ABSTRACT
Background
The World Health Organization declared vaccine hesitancy a top threat to global health following resurgence of vaccine-preventable diseases close to eradication in many countries (e.g. measles). Vaccines are effective in preventing severe illness, hospitalization, and death from COVID-19, yet there remains a small proportion of the eligible population who choose not to vaccinate. Social media and online news sources are opportunities for targeted public health interventions to improve vaccine uptake. This study reports the results of a semi-structured interview study that explored the influence of media and information on individuals’ self-reported intentions to vaccinate against COVID-19.
Methods
A qualitative descriptive study was employed to gain insight from a diverse group of individuals. Adult participants were recruited through a related COVID-19 study; we used a maximum variation sampling technique and purposively sampled participants based on demographics. Interviews were conducted from February 2021 to May 2021. Themes from interviews were summarized with representative quotations according to the 3C Theoretical Framework (Confidence, Complacency, Convenience).
Results
Key themes identified following thematic analysis from 60 participants included: vaccine safety, choice of vaccine, fear mongering, trust in authority, belief in vaccinations (Confidence); delaying vaccination (Complacency); confusing information, access to vaccines and information (Convenience). While most participants intended to vaccinate, many expressed concerns and hesitancy.
Conclusions
COVID-19 vaccine hesitancy prevents universal immunization and contradictory messages in media are a source of concern and fear. The success of future vaccine campaigns will depend upon authorities’ ability to disseminate accessible, detailed, and consistent information promoting public confidence.
KEYWORDS: Vaccination hesitancy, media, misinformation, COVID-19, interviews
Introduction
The novel coronavirus disease 2019 (COVID-19) continues to pose severe risk to individuals and societies worldwide.1 Initially, efforts to mitigate community spread of COVID-19 were non-pharmaceutical interventions such as masking, hand washing, testing and stay-at-home orders. As of December 2020, governments began approving vaccines for use against COVID-19.2 Vaccines are one of the most effective public health measures against infectious disease,3,4 and are a powerful tool in mitigating the long-term health and economic impacts of the current pandemic.5,6 Moreover, research shows that vaccines are effective in preventing severe illness, hospitalization and death from COVID-19.7
Vaccinating all eligible individuals, while also supporting continued adherence to non-pharmaceutical interventions, is our best line of defense to prevent, detect and manage COVID-19. However, despite the widespread use of vaccines, the global phenomenon of vaccine hesitancy is challenging current vaccination efforts.8–11 The World Health Organization (WHO) Strategic Advisory Group of Experts (SAGE) on Immunization describes vaccine hesitancy as the delay or refusal of vaccination despite the availability of vaccines.12 In Canada, as of November 2021, only 75% of the total population is fully vaccinated13 and recent data indicate that approximately one quarter of parents will not vaccinate their children (<12) when a pediatric vaccine is approved for use.14 Vaccine hesitancy is not a novel phenomenon; the WHO declared it a top threat to global health in 2019 following the resurgence of vaccine-preventable diseases that had been close to elimination in many countries (e.g., measles).15
Existing research highlights the importance of monitoring and assessing vaccine concerns as they develop in real time.16 According to this research, it is important to tailor vaccine information to specific communities (e.g., addressing levels of health literacy), and to use trusted sources of information for dissemination17 to achieve optimal vaccine confidence and uptake.3 There has been a large amount of information emerging regarding socio-economic determinants of vaccine hesitancy;6,9,18,19 however, less is known about the impact of (social and broadcasted) media and information (sources) on the public’s intentions to vaccinate. Increased access to online media sources16,18,20 which regularly include mis- and dis-information about COVID-19 and associated vaccines, has been shown to be associated with decreased vaccine confidence and acceptance globally.8,21 As more people turn to social media and online news sources for information about COVID-19,17 the need to understand its influence on vaccine confidence and acceptance is rising. This may provide important opportunities for the development of targeted public health interventions that aim to improve vaccine acceptance. Thus, the goal of our research was to explore and understand the influence of media and information on individuals’ self-reported intentions to vaccinate against COVID-19.
Methods
Study design
We used a qualitative descriptive study design executed in accordance with the Consolidated Criteria for Reporting Qualitative Research (Supplemental File Table 1 Appendix 1). The University of Calgary Conjoint Health Research Ethics Board (ID: REB20–0358) and Dalhousie University Health Science Research Ethics Board (ID: REB2020–5121) approved this study and of participants providing oral consent in lieu of written consent. By using a qualitative descriptive study design,22 researchers gained insight from a diverse group of individuals about their perspectives and experiences. This methodology also facilitated the use of the 3C Theoretical Framework (Confidence, Complacency, Convenience), developed by the SAGE working group,23 for assessment of experiences which is used to shed light on factors impacting individuals decisions to be vaccinated. We conducted interviews from 11 February 2021, to 19 May 2021.
Table 1.
Interview participant characteristics (n = 60)
| Characteristic | N (%) |
|---|---|
| Region in Canadaa | |
| Alberta | 9 (15.0) |
| British Columbia | 10 (16.7) |
| Maritimesb | 11 (18.3) |
| Ontario | 12 (20) |
| Québec | 9 (15.0) |
| Saskatchewan/Manitoba | 9 (15.0) |
| Age category, years | |
| Median, IQR | 47.0 (34.5, 63.0) |
| 18-29 | 9 (14.8) |
| 30-44 | 21 (34.4) |
| 45-64 | 17 (27.9) |
| 65+ | 14 (23.0) |
| Gender | |
| Women | 27 (45.0) |
| Men | 33 (55.0) |
| Ethnicityc | |
| White | 38 (63.3) |
| Asian | 14 (23.3) |
| Black | 2 (3.3) |
| Latin American | 1 (1.7) |
| Middle Eastern | 1 (1.7) |
| Multiracial | 3 (5.0) |
| Educationa | |
| Highschool | 7 (12.1) |
| Some post-secondary | 40 (69.0) |
| Post-secondary degree | 11 (19.0) |
| Household Incomea | |
| $0-$50,000 | 15 (25.9) |
| $50,000-$99,999 | 30 (51.7) |
| $100,000 and over | 13 (22.4) |
| Employment Statusa | |
| Full-time | 31 (53.4) |
| Part-time | 4 (6.9) |
| Retired | 17 (29.3) |
| Otherd | 6 (10.3) |
| Marital Statusa | |
| Single | 21 (36.2) |
| Partnered | 27 (46.6) |
| Divorced/Widowed | 10 (17.2) |
| Has childrena | |
| Yes | 24 (41.4) |
aMissing data, n=2.
bMaritimes region includes Nova Scotia, New Brunswick, and Prince Edward.
cMissing data, n=1.
dOther includes unemployed, maternity leave, disability.
Participants
Participants were eligible if they were English or French-speaking adults (≥18 years) residing in Canada and able to provide informed consent. We recruited eligible participants through a related study17 whereby participants consented to be contacted for future COVID-19 research opportunities. We used a maximum variation sampling technique and purposively sampled participants based on broad regional, gender, age, and ethnic categories to ensure diversity across participants. All participants provided oral consent before participating in the interview.
Data collection
We iteratively developed a semi-structured interview guide that was pilot tested with four members of the public to ensure core and probing questions adequately captured our study objectives. We asked participants to reflect on three overarching topics related to their consumption of COVID-19 information: (1) information access and evaluation, (2) media coverage (3) personal and community impacts of messaging on behaviors and perceptions of the pandemic. The term media was used to refer to TV, print and online coverage, as well as social media websites and applications, defined as platforms that enable users to create and share content or socially network.24 We collected participants’ demographic information at the end of each interview. Two researchers (SM, ML) trained in qualitative methods, conducted the interviews via Zoom (https://zoom.us) and telephone, based on participant preference. Interviews lasted an average of 27 minutes. We digitally recorded the interviews and sent the English audio files to a transcription company (www.rev.com/) to produce verbatim transcripts; the French interviews were transcribed using NVivo 12 (QSR International, Melbourne, Australia) and corrected by SM prior to being translated by the AI software, Sonix (www.my.sonix.ai). SM then reviewed and corrected the translated transcripts to improve clarity when typos occurred. The researchers who conducted the interviews also reviewed, cleaned, and de-identified the textual data prior to analysis. Participants were offered the opportunity to review their interview transcripts as a form of member checking to maximize validity; however, no participants chose to do so.
Data management and analysis
We used NVivo 12 (QSR International, Melbourne, Australia) to manage the data and facilitate thematic analysis.25 Three researchers (SM, CD, EF) first reviewed and coded a small sample of the transcripts (n = 5) independently and in duplicate using open coding.25 Initial codes were compared and discussed with a senior qualitative researcher (JPL) to create a first draft of the codebook. The researchers then analyzed an additional 35 transcripts using both open and axial coding, iteratively refining the codebook until all relevant ideas were included. The complete dataset (n = 60 transcripts) was then coded in duplicate with the finalized codebook. The researchers used memos to document emerging ideas and relationships between codes during analysis. The researchers held weekly meetings during the initial period of analysis, wherein themes were developed, revised, and refined. Themes were then reported through the 3C Theoretical Framework. The researchers conducted a secondary stratified analysis of textual data, which included age, sex, region, and household income.
Results
Sample characteristics
We invited 126 individuals to participate (Figure 1). We aimed to interview 10 participants from each region and to include a diverse group of individuals, considering region, gender, age, and ethnicity. Data saturation was achieved after analysis of the first 35 interviews, prior to analysis of the full data set (n = 60), though the study team continued to collect and analyze data from all participants who were interviewed to increase diversity within the data. Sixty individuals, from nine provinces participated. 27 (45.0%) individuals self-reported as women, 40 (69.0%) had some post-secondary education, 30 (51.7%) had a household income of $50,000-$99,000, and the median age of participants was 47 years (Table 1).
Figure 1.
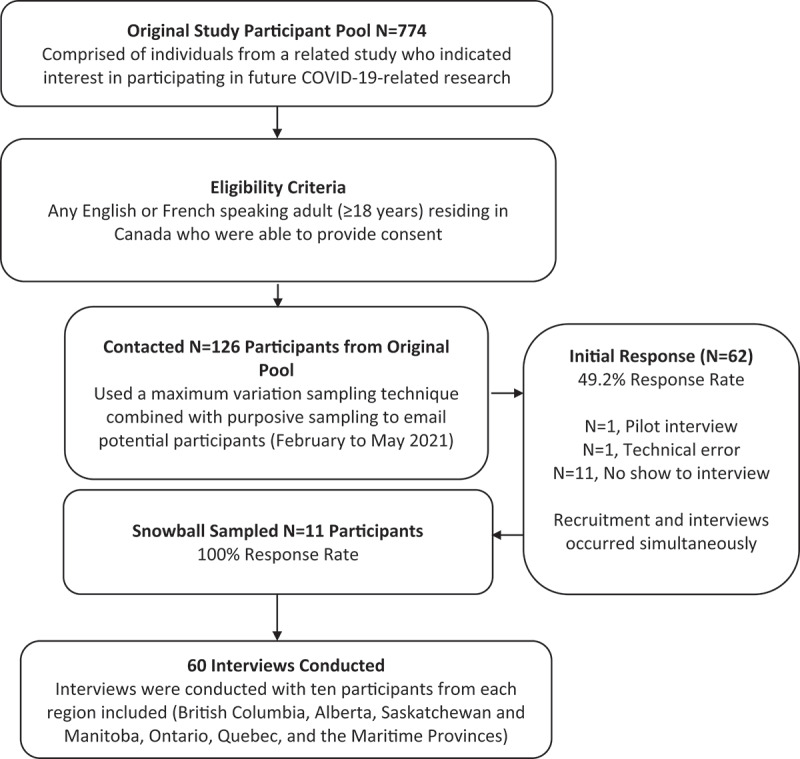
Methods of study sample inclusion.
Findings
Thematic analysis of data resulted in the development of 8 themes describing the influence of media and information on self-reported intentions to vaccinate: vaccine safety, choice of vaccine, fear mongering, trust in authority, belief in vaccinations, delaying vaccination, confusing information, and access to vaccines and information. Exemplary quotes are provided in-text; additional salient quotes are provided in Table 2. Furthermore, utilizing the 3C Theoretical Framework, we reported the themes within the categories of vaccine confidence, complacency, and convenience23 (Table 3). Salient findings of analysis by demographic characteristics are reported.
Table 2.
Quotations of participants matched to themes
| Vaccine safety | “Well, my understanding is the vaccine may not necessarily prevent you from getting COVID. It might lessen the symptoms, and we still don’t know how long it’s good for. There’s a lot of questions there, and it just seems that’s brushed aside. That concerns me, because I don’t feel like my questions are answered.” Par 58, female, 47, Prince Edward Island “I do have some concerns about how quickly the vaccines were rolled out and whether there’s going to be long-term side effects down the line, because they were tested over a period of … What did I hear? 10 months instead of 10 years. I know the government says they’re safe and stuff, but the logic part of my brain says, “How do you know it’s safe if you haven’t done a long-term five- or 10-year study on these things?” Right.” Par 36, male, 34, British Colombia |
| Choice of vaccine | “So I’m not really 100% sure right now, but I’m still waiting to see before I get back to when my time comes, and I have to either decide. Or hopefully if I miss it, they’ll still have some at the end for those who didn’t get, so they’ll have enough to still get vaccinated. But right now you have no choice. Whatever comes out now or whatever’s left over, first come first serve. So you can’t just pick what you want. It’s like ordering food.” Par 26, male, 53, British Colombia “That’s one question I’ve had, that’s why I’ve got a hesitancy. I can tell you right off the bat, I’m not into the AstraZeneca thing. I’m not. I will be vaccinated in about eight days and it’s either Moderna or Pfizer.” Par 46, male, 65, Quebec “Well, just because of one vaccine, the AstraZeneca there that I will not take because of the side effects,” Par 56, female, 61, Quebec |
| Fear mongering | “I just don’t like the idea of feeling like I have to get that in order to … I’m sure things are exaggerated. I’ve heard to leave the country, to leave your province, to go to work. How far does this go sort of thing? That’s what concerns me. Like I say, there’s probably a lot of misinformation and a lot of scare tactics out there, because it gets more attention, but it is a concern, because you don’t know.” Par 58, female, 47, Prince Edward Island “So the wastage rate was less than 1%, which that doesn’t make an article. You wasted a thousand doses. And if you don’t, if you wait until the second to last paragraph in your story to say that a thousand doses represents less than 1% of the doses administered, nobody reads that far down. They read the first couple of paragraphs of the story. They see the headline and they form their opinion. So that’s why I didn’t rely on the media for my opinion on vaccination, and most people that got vaccinated didn’t. “Par 41, female, 63, Manitoba “I don’t know if it’s false, but occasionally a couple articles early of like, “Oh, this person had an allergic reaction and blah, blah, blah.” And the clickbaiting fear of vaccines. I’ve seen that, I obviously didn’t go down that rabbit hole, but I’ve seen it there, so I know it’s out there.” – Par 13, female, 38, Alberta |
| Trust in authority | “But, yeah. I don’t know. I think it’s a bit of cognitive dissonance there. I don’t know if I want to know that much about the vaccine. Everybody’s getting it. I’m sure this is probably just my cognitive dissonance talking, but I’m sure the government’s done what they need to do to make sure it’s safe.” Par 14, female, 31, Alberta “I’m of the opinion that if government has signed off on these things that are safe, which might put me in the minority in this day and age, but anyways, so basically if it’s directly from government, I think it’s legit.” Par 36, male, 34, British Colombia |
| Belief in vaccinations | “It hasn’t impacted my decision at all. I was just like, yeah as soon as the vaccine’s here, I’m ready. Give me as many doses as it takes.” Par 12, female, 35, Ontario “Oh, well, I’m a vaccine believer. So, I’m just like, I would have the flu vaccine every year. There’s no way I would not have this vaccine. So we were really anxious as to when we would get it. And we were watching and watching to see when we would be allowed to do so.” Par 45, female, 81, Ontario “I would’ve got the vaccine anyway, because number one, I believe in it. When I was a kid, getting the smallpox, chicken pox, all those shots, I’ve had them all. So I believe in that. I’ve got my shingles vaccine as well. I’ve been a science person, so I would’ve gotten it anyway.” Par 19, male, 65, Saskatchewan |
| Delaying vaccination | “That I’m still not sure, because it’s kind of … Where the information we get, which vaccines are we’re going to get? We don’t know. Is there a possibility that we could pay and get the vaccine we want? That I would like but that’s impossible. And the vaccines, one dose or two doses … Who are they to make the decision that, that one is better that than that one. That one, I’m really not sure. I’m going to get vaccinated. But I’ll probably be one of the last. I want to see if people get any disadvantages of the vaccine before getting vaccinated. I won’t be the first one.” Par 21, female, 54, Quebec “Just to see how the reaction is on the general public. I think that’s more my theory and I know they’ve done the testing and stuff like that and they’ve come out relatively good, which is why they’re doing it on the general population now. But like I said, I’d rather wait it out. No rush. You don’t need it anyways.” Par 42, male, 42, Manitoba “I’m very mixed on taking it. I don’t think I’d be the first to jump in when my age comes along.” Par 20, male, 66, Saskatchewan |
| Confusing information | “And I understand that they were operating with older information but I think that maybe there should have been a little editorial discretion on their part when they came out with that because I think that was very confusing to people. Because on one hand they’re saying 65 and over shouldn’t have that particular one but then if you look at the real world information from Europe and Great Britain, it’s been fine. So that causes some consternation … ” Par 22, male, 68, Manitoba “Because with these vaccines, I don’t think any of us understand. We don’t understand one has two shots, but they’re holding back the second shot and they’re telling them not to hold back. We don’t understand … You know, there’s a lot of confusion with vaccines.” Par 32, female, 81, New Brunswick “I don’t know what’s true or what’s not true about all this stuff but there’s so much and so many reports and it’s like when I was talking to my sister the other day, I said, “Yeah, you don’t know what to believe or what not to believe and what’s exaggerated and what’s over the top, what’s true, what’s not true”.” Par 51, male, 65, Alberta |
| Access to vaccines and information | “But at the same time, I feel like I know nothing about the vaccination rollout, I have no idea really when I myself will have access to it.” Par 3, male, 22, Nova Scotia “So I don’t really make that decision for them [parents] whether or not they should be vaccinated, but I kind of keep a lookout and make sure that you know when it’s their turn, that they do go get vaccinated.” Par 14, female, 31, Alberta |
Table 3.
Research themes mapped to the 3C Theoretical Framework
| 3C Model of Vaccine Hesitancy | Themes |
|---|---|
| Confidence | Vaccine safety |
| Trust in government | |
| Belief in vaccinations | |
| Fear mongering | |
| Choice of vaccine | |
| Complacency | Delaying vaccination |
| Convenience | Confusing information |
| Access to vaccines and information |
Confidence
Vaccine confidence relates to individuals’ trust in the safety of vaccines, the system and authorities that deliver them, and the motivations of those in charge.23 Five themes reflected participant’s confidence and self-reported intentions to vaccinate, in relation to media and information: vaccine safety, choice of vaccine, fear mongering, trust in authority, and belief in vaccinations.
Vaccine safety
While most participants expressed intention to be vaccinated, some voiced concern regarding vaccine safety. Participants frequently discussed their lack of confidence in information regarding the safety of COVID-19 vaccines, including the expedited development and release of the vaccine, as well as the unknown long-term side effects. For many, this information originated from sources such as broadcast news, social media and online articles. One participant from British Columbia described feeling like a “guinea pig” while discussing the lack of long-term studies. Moreover, participants generally pointed to the lack of information on vaccine side effects and the impact it had on their intentions to vaccinate:
They haven’t told us what this vaccine does. What the effects are. If we do have an adverse reaction to it, what could that be? I don’t feel like they’re giving us enough information about it. So at this point, I don’t want to get the vaccine because I don’t know what these effects are and what this can do to me. – 28-year-old female from Ontario.
While many participants expressed concern over the safety of an expedited vaccine, some distanced themselves from the ensuing ‘anti-vaxxer’ movement.
I trust my government to be like, “Hey, this is what you should be doing.” And I will do that. I’ll say that as far as maybe them telling people to get vaccinated when it comes out. And that’s the one thing I don’t know if I agree with doing right away … but not because I’m an anti-vaxxer, but because when it comes to new vaccinations that have been very expedited, quickly sent to markets, it seems kind of scary. I don’t really know what the long-term effects are going to be. − 30-year-old man from Ontario.
When stratified by region, participants from Maritime provinces were less likely to discuss safety concerns than those from other provinces. Additionally, participants with an average household income above $100K voiced concerns about vaccine safety less frequently than other participants.
Choice of vaccine
The importance of media and information on choice in vaccine was found associated with individuals’ intent to vaccinate. Some participants indicated that media and information obtained regarding side effects or complications (e.g., blood clots) associated with a particular type of COVID-19 vaccine, influenced their confidence in vaccines, and intentions to prioritize a specific choice in vaccine. These sentiments were largely noted by respondents from Quebec.
The news cover says we could have blood clot complications from the adjustment Johnson or Johnson, or AstraZeneca vaccine. So I’m categorically not going to get those vaccines … − 46-year-old male from Quebec.
In general, participants discussed the need to take time to choose which vaccine was right for them.
At the onset, I already knew that without a doubt, I was going to get the vaccine. My concern was, will there be enough vaccine for everyone? But now I’m actually taking my time because I’m trying to choose which vaccine. − 52-year-old female from Alberta.
Oneparticipant echoed this sentiment, also voicing some concern about vaccine shortages:
So I’m not really 100% sure right now, but I’m still waiting to see before I get back to when my time comes, and I have to either decide. Or hopefully if I miss it, they’ll still have some at the end for those who didn’t get, so they’ll have enough to still get vaccinated. But right now you have no choice. Whatever comes out now or whatever’s left over, first come first serve. So you can’t just pick what you want. It’s like ordering food. – 53-year-old male from British Columbia.
Fear mongering
Participants described fear mongering as media and information that was sensationalizing vaccine information to create headlines. Rather than impact their personal intentions to vaccinate, participants were worried of the impact of fear mongering for other individuals’ confidence and their intentions to vaccinate. As one participant described:
(These stories) could have been cut and dry, but it’s more profitable to drag, to show the stories of people getting vaccinated and having reactions or dying … because that’s what drives the money and that’s what makes people more unsure … – 23-year-old man from Nova Scotia.
Gender-based differences also presented in this theme, with female participants expressing a deeper level of concern about the impact of fear mongering on vaccine uptake than men. Some participants felt that responsible reporting would involve addressing people’s concerns in a way that answered questions without fueling further mistrust and fear.
I understand that an opposing view can sometimes be the correct view. Right? But you have to check it out … to make sure that the view is indeed correct before giving it any credence. I mean, the business where they give an incorrect take as often as they give the correct take, is just wholly frustrating. I can’t tolerate it. I’ll actually tune out that news source. If the opinion is held by only 1% of the people, well, maybe give it 1% exposure in the media, please, not 50%. − 38-year-old female from Alberta.
Trust in authority
In contrast to previous themes that explored elements that undermined participants’ vaccine confidence, trust in authorities’ information (i.e., government, public health organizations) helped to build participant’s confidence in their intentions to vaccinate. Participants held a firm belief that government officials had done their due diligence in checking the efficacy of the vaccines and that they would not approve of something unsafe for the general population:
The Canadian government says it [COVID-19 vaccine] is safe. So because of that, I’m ready for it. - 60-year-old female from British Columbia.
This trust in information helped to balance some common concerns (i.e., the speed of the vaccine rollout). When discussing the availability of certain vaccines to the Canadian public, one participant explained:
That [quick availability] is because it’s [COVID-19 vaccine] reliable and it’s correct. I have some concerns, but if the government thinks [it’s reliable] that is what is good now. – 38-year-old female from Quebec.
Belief in vaccinations
The firm belief in the efficacy of vaccinations was a common sentiment among participants. Their positive experiences with vaccines, and their belief that vaccines were important for disease prevention, shaped their support. Rather than be influenced by media and information, many participants noted that media would not change their confidence in vaccination:
As soon as it’s available, I will get it. There is no news that would change my mind on that. – 38-year-old female from Alberta.
Complacency
Vaccine complacency relates to beliefs in risk of infection or impact of disease, and importance of vaccination for health and prevention.23 Complacency typically occurs when people perceive that the risk of the virus, and health-related impact of disease, is low. In these situations, vaccines can be seen as unnecessary. One theme aligned with individuals’ complacency in relation to media and information and intentions to vaccinate: delaying vaccination.
Delaying vaccination
Some participants indicated that even with the information obtained regarding vaccines, they would delay vaccination due to worry of vaccine safety. There were some who also believed that the risk of being diagnosed with COVID-19 was low, so the vaccine wasn’t necessary when it came to keeping themselves safe. These findings were largely expressed by middle-aged (30–64), non-Maritime participants. When asked about his decision to delay being vaccinated, one participant explained:
Just to see how the reaction is on the general public. I think that’s more my theory and I know they’ve done the testing and stuff like that and they’ve come out relatively good, which is why they’re doing it on the general population now. But like I said, I’d rather wait it out. No rush. You don’t need it anyways. – 42-year-old male from Manitoba.
Furthermore, participants noted that delaying vaccination when it was available to them would depend on what information they had at that time:
Of course, we are reading and therefore based upon that, when our time comes, maybe we would get vaccinated, depending upon how safe it is, and if there are many adverse reactions, then we might consider delaying it. – 37-year-old man from Ontario.
Convenience
Vaccine convenience relates to the influence of factors that impact individuals’ decision to vaccinate, including, availability, accessibility, affordability, willingness to pay, ability to understand (e.g., health literacy), and a belief and satisfaction in services.23 Two themes aligned with media and information and convenience of vaccines: confusing information, and access to vaccines and information.
Confusing information
Media and information portrayal regarding vaccinations resulted in confusion for participants and placed constraints on general understanding of vaccine safety. High amounts of contradictory information regarding the safety of the vaccines was associated with self-reported intentions to vaccinate:
Information about the vaccine is everywhere. I’ve seen so much stuff in the news … Things you see online too, and you don’t know how, if they’re exaggerated. Who knows anymore. It’s just so all over the place … When I start hearing things about blood clots, and a vaccine being allowed, and then it’s not allowed, that’s when things get a little sketchy to me. – 68-year-old female from PEI.
Moreover, another participant noted:
There’s a lot of alerts and videos about, Hey, don’t get the vaccine because they’re going to … [infiltrate your] DNA and stuff. And also with the blood clots people are getting, so I’ll say that’s kind of alerting, but at the same time the government says is totally safe. Then social media says another thing. And now government says like, Oh, actually Astra is not that safe. We’re going to take it out. – 29-year-old female from British Columbia.
Access to vaccines and information
Participants expressed challenges in accessing information regarding when, where, and how to receive the vaccine. They also noted that information on this topic was generally confusing. Access to information impacted convenience for individuals trying to get the vaccine for themselves, or for others.
I’m very disappointed in the way our government has rolled out this vaccination plan and changed it so often. In terms of accessibility … We have lots of seniors and older adults in our province who don’t have access to the online stuff where they’re staying. You got to register online. Well, it ain’t going to happen in small towns where the internet is not very good. − 65-year-old man from Saskatchewan.
This was especially poignant in middle-aged (30–64) and older adults as some described challenges faced trying to help older friends and family navigate the vaccine rollout. For many, this meant taking on the role of advocate to ensure a convenient and comfortable process for their older loved ones. One participant described the issue as a lack of information during the vaccine role out.
When they started rolling out the vaccine here … they had a very limited information campaign for who was eligible and when. I phoned my mother, when I found out she would be eligible and I said, ‘Look, you need to phone this week, so you can go next week’. − 68-year-old male from Manitoba.
Moreover, some participants expressed that they had given up trying to be proactive about the vaccine rollout as they were unable to find information about availability. As one participant stated:
I have tried to find out are they expediting second doses for any reason, but that doesn’t seem to be something you can find out. – 81-year-old woman from Ontario.
Discussion
The influence of media and information on individuals’ self-reported intentions to vaccinate against COVID-19 were examined through the lens of the 3C Theoretical Framework: confidence, complacency, and convenience.23 Our study suggests media and information influenced Canadians’ confidence in the COVID-19 vaccine and their intentions to vaccinate. A lack of confidence in the COVID-19 vaccine was associated with media portrayal of vaccine safety, types of vaccine, and tendency to sensationalize information through fear mongering. Complacency of individuals was associated with certain media and information, in which individuals noted the choice of delaying vaccinations based on limited information available on the vaccine. This dearth of information may have contributed to a relative sense of in-urgency amongst a number of participants, commenting their desires to wait to see the efficacy of the vaccine when deployed to the general population. Our findings also suggest a negative association of media and information with participants’ beliefs of convenience regarding vaccination. Many participants found their access to information and physical vaccines were limited, and that information coming from the media and government, was contradictory and confusing.
Successful pandemic preparedness and response relies on effective communication of public health policies and recommendations.26–28 Our findings highlight the importance of accessible and acceptable messaging, particularly within the media, that promote vaccination given reports that Canadian news-based television, print, or websites have been the most accessed sources for pandemic information.17 Previous research has also shown the association of misinformation and decreased likelihood of vaccination.21,29,30 Researchers have highlighted a critical need to ensure equity in public health communication to optimize public response.31 While there is a gap currently in the evidence base related to the COVID-19 pandemic, studies on early pandemics (i.e., influenza type A virus [H1N1]) observed communication inequities that reflected existing social inequalities, thus highlighting the association between individual circumstance and behavioral compliance in regards to public health recommendations.32 We found that older participants tended to have challenges accessing information about vaccine logistics and safety as much of it was online. Previous research has shown a positive association between older age and intentions to vaccinate;10,33–35 therefore, our findings highlight how quickly vaccine rates could increase simply by ensuring information is accessible to a population already predisposed to being vaccinated. Additionally, our work validates earlier Canadian findings that differences in self-reported intentions to vaccinate are associated with geographic regional locations.36
Our findings, in conjunction with existing research, highlight the importance of tailoring media and information to target audiences.4,8,35,37,38 Schmid et al.37 conducted a systematic review of barriers to influenza vaccination intention and behavior, and found differences between vaccine hesitancy for seasonal versus pandemic influenza, highlighting the importance of targeted vaccine public health campaigns. Researchers have discussed the importance of understanding vaccine hesitancy toward the COVID-19 vaccines specifically, due to the novel and nuanced factors involved like speed of development and roll-out.6,8 For example, complacency toward influenza vaccination has been associated with low perceived risk and worry of disease37 which aligns with some our participants beliefs. Comparingly, our research describes the novelty of COVID-19 and the resultant lack of long-term studies on the vaccine’s side effects, as well as the influx of constantly changing information in association with individuals’ complacency and choice to delay vaccination. For example, at the time of our study, fluctuating media coverage of the side effects of specific COVID-19 vaccines (i.e., risk of blood clots) was noted by participants as confusing and worrisome and influenced their intentions to vaccinate. Our findings suggest national vaccine campaigns should provide specific information on COVID-19 vaccine safety to increase confidence and decrease complacency in Canadians’ intentions to vaccinate. This will require broad dissemination of reliable, tailorable, accessible media and information to all population subsets.
Limitations
There are limitations to be considered when interpreting our findings. We were unable to recruit participants from Newfoundland and the Territories as they were not surveyed in the previous study, which limits the translation of findings to these locations. Although we are unable to generalize statistically our findings to the entire population, our representative survey and subsequent maximum variation sampling technique well position the results of our study to be readily applicable and transferable more broadly. While we purposively sampled a diverse group of participants, including broad regional, sex, age, and ethnic categories, the qualitative nature of our study limited statistical generalization to the broader population. However, the reported experiences provide great depth and understanding. Selection bias is a possibility for this work as we recruited eligible participants through a related study whereby participants consented to be contacted for future COVID-19 research opportunities. It is likely that those who agreed to be contacted (and subsequently interviewed) were engaged and interested in COVID-19-related research, potentially more accepting of vaccines in general. As well, our sample was largely comprised of individuals who reported a white ethnicity. Future research should seek to sample from the general population, including a representative and diverse sample, so that perspectives from non-Western cultures are included in the evidence base. Finally, as the Canadian vaccine roll-out is a rapidly changing landscape, information and access to vaccines were changing daily, which may have influenced participants responses. To combat this challenge, we adapted our interview questions to remain broad to allow for a breadth of experiences of participants from the initial interviews (February) to the later interviews (May).
Conclusion
Vaccines are a vital tool in the fight to protect communities from the continued detrimental impacts of the COVID-19 pandemic. Despite the remarkable increase in vaccine uptake within Canada, there remains a small but significant amount of vaccine hesitancy which continues to prevent universal immunization. The impact and importance of media and information on vaccine hesitancy cannot be overlooked, as participants often pointed to confusing and contradictory messages in the media a source of concern and fear regarding COVID-19 vaccines. Moreover, as vaccine approval for children is forthcoming, there is an opportunity to utilize lessons learned to optimize vaccine confidence in parents. Utilizing the 3C Theoretical Framework, our data makes visible the association of vaccine confidence and self-reported intentions to vaccinate. The success of future vaccine campaigns will depend upon authorities’ ability to disseminate accessible, detailed, and consistent information promoting confidence in the public as we learn how to navigate global pandemics in an increasingly connected world.
Supplementary Material
Funding Statement
Dr. Parsons Leigh has received a Grant from the Canadian Institutes of Health Research [grant number RN420046-439965] to fund this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data cannot be shared publicly because of patient confidentiality. Data may be available upon reasonable request from the University of Calgary and Dalhousie University research ethics board for researchers who meet the criteria for access to confidential data.
Supplemental data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2048623.
References
- 1.World Health Organization . WHO Director-General’s opening remarks at the media briefing on COVID-19. Geneva (Switzerland): World Health Organization; 2020. Mar 11 [accessed 2022 Feb 1]. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. [Google Scholar]
- 2.Government of Canada . Approved COVID-19 vaccines. Ottawa (Canada): Government of Canada; 2021. [accessed 2022 Feb 1]. https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines.html. [Google Scholar]
- 3.Dube E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J.. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9:1763–9. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E.. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–79. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chou WS, Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35:1718–22. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 6.Guidry JPD, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49:137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Government of Canada . COVID-19: effectiveness and benefits of vaccination. Ottawa (Canada): Government of Canada; 2021. [accessed 2022 Feb 1]. https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19/vaccines/effectiveness-benefits-vaccination.html. [Google Scholar]
- 8.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2020;27(2):225–28. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl Trop Dis. 2020;14:e0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ogilvie GS, Gordon S, Smith LW, Albert A, Racey CS, Booth A, et al. Intention to receive a COVID-19 vaccine: results from a population-based survey in Canada. BMC Public Health. 2021;21:1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dubé E, Gagnon D, Nickels E, Jeram S, Schuster M. Mapping vaccine hesitancy–country-specific characteristics of a global phenomenon. Vaccine. 2014;32:6649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacDonald NE. Hesitancy SWGoV . Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–64. [DOI] [PubMed] [Google Scholar]
- 13.Government of Canada . COVID-19 vaccination in Canada. Ottawa (Canada): Government of Canada; 2021. [accessed 2022 Feb 1]. https://health-infobase.canada.ca/covid-19/vaccination-coverage/. [Google Scholar]
- 14.Angus Reid Institute . Kids and COVID: half of Canadian parents with children aged 5-11 ready to vaccine their little ones ASAP. Ontario (Canada): Angus Reid Institute; 2021. [accessed 2022 Feb 1]. https://angusreid.org/covid-kids-vaccine/. [Google Scholar]
- 15.World Health Organization . Ten threats to global health in 2019. Geneva (Switzerland): World Health Organization; 2019. [accessed 2022 Feb 1]. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. [Google Scholar]
- 16.Larson HJ, Smith DM, Paterson P, Cumming M, Eckersberger E, Freifeld CC, et al. Measuring vaccine confidence: analysis of data obtained by a media surveillance system used to analyse public concerns about vaccines. Lancet Infect Dis. 2013;13:606–13. [DOI] [PubMed] [Google Scholar]
- 17.Parsons Leigh J, Fiest K, Brundin-Mather R, Plotnikoff K, Soo A, Sypes EE, et al. A national cross-sectional survey of public perceptions of the COVID-19 pandemic: Self-reported beliefs, knowledge, and behaviors. Plos One. 2020;15:e0241259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health. 2020;5:e004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173:964–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16:2586–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roozenbeek J, Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. 2020;7:201199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim H, Sefcik JS, Bradway C. Characteristics of qualitative descriptive studies: a systematic review. Res Nurs Health. 2017;40:23–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization . Report of the SAGE working group on vaccine hesitancy. Geneva (Switzerland): World Health Organization; 2014. [accessed 2022 Feb 1]. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf:63. [Google Scholar]
- 24.Chen J, Wang Y. Social media use for health purposes: systematic review. J Med Internet Res. 2021;23(5):e17917. doi: 10.2196/17917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual. 2017;16:1–13. doi: 10.1177/1609406917733847. [DOI] [Google Scholar]
- 26.Henrich N, Holmes B. Communicating during a pandemic: information the public wants about the disease and new vaccines and drugs. Health Promot Pract. 2011;12:610–19. [DOI] [PubMed] [Google Scholar]
- 27.Mheidly N, Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Public Health Policy. 2020;41:410–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sandell T, Sebar B, Harris N. Framing risk: communication messages in the Australian and Swedish print media surrounding the 2009 H1N1 pandemic. Scand J Public Health. 2013;41:860–65. [DOI] [PubMed] [Google Scholar]
- 29.Montagni I, Ouazzani-Touhami K, Mebarki A, Texier N, Schück S, Tzourio C, et al. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health. 2021;43(4):695–702. doi: 10.1093/pubmed/fdab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021;5:337–48. [DOI] [PubMed] [Google Scholar]
- 31.Viswanath K, Lee EWJ, Pinnamaneni R. We need the lens of equity in COVID-19 communication. Health Commun. 2020;35:1743–46. [DOI] [PubMed] [Google Scholar]
- 32.Lin L, Savoia E, Agboola F, Viswanath K. What have we learned about communication inequalities during the H1N1 pandemic: a systematic review of the literature. BMC Public Health. 2014;14:484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39:1080–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sherman SM, Smith LE, Sim J, Amlot R, Cutts M, Dasch H, et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVaccs), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021;17:1612–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.AlShurman BA, Khan AF, Mac C, Majeed M, Butt ZA. What demographic, social, and contextual factors influence the intention to use COVID-19 vaccines: a scoping review. Int J Environ Res Public Health. 2021;18(17):9342. doi: 10.3390/ijerph18179342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tang X, Gelband H, Nagelkerke N, Bogoch II, Brown P, Morawski E, et al. COVID-19 vaccination intention during early vaccine rollout in Canada: a nationwide online survey. Lancet Reg Health Am. 2021;2:100055. doi: 10.1016/j.lana.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005 - 2016. Plos One. 2017;12:e0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boucher J-C, Cornelson K, Benham JL, Fullerton MM, Tang T, Constantinescu C, et al. Analyzing social media to explore the attitudes and behaviors following the announcement of successful COVID-19 vaccine trials: infodemiology study. JMIR Infodemiology. 2021;1:e28800. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data cannot be shared publicly because of patient confidentiality. Data may be available upon reasonable request from the University of Calgary and Dalhousie University research ethics board for researchers who meet the criteria for access to confidential data.


