ABSTRACT
Purpose
Vaccination of adolescent girls against human papillomavirus (HPV) significantly reduces the incidence of cervical cancer. HPV vaccines are available in Pakistan but plans to develop HPV vaccination program are at a nascent stage. We conducted a formative study to explore adolescent girls’ knowledge and perspectives on HPV and cervical cancer and collect their recommendations for implementing an HPV vaccination program in their community.
Methods
Using qualitative exploratory study design, we conducted four focus group discussions (FGDs) with 12 adolescent girls per group in District West, Karachi. We recruited unmarried girls aged 16–19 years from schools and community settings between May—December 2020. Data analysis was done using NVivo.
Results
Overall, participants displayed a positive attitude toward HPV vaccine. However, they were unfamiliar with basic concepts related to female reproductive health. Female relatives were indicated as girls’ preferred point of contact for discussions on HPV and cervical cancer, but fathers were portrayed as decision-making authority on vaccination. Participants indicated vaccine hesitancy among parents may affect HPV vaccination uptake. Girls suggested individual household visits and community-based camps as strategies for successful implementation of HPV vaccination program. A solid foundation of trust between girls’ families, program managers, and other stakeholders emerged as a key asset for the program’s success.
Conclusion
Adolescent girls’ suggestions of informing key decision-makers in the family (particularly fathers) of the benefits of HPV vaccination, establishing trust with vaccine providers, and increasing accessibility of vaccinations should be explored for successful implementation of an HPV vaccination program in Pakistan.
KEYWORDS: Human papilloma virus, HPV, cervical cancer, adolescents, vaccine hesitancy, vaccination programs
Introduction
Cervical cancer is the fourth most common cancer in women worldwide, with >570,000 reported cases and >310,000 deaths per year.1 Virtually all cervical cancer cases are caused by sexually-acquired infection through human papillomaviruses (HPV).2 The World Health Organization recommends adolescent girls aged 9–14 years to receive two doses of the HPV vaccine before initiation of sexual activity.2
In Pakistan, cervical cancer is the third most frequent cancer among women,3 and also the third leading cause of female cancer deaths.4 In 2020, there were >5,000 new cervical cancer cases, amounting to 5.5% of all female cancer cases in Pakistan, and >3,100 cervical cancer deaths.3 Most (88%) cervical cancer cases in the country were attributed to infections with HPV types 16 and 18, which are both vaccine-preventable.4,5 HPV vaccination is available in Pakistan, but is not included in the national immunization schedule.
The design and evaluation of HPV vaccination programs in countries worldwide has rarely incorporated adolescent girls’ perspectives.6-8 However, integrating adolescents’ recommendations when developing a health intervention that is directly relevant to them may help to design a well-targeted program, implemented more effectively in the local context. We conducted this formative study to explore adolescent girls’ knowledge and perspectives on HPV and cervical cancer and collect their recommendations for the design and implementation of a future HPV vaccination program in Sindh province, Pakistan.
Methods
Background settings
Karachi is the capital of Sindh province, Pakistan. It is home to around 16 million people, with an average annual growth rate of 2.6% and a literacy rate of 78%.9,10 Administratively, Karachi is subdivided into six districts, which are further sectioned into a total of 178 union councils (UCs),11 the smallest geographic administrative unit.12 We recruited participants from District West, the largest district in Karachi. It comprises seven different towns subdivided into a total of 30 UCs with a mixed urban-rural infrastructure.12 The district covers a population of 3.9 million residents with mixed socioeconomic, religious, and ethnic background;9 a male:female ratio of 1.1; and infant and maternal mortality rates of 25 and 4 per 1,000 individuals, respectively.13
Study design
We used a qualitative exploratory study design and conducted focus group discussions (FGDs) with adolescent girls in District West, Karachi. At the end of the last FGD session, each girl received a small gift in compensation for her time and effort in this study. The gifts were non-monetary and consisted of a notebook and a pen. Participants were also provided refreshments (tea and snacks) during the FGDs. Necessary infection control measures related to the ongoing SARS-CoV-2 pandemic, including social distancing and mask wearing, were in place throughout recruitment and data collection.
Sample size
We aimed to interview up to 60 adolescent girls. The target sample size was based on a predicted thematic saturation after 4 FGDs, with allowance for one extra FGD if saturation was not reached.
Participants and recruitment
We recruited participants at two public secondary schools selected through convenience sampling in two different towns in District West. During inception meetings with school managements, we obtained formal permission to conduct participant recruitment on the school premises. An introductory talk was given to all grade 8–10 students to explain the background and objectives of this research. Talks were given in the presence of teachers, and students were encouraged to ask questions. After each talk, hard copies of the study consent form were distributed (to be taken home) to all girls whose eligibility was confirmed by the field team (eligible girls were unmarried and aged 16 to 19 years). In Pakistan the age of majority to consent is 18 years, therefore, parental consent was obtained from all study participants. During the following days, signed written consent forms were collected until the target sample size was reached.
In addition, we engaged a Lady Health Worker (LHW), a female health practitioner who commonly provides door-step primary care services in Pakistan, to recruit participants through household visits in a third town in District West. Households of eligible girls were selected through convenience sampling. During in-person visits, the LHW explained the study to girls’ parents or guardians and collected written consent forms from those who agreed for their daughter/granddaughter to participate.
Contact details, baseline socio-demographic characteristics, parental age, educational level, and occupation, were collected from all participants.
Focus group discussions
We conducted four FGDs with 12 participants each. Girls were informed about the date, time, and venue for their respective FGD sessions through a phone call. For girls recruited at schools, FGDs were carried out in dedicated classrooms allocated by the school management. In the community setting, FGDs were conducted in meeting rooms within government health facilities.
All FGDs were conducted in the local language (Urdu). Each FGD comprised two two-hour sessions over the course of one to two days. Before commencing the FGD, a trained interviewer answered any outstanding questions from participants. All sessions were audio-recorded, and a note-taker took detailed notes throughout each session.
The semi-structured topic guide included open-ended questions and discussion prompts on the following topics:
Adolescent girls’ knowledge and attitudes towards cervical cancer, HPV infection, and HPV vaccination, including risk perceptions and perceived safety and efficacy of the HPV vaccine.
Vaccination decision-making dynamics within girls’ families, including participants’ own ability to be part of the decision-making process for HPV vaccination.
Participants perceived informational needs regarding HPV vaccination, including girls’ preferred sources of information, and main criteria for choosing one information source over the other.
Factors participants would consider important for the successful implementation of an HPV vaccination program in their community, including age-appropriate information channels; recruitment and informed consent procedures; ideal vaccination location and administration procedures; follow-up methodology; inclusion of hard-to-reach populations.
To ensure validity and reliability of the FGD tool, we piloted the semi-structured interview guide with girls in one participating school. Since sexual and reproductive health is a sensitive topic of discussion in the local context, the piloting helped ensure that prompts were appropriate and captured the essence of the research question. Following piloting and participant and interviewer debriefing, iterative revisions were made in the interview guide by removing some duplicate questions, reordering the prompts and updating their language. Triangulation of FGD recordings and comparison and discussion of notes among investigators also helped ensure that the FGD guides were valid and reliable.
Data analysis
Descriptive analysis of participants’ demographic characteristics was performed using STATA 14.2 software.
For the qualitative analysis, FGDs were transcribed verbatim, translated into English, and analyzed by thematic analysis using NVivo 11 software. The investigators first examined the transcripts repeatedly to familiarize themselves with the data, and added notes and analytic memos to the transcripts to interpret the data and begin the initial coding process. After this, a coding frame was developed using an open coding approach by enlisting the notes/memos into categories and subcategories, (level 1 (root) and level 2 (sub) codes respectively). A definition and description were added to each of these codes to make it evident when to assign other text to this code. As additional data was analyzed, it was either collated under existing categories or additional categories were added to reflect emerging findings in the codebook. Themes were simultaneously extracted and relationships between codes were analyzed to merge them and determine the key themes in the data. Lastly, thematic charting was done to rearrange the data extracts according to appropriate thematic references in charts to interpret the findings.14,15
Two investigators independently coded all four transcripts. For the first two FGDs, the investigators discussed and compared the codes, for the third and fourth FGDs, the investigators independently added the codes in the codebook either under existing categories or created additional categories to reflect emerging findings. A third investigator was engaged to resolve any discrepancies. The investigators ensured that data saturation was reached for the analysis i.e. they continued the analysis until no new codes were emerging from the additional data and no further insights were originating from the analysis.
To maintain rigor in the analysis, we aimed for reflexivity in the team through including investigators with diverse backgrounds. Both the coders were public health experts, but had varying socio-cultural backgrounds. Close coordination and discussions between the coders helped bring diverse perspectives while interpreting the results to maintain objectivity of the research. Additionally, the coders and investigators frequently referred to the recordings of the FGDs as well as the notes of the study implementation team that commented on the rapport with participants, main topics that were discussed, and nonverbal communication, to ensure all perspectives were accounted for in the results.
Ethics approval
This study was approved by the Institutional Review Board of Interactive Research and Development (IRD_IRB_2020_04_001) and the Institutional Review Board of the National University of Singapore (S-19-030).
Results
Study population
Between September 20 and 24 December 2020, a total of 48 girls participated in the FGDs from schools and community settings. We approached a total of 317 girls across three towns of District West in Karachi out of which 96% (305/317) were approached at secondary schools, and 4% (12/317) were approached through household visits. Among girls approached at schools, 48% (146/305) were younger than 16 years, and none were married. Guardians of 30% (48/159) of eligible girls consented for their daughter/granddaughter to participate in this research. Those who refused consent were either not interested in the study or were worried participation would result in the girl missing school lessons or being vaccinated against HPV. Consenting participants from schools were divided into 3 separate FGD groups. Out of 48 girls recruited in schools, 75% (36/48) ultimately took part in FGDs. Twelve girls who initially consented to take part in the study were not present on the day of data collection. All 12 girls invited to take part in this study during household visits were eligible and took part in a fourth FGD (Figure 1).
Figure 1.
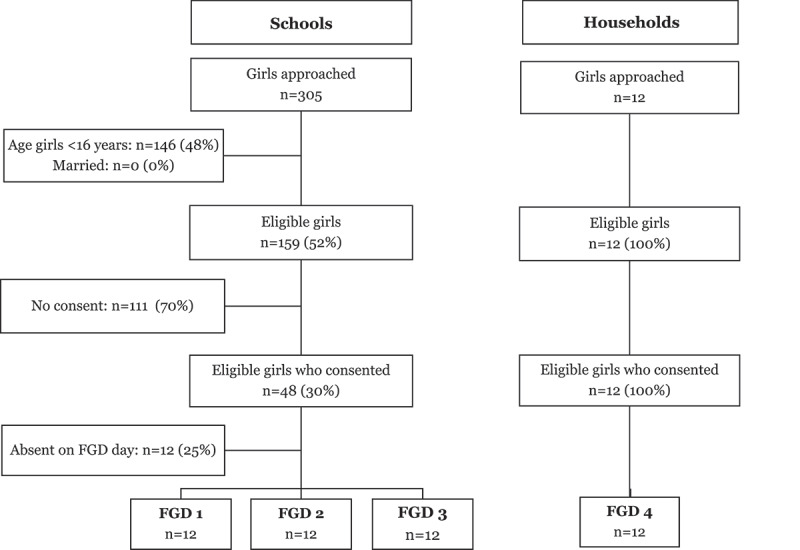
Participant recruitment chart between September and December 2020, recruitment was conducted at two secondary schools and through household visits in District West, Karachi. Unmarried girls aged 16 to 19 years were included. FGD= Focus group discussion.
Average age of study participants was 17.1 years. Participants had an average of three siblings, and 63% (30/48) of participating girls were born at home. A total of 23% (11/48) of the girls’ fathers and 40% (19/48) of the girls’ mothers were not educated. All fathers were employed, while 79% (38/48) of mothers worked as home makers (Table 1).
Table 1.
Participants’ characteristics: Baseline socio-demographic indicators among study participants (n = 48) and their guardians
| Indicator | Mean | SD | |
|---|---|---|---|
| Participant’s age (years) | 17.1 | ±.8 | |
| Father’s age (years) | 44.6 | ±11.3 | |
| Mother’s age (years) | 41.0 | ±5.0 | |
| Number of siblings | 3 | ±3 | |
| Ethnicity | n | % | |
| Muhajir | 16 | 33.3 | |
| Punjabi | 13 | 27.1 | |
| Sindhi | 12 | 25.0 | |
| Pashto | 5 | 10.4 | |
| Balochi | 2 | 4.2 | |
| Birth place | |||
| Home | 30 | 62.5 | |
| Hospital | 18 | 37.5 | |
| Father’s education | |||
| No education | 11 | 22.9 | |
| Primary (1–5 years) | 10 | 20.8 | |
| Secondary (6–10 years) | 21 | 43.8 | |
| Higher Secondary (11–12 years) | 5 | 10.4 | |
| Bachelors and above (≥13 years) | 1 | 2.1 | |
| Mother’s Education | |||
| No education | 19 | 39.6 | |
| Primary (1–5 years) | 11 | 22.9 | |
| Secondary (6–10 years) | 11 | 22.9 | |
| Higher Secondary (11–12 years) | 6 | 12.5 | |
| Bachelors and above (≥13 years) | 1 | 2.1 | |
| Father’s Occupation | |||
| Private Organization | 19 | 39.6 | |
| Daily wages | 10 | 20.8 | |
| Self-employed | 8 | 16.7 | |
| Others | 11 | 22.9 | |
| Mother’s Occupation | |||
| Home maker | 38 | 79.2 | |
| Others | 10 | 20.8 | |
SD= Standard deviation.
Knowledge
Overall, girls displayed a good understanding of virology, and 60% (29/48) were able to describe viruses as harmful agents that can “cause infection […] [focus Group; FG1, Participant; P10], spread quickly […][FG4, P8], and transmit from one person to another [FG3, P2]”. However, 96% (46/48) of the girls harbored specific misconceptions regarding the mode of transmission of HPV. Individual participants believed that the virus is transmitted through “poor hygienic conditions”[FG4, P3], by “using objects from an infected person” [FG3, P5] or “through breathing” [FG2, P9]. 71% (34/48) of the participants had no specific knowledge of the HPV vaccine, but they were able to identify vaccination as a “protective” [FG1, P5] intervention against infection. Half of the girls (50%, 24/48) expressed interest in finding out more about the benefits and effectiveness of the HPV vaccine, as well as vaccination side effects.
A majority of the girls’(92%, 44/48) knowledge of female anatomy and reproductive health was poor, and 42% (20/48) had never heard of a uterus or cervix before this study, even though age- and culture-appropriate language was used. Despite these knowledge gaps, 79% (38/48) of the participants were still able to recognize cervical cancer as a female disease: “These organs do not exist in men, this is why they can’t get [cervical] cancer” [FG4, P7].
Risk perceptions
All the girls (100%, 48/48) perceived cancer as a severe disease, which can “cause internal destruction and destroy a person completely” [FG3, P7]. But since most girls had not heard the term ‘cervical cancer’ before the study, 48% (23/48) assumed it was a rare illness. Because of the uncertainty surrounding the relationship between HPV infection and cervical cancer, 81% (39/48) of the girls were unable to correctly identify risk factors of cervical cancer: “[Cervical cancer] is a virus and since a farmer lives in unhygienic condition […], this can also happen to him”[FG1, P2]. Among 10% (5/48) of the girls, being well informed about cervical cancer was perceived as a protective factor: “[Cervical cancer] might not happen to […] a teacher, [as] she must have all the information about this, and she can take care of herself” [FG1, P4]
Information sources
Participants mentioned numerous information sources to collect information on HPV vaccination. Girls’ preferred sources were either doctors (69%, 33/48) and nurses (12%, 6/48), or individuals who are already part of their everyday life, including family (46%, 22/48), friends (15%, 7/48), teachers (27%, 13/48), and neighbors (15%, 7/48). Other frequently used information channels were instant messaging applications (15%, 7/48), internet search engines (65%, 31/48), community health workers (19%, 9/48) and social media (33%, 16/48), such as Facebook (29%, 14/48) or Instagram (4%, 2/48). Less coveted sources included traditional healers (12%, 6/48), and mass media, such as news channels (12%, 6/48), TV shows (12%, 6/48), and newspapers (12%, 6/48).
When choosing information delivery channels for the dissemination of information on the HPV vaccine to the broader community, girls considered accessibility to be a key requisite. For instance, 17% (8/48) of the girls regarded internet not be appropriate as the main source of information, because “most people don’t have access to it” [FG3, P11], and people “sometimes don’t know how to use it and won’t be able to search it” [FG3, P9]. TV may not be a good medium to spread information specifically related to HPV and cervical cancer, because “news and TV is mostly watched by male members, […] and it’s possible that they might not share the information with other family members. Hence, information could not be [conveyed] to [the] target population” [FG1, P2].
HPV vaccination program
Vaccination decision-making
Mothers (81%, 39/48), sisters (19%, 9/48), and other female relatives (21%, 10/48) were indicated as girls’ preferred point of contact for discussions related to HPV and cervical cancer. However, fathers (50%, 24/48) were generally portrayed as the definitive decision-making authority with regards to vaccination. In many of the girls’ families, “if [the] father says no, then no one can argue with him” [FG1, P10]. However, 56% (27/48) of the girls regarded mothers as efficient agents of persuasion and several girls were adamant that “if [the] mother agrees to [vaccination], then she could easily convince the father” [FG3, P2].
Elderly family members (31%, 15/48) can also play a crucial role, because “if the information is provided by younger people, [parents] are not convinced […], but if similar information is given by some elderly person in the family, they accept it”[FG1,P6]. However, 2% (1/48) of the girls postulated that elderly relatives may not acknowledge the existence of cervical cancer, if they were not aware of the disease before the HPV vaccine was offered to a girl in family.
Vaccine hesitancy and refusal
More than half of the participants (56%, 27/48) indicated vaccine hesitancy as the most likely obstacle to successful implementation of an HPV vaccination program (Figure 2). Girls anticipated that parents, and fathers in particular (33%, 16/48), may hesitate to provide consent to HPV vaccination for their daughters, and some (17%, 8/48) expected their parents would not agree to vaccination “by any means” [FG1, P4]. Fear of vaccination side effects and similar misconceptions including cosmetic issues (10%, 5/48), such as a “scar mark on [girls’] hands” [FG1, P5] were highlighted as key reasons. Girls attributed the spread of these misconceptions to the general lack of information on vaccination among parents (27%, 13/48), as well as the circulation of negative rumors about vaccines in their community (49%, 22/48): “Because they have heard negative things about vaccination from people […], they won’t agree to it [themselves]” [FG1, P1].
Figure 2.
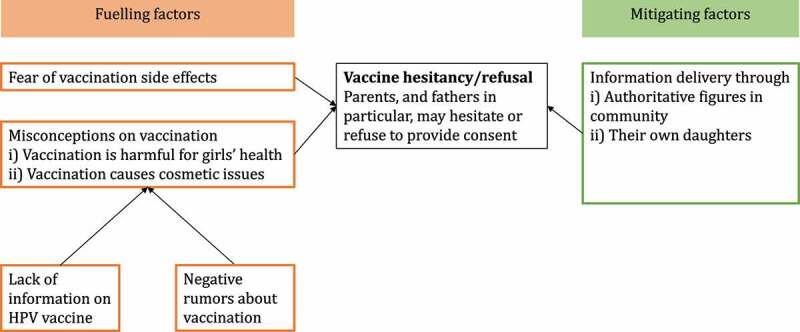
Fueling and mitigating factors for vaccine hesitancy and refusal.
HPV vaccine educational campaign
60% (29/48) of the girls suggested a multi-channel, community-based educational campaign should be implemented alongside the HPV vaccination program, to increase the likelihood of parents giving consent and potentially mitigate the impact of vaccine hesitancy on the program. 17% (8/48) of the girls’ recommended that the campaign should not be limited to the families of eligible girls, but rather target their entire community. Girls expected the campaign’s impact to be greatest if information was delivered through several different channels at the same time, including school- or community-based information camps (27%, 13/48), dedicated websites (15%, 7/48) and instant messaging groups (29%, 14/48), household visits (67%, 32/48), street banners or flyers (37%, 18/48), announcements at religious gatherings (27%, 13/48), and peer education (25%, 12/48). Half of the girls (50%, 24/48) believed community-based polio workers could also play an important role: “When they go for polio vaccination, they will spread HPV information as well” [FG3, P1].
HPV vaccination program implementation
When developing strategies for implementation of HPV vaccination program in their communities, 42% (20/48) of the girls’ recommended household visits in the community, because this would allow the inclusion of girls who do not attend school or are otherwise marginalised (Figure 3). To ensure accessibility, 60% (29/48) of the girls believed vaccination itself should then be offered at community-based camps (a stationary or mobile solution set up at a central place within the community to deliver short-term medical interventions such as immunizations to the targeted population), because “it would be difficult for all to go to [a] hospital or [a] clinic to get vaccination” [FG2, P8]. In addition, community-based vaccination would encourage vaccination uptake among those who do not trust vaccinations at healthcare facilities, such as general practitioner clinics. However, 44% (21/48) girls suggested that vaccine should be administered by a doctor in the presence of girl’s parents or other adult family members. Half of the participants (50%, 24/48) did not anticipate high dropout rates between the first and second HPV vaccine dose, unless a girl had pain or other side effects following the first injection: “If they get any side effects […], they will not go for second dose” [FG1, P9]. Therefore, 31% (15/48) participants suggested efforts should be made to mitigate vaccination side effects at the point of delivery. In addition, 29% (14/48) of the participants recommended a vaccination record with a follow-up appointment date should be issued to each girl and girls’ contact details should be collected to allow call reminders prior to the second dose.
Figure 3.
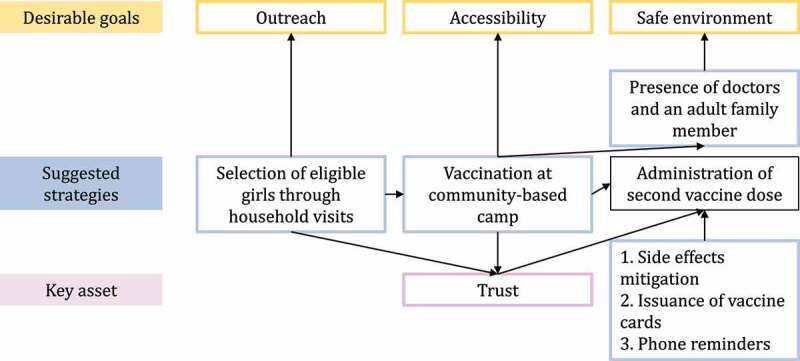
Participant suggestions for implementation of a HPV vaccination program.
Trust
The theme of trust emerged in different contexts throughout the FGDs as a key asset for the success of the HPV vaccination program (Figure 3). Girls’ conscious suggestion to identify eligible individuals through household visits was linked to the goal of building a trustful relationship with parents before inviting girls to be vaccinated: “We will visit their homes and tell them about [HPV] vaccine. We will take parents in confidence and take their permission to vaccinate their children” [FG2, P10]. According to our participants, trust would also play a key role in girls’ decision whether or not to return for the second vaccination dose: “It’s just a matter of trust. If [girls] trust, they will come [back]” [FG1, P3].
Discussion
This study was the first to analyze young adolescents’ perspectives on HPV vaccination in Pakistan, and to involve youth into formative discussions on the implementation of HPV vaccine programs in their community. Although several countries successfully rolled out HPV vaccination programs,16 program design and evaluation have rarely included adolescents’ perspectives.5–7 Our study focused on seeking girls’ perspectives on HPV vaccination only, given they will be the primary target population of an upcoming HPV Vaccination Program in the country. Study participants displayed an overall positive attitude toward HPV vaccine, but indicated vaccine hesitancy among parents as the most likely obstacle for successful implementation of an HPV vaccination program in their community. Girls gave critical input for the development of a HPV vaccination program, where eligible girls are recruited through individual household visits and vaccine is administered at community-based camps, which would ensure both good accessibility and a broader outreach. A solid foundation of trust between girls’ families, program managers, and other stakeholders emerged as a key asset for the program’s success.
School-based vaccination has proven a successful strategy to achieve high HPV vaccine coverage in many countries,17,18 and was previously indicated as the most acceptable approach by adolescents in the United States.19 However, our study participants consistently argued that community-based vaccination delivery would be preferable in the local setting, because it may improve accessibility and promote vaccination uptake among those who do not trust healthcare facilities. In November 2019, Pakistan introduced typhoid conjugate vaccine administration through schools and hospitals. While this program achieved high coverage, with >9.4 million children vaccinated in Sindh province alone,20 its success was largely attributed to comprehensive community engagement, which was crucial to build trust in the newly introduced vaccine and preempt refusals.20 Although school-based HPV vaccination has been strongly recommended for low-middle income countries (LMICs),21 other strategies may be considered in a country like Pakistan, where mass immunization campaigns and outreach activities are regularly implemented in the community.22
Trust emerged as a key asset to persuade parents to provide consent and to maintain high schedule completion rates among girls. Little research exists to explicitly examine the concept of trust in the context of vaccination, especially in LMICs.23 Recent findings from Pakistan suggest fixing supply-oriented problems within immunization programs would be key to increase trust in vaccination among citizens.24 Evidence from Europe showed that lack of trust in health authorities, healthcare workers, and new vaccines was significantly associated with increased HPV vaccine hesitancy.11 However, determinants of trust may vary across epidemiologic conditions, cultural norms, and socio-political environment.25 More in-depth research is needed to better define the nuances of trust in the local context and build resilience against factors potentially undermining it over time.
This study revealed significant knowledge gaps and misconceptions regarding female reproductive health among adolescent girls. In Pakistan, the school curriculum lacks formal reproductive health education, and discussion of female reproductive health is attached to stigma and social taboo.26 Thus, most adolescents are unequipped to nurture and adequately take care of their health.27 The timely addition of sexual and reproductive health components to the primary and secondary school curriculum would be essential to pave the way for future educational campaigns promoting HPV vaccination.
Adolescents who took part in this study were able to formulate their informational needs in an accurate, detailed manner. Their proposed educational campaign included peer education, and they often carved out a role for themselves as information messengers for their family. Actively leveraging adolescents’ existing motivation and drive could boost the impact of a potential educational campaign and vaccination program, especially because adolescents’ attitudes may have a direct positive influence on parental decisions on whether to consent to HPV vaccination.28–30
Although none of the participants expressed any sort of anti-vaccine sentiment themselves, several girls revealed that anti-vaccine attitudes are deeply entrenched in their families. This confirms findings from a previous study in Karachi, where only 20% of adult women stated they would consent to their daughter being vaccinated against HPV.31 Hesitancy with regards to HPV vaccination is also common in other LMICs in the same region, and is often attributable to similar concerns regarding the vaccine’s safety and efficacy.32,33 In addition, HPV vaccination is designed to prevent illness much later in life, which may be more difficult for both parents and adolescents to appreciate. In existing HPV vaccination programs, public misconceptions regarding the vaccine were the most frequently reported obstacle to vaccine uptake.6,33 Future research efforts could be directed toward interviewing parents and caregivers to understand their perspectives and perceptions around the HPV vaccine, and further investigate the possible reasons and remedies for vaccine hesitancy.
Unlike young children, adolescents exhibit an expanding capacity to make informed choices. Their involvement into health decisions that are directly relevant to them, including vaccination, is increasingly valued around the world.34 However, parents’ authority in making decisions on their children’s health is often prioritised over young people’s autonomy, and this can have direct implications on the acceptance of vaccination programs.35 This finding is consistent with our study’s finding which confirms male family members particularly fathers as a key decision-maker in family.
Limitations
Knowledge of female reproductive health, cervical cancer, and HPV vaccine was limited among study participants, restricting the scope and depth of the FGDs. However, most girls demonstrated a sufficient level of understanding for a prolific discussion to be established, and they were able to draw on the available information to develop pertinent recommendations.
We observed a high consent refusal rate (70%), one of the reasons for which was that caregivers worried that the girls may get vaccinated against HPV if they participated in the study. While this may limit our sampling frame in terms of generalizability, it also corroborates the finding that vaccine hesitancy against HPV would be a challenge that will have to be addressed as part of the future roll-out of an HPV Program in the country. None of the approached girls mentioned fear of SARS-CoV-2 infection as a reason for refusing to take part in this study. However, refusal data was not collected systematically, so it is possible that this may have played a role. Moreover, girls did not express any unease in sharing their ideas within their discussion group, and gave explicitly positive feedback on both their interactions with the team and the overall environment during the FGDs.
Finally, parental attitudes toward vaccination were reported through the lens of their adolescent daughters, and may not fully correspond to parents’ actual stances.
Conclusions
This formative research helped develop a set of context-specific recommendations for the implementation of an HPV vaccination program in Pakistan reflective of adolescent girls’ perspectives. Based on the participants recommendations, the following strategies should be explored for successful implementation of an HPV vaccination program in Pakistan; establishing trust with vaccine providers, increasing accessibility of vaccinations and vaccine-related knowledge through community-based informational campaigns and vaccination camps, and informing key decision-makers in the family, particularly fathers, of the long-term benefits of HPV vaccination to counter vaccine hesitancy and refusal.
Acknowledgements
We would like to acknowledge all participants for their effort and time devoted to this study, as well as school managers and staff for facilitating the study implementation. In addition, we would like to thank Dr. Jane Mingjie Lim who contributed to developing the research questions, the IRD field team and Ms. Razia Begum Abdul Majeed (Lady Health Worker) who helped conduct participant recruitment and data collection for the study.
Funding Statement
This work was supported by the National University of Singapore – Saw Swee Hock School of Public Health Infectious Disease Program under Grant [PRG/PILOTGRANT/2018/02]; and through internal funding of Maternal & Child Health Program, IRD Global.
Contribution to authorship
VO, GK, and CCT conceptualized the idea. SA and VO drafted the protocol with input from DA and SC. RFA and AM implemented the study with support from VO, DA, and SC. RFA, NN and AM collected the data. RFA conducted the initial analysis while VO finalized the analysis. SC and DA provided advice for interpretation of research findings. VO and RFA wrote the first draft of manuscript and finalized with intellectual input from SC, DAS and SA. All authors contributed to critically revising the manuscript and approved the final article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics approval
This study was approved by the Institutional Review Board of Interactive Research and Development (IRD_IRB_2020_04_001) and the Institutional Review Board of the National University of Singapore (S-19-030).
References
- 1.Torgovnik J. Cervical Cancer. World Health Organization. Geneva (Switzerland): World Health Organization; 2021. Feb 18 [accessed 2021 Dec 10]. https://www.who.int/health-topics/cervical-cancer#tab=tab. [Google Scholar]
- 2.Immunization , Vaccines and biologicals. Human papillomavirus vaccines (HPV). World Health Organization. Geneva (Switzerland): World Health Organization; 2021. Feb 16 [accessed 2021 Dec 10]. https://www.who.int/teams/immunization-vaccines-and-biologicals/diseases/human-papillomavirus-vaccines-HPV. [Google Scholar]
- 3.International Agency for Research on Cancer . CANCER TODAY: data visualization tools for exploring the global cancer burden in 2020. World Health Organization; 2021. Feb 16 [accessed 2021 Dec 10]. https://www.who.int/teams/immunization-vaccines-and-biologicals/diseases/human-papillomavirus-vaccines-HPV.
- 4.Albero G, Bosch FX, Bruni L, Collado JJ, de Sanjosé S, Gómez D, Mena M, Muñoz J, Serrano B. Human papillomavirus and related diseases report in Pakistan. Barcelona (Spain): ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre); 2019. [accessed 2021 Dec 10]. https://hpvcentre.net/statistics/reports/XWX.pdf. [Google Scholar]
- 5.Raza SA, Franceschi S, Pallardy S, Malik FR, Avan BI, Zafar A, Ali SH, Pervez S, Serajuddaula S, Snijders PJF, et al. Human papillomavirus infection in women with and without cervical cancer in Karachi, Pakistan.Br. J Cancer. 2010;102(11):1657–9. PMID: 20407442. doi: 10.1038/sj.bjc.6605664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ladner J, Besson MH, Audureau E, Rodrigues M, Saba J.. Experiences and lessons learned from 29 HPV vaccination programs implemented in 19 low and middle-income countries, 2009-2014. BMC Health Serv Res. 2016;16(1):575. PMID: 27737666. doi: 10.1186/s12913-016-1824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallagher KE, Howard N, Kabakama S, Jack SM, Griffiths UK, Feletto M, Burchett HED, LaMontagne DS, Jones DW. Lessons learnt from human papillomavirus (HPV) vaccination in 45 low-and middle-income countries. PloS One. 2017;12(6):e0177773. PMID: 28575074. doi: 10.1371/journal.pone.0177773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kabakama S, Gallagher KE, Howard N, Jack SM, Burchett HED, Griffiths UK, Feletto M, LaMontagne DS, Jones DW. Social mobilisation, consent and acceptability: a review of human papillomavirus vaccination procedures in low and middle-income countries. BMC Public Health. 2016;16(1):1–10. doi: 10.1186/s12889-016-3517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pakistan Bureau of Statistics . District-Wise census results. Islamabad (Pakistan); [accessed 2021 Feb 16]. https://web.archive.org/web/20170829164748/http://www.pbscensus.gov.pk/sites/default/files/DISTRICT_WISE_CENSUS_RESULTS_CENSUS_2017.pdf. [Google Scholar]
- 10.Rehman A, Jingdong L, Hussain I. The province-wise literacy rate in Pakistan and its impact on the economy. Pac Sci Rev. 2015;1(3):140–44. doi: 10.1016/j.psrb.2016.09.001. [DOI] [Google Scholar]
- 11.Karafillakis E, Simas C, Jarrett C, Verger P, Peretti-Watel P, Dib F, De Angelis S, Takacs J, Ali KA, Pastore Celentano L, et al. HPV vaccination in a context of public mistrust and uncertainty: a systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum Vaccin Immunother. 2019;15(7–8):1615–27. PMID: 30633623. doi: 10.1080/21645515.2018.1564436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Division CK Administrative districts. Karachi (Pakistan): Commissioner Karachi Division; [accessed 2021 Feb 16]. https://commissionerkarachi.gos.pk/districts.html.
- 13.Bureau of Statistics . Development statistics of Sindh. Government of Sindh. Karachi (Pakistan): Bureau of Statistics; [accessed 2021 Mar 17]. www.sindhbos.gov.pk. [Google Scholar]
- 14.Mary Alison Durand TC. Principles of social research. Chapter 8. 2nd ed. Open University Press; 2014. [Google Scholar]
- 15.Judith Green NT. 2018. Qualitative methods for health research. Chapter 8, 9. 3rd ed. [Google Scholar]
- 16.Adams P. Reaching teenagers with three-times jab is a first for most countries: now that the GAVI alliance has agreed to subsidize the HPV vaccine, many low-income countries have the chance to roll out the HPV vaccine nationally–an opportunity for women’s health. Bull World Health Organ. 2012;90:874–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Das JK, Salam RA, Arshad A, Lassi ZS, Bhutta ZA. Systematic review and meta-analysis of interventions to improve access and coverage of adolescent immunizations. J Adolesc Health. 2016;59(4):S40–S48. PMID: 27664595. doi: 10.1016/j.jadohealth.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Binagwaho A, Wagner CM, Gatera M, Karema C, Nutt CT, Ngaboa F. Achieving high coverage in Rwanda’s national human papillomavirus vaccination programme. Bull World Health Organ. 2012;90:623–28. PMID: 22893746. doi: 10.2471/BLT.11.097253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramanadhan S, Fontanet C, Teixeira M, Mahtani S, Katz I. Exploring attitudes of adolescents and caregivers towards community-based delivery of the HPV vaccine: a qualitative study. BMC Public Health. 2020;20(1):1–10. doi: 10.1186/s12889-020-09632-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qamar FN, Batool R, Qureshi S, Ali M, Sadaf T, Mehmood J, Iqbal K, Sultan A, Duff N, et al. Strategies to improve coverage of typhoid conjugate vaccine (TCV) immunization campaign in Karachi, Pakistan. Vaccines. 2020;8(4):697. PMID: 33228111. doi: 10.3390/vaccines8040697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard N, Gallagher KE, Mounier-Jack S, Burchett HED, Kabakama S, LaMontagne DS, Watson-Jones D, et al. What works for human papillomavirus vaccine introduction in low and middle-income countries? Papillomavirus Res. 2017;4:22–25. PMID: 29179865. doi: 10.1016/j.pvr.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasan Q, Bosan A, Bile K. A review of EPI progress in Pakistan towards achieving coverage targets: present situation and the way forward. East Mediterr Health J. 2010;16(Supp):31–38. doi: 10.26719/2010.16.Supp.31. [DOI] [PubMed] [Google Scholar]
- 23.Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, Patersona P. Measuring trust in vaccination: A systematic review. Hum Vaccin Immunother. 2018;14(7):1599–609. PMID: 29617183. doi: 10.1080/21645515.2018.1459252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ali SAM, Altaf SW. Citizen trust, administrative capacity and administrative burden in Pakistan’s immunization program. J Behav Public Administration. 2021;4(1). doi: 10.30636/jbpa.41.184. [DOI] [Google Scholar]
- 25.Justwan F, Baumgaertner B, Carlisle JE, Carson E, Kizer J. The effect of trust and proximity on vaccine propensity. PloS One. 2019;14(8):e0220658. PMID: 31461443. doi: 10.1371/journal.pone.0220658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bashir Q, Usman A, Amjad A, Amjad U. The Taboo that silences’: Awareness about sexual and reproductive health issues among adolescent females during pubertal transition. Isra Med J. 2017;9:381–85. [Google Scholar]
- 27.Pal SA. Premarital health and social issues in Pakistan. Jpma. 2017;67:973–74. [PubMed] [Google Scholar]
- 28.Alexander AB, Stupiansky NW, Ott MA, Herbenick D, Reece M, Zimet GD. Parent-Son decision-making about human papillomavirus vaccination: a qualitative analysis. BMC Pediatr. 2012;12(1):1–9. PMID: 23241217. doi: 10.1186/1471-2431-12-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zimet GD, Silverman RD, Bednarczyk RA, English A, et al. Adolescent consent for human papillomavirus vaccine: ethical, legal, and practical considerations. J Pediatr. 2021;231:24–30. doi: 10.1016/j.jpeds.2021.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Toffolon-Weiss M, Hagan K, Leston J, Peterson L, Provost E, Hennessy T. Alaska ative parental attitudes on cervical cancer, HPV and the HPV vaccine. Int J Circumpolar Health. 2008;67(4):363–73. PMID: 19024805. doi: 10.3402/ijch.v67i4.18347. [DOI] [PubMed] [Google Scholar]
- 31.Ismail H, Rafiq S, Shakoor S, Karim MT, Raheel R. Assessing the role of education in adult women’s knowledge and awareness of human papillomavirus and human papillomavirus vaccine. Jamc. 2017;29(1):128–31. PMID: 28712191. [PubMed] [Google Scholar]
- 32.Santhanes D, Wong CP, Yap YY, San SP, Chaiyakunapruk N, Khana TM. Factors involved in human papillomavirus (HPV) vaccine hesitancy among women in the South-East Asian Region (SEAR) and Western Pacific Region (WPR): a scoping review. Hum Vaccin Immunother. 2018;14(1):124–33. PMID: 28933635. doi: 10.1080/21645515.2017.1381811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Santhanes D, Yong CP, Yap YY, Saw PS, Chaiyakunapruk N, Khan TM. Factors influencing intention to obtain the HPV vaccine in South East Asian and Western Pacific regions: A systematic review and meta-analysis. Sci Rep. 2018;8(1):1–11. PMID: 29483541. doi: 10.1038/s41598-018-21912-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Katz AL, Webb, SA; COMMITTEE on BIOETHICS . Informed consent in decision-making in pediatric practice. Pediatrics. 2016;138(2). PMID: 27456510. doi: 10.1542/peds.2016-1485. [DOI] [PubMed] [Google Scholar]
- 35.Fisher H, Harding S, Hickman M, Macleod J, Audrey S. Barriers and enablers to adolescent self-consent for vaccination: A mixed-methods evidence synthesis. Vaccine. 2019;37(3):417–29. PMID: 30573357. doi: 10.1016/j.vaccine.2018.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


