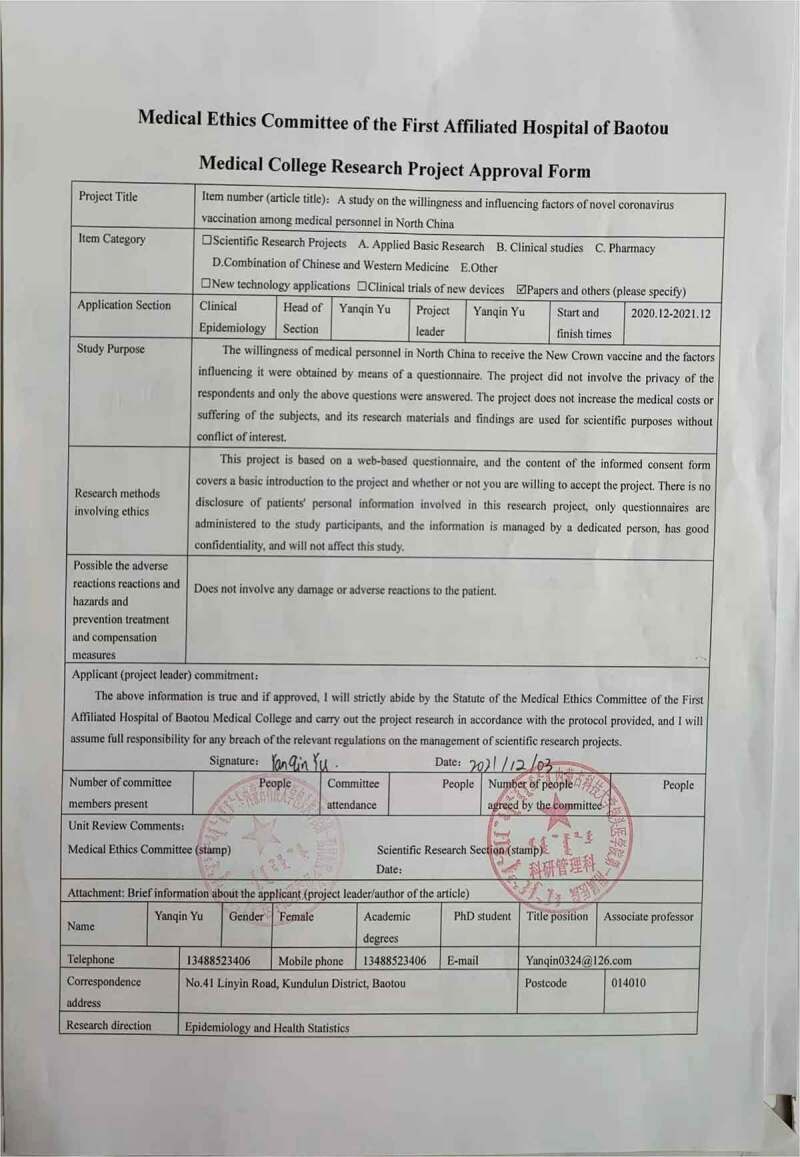
Ethics statement
The Ethical Review Committee of the Chinese Center for Disease Control and Prevention reviewed the proposed use of human subjects in the abovementioned project (Number 202020). This study was also approved by the Medical Ethics Committee of the First Affiliated Hospital of Baotou Medical College (Approval number: 20210010). Subjects participated voluntarily.
References
- 1.Alshammary AF, Al-Sulaiman AM.. The journey of SARS-CoV-2 in human hosts: a review of immune responses, immunosuppression, and their consequences. Virulence. 2021. Dec;12(1):1771–7. doi: 10.1080/21505594.2021.1929800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li H, Burm SW, Hong SH, Ghayda RA, Kronbichler A, Smith L, Koyanagi A, Jacob L, Lee KH, Shin JI, et al. Review of coronavirus disease 2019: epidemiology, transmission, risk factors, and international responses. Yonsei Med J. 2021. Jan;62(1):1–11. doi: 10.3349/ymj.2021.62.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laine C, Cotton D, Moyer DV.. COVID-19 vaccine: promoting vaccine acceptance. Ann Intern Med. 2021. Feb;174(2):252–53. Epub 2020 Dec 21. PMID: 33347321; PMCID: PMC7901662. doi: 10.7326/M20-8008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qian S, Wan R, Ping Z, Qi Z. Research progress of novel coronavirus vaccine[J/OL]. PLA Med J. 2021-Jul-19;{3},{4}{5}:1–12. http://kns.cnki.net/kcms/detail/11.1056.R.20210616.1003.002.html. [Google Scholar]
- 5.Li W, Yu J, Hong D, Ren C, Chen G. A study on people’s perception of new coronary pneumonia based on health belief theory. China Rural Health Manage. 2021;41:372–76. [Google Scholar]
- 6.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP, Understanding COVID-19. vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020. Dec 17;14(12):e0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solís Arce JS, Warren SS, Meriggi NF, Scacco A. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. Jul 16 2021. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Setiawan AM, Rajamoorthy Y, Sofyan H, Vo TQ, et al. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Hum Vaccin Immunother. 2020. Dec 1;16(12):3074–80. doi: 10.1080/21645515.2020.1819741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020. Oct 21;38(45):7002–06. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020. Aug;35(8):775–79. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaw J, Stewart T, Anderson KB, Hanley S, Thomas SJ, Salmon DA, Morley C. Assessment of U.S. health care personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system. Clin Infect Dis. 2021. Jan 25;ciab054. doi: 10.1093/cid/ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheikh AB, Pal S, Javed N, Shekhar RCOVID-19. Vaccination in developing nations: challenges and opportunities for innovation. Infect Dis Rep. 2021. May 14;13(2):429–36. doi: 10.3390/idr13020041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karpiński TM, Ożarowski M, Seremak-Mrozikiewicz A, Wolski H, The WD. 2020 race towards SARS-CoV-2 specific vaccines. Theranostics. 2021. Jan 1;11(4):1690–702. doi: 10.7150/thno.53691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raoofi S, Pashazadeh Kan F, Rafiei S, Khani S, Hosseinifard H, Tajik F, Masoumi M, Raoofi N, Ahmadi S, Aghalou S, et al. Anxiety during the COVID-19 pandemic in hospital staff: systematic review plus meta-analysis. BMJ Support Palliat Care. 2021. Jul 26;bmjspcare-2021-003125. doi: 10.1136/bmjspcare-2021-003125. [DOI] [PubMed] [Google Scholar]
- 15.Leng A, Maitland E, Wang S, Nicholas S, Liu R, Wang J. Individual preferences for COVID-19 vaccination in China. Vaccine. 2021. Jan 8;39(2):247–54. doi: 10.1016/j.vaccine.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mejri N, Berrazega Y, Ouertani E, Rachdi H, Bohli M, Kochbati L, Boussen H. Understanding COVID-19 vaccine hesitancy and resistance: another challenge in cancer patients. Support Care Cancer. 2022;30(1):289–93. doi: 10.1007/s00520-021-06419-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Qahtani WS, Alsafhi FA. A commentary on realities of developing COVID-19 vaccines discussed through the global health safety perspective. Vaccines (Basel). 2021. Mar 18;9(3):274. doi: 10.3390/vaccines9030274. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


