Abstract
Introduction.
While a growing body of research examines individual factors affecting the prevalence and management of hypertension among Latinos, less is known about how socioecological factors operate to determine health and affect implementation of interventions in rural communities.
Method.
We conducted eight focus groups to assess perceived risks and protective factors associated with managing hypertension among Latino adults and their family members living in two rural/frontier counties in the U.S.–Mexico border region. This analysis is part of a larger study, Corazon por la Vida (Heart for Life), which involved multiple data collection strategies to evaluate the effectiveness of a primary care and a promotora de salud intervention to manage hypertension.
Results.
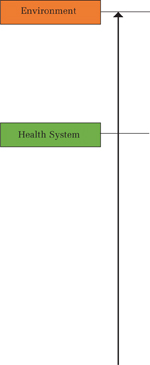
Of the 49 focus group participants, 70% were female and 30% were male, 39% were Spanish-only speakers, and 84% had hypertension. Participants’ ages ranged between 18 and 75 years, and 63% reported annual incomes below $30,000. Drawing from a social–ecological framework to analyze focus group data, four major themes and subthemes emerged as factors facilitating or inhibiting disease management: (1) individual (emotional burdens, coping mechanisms), (2) social relationships (family as a source of support, family as a source of stress), (3) health system (trust/mistrust, patient–provider communication), and (4) environment (lack of access to safe exercise environment, lack of affordable food).
Conclusion.
Our findings are relevant to public health practitioners, researchers, and policymakers seeking to shift from individual level or single interventions aimed at improving treatment-modality adherence to multilevel or multiple interventions for rural Latino communities.
Keywords: hypertension, Hispanic Americans, disease management, focus groups, implementation research
In the past 30 years, the prevalence rates of hypertension among Latinos have shown an upward trend. From 1994 to 2016, hypertension rates in adults of Mexican origin increased from 25.0% in women and 26.9% in men to 30.1% in women and 27.9% in men (National Center for Health Statistics, 2019). The prevalence of hypertension in Latino populations is characterized by low levels of awareness and treatment control as compared with other populations (Elfassy et al., 2020; Foti et al., 2019; Hicks et al., 2005). Other factors associated with the increased risks for hypertension among Latino adults include gender, age, migration/acculturation, and socioeconomic position (Cooper-DeHoff et al., 2007; Thomas & Allison, 2019). Additionally, Latinos experience other barriers to needed care such as the high cost of health care, high rates of uninsurance, immigration status (Cristancho et al., 2008; Reininger et al., 2014), language barriers, and discrimination (Elder et al., 2009).
The past two decades of research has demonstrated the efficacy of chronic disease self-management interventions (Barlow et al., 2002; Turnbull et al., 2020). Previous racial and ethnic health disparities research has underscored how psychosocial risk factors such as social support, social class, hostility, and depression are linked to illness (Syme et al., 2019). More recently, studies have examined the potential of coordinated home-based, community population health, and culturally adaptive interventions for improving cardiovascular risk factors in Latinx populations (Langabeer et al., 2018; Mudd-Martin et al., 2013; Rocha-Goldberg et al., 2010; Thomas & Allison, 2019). Yet despite the evidence for socioecological interventions and calls for research in rural settings (National Academies of Sciences, Engineering, and Medicine, 2017), health disparities research has mostly tested individual-level interventions in urban settings (Carey et al., 2018; Eakin et al., 2007).
Advancing the science of interventions requires a more dynamic perspective on the role of social determinants of health on cardiovascular diseases (Kreatsoulas & Anand, 2010), including the effect of social networks and social support in neighborhoods (Agurs-Collins et al., 2019; Cristancho et al., 2008). These interventions require innovative approaches that incorporate individuals, families, and organizations in ways that capture the experiences of Latinx peoples from within their specific and unique social, cultural, and structural settings (Baquero & Parra-Medina, 2020; National Academies of Sciences, Engineering, and Medicine, 2017). Our article addresses the need to understand the wider range of determinants that either improve or worsen chronic conditions among Latinos in the United States. Drawing from a larger study comparing the effectiveness of community health workers, social support and primary care with primary care only, we analyze eight focus groups composed of Latinos living in two rural/frontier counties in the U.S.–Mexico border region.
METHOD
Setting
The intervention study took place in two rural counties in the southern U.S.–Mexico border region of New Mexico, which we will refer to by pseudonyms here—Copper County and Burg County—in order to protect the confidentiality of these border communities. Both communities are ideal sites for understanding the influence of interventions from a socioecological lens. Copper County is predominately rural, with a population of 29,514 and 7.4 persons per square mile; the neighboring Burg County qualifies as a frontier community, with a population of 4,894 and 1.4 persons per square mile (U.S. Census Bureau, 2012). Once known for their lumber, mining, and agricultural production, both counties now experience extremely high poverty rates: unemployment in the region ranges from 8.3% in Copper County to 6.6% in Burg County, with neighboring counties having rates of unemployment above 20% (U.S. Census Bureau, 2012).
In these rural settings, it is common for residents to drive 2 to 4 hours, through national forests and the Chihuahuan Desert Plains, to access supermarkets, health centers, or social and cultural activities (Bruna et al., 2014). Rates of uninsured in the study area are 25% in Burg County and 20% in Copper County, compared with the statewide rate of 23% (U.S. Census Bureau, 2010). The ratio of primary care physicians to population size is higher for these two counties than the rest of the nation (1,226:1 vs. 2,596:1; U.S. Census Bureau, 2012). Latinos living in Copper County are less likely than non-Latino Whites to be physically active (33.8% vs. 12.6%), to have a higher prevalence of high blood pressure (29.2% vs. 23.4%) and diabetes (17.1% compared with 3.3%), and to be overweight or obese (81% vs. 59%; U.S. Census Bureau, 2012).
Sample
The focus group data are from a larger multilevel chronic disease trial, Corazon por la Vida (CPLV, Heart for Life), which involved multiple data collection strategies and measures in order to compare the effectiveness of primary care–only versus a promotora-led health education curriculum to manage hypertension among Hispanics (Sánchez et al., 2014). The study protocol was approved by the Institutional Review Board of the University of New Mexico Health Sciences Center (HRRC No. 10–634). We conducted eight focus groups (three in Spanish and five in English) that were composed of participants in the CPLV intervention (January to June 2013). The purpose of the focus groups was to explore the perceptions and experiences of the intervention participants and their families regarding how they managed living with hypertension. Questions in the focus group were designed to elicit personal, family, and social resources that enable or inhibit lifestyle changes. The focus group guides are available in the Supplemental Material.
Participants for the focus groups were recruited from the total sample of patients (115) who agreed to participate in the intervention. The intervention group was derived from the larger pool of 920 Hispanic hypertension patients actively enrolled with the primary care clinic. Of the 128 eligible patients for the intervention, 115 enrolled and 13 dropped the study resulting in a final enrollment of 102. Patients for the intervention study were recruited, consented, and enrolled in three waves. To assess the perspectives and experiences of participants, we intentionally recruited a smaller sample of individuals into the focus groups that were representative of the total sample. For the focus groups, a letter of invitation in English and Spanish was distributed to the patients by the medical director and recruited by the promotoras de salud. Consent agreement occurred after the affirmative response from the invitation letter. Based on feedback from the promotoras who participated in the development of the intervention design, it was recommended that family members be invited to the focus groups. This is a culturally responsive innovation of the research in order to recognize the strong role that familial ties play in disease management and daily lifestyle and behavior change.
Of the 49 focus group members, 70% were female (n = 34) and 30% were male (n = 15), 39% were Spanish-only speakers (n = 19), and 16% were family members (n = 8). Members’ ages ranged between 18 and 75 years, and 63% reported annual incomes below $30,000. The size of the eight focus groups varied between three and nine participants. This allowed for ample time for discussion and assured inclusion of voice across participants (see Table 1).
TABLE 1.
Focus Groups (N = 8) Participant Demographics
| Individual characteristics | n | % |
|---|---|---|
| Participant sex | ||
| Male | 15 | 30.61 |
| Female | 34 | 69.39 |
| Language | ||
| English | 30 | 61.22 |
| Spanish only | 19 | 38.78 |
| Income ($) | ||
| 0–10,000 | 10 | 20.41 |
| 11,000–20,000 | 11 | 22.45 |
| 21,000–30,000 | 10 | 20.41 |
| 31,000+ | 7 | 14.29 |
| No answer | 11 | 22.45 |
Analysis
Our conceptual framework informing our data analysis draws from the social–ecological model (SEM) that examines the multiple influences and interrelationships between personal and environmental factors that influence the management of chronic conditions (Stokols, 1996). First introduced by Bronfenbrenner (1977), the SEM provides a way to conceptualize a wide array of determinants that influence chronic conditions and inform multilevel interventions aimed at reducing health disparities (Bronfenbrenner, 1977). We adapted the SEM to include four levels to guide our data analysis: (1) Intrapersonal: Individual-level factors that inform or guide, generally attitudes, behaviors, knowledge, personal practices, and skills; (2) Interpersonal: The influence of and interaction between family, peers, friends, and close social networks; (3) Organizational/community: Programs or services; settings, for example, health care organizations, schools, workplaces, and churches; and (4) Built environment: The greater physical and social environment, including, for example, elements of the infrastructure such as streets, open spaces, and food deserts. Using the SEM as a framework for our analysis, we examine the interplay between the intra- to interpersonal behaviors with organizational/community and the larger built environment (McLeroy et al., 1998).
Focus groups conducted in English were recorded, transcribed, and reviewed by members of the research team for accuracy. Focus groups conducted in Spanish were transcribed, translated into English by a professional transcription company, and reviewed by bilingual members of the research team for accuracy. All files were saved in NVivo (QSR International, 2020) for team coding and analysis. Qualitative data analysis followed procedures outlined by Ryan and Bernard (2000) where researchers identified themes, built codebooks, marked texts, and applied to models. A preliminary code book of likely major themes was developed and later expanded to include subthemes that emerged from the focus groups and the coding process (Corbin & Strauss, 1990; Rubin & Rubin, 1995; Silverman, 1993).
Three team members independently coded all transcripts based on the preliminary codebook. Team members then adopted thematic content analysis in an iterative process (Green & Thorogood, 2013). Coding differences were discussed and reconciled in regular group discussions. Relevant quotes were grouped together, which allowed team members to develop interpretive memos and reports (Saldaña, 2012) for an understanding of personal to environmental perspectives of hypertension management.
RESULTS
Several major themes emerged from our analysis as summarized in Table 2 that reflect the socioecological determinants and exemplary quotes from more downstream individual behaviors to midstream family and social relationships to the more upstream health system and environmental conditions.
TABLE 2.
Socioecological Determinants of Hypertension Management Among Latinos Living in the U.S.–Mexico Border Region
| Theme | Subtheme | Sample quotes |
|---|---|---|
|
Lack of safe exercise environments | We don’t have a place to walk here, you know. Most communities have a park where people gather and they can walk; we don’t. |
| Lack of affordable food | The prices have doubled in the last year, the olive oil. The reason I buy the vegetable oil is because I buy the big one and then it’s like $5.98 and olive oil is a couple dollars more … The fruits and vegetables have gone up in price too. | |
| Well, yes, sometimes you have with what to buy but sometimes it becomes difficult to buy in large quantities, because the vegetables are expensive, all vegetables are very expensive. | ||
| Trust/mistrust | What I would like is the doctors to be more humanist, that they could be doctors for vocation, any profession with vocation is very beautiful and very decent, a doctor without vocation doesn’t work. Well, I trust my doctor because she has been so human, so pretty, she explains, she asks, she does talk to you, she asks you what happens to you, how do you feel, and she puts a special attention on me that I have never received. | |
| My doctor told me I’m supposed to take it twice a day, but I only take it once a day ‘cuz I’m kind of afraid of the pill. It seems to me like they control me instead of me in control of the pill [laughter]. But I suppose I’m doing okay now. I’m still taking my pills every day. | ||
| Quality of patient–provider communication | But a lot of people are afraid to communicate with their doctor or they don’t hear anything else. So. And I always tell everybody, “Take somebody else with you to your appointment, because you don’t hear everything that they’re telling you.” | |
| When I’ve gone sometimes to the doctor when they try, I know they’re busy. They try and scoot you out the door and not answer all the fully questions that you need to be answered. | ||
| There’s no dialogue. It’s just “What do you have? What is your pain? Or what do you have? The ears, the nose or the eyes? Or this or the other …” and there, nothing … | ||
| (No hay un diálogo. Éste … ¿qué tienes? ¿Qué te duele? O ¿qué tienes? O los oídos, la nariz, con los ojos, o esto o lo otro … y de allí nada ni …) | ||
|
Family as a social support | The only thing I can say is, my family keeps me going. My grandkids and my kids, because they have me going here, there, do this, do that. That’s what helps me. |
| But uh, then I met my wife now, and she helped me out a lot. That is one of my biggest inner strengths is my wife. 42 years she stuck with me. | ||
| Well, we exercise. We split the housework, cooking, doing the dishes, laundry, takes pressure off her to have this or that done. Get home in the evening, might do the laundry or I might fix the meal, do the dishes, days off I change sheets, make beds. It just lessens the workload on her, it makes it easier. | ||
| Family as a source of stress | A lot of the families don’t know how to help you. I mean, they’re in the same, same you know, they’re in the same boat that we’re in. You know? | |
| I said [to my brothers and sisters], “Well, can’t you understand that this is a problem? A pill isn’t going to take care of it, you need to help bring her stress factors down, don’t call her and give her the woe-is-me I don’t have the money for this, or I don’t do this, or call and tell her, ‘I’m mad at my kids because they didn’t do this or that,’ or ‘So-and-so is saying’”—I tell them, “She’s far away enough, just call and say, ‘Mom, how are you?’ Don’t put any more weight. | ||
| Cultural traditions | I think the hard part is the traditional, you know, what our families have shown us and stuff, I mean it’s just hard. I mean the tacos, the flautas, or tostadas. So all that, you know, and I mean, I’m so used to doing that, I don’t know. I mean I think it’s harder to try something different because I’m so used to the traditional stuff we have in our families. | |
| And then, like I’ve changed a lot of what I eat, but I still need to know the right way to cook. Because it’s very hard to have my family and they want to eat what I make, and that’s what makes it hard for me to you know. A lot of times, it’s a lot of fat. And that’s not good for the family. Yeah. | ||
|
Emotional burdens | You know, being stressed out, I know because I’ve been there. My grandma just passed … and we—me and my mom—took care of her 24/7.… And I went to the doctor because I have headaches, headaches, and more headaches. |
| And I see that it’s a sadness … and in the afternoon it’s the same and I am sorry because I am so foolish because I don’t accept … that I only accept God’s will that I am human, and I tell you that one mourns one’s parents, one’s husband, hey, but mourning a son … no, there is no pain.… No, there is no bigger pain. | ||
| See, that’s the way I think. If you’re going to dwell on something, it’s going to happen to you. And if you think negatively instead of so positive about what your health is, you’re going to, you’re going to get your health down. And I don’t think like that. I try and think positive thoughts. | ||
| I also feel that if you have some kind of faith that you can cling on to, that helps. That helps a lot. Knowing there is some superpower over there that might listen to you. Just deep breathing, and exercises, breathing exercises, and there’s many little things we can do. | ||
| Coping mechanisms | I think um, exercise itself will help relieve your stress. And it’s—not only your faith, but exercise, getting out. Not um, being at home all the time and worrying about your kids, worrying about your husband, worrying about the things at home, like getting out and just enjoying something that you really like to do. | |
| And so finally I calm myself down. Or I’ll take a long walk. And uh, if I need to go without him, just to work it out. And I come back, and I feel relieved. And if I’m driving or I’m walking, I’m praying, I’m talking to my dear lord, get me out of this, I’m okay. |
Individual Behaviors
Two subthemes emerged from both intervention participants and their family members across focus group data regarding individual behaviors that inhibited or supported how they managed their hypertension: emotional burdens and coping mechanisms.
Emotional Burdens.
Intervention participants expressed the need to balance their emotions in response to learning about their diagnosis and/or interrelated life events, such as the impact that death or loss of a family member had on how they coped with their own health. These burdens included stressors such as feelings of sadness, depression, or fear. For instance, a participant shared, “When I found out I had high blood pressure I got depressed” and family members of participants in the study explained,
He becomes very sad, he just wants to go sleep … he’s depressed. … When people are depressed they say, I don’t want to do this.
While the participant above recognized her own loss and stress, others explained that stress resulting from death of family members was initially recognized by their health provider. For example, another individual stated,
You know, being stressed out, I know because I’ve been there. My grandma just passed away in January and we—me and my mom—took care of her 24/7, and that’s where mine came from. And I went to the doctor because I have headaches and finally he’s like, “You are stressed out.”
Coping Mechanisms.
To address emotional burdens, intervention participants used a spectrum of coping mechanisms that helped them manage their hypertension and the associated emotions and stress. One woman explained that when she felt scared or stressed, she would go to her room and cry, while others said they would “lay down until they found the strength” to acknowledge the situation at hand. In contrast, other participants expressed that when they did not feel well, they exercised to relieve stress. As one individual explained,
It is important to get out and just enjoying something that you really like to do [instead of] be[ing] at home all the time and worry about your kids, worry about your husband …
Other focus group participants relied on faith and spirituality as a coping mechanism. They talked about how being in nature, having a spiritual life, and giving to others helped them manage their health. One woman shared,
Some places you can go to clear your mind in the community, the church for example. The church, and going to visit a sick one, you go to visit people in jail, go to the hospitals. This is very big, because what you give you receive.
Others expressed similar relationships with faith:
I also feel that if you have some kind of faith that you can cling on to, that helps. That helps a lot. Knowing there is some superpower over there that might listen to you … and there’s many little things we can do.
Social Relationships
The notion of self-management was clearly one dimension of how participants described hypertension management. However, an even more noteworthy theme in hypertension management was the role of family (as a support and stressor) and the influence of culture in managing their hypertension.
Family as a Social Support.
Most of the participants in both the individual and family focus groups viewed their families as sources of support. For instance, one female participant stated,
The only thing I can say is, my family keeps me going. My grandkids, and my kids, because they have me going here, there, do this, do that. That’s what helps me.
Focus group participants in the intervention reported that through participation in the CPLV, behavioral changes such as choosing and preparing healthier food expanded not only beyond their group or family but also to their extended family members. One individual in a postintervention family focus group explained,
My aunt, she started buying, like, the whole wheat stuff and I started doing it too. And my mom, she also has the same, the high blood pressure problem … and my mom has also started, like, buying the whole wheats, and my aunt has helped her, like, with the labels. So I’ve changed my cooking too because of my aunt. Because sometimes I’ll take her food or, ‘cuz most of the time she’s alone.
Family members offered other kinds of social support, including the sharing of child care and household duties so that participants could exercise. One family member stated,
We support each other by exercising … when she, goes to exercise I’ll watch her mom and the kids. We exercise. We split the housework, cooking, doing the dishes, the laundry. It takes pressure off her.
Family as a Source of Stress.
Other participants, women in particular, acknowledged that while families can be supportive, they are also sources of stress. They expressed that they carried the burden of managing household duties and regularly identified these traditional gender roles as burdens in managing either their own or their family member’s hypertension. Women spoke about “family as a stressor,” for instance, one woman explained,
I think it’s just that the women are really the ones that carry the burden in the household, their children, their parents, their grandchildren, you know? The bills.
Another participant expanded on this to show the burden of being isolated in the home due to child care and chores:
I need to leave. I need to go, by myself. But there’s no way I can go anywhere, but there is my boy that’s 14 years old that will always be with me. I’m going to need to play a day, to where it’s going to be my husband and I, for a weekend out. I’m constantly doing something, all day long, seven days a week, nonstop.
Traditional Food Practices.
Many individuals in the family focus group discussed the influence of cultural practices and expectation to prepare traditional foods as challenges. For example, individuals in a family focus group discussed the resiliency of traditional cooking methods for Latino foods. A family member explained,
I think the hard part is the traditional, you know, what our families have shown us and stuff ‘cuz, I mean it’s hard for me because my boyfriend, he works in the mine and, like, I have to make him, like, finger foods because he drives the haul trucks. … And you know I use hamburger meat and I try to drain the grease and everything out it, but I mean I still have to put the salt in it. I mean the tacos, the flautas, or tostadas. I think it’s harder to try something different because I’m so used to the traditional stuff we have in our families.
While traditional food practices posed challenges for some, there is indication that food substitutions were also welcome in postintervention participants as long as the taste of traditional foods was not dramatically changed. As one participant explained,
[The promotora] told us to use this oil, like if I see her [my spouse] going to get the other oil I tell her, “No, get the one you need to use.”
Health System
Patients and family members repeatedly described the nature of their relationship and interactions with their primary care doctor. Two salient issues emerged in the focus groups: trust/mistrust and quality of patient–provider communication.
Trust/Mistrust.
Participants identified trust as fundamental to the quality of the communication they have with their primary care provider. Several described their perception and experiences around not being able to trust “doctors” in general. A family member expressed her concern for her mother and her mother’s reaction to her doctor:
There are so many people sick that it’s like the doctors were experimenting with us. Like, not long ago she felt bad so she started taking her medicine and then she began to vomit and tremble and she talked to the doctor, and he said, “You don’t have to have that …” Then she said, “But I have it, what should I do?” She doesn’t want anything else to do with doctors. She says, “No, what are they going to do for me?”
The lack of trust was discussed more often among the Spanish-speaking patients, many of whom had previous experience with the Mexican health care system. There was a sentiment among participants that doctors in the United States do not consider their work a vocation to humanity like they do in Mexico, which creates mistrust. For instance, one Spanish-speaking female shared,
What I would like is [for] the doctors to be more humanist, that they could be doctors, any profession with vocation is very beautiful and very decent, a doctor without vocation doesn’t work. Well, I trust Dr. Gonzales because she has been so human, she does talk to you, she asks you what happens to you, how you feel, and she puts a special attention on me that I have never received. I would like that because now there are so many contradictions with the U.S. doctors.
Quality of Patient–Provider Communication.
Trust was described in terms of the perceived quality of the communication that the patient had with their doctor. Participants felt it was important that their provider relate to them personally and help educate them on their condition. Participants also expressed that as patients they want to feel understood and listened to by their provider. For instance, one family member described her and her husband’s experience with their primary care physician and the importance of having an advocate to help negotiate their treatment options:
We get good attention from our primary care person. I ask questions, and … she says, “Well, I’m going to do this,” or “No, I don’t think so,” or “Why are you doing it?” But a lot of people are afraid to communicate with their doctor. And I always tell everybody, take somebody else with you to your appointment, because you don’t hear everything that they’re telling you.
Environment
Participants expressed several environmental and policy factors that negatively affected their ability to manage their hypertension. Of central concern were a lack of safe facilities and the lack of affordable high-quality foods.
Lack of Access to a Safe Exercise Environment.
Many individuals in the focus group were in agreement that the frontier landscape did not provide opportunities for safe physical activity, an ongoing need in the desert region (Bruna et al., 2014), particularly for adults with mobility concerns. As one individual explained,
We don’t have a place to walk here, you know. Most communities have a park where people gather and they can walk; we don’t … there needs to be something like more, more secure for older people. Something that if you don’t feel good you can go and you can hold on to, and we don’t have that here … and whenever you start mixing the kids and the elderly, you never know when a kid’s going to run by [and knock you down].
Lack of Affordable Food.
The lack of affordable high-quality supermarkets in the region was a major concern among participants. As explained by one woman,
Not only that, but the prices have doubled in the last year, the olive oil. The reason I buy the vegetable oil is because I buy the big one and then it’s like $5.98 and olive oil is a couple dollars more and I’m like, “Oh no, well this one’s cheaper.” The fruits and vegetables have gone up in price too. Because I buy my girls vegetables through sale. The strawberries were like $1.98 the other day at Walmart, and then I came here and they were like $2 something each.
DISCUSSION
Our findings highlight the experiences of Latinos living with hypertension across multiple social–ecological levels. While a growing body of research has demonstrated the effectiveness of chronic disease management, less is known about the efficacy of multilevel approaches (Liao et al., 2016). Thus, there remains the need to understand how social factors, including communication with providers and family relationships, play a critical role in how patients manage their high blood pressure and overall health. Health care providers may need to consider incorporating a culture-centered approach that would include an understanding of how patients handle fears and practice their spiritual beliefs (Heuman et al., 2013; Koerner et al., 2013).
One theme emerging from research on U.S. Latinos that supports our findings is the importance of family or familismo. Familismo describes “feelings of loyalty, reciprocity, and solidarity towards members of the family” (Sabogal et al., 1987, p. 398), and the notion of the family as an extension of self. A commitment and dedication to one’s family is seen as protective against risk behaviors for Latinos (Elder et al., 2009). In a diabetes study with Latino participants from a rural West Texas community, Heuman et al. (2013) identified a three-tiered set of risk factors for diabetes: heredity, preferences for unhealthy, culturally based foods, and temptations from U.S. mainstream fast-food culture.
We also found a counter theme suggesting that non-supportive family members can affect individual mental and physical health (Repetti et al., 2002). For Latinos, even within the concept of familismo, the caregiving role can prove to be stressful, difficult, and lonely (Gelman, 2014). Recent studies emphasize the burden placed on Latinas in caring for the health of family members and how this inhibits their ability to pursue personal interests, be physically active, or participate in health-promoting behaviors (D’Alonzo & Saimbert, 2013). Latinas as caregivers often lack the support they require (either from family members or social networks and institutions) to engage in physical activities that could promote their own health. Our data indicated that families may not always be key or sole sources of support and interventions must address broader political–economic realities in the home.
Unique from other research on chronic disease management, this study underscores the role of geography on disparities in health and health care. Latinos living in rural areas of the nation face unique challenges in addition to lack of access to transportation, affordable healthy foods, and costly medications (Garcia et al., 2017). The major themes were reflective of the interconnected factors determining a holistic state of health and their “shared community and cultural” context in the rural border region of the United States. As of yet, rural/frontier interventions remain somewhat underexplored in the published intervention literature (Golden & Earp, 2012).
One limitation to the analysis is that we were unable to follow up with the focus group participants to share the results with them and garner their input to develop adaptations for future interventions. Second, we did not assess differences in experiences and attitudes as part of a pre-/postimplementation evaluation, which may have provided a different perspective on influences at multiple levels. In addition, higher female participation is a limitation that may have influenced the findings. However, given the dearth of information on interventions conducted with rural/frontier/border Latino communities, our findings can contribute to future multilevel intervention research.
Regardless, our focus group data illustrated a central tenet of the social–ecological framework: the interdependence between the immediate and more distant contexts of people’s lives (McLeroy et al., 1998; Stokols, 1996). These interdependencies make it clear that interventions must move beyond the personal behavior change modalities to include interventions at the family, community, organizational, environmental, and policy levels (Golden & Earp, 2012; Painter et al., 2008).
Supplementary Material
Acknowledgments
This research is supported by the National Institute of Minority Health and Health Disparities, National Institutes of Health (Principal Investigator, Lisa Cacari Stone, Grant No. 3P20MD004996–01S).
Footnotes
We appreciate the earlier qualitative data analysis of focus groups conducted by Dr. Lavinia Nicolae. We are especially grateful for the dedicated work of the promotoras de salud at Hidalgo Medical Services: Rita Chauvin, Elva Quimby, Gloria Vargas, and Barbara Cabrera. Lisa Cacari-Stone, Victoria Sanchez, Sean Patrick Bruna, Michael Muhammad, and Carmen Zamora all declare no financial or professional conflict of interest related to the content and work of this article.
SUPPLEMENTAL MATERIAL
Supplemental material for this article is available at https://journals.sagepub.com/home/hpp.
REFERENCES
- Agurs-Collins T, Persky S, Paskett ED, Barkin SL, Meissner HI, Nansel TR, Arteaga SS, Zhang X, Das R, & Farhat T (2019). Designing and assessing multilevel interventions to improve minority health and reduce health disparities. American Journal of Public Health, 109(Suppl. 1), S86–S93. 10.2105/AJPH.2018.304730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baquero B, & Parra-Medina DM (2020). Chronic disease and the Latinx population: Threats, challenges, and opportunities. In Martínez A & Rhodes S (Eds.), New and emerging issues in Latinx health (pp. 19–44). Springer. 10.1007/978-3-030-24043-1_2 [DOI] [Google Scholar]
- Barlow J, Wright C, Sheasby J, Turner A, & Hainsworth J (2002). Self-management approaches for people with chronic conditions: a review. Patient Education and Counseling, 48(2), 177–187. 10.1016/s0738-3991(02)00032-0 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513. 10.1037/0003-066X.32.7.513 [DOI] [Google Scholar]
- Bruna S, Stone LC, Wilger S, Cantor J, & Guzman C (2014). The role of community health centers in assessing the social determinants of health for planning and policy: The example of frontier New Mexico. Journal of Ambulatory Care Management, 37(3), 258–268. 10.1097/JAC.0000000000000004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey RM, Muntner P, Bosworth HB, & Whelton PK (2018). Prevention and control of hypertension: JACC health promotion series. Journal of the American College of Cardiology, 72(11), 1278–1293. 10.1016/j.jacc.2018.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper-DeHoff RM, Zhou Q, Gaxiola E, Cangiano JL, Garcia-Barreto D, Handberg E, Pepine CJ, & INVEST Investigators. (2007). Influence of Hispanic ethnicity on blood pressure control and cardiovascular outcomes in women with CAD and hypertension: Findings from INVEST. Journal of Women’s Health, 16(5), 632–640. 10.1089/jwh.2006.0086 [DOI] [PubMed] [Google Scholar]
- Corbin JM, & Strauss A (1990). Grounded theory research: Procedures, canons, and evaluative criteria. Qualitative Sociology, 13(1), 3–21. 10.1007/BF00988593 [DOI] [Google Scholar]
- Cristancho S, Garces D, Peters K, & Mueller B (2008). Listening to rural Hispanic immigrants in the midwest: A community-based participatory assessment of major barriers to health care access and use. Qualitative Health Research, 18(5), 633–646. 10.1177/1049732308316669 [DOI] [PubMed] [Google Scholar]
- D’Alonzo KT, & Saimbert MK (2013). Hispanic women and physical activity. Annual Review of Nursing Research, 31 (October), 209–234. 10.1891/0739-6686.31.209 [DOI] [PubMed] [Google Scholar]
- Eakin EG, Bull SS, Riley KM, Reeves MM, McLaughlin P, & Gutierrez S (2007). Resources for health: A primary-care-based diet and physical activity intervention targeting urban Latinos with multiple chronic conditions. Health Psychology, 26(4), 392–400. 10.1037/0278-6133.26.4.392 [DOI] [PubMed] [Google Scholar]
- Elder JP, Ayala GX, Parra-Medina D, & Talavera GA (2009). Health communication in the Latino community: Issues and approaches. Annual Review of Public Health, 30(1), 227–251. 10.1146/annurev.publhealth.031308.100300 [DOI] [PubMed] [Google Scholar]
- Elfassy T, Hazzouri AZA, Cai J, Baldoni PL, Llabre MM, Rundek T, Raij L, Lash JP, Talavera GA, Wassertheil-Smoller S, Daviglus M, BoothIII JN, Castaneda SF, Garcia M, & Schneiderman N (2020). Incidence of hypertension among US Hispanics/Latinos: The Hispanic Community Health Study/Study of Latinos, 2008 to 2017. Journal of the American Heart Association, 9(12), e015031. 10.1161/JAHA.119.015031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foti K, Wang D, Appel LJ, & Selvin E (2019). Hypertension awareness, treatment, and control in US adults: Trends in the hypertension control cascade by population subgroup (National Health and Nutrition Examination Survey, 1999–2016). American Journal of Epidemiology, 188(12), 2165–2174. 10.1093/aje/kwz177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia MC, Faul M, Massetti G, Thomas CC, Hong Y, Bauer UE, & Iademarco MF (2017). Reducing potentially excess deaths from the five leading causes of death in the rural United States. MMWR Surveillance Summaries, 66(2), 1–7. 10.15585/mmwr.ss6602a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman CR (2014). Familismo and its impact on the family caregiving of Latinos with Alzheimer’s disease: A complex narrative. Research on Aging, 36(1), 40–71. 10.1177/0164027512469213 [DOI] [PubMed] [Google Scholar]
- Golden SD, & Earp JAL (2012). Social ecological approaches to individuals and their contexts: Twenty years of Health Education & Behavior Health promotion interventions. Health Education & Behavior, 39(3), 364–372. 10.1177/1090198111418634 [DOI] [PubMed] [Google Scholar]
- Green J, & Thorogood N (2013). Qualitative methods for health research Sage. [Google Scholar]
- Heuman AN, Scholl JC, & Wilkinson K (2013). Rural Hispanic populations at risk in developing diabetes: Sociocultural and familial challenges in promoting a healthy diet. Health Communication, 28(3), 260–274. 10.1080/10410236.2012.680947 [DOI] [PubMed] [Google Scholar]
- Hicks LRS, Shaykevich S, Bates DW, & Ayanian JZ (2005). Determinants of racial/ethnic differences in blood pressure management among hypertensive patients. BMC Cardiovascular Disorders, 5, Article 16. 10.1186/1471-2261-5-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koerner SS, Shirai Y, & Pedroza R (2013). Role of religious/ spiritual beliefs and practices among Latino family caregivers of Mexican descent. Journal of Latina/o Psychology, 1(2), 95–111. 10.1037/a0032438 [DOI] [Google Scholar]
- Kreatsoulas C, & Anand SS (2010). The impact of social determinants on cardiovascular disease. Canadian Journal of Cardiology, 26(Suppl. C), 8C–13C. 10.1016/S0828-282X(10)71075-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langabeer JR, Henry TD, Perez Aldana C, DeLuna L, Silva N, & Champagne-Langabeer T (2018). Effects of a community population health initiative on blood pressure control in Latinos. Journal of the American Heart Association, 7(21), Article e010282. 10.1161/JAHA.118.010282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Y, Siegel PZ, White S, Dulin R, & Taylor A (2016). Improving actions to control high blood pressure in Hispanic communities: Racial and ethnic approaches to community health across the U.S. project, 2009–2012. Preventive Medicine, 83, 11–15. 10.1016/j.ypmed.2015.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonough MA, & Kamasaki C (2014). An inside look at chronic disease and health care among Hispanics in the United States http://www.lchc.org/wp-content/uploads/Chronic_Disease_Report_2014.pdf
- McLeroy KR, Bibeau D, Steckler A, & Glanz K (1998). Ecological perspective on promotion programs. Health Education Quarterly, 15(4), 351–377. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- Mudd-Martin G, Martinez MC, Rayens MK, Gokun Y, & Meininger JC (2013). Peer reviewed: Sociocultural tailoring of a healthy lifestyle intervention to reduce cardiovascular disease and type 2 diabetes risk among Latinos. Preventing Chronic Disease, 10, Article 130137. 10.5888/pcd10.130137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2017). Chapter 5: Examples of communities tackling health inequity. In Weinstein JN, Geller A, Negussie Y, & Baciu A (Eds.), Communities in action: Pathways to health equity (pp. 211–334). National Academies Press. 10.17226/24624 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2019). Health, United States, 2018 https://www.cdc.gov/nchs/hus/contents2018.htm#Table_022 [PubMed]
- Painter JE, Borba CPC, Hynes M, Mays D, & Glanz K (2008). The use of theory in health behavior research from 2000 to 2005: A systematic review. Annals of Behavioral Medicine, 35(3), 358–362. 10.1007/s12160-008-9042-y [DOI] [PubMed] [Google Scholar]
- QSR International. (2020). NVivo qualitative data analysis software https://qsrinternational.com/nvivo/nvivo-products/
- Reininger BM, Barroso CS, Mitchell-Bennett L, Chavez M, Fernandez ME, Cantu E, Smith KL, & Fisher-Hoch SP (2014). Socio-ecological influences on health-care access and navigation among persons of Mexican descent living on the U.S./ Mexico border. Journal of Immigrant and Minority Health, 16(2), 218–228. 10.1007/s10903-012-9714-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128(2), 330–366. 10.1037/0033-2909.128.2.330 [DOI] [PubMed] [Google Scholar]
- Rocha-Goldberg MDP, Corsino L, Batch B, Voils CI, Thorpe CT, Bosworth HB, & Svetkey LP (2010). Hypertension Improvement Project (HIP) Latino: Results of a pilot study of lifestyle intervention for lowering blood pressure in Latino adults. Ethnicity & Health, 15(3), 269–282. 10.1080/13557851003674997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin HJ, & Rubin IS (1995). Qualitative interviewing: The art of handling data Sage. [Google Scholar]
- Ryan GW, & Bernard HR (2000). Data management and analysis methods. In Densin N & Lincoln Y (Eds.), Handbook of qualitative research (2nd ed., pp. 769–802). Sage. [Google Scholar]
- Sabogal F, Marín G, Otero-Sabogal R, Marín BV, & Perez-Stable EJ (1987). Hispanic familism and acculturation: What changes and what doesn’t? Hispanic Journal of Behavioral Sciences, 9(4), 397–412. 10.1177/07399863870094003 [DOI] [Google Scholar]
- Saldaña J (2012). The coding manual for qualitative researchers (No. 14). Sage. [Google Scholar]
- Sánchez V, Cacari Stone L, Moffett ML, Nguyen PG, Muhammad M, Bruna-Lewis S, & Urias-Chauvin R (2014). Process evaluation of a promotora de salud intervention for improving hypertension outcomes for Latinos living in a rural U.S.-Mexico border region. Health Promotion Practice, 15(3), 356–364. 10.1177/1524839913516343 [DOI] [PubMed] [Google Scholar]
- Silverman D (1993). Interpreting qualitative data: Methods for analyzing talk, text and interaction Sage. [Google Scholar]
- Stokols D (1996). Translating social ecological theory into. American Journal of Health Promotion, 10(4), 282–298. 10.4278/0890-1171-10.4.282 [DOI] [PubMed] [Google Scholar]
- Syme SL, Hyman MM, & Enterline PE (2019). Cultural mobility and the occurrence of coronary heart disease. Journal of Health and Human Behavior,6(4), 178–189. 10.2307/2948634 [DOI] [PubMed] [Google Scholar]
- Thomas IC, & Allison MA (2019). Hypertension in Hispanics/ Latinos: Epidemiology and considerations for management. Current Hypertension Reports, 21(6), 43. 10.1007/s11906-019-0947-6 [DOI] [PubMed] [Google Scholar]
- Turnbull S, Cabral C, Hay A, & Lucas PJ (2020). Health equity in the effectiveness of web-based health interventions for the selfcare of people with chronic health conditions: Systematic Review. Journal of Medical Internet Research, 22(6), Article e17849. 10.2196/17849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2010). Small Area Health Insurance Estimates https://www.census.gov/programs-surveys/sahie.html
- U.S. Census Bureau. (2012). State and county quick facts: New Mexico [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


