Abstract
Acute renal infarction is a rare condition that can progress to renovascular hypertension, chronic kidney disease, and end-stage kidney disease, depending on the severity. We present a case of a 30-year-old man with no significant past medical history who presented with sudden onset right flank pain. Initially pyelonephritis was suspected but it was later found to be acute renal infarction secondary to cardioemboli from atrial fibrillation.
Keywords: Atrial fibrillation, cardioembolism, renal infarction
Renal infarction is a rare condition that can progress to renovascular hypertension, chronic kidney disease, and end-stage kidney disease, depending on the severity. Two major causes of renal infarction are thromboemboli, commonly from the heart or aorta, and in situ thrombosis, commonly due to hypercoagulability or renal artery injury.1 Atrial fibrillation (AF) is usually associated with underlying heart disease, such as atrial enlargement. Common predisposing conditions for AF include hypertension, coronary artery disease, valvular heart disease, and heart failure. Complications of AF include thromboembolism and heart failure. We present a 30-year-old man with acute renal infarction secondary to cardioembolic etiology.
CASE DESCRIPTION
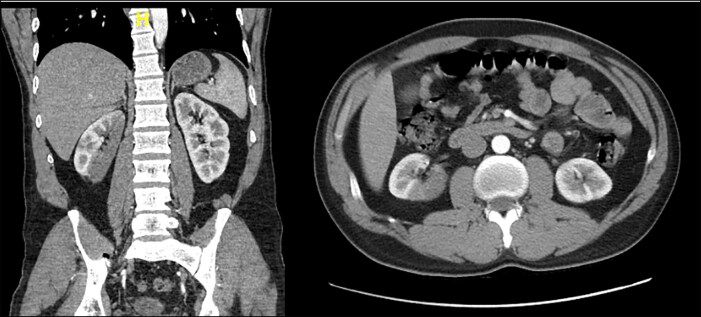
A 30-year-old man with no significant past medical history presented to the emergency department with sudden onset of right flank pain radiating to the groin with associated nausea and vomiting. The patient admitted to alcohol consumption and cocaine use. Initial vital signs were unremarkable. Urinalysis disclosed a creatinine of 1.2 mg/dL. Computed tomography (CT) of the abdomen was initially read as right pyelonephritis or nephronia (Figure 1). Telemetry showed AF with a ventricular rate of 63 beats/minute, which was later confirmed with an electrocardiogram. A transthoracic echocardiogram showed an ejection fraction of 30%, a dilated left atrium, and a mitral valve with a rheumatic appearance and increased velocities across the valve, a calcified annulus, and mild to moderate regurgitation. A transesophageal echocardiogram revealed an ejection fraction of 25% to 29%, a dilated left ventricle and left atrium, no thrombus in the atrial cavities, no evidence of vegetation, and mild stenosis of the mitral valve with a pressure of 1.7 cm2 and mean gradient of 5 mm Hg. The patient was successfully converted to sinus rhythm. His CHA2DS2-VASc score was zero, but given the current embolic event, the patient received therapeutic enoxaparin during his hospital stay. He did not want to be on warfarin; therefore, he was switched to oral apixaban for anticoagulation. He was discharged on apixaban, metoprolol succinate, lisinopril, aspirin, folic acid, and thiamin. The patient was requested to follow-up with cardiology for his AF and counseled to quit his substance abuse.
Figure 1.
Renal infarction as seen on CT of the abdomen and pelvis, coronal and axial views.
DISCUSSION
Renal infarction is a rare condition with a prevalence of only about 0.007% among patients visiting the emergency department.2 Due to its nonspecific symptoms, it is commonly misdiagnosed as renal colic, pyelonephritis, renal cancer, or infective endocarditis.3
Common etiologies of renal infarction include cardioembolic disease, renal artery injury, and hypercoagulability. Cardioembolic etiologies include AF, cardiomyopathy, and endocarditis. Commonly, patients with renal infarction present with acute onset flank or abdominal pain which may be associated with nausea, vomiting, and fever. In addition to hematuria and proteinuria, elevations in blood pressure due to increased renin release may also be seen.1
Due to the rarity of renal infarction, many clinicians may not have experience diagnosing and treating it. Renal infarction should be approached by considering its major causes: AF, hypercoagulability, and renal artery injury. To evaluate these, it is necessary to obtain a detailed history and physical exam and studies including an electrocardiogram, echocardiogram, basic metabolic panel, complete blood count, coagulation studies, and a CT scan with angiography. A urinalysis, urine culture, and lactate dehydrogenase should also be obtained, as hematuria, proteinuria, and an elevated lactate dehydrogenase level are commonly associated with renal infarction.4
Treatment of renal infarction should involve treating the underlying condition. Patients without a preexisting diagnosis should be evaluated for AF or an underlying hypercoagulable state. In patients with a main renal artery infarction, interventions to restore perfusion should be considered, especially in patients with a solitary kidney or a significantly reduced glomerular filtration rate.5
References
- 1.Bourgault M, Grimbert P, Verret C, et al. Acute renal infarction: a case series. Clin J Am Soc Nephrol. 2013;8(3):392–398. doi: 10.2215/CJN.05570612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Domanovits H, Paulis M, Nikfardjam M, et al. Acute renal infarction. Clinical characteristics of 17 patients. Medicine (Baltimore). 1999;78(6):386–394. doi: 10.1097/00005792-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Korzets Z, Plotkin E, Bernheim J, Zissin R.. The clinical spectrum of acute renal infarction. Isr Med Assoc J. 2002;4(10):781–784. [PubMed] [Google Scholar]
- 4.Hazanov N, Somin M, Attali M, et al. Acute renal embolism. Forty-four cases of renal infarction in patients with atrial fibrillation. Medicine. 2004;83(5):292–299. doi: 10.1097/01.md.0000141097.08000.99. [DOI] [PubMed] [Google Scholar]
- 5.Koivuviita N, Tertti R, Heiro M, Manner I, Metsärinne K.. Thromboembolism as a cause of renal artery occlusion and acute kidney injury: the recovery of kidney function after two weeks. Case Rep Nephrol Urol. 2014;4(1):82–87. doi: 10.1159/000362538. [DOI] [PMC free article] [PubMed] [Google Scholar]