Abstract
Coronavirus disease 19 (COVID-19) has posed an unprecedented public health challenge for most countries, and the repeated outbreaks of this disease have created a largest disruption of education systems. The intent of this work was to examine the intersection of COVID-19 fear and mental health consequences among college students in Northern Michigan, a region of the U.S. severely affected by the pandemic. This study was conducted from January 17 to February 25, 2022, two years later since the outbreak of the pandemic, and 151 college students (female, 76) were involved. Participants' potential psychological symptoms, anxiety, happiness, learning difficulty, and demographic information were surveyed. We have three main findings. First, 60.3% of students had tested positive for COVID-19, and more female than male students were affected (female, 69.7%; male, 50.7%). Second, there was a high prevalence of mental problems among college students, with 95.7% of the sample experiencing moderate or severe mood disorders. Third, respondents' education was severely affected by the pandemic, averaging a score of 7.6 on a scale of 10 when asked how much their learning quality was affected. They showed increased fear, stress, and decreased happiness, and these were associated with their learning quality change. Given the impact would be far-reaching, not only college students’ mental health but also their learning difficulties should be monitored during the pandemic. These findings are alarming and timely, and their implications are discussed.
Keywords: COVID-19, Fear, Anxiety, Depression, Learning difficulties, Self-efficacy
Severe acute respiratory syndrome coronavirus (the causative virus of coronavirus disease 2019, COVID-19), first detected in Wuhan, China, in early December 2019, has been seen in many countries, threatens to be one of the most challenging tests faced by humanity in modern history (Mahase, 2020; Pfefferbaum & North, 2020; Rodriguez-Dominguez et al., 2021; Wang, Horby, et al., 2020). So far, the COVID-19 has affected over 491 million reported cases (death rate, 1.28%), according to a recent report (April 4, 2022) from the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (Johns Hopkins University, 2022). There were over eighty million confirmed cases with 982,565 deaths in the U.S., with Michigan among the hardest-hit states in the country, reporting 2,080,612 confirmed cases and 32,863 deaths (Michigan CDC, 2022). People immediately found themselves in an environment at once changed and frustratingly familiar. At the time of this study, the counties in Northern Michigan, where this study took place, had some of the highest confirmed case counts. COVID-19 has created an uncertain world, and the current ongoing COVID-19 pandemic can be one of the most significant global biopsychosocial stressors in living memory to everyone (Torales et al., 2020). It is suggested that the severe psychological consequences for individuals, societies, and the entire public life are perhaps even long-lasting effects, although the full impact of coronavirus is yet to be felt (Brooks et al., 2020; Valtorta et al., 2016).
During the earlier stage (e.g., February – May 2020) of this pandemic, combatting this virus had forced people to recognize the importance of fundamental measures of disease control, including 'physical distancing', 'movement restrictions', and 'physical isolation’. The immediate and comprehensive psychological consequences have been highlighted in quite a few studies (Cullen et al., 2020; Perez-Arce et al., 2021; Pfefferbaum & North, 2020; Wang et al., 2020). Definitely, this pandemic has introduced numerous health concerns across the globe along with various mental health challenges. It was suggested that people's mental distress peaked in the spring of 2020. One group reported that in March 2020, people were quite fearful, averaging a score of nearly 7 on a scale of 10 when asked how fearful they were of COVID-19 (Fitzpatrick et al., 2020). The authors were interested in the question of how the COVID-19 fear was distributed across the States, and reported that over 25% of respondents experienced moderate to severe anxiety symptoms. This was more to estimate the immediate impact of this pandemic on mental health. Because these researchers used a single-item measure for fear, we do not know how the fear changed during the period since the outbreak of the pandemic in the States. As the university context is particular, some researchers reported that the pandemic situation had a negative impact on students (Alemany-Arrebola et al., 2020; Cao et al., 2020; Clabaugh et al., 2021; Khubchandani et al., 2022; Li et al., 2020; Son et al., 2020; Wang et al., 2020). For perhaps the first time in American history, nearly all students at institutions of higher education faced campus closures and transitioned rapidly to remote online education. When more and more cases were reported in the United States, college students' lives dramatically changed as they had to leave campus, adjust to new living circumstances, and adapt to online learning platforms. For instance, in April 2020, college students in New Jersey demonstrated a number of academic and everyday difficulties and high levels of mental health distress (Kecojevic et al., 2020). Specifically, those with higher levels of perceived stress were more likely to be females. Because the studies were conducted before that vaccine was available (for a recent review, see, Khubchandani et al., 2022), we do not know how the pandemic affected college students two years later since the outbreak of the COVID-19 in the U.S., i.e., the long-term impact of the pandemic on college students.
The COVID-19 vaccinations started on December 14, 2020, in the States, and because of the priority setting, most people, including university students and faculties, got vaccinated after January 2021 in Michigan. It was reported that COVID-19 vaccines resulted in significant improvements in mental health since mental distress peaked in the spring of 2020 (Perez-Arce et al., 2021). Although vaccines have been widely distributed and administered among large populations, including college students, vaccine hesitancy and anti-vaccine attitudes exist. So far, no empirical study has examined the gender difference in COVID and vaccine hesitancy after the COVID-19 vaccine era in the States. Here we assessed the vaccination rates, and the positive COVID-19 testing rates in college students, asking whether there was a gender difference on these among college students. We investigated how male and female students reacted differentially, and how the highly naturalistic disease threat implicitly and explicitly influenced college students in Michigan.
The coronavirus pandemic so far has been a series of COVID-19 waves, surges in new cases followed by declines. With the challenging situation around, acceptance of the drastic changes has become hard for people to adapt to, and exactly people resist adopting it. The central aim of this study was to discover how the pandemic produced changes in college students, how it influenced students' fear, stress, and happiness, and how these factors jointly influenced their academic performance. Therefore, unique to our study, participants' mental health before the outbreak of COVID-19 and after the vaccine era (i.e., January-February, 2022) and their learning and self-efficacy were surveyed. We expected that 1) the prevalence of COVID-19 was higher in male than female students (Abate et al., 2020); 2)the vaccinations decreased participants' anxiety, stress, and the relevant mental disorder levels after the COVID-19 vaccine era (Nguyen, 2021), and 3) the anxiety, stress, psychological dysfunctions jointly influenced college students self-efficacy and academic performance (Alemany-Arrebola et al., 2020). The results of the study would help determine the mental health care that might be needed.
1. Methods
Sample. To evaluate the mental health consequences of the COVID-19 pandemic in the States, we administrated this cross-sectional survey study at a public university in Northern Michigan, U.S., from January 17 to February 25, 2022. All students (n=335) taking an introductory core curriculum course focusing on psychology, nursing, or biology were invited to participate in this study. The surveys were completed in the research lab or reserved classroom. Participants provided informed consent to participate in this anonymous survey study. All data were self-reported, and finally, 151 students (female, 76) completed the study, resulting in a response rate of 45.1%. The participants were given extra credit for their involvement. Study procedures were approved by the Institution Review Board (IRB-Protocol, # 120521B). Students' privacy and safety were protected using data collection and storage precautions by providing all with accurate, up-to-date information on safety precautions from trusted sources (i.e., the local CDC), contact information of COVID-19 resources (e.g., the university COVID-19 information web page, state COVID-19 hotline, CDC COVID-19 website), and the contact information for the study investigator.
Demographics. Demographic information included age (recorded as a continuous variable), sex (male, female, other), and ethnicity (e.g., White, American Indian, Black/African American, Asian).
Vaccine. Participants reported whether they were vaccinated and, if so, how many doses of COVID-19 vaccine they had had (i.e., 1 dose or fully vaccinated). People who were fully vaccinated may have received more than two doses. Also, they reported whether they were affected by COVID-19 (i.e., tested positive).
Academic performance. Participants reported how seriously the current pandemic affected their learning/studying, where 0 = not at all to 10= very much. Supplementing this, we also asked the participants to complete the General Self-Efficacy Scale (GSE). This scale assesses a general sense of perceived self-efficacy with the aim in mind to predict coping with daily hassles and adaptation after experiencing all kinds of stressful life events (Schwarzer & Jerusalem, 1995).
Mental health measures The 5-item brief symptom rating scale (BSRS-5) was used to screen psychological disorders. It measures anxiety (feeling tense or high-strung), depression (feeling depressed or in a low mood), hostility (feeling easily annoyed or irritated), interpersonal sensitivity (feeling inferior to others), and additional sleep symptoms (having trouble falling asleep in the past week). The score for each item ranges from 1 to 5 (1, not at all; 2, a little bit, 3, moderately, 4, quite a bit, and 5, extremely). A total score above 15 may indicate a severe mood disorder, scores between 11 and 15 may indicate moderate mood disorders, and those between 7 and 10 could indicate mild mood disorders. According to a previous study, the optimal cutoff point of normal/psychological symptoms was 6/7, so people with BSRS-5 scores lower than 6 are considered normal (Chen et al., 2005; Lu et al., 2011).
Besides, participants were asked to rank, on a sliding scale of 0-10, 1) "How would you rate your fear of COVID-19 before its emergence in the United States, where 0 = not at all fearful to 10= very fearful?"; 2) "How would you currently rate your fear of COVID-19, where 0 = not at all fearful to 10= very fearful?" (for the similar method, see Fitzpatrick et al., 2020); 3) "How would you rate your happiness before its emergence in the United States, where 0 = not at all happy to 10= very happy?"; 4) "How would you currently rate your happiness, where 0 = not at all happy to 10= very happy?".
Supplementing this, participants also did the Perceived Stress Scale (PSS) with 10 items (Cohen, 1988). PSS was adopted as it is a widely used psychological instrument that measures the degree how circumstances in one's life are detected as stressful. In addition, subjects' happiness was assessed using the Subjective Happiness Scale (SHS) with 4 items (Lyubomirsky & Lepper, 1999). The total score ranges between 4 and 28, with lower scores indicating poorer subjective happiness.
Categorical variables were presented by frequency, and chi-square tests were adopted to make the comparison between groups. For psychological symptoms (e.g., fear, stress, anxiety, depression, and happiness), t-tests together with the bootstrap tests were used. Following (Jacob, 1992), effect sizes were reported as partial η2 (small = 0.01; medium = 0.06; large = 0.14) for ANOVAs, and as Cohen's d (small = 0.30; medium = 0.50; large = 0.80) for planned comparison t-tests. For the correlation analysis, besides the Pearson correlation analysis, as elsewhere (Hu et al., 2013, 2018), we ran an across-subject robust regression analysis to confirm the effects, given that standard Pearson correlation is very sensitive to even a few influential data points (Wilcox, 2005).
2. Results
The intent of this work was to examine the intersection of COVID-19 fear and mental health consequences among college students in Northern Michigan, the region of the U.S. severely affected by the outbreak of COVID-19. This study was conducted from January 17 to February 25, 2022, and 151 participants were involved (76 females; mean age =21.5, Standard Division/std =3.13). Most participants were white (115, 76%), with a few American Indian inhabitants (33, 22%). Besides, 2 (1%) were African American, and 1 (1%) was Asian.
2.1. Vaccination and COVID-19 tests
We first looked at the vaccination data (Table 1 ). Among n=151 participants, the vaccination rate was 95.4% (1 dose) and 46.4% (fully vaccinated). It should be noted that 4.6% (n=7) of participants were unvaccinated. According to the vaccine tracker (Mayoclinic, 2022), on January 31, 2022, the vaccination rate was 76.3% (1 dose) and 64.8% (fully vaccinated) for the whole country, while the vaccination rate 65.2% and 58.2% for Michigan State. Our data thus show that for college students, the vaccination rate was higher than the mean level in the state (95.4% vs. 65.2%); however, the full vaccination rate of college students was lower than the mean level (46.4% vs. 58.2%). No statistically gender difference appeared in the vaccination rates, X2(2, n=151) =2.24, p=.301, ɸ=.13. These data perhaps reflected a special vaccine hesitancy in the COVID-19 vaccine era in Michigan.
Table 1.
Vaccination and COVID-19 tests for male and female college students.
| Vaccination | Test Negative % | Test Positive % | |
|---|---|---|---|
| Male | Non vaccinated | 2.67 | 4.00 |
| Vaccinated - 1 dose | 14.67 | 28.00 | |
| Full vaccinated | 32.00 | 20.00 | |
| Female | Non vaccinated | 0.00 | 3.95 |
| Vaccinated - 1 dose | 11.84 | 43.42 | |
| Full vaccinated | 18.42 | 22.37 | |
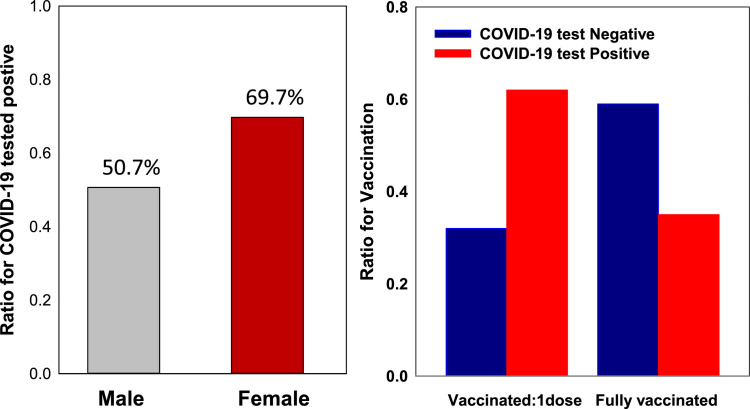
We then considered the COVID-19 test results (positive vs. negative). The mean positive test rate was 60.3%. Although there was no gender difference in vaccination rate, there was a statistically significant difference between males and females on COVID-19 test results; 50.7% of male participants were tested positive, while 69.7% of female participants were tested positive, X2(1, n=151) =5.73, p=.017, ɸ=.20(Fig. 1 , Left). Further tests showed that compared to those who only received one dose vaccination shot, people who were fully vaccinated were less likely to be affected by the COVID-19 (i.e., tested positive) (Fig. 1, Right). For those who only received one dose vaccine shot, 54% tested positive, while for those who were fully vaccinated, the positive test rate was 35%. The difference was statistically significant, X2(1, n=144) =11.11, p=.001, ɸ=-.28. These data suggested that full vaccination is critical in the pandemic.
Fig. 1.
Left panel, Gender difference on COVID-19 tested positive; Right panel, the influence of vaccination on COVID-19 infection: People who were fully vaccinated were less likely infected (for interpretation of the references to color in the figure legend, the reader is referred to the web version of this article).
2.2. Influence of COVID-19 on Mental health
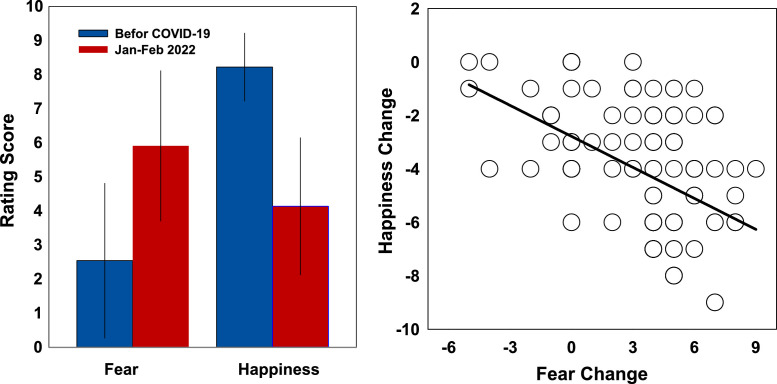
First, at the moment of testing, January-February 2022, participants reported to have a higher fear level (5.91; std = 2.20) than before the outbreak of the COVID-19 (2.54; std = 2.27, retrospectively reported). So the pandemic had largely increased fear in college students, t(150)=14.79, p<.0001, Cohen's d=1.20. Yet, the fear level of 5.91 was lower than what was reported before. In a study conducted in March 2020 with the same method, researchers reported that people were fearful, with an average score of nearly 7 (Fitzpatrick et al., 2020). Second, before the outbreak of the COVID-19 (retrospectively reported), participants' happiness level was 8.23 (std= .99), and then in January -February 2022, it was 4.14 (std = 2.01), suggesting that the pandemic decreased students' happiness, t(150)=21.25, p<.0001, Cohen's d=1.73,. No gender difference was detected in either fear, happiness, or changes in these indexes (largest t=1.59, p=.115, Cohen's d=.26). The size of fear change was negatively associated with the happiness change, r=.459, p<.0001. (Fig. 2 ).
Fig. 2.
Left panel, Fear and Happiness change: Before the outbreak of the COVID-19 (retrospectively reported) and now (January-February, 2022); Right panel, scatter plot of the fear and happiness changes.
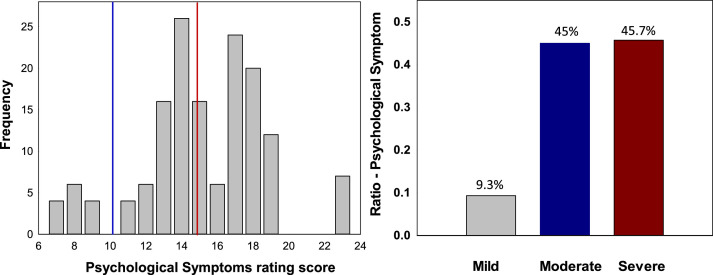
We also surveyed mental health using existing surveys. We assessed participants' psychological symptoms with the 5-item brief symptom rating scale (BSRS-5). These five items consist of anxiety, depression, hostility, interpersonal sensitivity, and sleep problem. The mean score was 15.19 (std, 3.48), indicating a severe mood disorder. We were noted there was a large individual difference in the mood symptom assessment, 9.3 % experienced mild mood disorders (BSRS score was between 7 and 10), 45 % experienced moderate mood disorders (BSRS score was between 11 and 15), and 45.7% experienced severe mood disorders (BSRS was larger than 15). Note, there was no gender difference on the BSRS score, t(149) =.883, p=.379, Cohen's d=.14 (Fig. 3 ).
Fig. 3.
Left panel, bar plot for BSRS score frequency; Right panel, a summary for the BSRS assessments. There was a large individual difference in the mood symptom assessment; 9.3% experienced mild mood disorders (BSRS score was between 7 and 10), 45 % experienced moderate mood disorders(BSRS score was between 11 and 15), and 45.7% experienced severe mood disorders(BSRS was larger than 15).
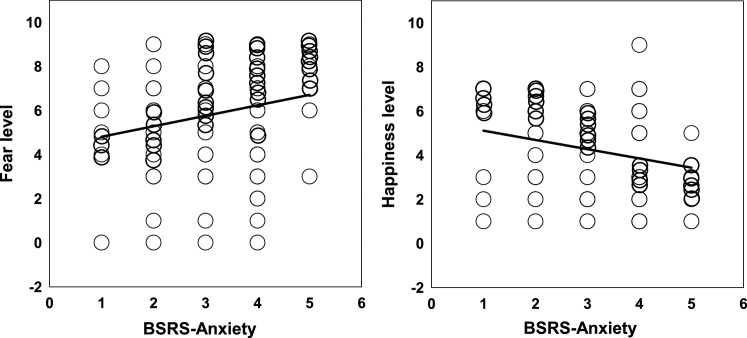
Consistently, the anxiety tested in the BSRS-5 correlated positively with self-reported fear (r=.203, p=.012) and negatively with happiness (r=-.097, p=.016) (Fig. 4 ).
Fig. 4.
Left panel, scatter plot for the correlation between BSRS-Anxiety and Fear; Right panel, scatter plot for the correlation between BSRS-Anxiety and Happiness.
In line with those assessments, stress measurement (Perceived Stress Scale, PSS) correlated positively with fear change, r=.160, p=.049; and correlated negatively with happiness (Subjective Happiness Scale, SHS), r=-.177, p=.030.
We further compared the scores on the mood state between the fully vaccinated and those having only one dose vaccination shot. As very few (n=7) participants were unvaccinated, these unvaccination data were not considered. The analyses showed that 1) although retrospectively, participants with only a single dose vaccination shot were less fearful than those fully vaccinated before the outbreak of the COVID-19, F(1,142) =4.16, P=.043, ηp 2 = .03, and their fear change in January-February 2022 was more prominent than those fully vaccinated, F(1, 142) =5.06, P=.026, ηp 2 = .03; 2) again, although retrospectively, participants with only a single dose vaccination shot were equally happy as those fully vaccinated before the outbreak of the COVID-19, F(1,142) =.317, P=.574, ηp 2 = .002, but they well less happy than those fully vaccinated, F(1, 142) =5.88, p=.017, ηp 2 = .04. No other significant effects were detected.
2.3. Influence of COVID-19 on students’ learning
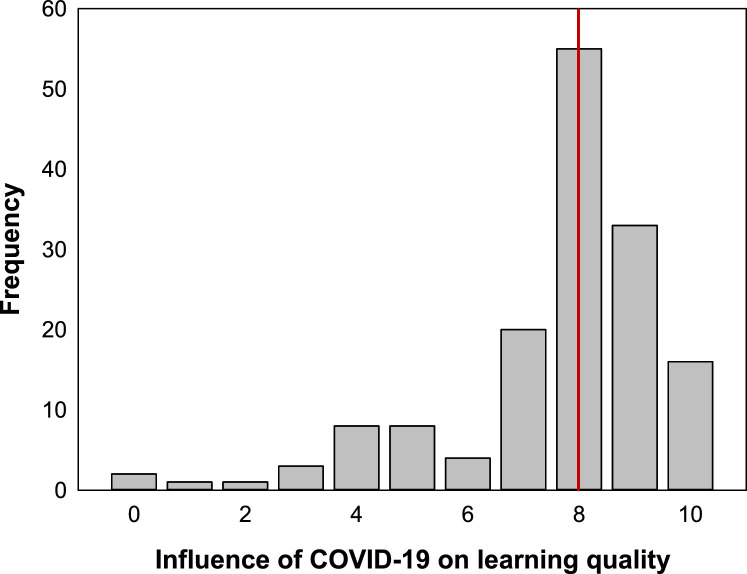
Our data showed that respondents were largely affected by the COVID-19 pandemic, averaging a score of nearly 7.58 (std, 1.99) on a scale of 10 when asked how their learning quality was influenced by the COVID-19, t(150)=15.94, p<.0001, Cohen's d=3.81 (Fig. 5 ).
Fig. 5.
Frequency plot: COVID-19 impaired students’ learning quality. Red line stands for the mean of 7.6, suggesting that students’ learning was largely influenced by the pandemic.
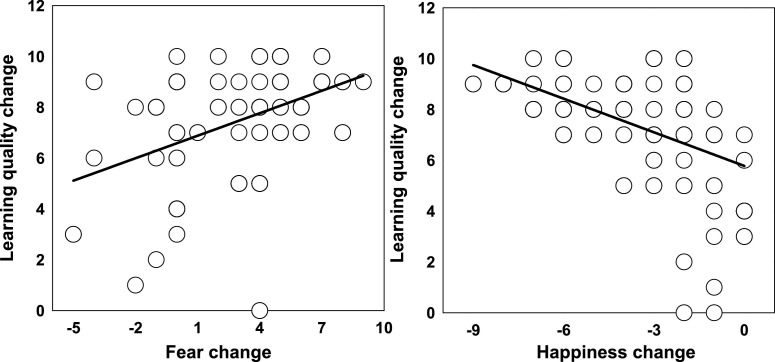
This effect was general between males and females, t(149)=.302, p=.763, Cohen's d=.05. Further analysis showed that fear change (enhanced fear) predicated learning difficulties, r=.415, p<.0001. But happiness change negatively correlated with learning difficulties, r=-.523, p<.0001 (Fig. 6 ). Consistently, stress measurement (Perceived Stress Scale, PSS) positively correlated with learning change, r=.162, p=.046.
Fig. 6.
Left panel, the learning change was positively correlated with the fear change; Right panel, the learning change was negatively correlated with the happiness change.
Self-efficacy is about people's belief and a sense of confidence in whether individuals can use their capacity to deal with various situations (Bandura, 1977; Bandura et al., 1999). How did the pandemic impact college students' self-efficacy? We found no relationship between participants' perceived self-efficacy and their learning difficulties, r=-.037, p=.648. Self-efficacy did not correlate with any emotional components, including fear, anxiety, and happiness. Also, no significant gender effect appeared with self-efficacy, t(149)=.104, p=.917, Cohen's d=.02. A multiple regression was carried out to investigate whether fear change, happiness change, and self-efficacy could predict participants’ learning. The model predicted participants’ learning difficulty well, F(3,147) = 22.465, p<.001. Consistent with what was reported above, both fear and happiness change contributed significantly to the model (Fear change, B=.157, p=.005; Happiness change, B=-.356, p<.0001), yet self-efficacy did not, B=-.016, p=.563. For detailed information on the influence of COVID-19 on learning quality and self-efficacy, see Table 2 .
Table 2.
The influence of COVID-19 on Self-efficacy and Learning quality.
| COVID-TEST | Self-Efficacy Index | Learning-difficulty Index | |
|---|---|---|---|
| Male | Negative: 37 | 3.17(.44) | 7.7(2.00) |
| Positive: 38 | 3.16(.48) | 7.37(2.12) | |
| Female | Negative: 23 | 3.2(.41) | 7.35(2.39) |
| Positive: 53 | 3.17(.56) | 7.75(1.72) | |
3. Discussion
COVID-19 outbreaks disrupted basic life activities and elicited acute and potentially long-term effects on individuals' well-being and health, including psychological distress, anxiety, and depression (Clabaugh et al., 2021; Khubchandani et al., 2022; Pfefferbaum & North, 2020; Son et al., 2020). On January 20, 2020, CDC confirmed the first case of COVID-19 in the U.S (Johns Hopkins University, 2022), and vaccinations in the United States began on December 14, 2020. As of April 4, 2022, over two years have passed since the outbreak of COVID-19. But the devastating recurrence of COVID-19 is difficult to accept, and people resist adopting it. This survey study was conducted from January 17 to February 25, 2022. We aimed to discover how the ongoing pandemic affected college students two years later since its outbreak in the U.S. Specifically, we explored how the consequences of the pandemic (e.g., changes in fear, stress, happiness, and self-efficacy) jointly influenced their academic performance. In the following, we discuss our findings at greater length.
Vaccines are critical for curtailing the COVID-19 pandemic and an important tool for return to "normalcy" on college campuses. According to a recent review (Khubchandani et al., 2022), in American colleges, the COVID-19 vaccination refusal rates were 29.8%, 51.5%, 24.3%, 8.4% (four studies; mean=28.5%)in 2019-2020, while 17.1%, 43.3%, 36.3%, and 47.5% (four studies; mean=36.1%) in 2020-2021. These earlier studies did not tell us the vaccination rates for 2nd does and full vaccination rates. Our data were collected in January and February 2022, and the vaccination coverage (first dose) was above 95%. This is encouraging but not surprising, as, in Michigan, vaccination was required for college students. Many students were instructed to be vaccinated to protect others from infection or to decrease their chances of experiencing severe illness, end their social isolation and attend in-person classes. However, the vaccination coverage for two or more doses (fully vaccinated) was only 65.2%. These findings are important and timely. Although vaccines have become more widely available, there were still over 35% of college students who refused to be fully vaccinated. This vaccination hesitancy effect was equally among male and female students.
Among n=151 participants, the COVID-19 test positive rate was 60.3%. Several factors may explain this. For instance, the vaccine coverage, especially the full vaccination rate, was not high enough (e.g., 80-90%) to reach population immunity through vaccination (Aschwanden, 2021; Liu et al., 2021), and college students were gathering indoors and socialized without physical distancing. Compared to male students (50.7%), more female students (69.7%) tested positive, suggesting that female students were more vulnerable to the infection. These results differed from the findings that the prevalence of symptomatic COVID-19 was higher in men than women, reported earlier in 2020 (Abate et al., 2020). Therefore it seems that for a long time, the prevalence of symptomatic COVID-19 was higher in females than males. We are now doing vaccine disgust and perception research to understand the gender difference (Clifford & Wendell, 2016; Rohrmann et al., 2008). It is suggested that the mRNA vaccines are a two-dose series: the first dose helps our body create an immune response, while the second dose strengthens our immunity to the virus (Johns Hopkins University, 2022). The effects of vaccination decreased over time. Consistently with this, in the present study, among those who tested positive for COVID-19, only 35% were fully vaccinated, while among those who tested negative for COVID-19, the full vaccination rate was 62%. Vaccination is associated with a significant reduction in transmission of the COVID-19; for its effect on recent Alpha and Delta Variants, see (Eyre et al., 2022). Our results highlighted the need for additional education (i.e., full vaccination) and vaccine outreach among college students (Kecojevic et al., 2021). This also had a general implication for the society that complete vaccination decreased the COVID-19 transmission, and social media should be harnessed to promote full vaccination (Khubchandani et al., 2022).
Since two years have passed since the outbreak of the COVID-19 in the States, we expected that the influence of the pandemic would be less severe than before, and people's fear would decrease. Earlier in March 2020, researchers reported that people in the States were highly stressed, averaging a score of nearly 7 on a scale of 10 when asked how fearful they were of COVID-19 - "how would you currently rate your fear of COVID-19 where 0=not at all fearful to 10=very fearful" (Fitzpatrick et al., 2020). These researchers did not survey participants' fear levels before the pandemic outbreak. Almost at the same time, another group reported that during the pandemic, psychological stress did not change over time (Laurene et al., 2022), yet the time span observed was about one month, so short, and all were after the outbreak of the pandemic. In the present study, we showed that retrospectively before the emergence of the COVID-19, participants' fear level was nearly 3, and two years later, the fear level was roughly 6 with the same question as used by Fitzpatrick et al. (2020), suggesting that two years later, people's fear level decreased, but never recovered to the level before the outbreak of the pandemic. Although vaccinations could reduce participants' anxiety and stress in COVID-19 vaccine era (Nguyen, 2021), the series of COVID-19 waves were difficult to accept and get used to.
One important indicator of good mental health is subjective happiness, and the fear of COVID-19 has the potential to affect people's happiness. People's happiness level reflects the balance of positive and negative feelings and satisfaction in one's life. In the present study, at the moment of testing, January-February 2022, participants reported to have a lower happiness level (size, 4) than before the outbreak of the COVID-19 (size 8), suggesting that the two components, fear, and happiness, were closely linked with each other. Together two years later, students' fear levels doubled, and consistently, their happiness decreased to one-half of the previous level. As expected, the size of fear change was negatively associated with the size of happiness change, suggesting that our assessments were highly reliable.
Further, we surveyed participants' psychological symptoms of anxiety, depression, hostility, interpersonal sensitivity, and sleep symptoms with the 5-item brief symptom rating scale. Alarmingly, among n=151 students, 95.7% experienced moderate to severe mood disorders, including anxiety, depression, hostility, interpersonal sensitivity, and sleep problems. Although more females were tested COVID-19 positive, however, there was no gender difference in the mood disorders, suggesting that college students had mood symptoms in general (Chen et al., 2005; Lu et al., 2011). These findings followed the fear and happiness measures. For instance, the anxiety tested in the BSRS-5 positively correlated with self-reported fear and negatively correlated with happiness reported above. These results have alarming implications for individuals and the whole society regarding mental health, emotional and social functioning.
How this severe biopsychosocial stress, a mental health pandemic, affected college students' academic performance two years later was unexplored so far. It can be anticipated that the crisis influenced and is still influencing college students, especially those with learning disabilities. One study showed that females experienced more psychological stress than males, but this study was conducted in March 2020 (Laurene et al., 2022). Our data showed that respondents were largely affected by the pandemic, averaging a score of nearly 8 on a scale of 10 when asked how their learning quality was influenced by the COVID-19, and male and female students were equally affected. Learning quality change reflected the academic difficulties, for instance, the ability to focus on academic work. Due to the repeated outbreaks of the COVID-19, students were worried about their own health, the health of their families, or even struggled financially, and these made them less focused on academic performance. Online or remoted learning may further exacerbate mental health distress among college students. Exactly, students' learning quality changes were positively correlated with their fear change and perceived stress and negatively correlated with their happiness change.
Finally, we used a reliable self-efficacy scale to test students' perceived self-efficacy (Schwarzer, 1997; Schwarzer & Jerusalem, 1995), and asked whether there was a correlation between self-efficacy and learning performance. However, we did not find a statistically significant correlation between self-efficacy with factors, including their learning quality change. Self-efficacy refers to an individual's overall self-confidence in dealing with challenges of various environmental situations (Bandura, 1977; Bandura et al., 1999). We suggested that the series of COVID-19 waves impaired students' self-efficacy and self-confidence in general; hence this index was not sensitive anymore. This is alarming, and further research is necessary. Clinical research has, until recently, focused mainly on risk factors and vulnerability in understanding the vial features, epidemiologic characteristics, clinical spectrum, and treatment. COVID-19 and the stress, anxiety, and depression may spread to the nervous system. Definitely, more attention is needed to be placed on college students' self-perception, confidence, and beliefs.
During this epidemic, mental health problems such as fear, anxiety, and depression were common among the general public, especially children and older adults (Brooks et al., 2020; Pfefferbaum & North, 2020). Several studies explored the psychological impact of the pandemic on college students, and most of these studies were conducted earlier in 2020 (Cao et al., 2020; Clabaugh et al., 2021; Khubchandani et al., 2022; Son et al., 2020; Wang et al., 2020). Yet, this is the first study on how the COVID-19 influenced college students' learning quality in the States, two years later since the outbreak of the pandemic. The uniqueness of this study was that we surveyed participants' mental health before the outbreak of COVID-19 and after the vaccine era (i.e., January and February 2022), and how they together affected their learning. Our findings have important clinical and educational implications. First, there were about 35% of students not fully vaccinated, and full vaccination is associated with a significant reduction in transmission of the COVID-19. These findings have important clinical implications, as the effects of vaccination decrease over time. Second, we found a statistically significant gender difference that more female than male students tested positive for the COVID-19, while male and female students experienced similar stresses and negative emotions because of the COVID-19 pandemic. Third, two years later, roughly 50% of college students were experiencing severe mood disorders and hence urgently needed attention and support from society, families, and colleges. This does not necessarily mean that most students were mentally ill but does indicate more individuals had mental health issues even if their symptoms were not debilitating. Fourth, college students were experiencing learning difficulties, and definitely, its impact would be far-reaching. Therefore, not only college students’ mental health but also their learning should be monitored during epidemics. The psychological and psychiatric consequences for individuals are perhaps even longer than people would anticipate. Definitely, the expansion of campus services, counseling services and promoting social connectedness are critical in helping students navigate the life challenges associated with the pandemic (Salimi et al., 2021; Wang, Hegde, et al., 2020). Past is the future. This study provided a snapshot of how the COVID-19 was reacted to by the general college student population two years later and would help to inform potential mental health risks.
There are several limitations to this study. It is straightforward that the current study is a cross-sectional survey, and we were not able to establish causality. Our sample size was largely dependent on how many participants were collected in a fixed amount of time (from January 17 to February 25, 2022). Given the limited resources available, the response rate was somewhat low (roughly 45%), and we lacked data on non-responders. Also, a large sample size is always desirable, and precisely, we are continuing this effort. Further, while the sample was selected in a random fashion, and demographic characteristics reflected the student population at a northern Michigan university the data were subject to social desirability bias.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
This study was supported by the LSSU Foundation's Enrichment Grant to K. Hu. It was also supported by the Open Research Fund of the CAS Key Laboratory of Behavioral Science, Institute of Psychology, Key project of Beijing Education Science Planning (BEAA21046), and National Natural Science Foundation of China (Grants 31571161) to Q. Li.
References
- Abate B.B., Kassie A.M., Kassaw M.W., Aragie T.G., Masresha S.A. Sex difference in coronavirus disease (COVID-19): a systematic review and meta-analysis. BMJ Open. 2020;10(10) doi: 10.1136/bmjopen-2020-040129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alemany-Arrebola I., Rojas-Ruiz G., Granda-Vera J., Mingorance-Estrada Á.C. Influence of COVID-19 on the perception of academic self-efficacy, state anxiety, and trait anxiety in college students. Frontiers in PsychologyFront. Psychol. 2020:2640. doi: 10.3389/fpsyg.2020.570017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature. 2021:520–522. doi: 10.1038/d41586-021-00728-2. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A., Freeman W.H., Lightsey R. Springer; 1999. Self-efficacy: The exercise of control. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet North Am. Ed. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H.-C., Wu C.-H., Lee Y.-J., Liao S.-C., Lee M.-B. Validity of the five-item Brief Symptom Rating Scale among subjects admitted for general health screening. J. Formos. Med. Assoc. 2005;104(11):824–829. [PubMed] [Google Scholar]
- Clabaugh A., Duque J.F., Fields L.J. Academic stress and emotional well-being in united states college students following onset of the COVID-19 pandemic. Frontiers in PsychologyFront. Psychol. 2021:12. doi: 10.3389/fpsyg.2021.628787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford S., Wendell D.G. How disgust influences health purity attitudes. Polit. Behav. 2016;38(1):155–178. [Google Scholar]
- Cohen S. In: The social psychology of health. Spacapan S., Oskamp S., editors. Sage Publications, Inc; 1988. Perceived stress in a probability sample of the United States; pp. 31–67. [Google Scholar]
- Cullen W., Gulati G., Kelly B.D. Mental health in the COVID-19 pandemic. QJM: An International Journal of Medicine. 2020;113(5):311–312. doi: 10.1093/qjmed/hcaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyre D.W., Taylor D., Purver M., Chapman D., Fowler T., Pouwels K.B., Walker A.S., Peto T.E.A. Effect of Covid-19 vaccination on transmission of alpha and delta variants. N. Engl. J. Med. 2022;386:744–756. doi: 10.1056/NEJMoa2116597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice, and PolicyPsycholog. Trauma. 2020;12(S1):S17. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Hu K., De Rosa E., Anderson A. Differential temporal salience of earning and saving. Nat. Commun. 2018;9:2843. doi: 10.1038/s41467-018-05201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Padmala, S., Pessoa L. Interactions between reward and threat during visual processing. Neuropsychologia. 2013;51(9):1763–1772. doi: 10.1016/j.neuropsychologia.2013.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob C. A power primer. Psychol. Bull. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins University. (2022, April 4). COVID-19 Report. https://coronavirus.jhu.edu/map.html.
- Kecojevic A., Basch C.H., Sullivan M., Chen Y.-T., Davi N.K. COVID-19 vaccination and intention to vaccinate among a sample of college students in New Jersey. J. Community Health. 2021;46(6):1059–1068. doi: 10.1007/s10900-021-00992-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A., Basch C.H., Sullivan M., Davi N.K. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khubchandani J., Biswas N., Mustapha T., Talbert S., Dharamsi S. COVID-19 vaccination refusal among college students: global trends and action priorities. Brain Behav. Immun. 2022;99:218–222. doi: 10.1016/j.bbi.2021.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurene K.R., Kodukula G., Lechner W.V, Grega C., Lumpkin E., Kenne D.R. Assessment of psychological distress as a function of positive psychological variables during the COVID-19 pandemic: A university longitudinal study. J. Am. Coll. Health. 2022:1–7. doi: 10.1080/07448481.2022.2032086. [DOI] [PubMed] [Google Scholar]
- Li H.Y., Cao H., Leung D.Y.P., Mak Y.W. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int. J. Environ. Res. Public Health. 2020;17(11):3933. doi: 10.3390/ijerph17113933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Zhang J., Cai J., Deng X., Peng C., Chen X., Yang J., Wu Q., Chen Z., Zheng W. Herd immunity induced by COVID-19 vaccination programs to suppress epidemics caused by SARS-CoV-2 wild type and variants in China. MedRxiv. 2021 [Google Scholar]
- Lu I.-C., Yen Jean M.-C., Lei S.-M., Cheng H.-H., Wang J.-D. BSRS-5 (5-item Brief Symptom Rating Scale) scores affect every aspect of quality of life measured by WHOQOL-BREF in healthy workers. Qual. Life Res. 2011;20(9):1469–1475. doi: 10.1007/s11136-011-9889-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyubomirsky S., Lepper H.S. A measure of subjective happiness: preliminary reliability and construct validation. Soc. Indic. Res. 1999;46(2):137–155. [Google Scholar]
- Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- Mayoclinic. (2022, April 10). Vaccine tracker. https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker.
- Michigan CDC. (2022, April 10). Michigan COVID-19 report. https://www.michigan.gov/coronavirus.
- Nguyen M. Advances in Public HealthAdva. Public Health. 2021. The psychological benefits of COVID-19 vaccination; p. 2021. [Google Scholar]
- Perez-Arce F., Angrisani M., Bennett D., Darling J., Kapteyn A., Thomas K. COVID-19 vaccines and mental distress. PLoS One. 2021;16(9) doi: 10.1371/journal.pone.0256406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Dominguez C., Carrascal-Caputto B., Duran M. Psychological Trauma: Theory, Research, Practice, and PolicyPsycholog. Trauma. 2021. Anxiety and intimate relationships in times of lockdown due to COVID-19. [DOI] [PubMed] [Google Scholar]
- Rohrmann S., Hopp H., Quirin M. Gender differences in psychophysiological responses to disgust. Journal of PsychophysiologyJ. Psychophysiol. 2008;22(2):65–75. [Google Scholar]
- Salimi N., Gere B., Talley W., Irioogbe B. College students mental health challenges: Concerns and considerations in the COVID-19 pandemic. Journal of College Student PsychotherapyJ. Coll. Stud. Psychother. 2021:1–13. [Google Scholar]
- Schwarzer R. Optimistic self-beliefs: Assessment of general perceived self-efficacy in thirteen cultures. World PsychologyPsychol. 1997;3(1):177–190. [Google Scholar]
- Schwarzer R., Jerusalem M. Generalized self-efficacy scale. J. Weinman, S. Wright, & M. Johnston, Measures in Health Psychology: A User's Portfolio. Causal and Control BeliefsCausal Control Belief. 1995;35:37. [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet ResearchJ. Med. Internet Res. 2020;22(9):e21279. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Valtorta N.K., Kanaan M., Gilbody S., Ronzi S., Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet North Am. Ed. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PR., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Hegde S., Son C., Keller B., Smith A., Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. Journal of Medical Internet ResearchJ. Med. Internet Res. 2020;22(9):e22817. doi: 10.2196/22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox R.R. 2nd ed. Academic Press; San Diego, CA: 2005. Introduction to robust estimation and hypothesis testing. [Google Scholar]