Abstract
A 41-year-old woman presented for evaluation of a pruritic eruption with an abrupt onset, starting on her flanks and then spreading to her arms and legs. She had 2 weeks of fever, chills, malaise, migratory joint pain, nausea, and mental confusion. An antistreptolysin O titer was positive. Upon hospital admission, bilateral lower-extremity chorea movements were observed, and her C-reactive protein level was elevated (3.7 mg/dL). Biopsy results supported erythema marginatum. Based on these clinical and laboratory findings, the diagnosis of acute rheumatic fever was established.
Keywords: Acute rheumatic fever, erythema marginatum, figurate erythema
Erythema marginatum is a highly specific cutaneous finding of acute rheumatic fever (ARF), occurring early in the disease course and resolving quickly. Timely admission and high-quality care are essential for prevention of severe long-term sequelae of ARF.
CASE DESCRIPTION
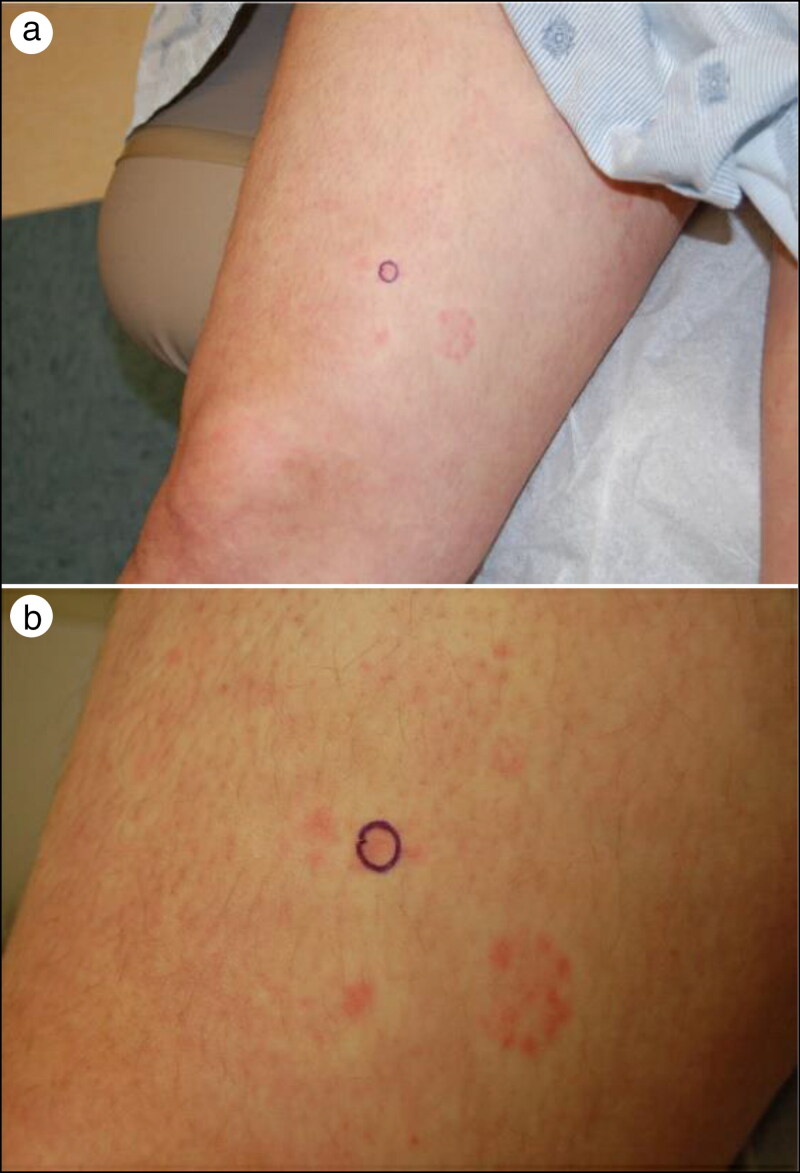
A 41-year-old woman presented for evaluation of a pruritic eruption with an abrupt onset, starting on her flanks and then spreading to her arms and legs. She had 2 weeks of fever, chills, malaise, joint pain, nausea, and mental confusion. Despite being evaluated in the emergency department, she had only been tested for illicit drug use, which was negative. Edematous papules and annular plaques with surrounding blanching were noted on the thighs, bilateral flanks, and forearms characteristic of erythema marginatum (Figure 1). A punch biopsy was positive for antistreptolysin O (ASO) titer at 200 IU/mL. Her past medical history included anxiety, gastritis, seasonal allergies, and vaginitis. Drug allergies included cephalexin, penicillin, aspirin, doxycycline, naproxen, and prednisone.
Figure 1.
(a) Subtle, pink cyclic papules on the upper right thigh. (b) Enhanced visualization of the blanching around the cyclic lesions.
Upon hospital admission, bilateral lower-extremity chorea movements were observed, and her C-reactive protein (CRP) level was elevated (3.7 mg/dL). No abnormalities were seen on transthoracic echocardiogram or electrocardiogram. Skin biopsy results supported erythema marginatum. Given our patient’s elevated ASO titer, erythema marginatum, migratory polyarthralgia, chorea, fever, and elevated CRP, the diagnosis of ARF was established. She began intravenous ceftriaxone for 10 days, followed with daily azithromycin for the next 5 years. The patient was discharged with resolution of her symptoms.
DISCUSSION
ARF is an inflammatory sequelae arising 2 to 3 weeks after group A beta-hemolytic streptococcal (GAS) pharyngitis.1 ARF manifests as a type II hypersensitivity reaction between streptococcal and host antigens.2 Diagnosis requires a combination of two major or one major and two minor Jones criteria.2 Major criteria include polyarthritis/polyarthralgia, carditis, chorea, subcutaneous nodules, and erythema marginatum.2 Minor criteria include fever, mono-arthralgia, elevated erythrocyte sedimentation rate (>30 mm in the first hour), elevated acute-phase reactants (CRP > 3.0 mg/dL), and prolonged PR interval.2 Evidence of prior GAS infection is also needed. Antistreptococcal antibodies are highly sensitive for this compared to throat culture, which is positive in only 25% of patients over 10 days after diagnosis.2,3
Diagnosis is challenging, as symptoms are nonspecific. ARF is rarely seen in developed countries due to improved hygiene, antibiotics, and reduced crowding.4 ARF typically presents in children between the ages of 5 and 14.1 Initial attacks are rare above the age of 40 and may not follow Jones criteria.1,2 An overlooked diagnosis poses a deadly risk of irreversible valvular damage from recurrent rheumatic fever.5 Our patient presented with erythema marginatum, an evanescent, polycyclic, pink eruption with serpiginous borders.4 It typically blanches with pressure and presents on the trunk and proximal extremities. Appearance may be heat induced.4 Erythema marginatum occurs early in the course and resolves quickly. It is the least common major criteria (<6%) but highly specific for ARF.4 In a review of adult ARF cases, similar presentations of positive ASO titers, erythema marginatum, polyarthritis, fever, and elevated inflammatory markers are observed.1,2,5,6 Of note is the absence of cardiac abnormalities, in line with our patient’s findings. First-line therapy to eradicate GAS and prevent recurrent attacks is long-term penicillin.5 For patients allergic to penicillin, a macrolide should be used. A history of a specific cephalosporin allergy does not preclude the use of other cephalosporins.
In conclusion, ARF in adults is rare in developed countries. Few reported cases render it difficult to understand variations in the clinical picture of ARF.
References
- 1.Gewitz MH, Baltimore RS, Tani LY, et al. Revision of the Jones criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography. Circulation. 2015;131(20):1806–1818. doi: 10.1161/CIR.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 2.Kasitanon N, Sukitawut W, Louthrenoo W.. Acute rheumatic fever in adults: case report together with an analysis of 25 patients with acute rheumatic fever. Rheumatol Int. 2009;29(9):1041–1045. doi: 10.1007/s00296-008-0796-0. [DOI] [PubMed] [Google Scholar]
- 3.Bordes SJ, Murray IVJ, Sylvester JA.. Atypical presentation of acute rheumatic fever (ARF) in a 25-year-old woman in the Caribbean: a challenging diagnosis. BMJ Case Rep. 2020;13(2):e231888. doi: 10.1136/bcr-2019-231888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shibata A, Yoshikawa T, Makita S, et al. A case of late middle age-onset recurrent rheumatic fever. Clin Exp Dermatol. 2020;45(5):595–596. doi: 10.1111/ced.14163. [DOI] [PubMed] [Google Scholar]
- 5.Saito M, Hatakeyama S.. Acute rheumatic fever with erythema marginatum. N Engl J Med. 2016;375(25):2480–2480. doi: 10.1056/nejmicm1601782. [DOI] [PubMed] [Google Scholar]
- 6.Steer AC, Smeesters PR, Curtis N. Streptococcal serology: secrets for the specialist. Pediatr Infect Dis J. 2015;34(11):1250–1252. doi: 10.1097/inf.0000000000000881. [DOI] [PubMed] [Google Scholar]