Abstract
Objectives
The non-pharmacological measures to contain the COVID-19 pandemic may lead to considerable psychological distress. The aim of the CoCo-Fakt study was to investigate possible coping strategies and their effects on psychological distress during legally enforced quarantine of infected persons (IPs) and their close contacts (CPs).
Study design
This was a cross-sectional cohort study.
Methods
From 12 December 2020 to 6 January 2021, all IPs and their CPs (n = 8232) registered by the public health department (Cologne, Germany) were surveyed online. Psychosocial distress and coping were measured using sum scores; free-text answers related to specific strategies were subsequently categorised.
Results
Psychosocial distress was higher in IPs than in CPs (P < .001). Although the mean coping score did not differ between both groups, it was influenced by the reason for quarantine (IP vs CP) besides gender, age, socio-economic status, living situation, psychological distress, resilience, physical activity and eating behaviour. This final regression model explained 25.9% of the variance. Most participants used active coping strategies, such as contact with the social environment, a positive attitude and hobbies.
Conclusions
Although psychological distress was higher in IPs than in CPs during the quarantine period, the mean coping score did not differ. The strategies most frequently used by IPs and CPs were activating social networks, a healthy lifestyle and professional support systems, such as the health department helpline. Appropriate advice should be implemented to prevent long-term psychological consequences when supporting affected people.
Keywords: Health department, Coping skills, COVID-19, Psychological distress, Legally enforced quarantine
Introduction
The COVID-19 pandemic, which first appeared in Wuhan, China, in December 2019, spread rapidly globally.1 , 2 In the absence of possible therapeutic countermeasures and the vaccinations that only became available in Germany at the end of 2020, various contact restrictions and curfews were imposed to protect high-risk groups and to prevent an overload of the health system. Because of these restrictions, the pandemic has had an enormous impact on the daily lives and mental health of the general population. Several studies described an increase in loneliness, symptoms of anxiety and depression.[3], [4], [5], [6] The ‘new’ term ‘social distancing’ with its negative connotation could intensify this burden through the feeling of being left alone, ignored and excluded or induce a feeling of being a burden for society and one's private surroundings.7
Previous studies implicate that quarantined people due to a SARS-CoV-2 infection or as close contacts might have particularly serious mental health consequences.8 Benke et al. examined the effects of different forms and levels of restriction resulting from public health measures (e.g. quarantine and stay-at-home order) on anxiety and depression symptomatology, health anxiety, loneliness, the occurrence of fearful spells, psychosocial distress and life satisfaction.9 Higher restrictions due to lockdown measures, a greater reduction of social contacts and greater perceived changes in life were associated with higher mental health impairments. Noteworthy, an officially announced stay-at-home order was not associated with poorer mental health; but in their study, only 28.4% (n = 1187) were mandatory quarantined.9 Other studies by Kołodziejczyk et al. and by the TMGH-Global COVID-19 Collaborative, in turn, were able to show significantly poorer mental health in people who were quarantined as an infected person (IP) or a close contact (CP).10 , 11 Psychopathological symptoms such as anxiety, insomnia and hyperarousal were much more frequent in this group.10 The extent to which psychological well-being, and thus long-term psychological outcome, is affected by a stressor may depend on the use of positive or negative coping strategies.12 However, even the designation or conceptualisation of coping is challenging.13 The most commonly used definition by Lazarus and Folkmann describes coping as a cognitive or behavioural reaction to manage a situation.14 Mostly coping is categorised in two main dimensions: problem-oriented coping and emotion-oriented coping.15 The starting points are the relationship to the surroundings and the interpretation of these, respectively. This can be supplemented by the perspective of distraction, which can be social as well as task oriented.16 Skinner et al., on the other hand, call for a revision of the previous classification towards a multidimensional and hierarchical system.13 However, given the complexity and lack of comparability to other studies, this model is not applied in our study.
Park et al. analysed the use and impact of different coping mechanisms during the onset of the COVID-19 pandemic in April 2020 in the United States. The most frequently cited strategies were distracting oneself, seeking emotional-social support and active problem-focused coping.17 Saalwirth et al. also examined the effects of coping strategies in spring 2020 in Germany via online questionnaire. The results show that meaning- and problem-focused coping were used most frequently. These types of coping were positively associated with positive affect. In contrast, social and avoidance coping showed a positive relationship to negative affect.18 Budimir et al. identified positive thinking as the strongest positive predictor for all measured mental health scales, including quality of life or depression.19 In a study by Golemis et al. from Greece, sharing thoughts and feelings with others about COVID-19 was reported as the most frequently used mechanism.20 Along with sports and humour, this predicted lower levels of loneliness.20 However, in these studies on coping, the term quarantine was used to refer to general isolation measures of the general population. So far, however, no studies have analysed the use of coping strategies in the context of a mandatory stay-at-home order and the relationship with psychosocial distress considering IPs and CPs in Germany. Therefore, the aim of the CoCo-Fakt study (Cologne–Corona Counselling and Support For Index and KontAKt Persons During the Quarantine Period) was to examine (1) the overall coping score and (2) type and frequency of coping strategies of officially quarantined IPs and CPs. (3) Additional factors influencing coping such as sociodemographic variables, psychological distress and/or resilience were also identified to develop recommendations for action during the quarantine period counteracting possible long-term psychological consequences.
Methods
Study design/study population
Since the occurrence of the first COVID-19 infection in Cologne at the end of February 2020, all people who tested positive for SARS-CoV-2 (IPs) in the urban area of Cologne were reported to the Cologne Health Department and quarantined based on the legal regulations for the control of infectious diseases defined by the Infection Protection Act. For this purpose, these people are contacted, registered in the database of the Cologne public health department's digital contact management (DiKoMa) system21 and questioned in a standardised manner about possible infection routes, chronic diseases and risk factors. In addition, close contacts (CPs) are also quarantined to interrupt infection chains. CPs are defined as those who have had close exposure to a confirmed COVID-19 case (<1.5 m) for a duration longer than 10 min without a mask within a time frame ranging from 2 days before symptom onset in the index case to 10 days after symptom onset. The quarantine duration was usually 10–14 days from the time of symptom onset or positive test in IPs and from the last contact in CPs.
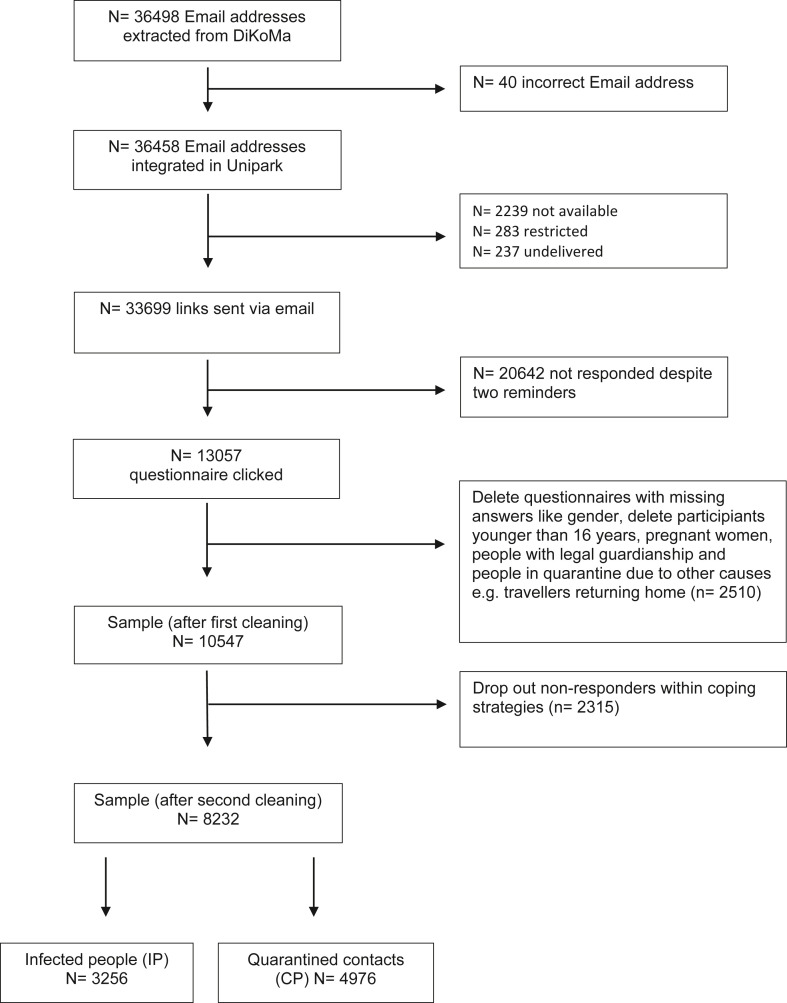
All individuals enrolled before and on 9 December 2020 were extracted from this data set; individuals aged <16 years, those with no informed consent, non-compliance, deceased patients and those who were placed in medical or nursing facilities were excluded. Pregnant women received a modified online questionnaire.22 From 12 December 2020 to 6 January 2021, the link to the online survey was emailed to 33,699 people. This link was clicked on by 13,057 people. After cleaning the data, only people who provided information on coping strategies were integrated into this evaluation (n = 8232; see Fig. 1 : Study population).
Fig. 1.
Study population.
Questionnaire
The online questionnaire was programmed with Unipark. It included both quantitative and qualitative parameters and was based on the COVID-19 snapshot study conducted by Betsch et al. and the World Health Organisation.23 Participants were explicitly informed of the period to which each question referred, for example, general data, such as education, exercise behaviour before the pandemic, psychological disstress or coping strategies during the legally mandated quarantine.
Demographic data
Information was collected on age (years) and gender (male/female). Educational status was calculated according to years of schooling completed (<10 years corresponds to low socio-economic status [SES], 10 years to medium SES and >10 years to high SES).24 , 25 Conclusions about migration background were based on the primary language spoken at home (No = speak German at home and Yes = speak a language other than German).
Personal situation
Information was collected regarding the presence of chronic diseases,25 the housing situation (house/flat with garden and/or balcony vs no balcony/no garden), the composition of the household (partner and children) and the symptom burden (only for infected people). The quarantine duration was measured in days.
Psychological distress
Five items from the COVID-19 Snapshot Monitoring study (COSMO) were integrated:26
-
-
‘I felt nervous, anxious or tense’27 (Item 1, Generalised Anxiety Disorder Scale-7 [GAD-7])
-
-
‘I felt down/depressed’28 , 29 (Item 6, Generalised Depression Scale [ADS])
- -
- -
-
-
‘Thoughts of my experience in the Corona pandemic triggered physical reactions in me, such as sweating, shortness of breath, dizziness or palpitations’30 (Item 19, IES-R).
Responses were given on a 6-point Likert scale from ‘not at all/less than 1 day’ to ‘always/daily’ and regrouped into ‘not at all’, ‘1–2 days’, ‘3–4 days’ and ‘5–7 days’ during time of quarantine. Some items were recoded in reverse terms so that all items could then be combined into a total relative sum score related to the number of questions to estimate the overall reported psychological distress in accordance with the COSMO study. A high score represents a high level of psychological distress. The present study found a Cronbach's alpha coefficient of 0.694 for the psychological distress score and reliabilities of the individual questions ranging from 0.532 to 0.781. A value higher than 0.70 would be ideal, a value of internal consistency close to 0.60 is satisfactory in terms of a screening tool with five questions.31 The complete instructions of the GAD, ADS and IES-R can be found in the respective manuals.27 , 28 , 30
Resilience
Resilience was measured via six items with the Brief Resilience Scale (BRS; e.g. ‘I do not need much time to recover from a stressful event’), ranging from ‘I strongly disagree’ (1) to ‘I strongly agree’ (6).32 , 33 In addition, some items that asked about the current quarantine situation were used (e.g. ‘I know I will not be discouraged’).34 After recoding, a relative sum score after Smith et al. related to the number of questions was formed in accordance with the COSMO study,32 with a high score representing high resilience. The present study found a Cronbach's alpha coefficient of 0.812 for the BRS.
Coping strategies
The application of coping strategies and the use of support systems were investigated with the help of six items, following the COSMO study:
-
-
‘I have received offers of support from family, friends or neighbours.’26 (Item 2, Federal Centre for Health Education [BZgA] – coping)
-
-
‘I had a plan for my daily life in terms of sleep, work or physical activities.’26 (Item 4, BzgA – coping)
-
-
‘I discovered activities for myself that made staying at home easier.’26 (Item 6, BzgA – coping)
-
-
‘I have used digital media to communicate with family, friends and acquaintances.’26 (Item 1, BzgA – coping, modified)
-
-
‘I was bored.’26 (Item 7, BzgA – coping)
-
-
‘I couldn't do anything myself to influence the situation positively.’26 (Item 2, solidarity)
Here, too, a 6-point Likert scale was used to collect responses, and a sum score was formed after recoding. A high score equates to increased use of coping strategies. The present study found a Cronbach's alpha coefficient of 0.685 for the coping score and the individual questions ranging from 0.599 to 0.684. Again a value higher than 0.70 would be ideal, a value of internal consistency close to 0.60 is satisfactory in terms of a screening tool with five questions.31 To compare the answers to the individual questions between the two groups, statements 1–3 on the scale were rated as “not applicable” and statements 4–6 as “applicable”.
Answers to the open question ‘What helped you most?’ were administered and analysed with MAXQDA 2020 (VERBI software) following a deductive approach.35 , 36 After an initial coding scheme derived from the given topics of the questionnaire, it was applied to the transcripts by two coders, and emerging themes were identified based on an inductive approach. Discrepancies in coding were resolved by consensus.37 Finally, 23 relevant categories were identified through selective coding compared with the literature and the COSMO study38 (see Supplemental material 1). Due to the multiplicity of these answers, the evaluation was exclusively descriptive (Table 4).
Table 4.
Descriptive analyses of the free-text answers on coping.
| Categories | IP |
CP |
||
|---|---|---|---|---|
| n | % | n | % | |
| Intrinsic categories (active coping) | ||||
| Contact with social environment | 1943 | 47.9 | 2489 | 39.1 |
| Offering help/responsibility for others | 507 | 12.5 | 800 | 12.6 |
| Daily structure | 412 | 10.2 | 822 | 12.9 |
| Attitude | 59 | 1.5 | 245 | 3.8 |
| Exercise/physical activity | 61 | 1.5 | 104 | 1.6 |
| Alcohol/drugs | 55 | 1.4 | 188 | 3 |
| Healthy nutrition | 28 | 0.7 | 45 | 0.7 |
| Hobbies | 15 | 0.4 | 33 | 0.5 |
| Being outside | 13 | 0.3 | 30 | 0.5 |
| Avoiding messages related to COVID-19 | 5 | 0.1 | 3 | 0.1 |
| Extrinsic categories (systemic factors) | ||||
| Care by the public health department | 217 | 5.4 | 301 | 4.7 |
| Medical care | 183 | 4.5 | 561 | 8.8 |
| Securing supplies (food, etc.) | 99 | 2.4 | 53 | .8 |
| Financial security | 87 | 2.1 | 22 | 0.4 |
| Work/education | 44 | 1.1 | 78 | 1.2 |
| Categories that cannot be influenced (circumstances/situational factors) | ||||
| Symptoms and risk factors | 118 | 2.9 | 94 | 1.5 |
| Weather | 111 | 2.7 | 258 | 4.1 |
| Housing situation | 41 | 1 | 85 | 1.3 |
| Transmission | 22 | 0.5 | 7 | 0.1 |
| Tests | 6 | 0.2 | 40 | 0.6 |
| Length of quarantine | 1 | 0 | 67 | 1.1 |
| No answer provided | 29 | 0.7 | 46 | 0.7 |
| Other/not attributable | 3 | 0.1 | 2 | 0 |
Exercise and eating behaviour
A yes/no question about exercise/physical activity during quarantine was included. Eating behaviour was assessed via a Healthy Eating Index. This index was calculated by summing the positive and negative responses from the following three categories: change in mealtime (four items), change in frequency (four items) and change in food (14 items). The score for change in meal time could take a value between 1 and 3; the score for change in frequency, a value between 1 and 5; and the score for change in food, a value between 1 and 2. These individual scores were then summed, a total percentage score was calculated based on the points to be achieved, and terciles were formed (>0.75 corresponded to eating healthier; 0.65–0.75 to no change; and <0.65, to eating less healthily).
Data analysis
The data analysis was carried out descriptively and inductively with the programme SPSS 27.0. Univariable differences were examined with the help of chi-square tests and t-tests. Effect sizes were calculated using Cohen's d (independent t-test; trivial: <0.2; small: 0.2–0.5; moderate; 0.5–0.8; large: ≥0.8) or Cramer's V (chi-square test; small: 0.06–0.15; moderate: 0.16–0.26; large >0.26) for significant differences in scores and coping answers between IPs and CPs. Multiple linear regression was used to examine possible influencing factors on the coping score. The considered variables contained in our full model were quarantine as IP (=1) or CP (=2), sex (female = 1 and male = 2), age (in years), migration background (no = 1, yes = 2), SES (low and middle = 1 vs high = 2), presence of chronic diseases (yes = 1, no = 2), living situation with balcony and/or garden vs no access to outdoors (yes = 0, no = 1), living with a partner (yes = 1, no = 2) or children (yes = 1, no = 2), psychological distress score, BRS score, physical activity (yes = 1, no = 2) and healthy eating (unhealthier = 1 vs healthier or no change = 2). Variables not contributing to the regression equation were removed via backward elimination. The significance level was set at α = .05.
Results
Study population and demographic data
Of the 8232 subjects included, 3256 (39.6%) tested positive for COVID-19, and 4976 (60.4%) were quarantined because they were CPs. Women composed 61.5% of the total sample, 57.5% of the IPs and 64.1% of the CPs. The mean age was 41.6 years (±14.2), and the mean quarantine duration was 11.8 days (±4.6) (see Table 1 ).
Table 1.
Demographic data.
| Variables | Total | IP | CP | P value IP vs CP | Effect size |
|---|---|---|---|---|---|
| N | 8232 (100.0) | 3256 (39.6) | 4976 (60.4) | ||
| Sex, n (%) | <.001a | .067b | |||
| Female | 5062 (61.5) | 1871 (57.5) | 3191 (64.1) | ||
| Male | 3170 (38.5) | 1385 (42.5) | 1785 (35.9) | ||
| Age (years) | <.001c | .103d | |||
| Mean (SDe) | 41.6 (14.2) | 42.6 (14.3) | 40.9 (14.1) | ||
| Range | 16–93 | 16–87 | 16–93 | ||
| Quarantine interval in days | <.001c | .122d | |||
| Mean (SDe) | 11.8 (4.6) | 12.1 (5.0) | 11.6 (4.3) | ||
| Range | 1–42 | 1–42 | 1–42 | ||
| Migration background, n (%) | <.001a | .056b | |||
| Yes | 404 (4.9) | 207 (6.5) | 197 (4.0) | ||
| No | 7695 (93.5) | 2977 (93.5) | 4718 (96.0) | ||
| Education level, n (%) | .033f | .029b | |||
| Low | 68 (0.8) | 34 (1.1) | 34 (0.7) | ||
| Middle | 1510 (18.3) | 628 (19.4) | 882 (17.8) | ||
| High | 6600 (80.2) | 2569 (79.5) | 4031 (81.5) | ||
| Household structure | |||||
| Partner, n (%) | .063a n.s. | ||||
| Yes | 5744 (69.8) | 2303 (72.6) | 3441 (70.6) | ||
| No | 2301 (28.0) | 871 (27.4) | 1430 (29.4) | ||
| Children, n (%) | .006a | .030b | |||
| Yes | 3582 (43.5) | 1476 (45.5) | 2106 (42.5) | ||
| No | 4620 (56.1) | 1765 (54.5) | 2855 (57.5) | ||
| Living situation, n (%) | .005a | .040b | |||
| Garden | 1832 (22.3) | 683 (21.0) | 1149 (23.2) | ||
| Balcony | 4093 (49.7) | 1675 (51.6) | 2418 (48.7) | ||
| Garden and balcony | 1022 (12.4) | 424 (13.1) | 598 (12.1) | ||
| None of them | 1259 (15.3) | 463 (14.3) | 796 (16.0) | ||
| Chronic diseases, n (%) | .013a | .028b | |||
| Yes | 1804 (21.9) | 757 (24.1) | 1047 (21.7) | ||
| No | 6148 (74.7) | 2380 (75.9) | 3768 (78.3) |
Chi-square test.
Cramer's V.
Independent t-test; significance level set at ≤.05.
Cohen's d.
SD is standard deviation.
According to chi-square test for SES low vs SES medium to high.
Relative sum scores of coping strategies, resilience and psychological distress
The relative sum scores of the coping strategies and the BRS indicated no significant difference between the two subgroups (see Table 2 ). In contrast, the sum score of psychological distress averaged 1.1 (±0.7) for IPs and was significantly higher than 1.0 (±0.7) for CPs (P < .001). Thus, IPs showed significantly higher psychological distress (see Table 2).
Table 2.
Sum scores of coping, resilience and psychological distress.
| Sum scores | IP |
CP |
P valuea | Effect sizeb | ||
|---|---|---|---|---|---|---|
| N | Mean (SD) | n | Mean (SD) | |||
| Coping score | 3256 | 4.6 (1.0) | 4976 | 4.6 (1.0) | .091 n.s. | |
| Brief resilience scale | 3229 | 3.7 (0.8) | 4948 | 3.6 (08) | .202 n.s. | |
| Psychological distress score | 3245 | 1.1 (0.7) | 4962 | 1.0 (0.7) | <.001 | .120 |
Independent t-test; significance level set at ≤ 0.05.
Cohen's d.
Coping strategies
IPs more frequently stated that they had received offers of support from family, friends or neighbours (item 1; IP: 92.9%, CP: 89.8%) and that they had more exchanges with their social environment via digital media (item 4; IP: 91.0%, CP: 90.0%). They also agreed significantly more often with the statement that they could not do anything themselves to positively influence the situation (item 6; IP: 32.3%, CP: 27.1%). In contrast, they reported having a plan for everyday life less often (item 2; IP: 68.7%, CP: 76.8%) or newly discovered activities that made it easier to stay at home (item 3; IP: 65.9%, CP: 70.1%). Boredom was very heterogeneously distributed in both groups (item 5; IP: 46.4%, CP: 47.0%; n.s.; see Table 3 ).
Table 3.
Coping items.
| Items n (%) | ‘I do not agree at all’ (1) | (2) | (3) | (4) | (5) | ‘I agree completely’ (6) | P valuea | Effect sizeb |
|---|---|---|---|---|---|---|---|---|
| I have received offers of support from family, friends or neighbours. | <.001 | .097 | ||||||
| IP | 91 (2.8) | 72 (2.2) | 67 (2.1) | 141 (4.3) | 327 (10.1) | 2554 (78.5) | ||
| CP | 225 (4.5) | 150 (3.0) | 130 (2.6) | 343 (6.9) | 641 (12.9) | 3479 (70.0) | ||
| I had a plan for my daily life in terms of sleep, work or physical activities. | <.001 | .101 | ||||||
| IP | 449 (13.9) | 283 (8.7) | 283 (8.7) | 484 (15.0) | 604 (18.7) | 1133 (35.0) | ||
| CP | 462 (9.3) | 313 (6.3) | 374 (7.6) | 696 (14.1) | 1078 (21.8) | 2021 (40.9) | ||
| I discovered activities for myself that made staying at home easier. | <.001 | .058 | ||||||
| IP | 474 (14.7) | 324 (10.1) | 300 (9.3) | 557 (17.3) | 634 (19.7) | 931 (28.9) | ||
| CP | 546 (11.0) | 476 (9.6) | 454 (9.2) | 874 (17.7) | 1034 (20.9) | 1559 (31.5) | ||
| I have used digital media to communicate with family, friends and acquaintances. | .035 | .038 | ||||||
| IP | 89 (2.7) | 86 (2.7) | 115 (3.5) | 251 (7.7) | 635 (19.6) | 2066 (63.7) | ||
| CP | 141 (2.8) | 152 (3.1) | 202 (4.1) | 435 (8.8) | 1050 (21.2) | 2975 (60.0) | ||
| I was bored. | .791 n.s. | |||||||
| IP | 843 (26.1) | 535 (16.5) | 355 (11.0) | 575 (17.8) | 440 (13.6) | 485 (15.0) | ||
| CP | 1293 (26.1) | 782 (15.8) | 545 (11.0) | 846 (17.1) | 704 (14.2) | 778 (15.7) | ||
| I couldn't do anything myself to influence the situation positively. | <.001 | .059 | ||||||
| IP | 1087 (33.6) | 696 (21.5) | 408 (12.6) | 478 (14.8) | 267 (8.3) | 298 (9.2) | ||
| CP | 1822 (36.9) | 1149 (23.3) | 628 (12.7) | 632 (12.8) | 355 (7.2) | 350 (7.1) | ||
Chi-square test; significance level set at ≤0.05.
Cramer's V.
Categories
A total of 6292 responses were integrated into the evaluation. Because multiple answers to the question ‘What helped you most?’ were possible, there were a total of 4059 answers for IPs and 6373 answers for CPs. The most frequently mentioned categories for both groups were contact with the social environment (IP: 47.9%; CP: 39.1%), a positive attitude (IP: 12.5%; CP: 12.6%), hobbies (IP: 10.2%; CP: 12.9%), securing care (IP: 5.4%; CP: 4.7%) and work/study (IP: 4.5%; CP: 8.8%; see Table 4 ). Institutional care provided by the health office was mentioned by 2.4% of IPs and 0.8% of CPs (see Table 4).
Multiple linear regression
In a stepwise regression, the variables chronic diseases, living with child(ren), living with a partner and migration background were sequentially excluded in the final model. The remaining variables explained 25.9% of the variance (see Table 5 ). Low psychological distress (β = −0.280; P < .001) as well as a high resilience score (β = 0.139; P < .001) were associated with a higher coping score. The quarantine reason ‘tested positive’ (β = −0.023; P = .034), female gender (β = −0.106; P < .001), higher age (β = 0.174; P < .001), a high SES (β = 0.042; P < .001), exercise (β = −0.171; P < .001) and unchanged or healthier eating behaviour (β = 0.123; P < .001) showed a positive correlation with the coping score. In addition, a living situation with balcony or garden access correlated with a higher coping score as well. However, this correlation was not found to be significant.
Table 5.
Baseline and final model explaining 25.9% of the variance of the coping score.
| Models | Independent variables | Standardised regression coefficient β (standard error) | P valuea |
|---|---|---|---|
| Baseline model | Quarantine as IP vs CP | −.022 [.022] | .040 |
| Age (in years) | .184 [.001] | <.001 | |
| Sex female vs male | −.106 [.022] | <.001 | |
| Migration background no vs yes | −0.011 [.047] | .292 n.s. | |
| SES medium or low vs high | .043 [.027] | <.001 | |
| Chronical diseases yes vs no | .000 [.025] | .984 n.s. | |
| Living situation with balcony and/or garden vs no access to outdoors | −.020 [.030] | .072 n.s. | |
| Living with a partner yes vs no | .011 [.024] | .335 n.s. | |
| Living with child(ren) yes vs no | −.007 [.026] | .611 n.s. | |
| Brief resilience scale score | .138 [.015] | <.001 | |
| Psychological disstress score | −.281 [.017] | <.001 | |
| Healthy Eating Index (unhealthier vs healthier or no change) | .122 [.023] | <.001 | |
| Physical activity during quarantine yes vs no | −.167 [.023] | <.001 | |
| Final model | Quarantine as IP vs CP | −.022 [.022] | .046 |
| Age (in years) | .186 [.001] | <.001 | |
| Sex female vs male | −.107 [.022] | <.001 | |
| SES medium or low vs high | .042 [.027] | <.001 | |
| Living situation with balcony and/or garden vs no access to outdoors | −.020 [.029] | .070 n.s. | |
| Brief resilience scale score | .138 [.015] | <.001 | |
| Psychological disstress score | −.280 [.017] | <.001 | |
| Healthy Eating Index (unhealthier vs healthier or no change) | .122 [.023] | <.001 | |
| Physical activity during quarantine yes vs no | −.167 [.023] | <.001 |
Linear regression; significance level set at ≤.05.
Discussion
To our knowledge, this is one of the first studies to examine coping strategies and their influencing factors in the context of a legally enforced quarantine in Germany. In summary, the IPs reported higher psychological distress than the CPs, though with a small effect size. However, there was no difference in the mean coping score. Approximately three-quarters of participants in the current study used active coping strategies (IP: 76.3%; CP: 74.7%), whereas a much smaller proportion considered extrinsic social or societal factors (IP: 15.5%; CP: 15.9%) or situational factors (IP: 7.3%; CP: 8.6%) to be helpful. The most relevant factors for both the IP and the CP groups were contact with the social environment followed by a positive attitude and engaging in hobbies. Regarding the extrinsic categories, providing for oneself and work or study played the most important roles for both groups. For those in the IP group, the third most important factor was sufficient support from the Cologne health authority (IP: 2.4%; CP: 0.8%); among the CP group, the third most important factor was financial security (IP: 1.1%; CP: 1.2%). Similarly, Fu et al. presented the frequencies of active and passive coping strategies in their study based on an online survey in Wuhan.6 Overall, a large proportion of respondents (70.2%) reported actively responding to the pandemic. This included participating in activities, talking to others about their concerns and looking at possible positives. Passive coping strategies, such as smoking and depending on others, were used by 29.8%.6 Singh et al. surveyed subjects with suspected COVID-19 infections in India regarding their experiences during institutional quarantine.39 The vast majority, 80.6%, reported that they perceived support from family and friends as helpful. Having a daily routine (57%), praying (70%) and music (45%) were also reported as other coping strategies.39
The results of the COSMO study showed a decrease in the use of coping strategies and general life satisfaction and a simultaneous increase in boredom and perceived helplessness between March 2020 and March 2021.40 Coping strategies that decreased over time included using the telephone or social media, making plans for daily life and implementing new activities to facilitate staying at home. Furthermore, both offering and receiving support diminished.40 In the same period, the self-reported perception of stress increased from 51.8% to 56.3%.40
In our study, a higher coping score was associated with female gender, higher age, the quarantine reason ‘tested positive’, a higher SES and resilience score as well as lower psychological distress during stay-at-home order. In addition, a healthy lifestyle, that is, a healthy diet or physical activity during quarantine, had a positive effect on the coping score. Thus, this study at least partially confirms already existing results. In a population-based study by Iddi et al. education and economic class were also significantly related with coping.41 Furthermore, especially emotion-focused and problem-focused coping strategies were associated with positive moods,19 , 42 , 43 whereas dysfunctional coping strategies were associated with negative moods43 and higher levels of worry.44 In contrast, physical activity, following a routine and pursuing hobbies were negatively correlated with depression, anxiety and acute stress symptoms.3 , 45 Adaptive coping strategies such as acceptance, reframing and a sense of humour, as well as seeking emotional support showed a negative correlation to psychopathological symptoms.10
Moreover, in the overall view of our results, a key function of the health department or care during the quarantine period can be inferred. Being a central contact, the health department has, on the one hand, an advisory function. By addressing possible coping strategies and providing hints to do things such as activating their social networks, citizens' intrinsic coping strategies and resources could be activated. Recommendations regarding a healthy lifestyle such as exercising or using relaxation techniques during the quarantine period should also be addressed in the care. In addition, the office can function as a mediator. It could establish connections between those affected and external support systems, such as everyday or neighbourhood helpers who can ensure that those affected are cared for. It could also establish a special quarantine hotline to make the office accessible to those affected. Corresponding offices have already been established, for example, by the health department of the city of Cologne; this hotline is known as the ‘worry phone.’ Potential beneficial effects of these measures are also reflected in the free responses on coping. In particular, participants in the IP group mentioned the effective, detailed and empathetic care and information provided by the authorities as a positive factor and coping strategy in itself. Qualified advise could thus avoid the long-term persistence of psychological distress that has already been observed in previous pandemics.46
Strengths and limitations
A clear strength of the present study is its large sample size, which includes a systematically recorded set of Cologne citizens under legally enforced quarantine. Through the possibility of free-text answers, this study also included qualitative questions and thus enabled a detailed insight into the respondents’ way of thinking. However, due to the subsequent anonymisation of the inputs, no analysis of the effects of individual coping strategies on the coping score and thus possibly on psychological distress is possible. Thus, this is a purely explorative and descriptive recording of applied mechanisms, which can form the basis for further studies and provides many suggestions for the accompaniment and care of quarantined people.
In addition, the questionnaire was based on the COSMO study so that the results could also be compared with its data. Therefore, items of established questionnaires such as the GAD-7, ADS and IES-R were combined. None of these classic questionnaires was used in their complete psychometrically evaluated form, and the COPE inventory was not used either. A largely stable Cronbach's alpha was found, indicating the internal reliability of our study. External validity, on the other hand, is not verifiable. The reason for this is firstly the complete anonymity of the study, which does not allow a comparison between responders and non-responders, and secondly, the lack of a matched unquarantined control group. Another limitation arises from the fact that the questionnaire was answered mainly by people with a high level of education. Citizens with a migration background are also underrepresented despite translated questionnaires. Furthermore, it should be noted that the participants sometimes answered the questionnaire months after the actual quarantine period. This could have influenced and distorted the answers and assessments given. The influence of the time of the quarantine, the concrete regulations, and the currently prevailing state of knowledge about the coronavirus were also omitted. Causal inferences are only possible to a limited extent due to the cross-sectional design.
Conclusion
In summary, IPs experienced a significantly higher psychological burden than CPs and benefited, above all, from the social environment and from close care during their legally enforced quarantine. In contrast to CPs, IPs more often felt powerless in the face of their situation. Conversely, CPs more often reported making plans for everyday life and finding new activities during their quarantine period.
In addition to providing support and counselling to quarantined people on how to cope with the disease and this crisis, health offices could also act as an interface between those affected and external support systems such as general practitioners and/or psychiatrists. This would give them a key role in combating the pandemic and reducing possible long-term psychological consequences.
Author statements
Ethical approval
The studies involving human participants were reviewed and approved by Rheinisch-Westfälische Technische Hochschule (RWTH) Aachen Human Ethics Research Committee (351/20).
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Availability of data and materials
The data sets used and/or analysed in the present study are not publicly available due to the inclusion of sensitive personal data.
Authors’ contributions
C.J., B.G., S.F., L.K., A.F., A.K., J.N. and G.W. conducted the study. Data collection was done by L.K., A.F., N.E. and C.G. L.K. and C.J. analysed the data. L.K. and C.J. wrote the manuscript. All authors critically revised the final version of the manuscript.
Acknowledgements
The authors would like to thank all members of the contact tracing team at the Cologne Public Health Department. The authors would also like to thank all persons who participated in this questionnaire.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2022.05.022.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.WHO. Coronavirus disease 2019 (COVID-19) situation report – 94; Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200423-sitrep-94-covid-19.pdf.
- 2.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020.
- 3.Fullana M.A., Hidalgo-Mazzei D., Vieta E., Radua J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J Affect Disord. 2020;275:80–81. doi: 10.1016/j.jad.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hossain M.M., Tasnim S., Sultana A., Faizah F., Mazumder H., Zou L., et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahman M.A., Hoque N., Alif S.M., Salehin M., Islam S.M.S., Banik B., et al. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Glob Health. 2020;16(1):95. doi: 10.1186/s12992-020-00624-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S., et al. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl Psychiatry. 2020;10(1):225. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wasserman D., van der Gaag R., Wise J. The term "physical distancing" is recommended rather than "social distancing" during the COVID-19 pandemic for reducing feelings of rejection among people with mental health problems. Eur Psychiatr. 2020;63(1):e52. doi: 10.1192/j.eurpsy.2020.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatr. 2020;63(1):e32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benke C., Autenrieth L.K., Asselmann E., Pané-Farré C.A. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatr Res. 2020;293:113462. doi: 10.1016/j.psychres.2020.113462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kołodziejczyk A., Misiak B., Szcześniak D., Maciaszek J., Ciułkowicz M., Łuc D., et al. Coping styles, mental health, and the COVID-19 quarantine: a nationwide survey in Poland. Front Psychiatr. 2021;12:625355. doi: 10.3389/fpsyt.2021.625355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.TMGH-Global COVID-19 Collaborative Perceived stress of quarantine and isolation during COVID-19 pandemic: a global survey. Front Psychiatr. 2021;12:656664. doi: 10.3389/fpsyt.2021.656664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rice V., Liu B. Personal resilience and coping with implications for work. Part I: a review. WOR. 2016;54(2):325–333. doi: 10.3233/WOR-162300. [DOI] [PubMed] [Google Scholar]
- 13.Skinner E.A., Edge K., Altman J., Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129(2):216–269. doi: 10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus R.S., Folkman S. Springer Publishing Company; New York, NY: 1984. Stress, appraisal, and coping. [Google Scholar]
- 15.Lazarus R.S. From psychological stress to the emotions: a history of changing outlooks. Annu Rev Psychol. 1993;44:1–21. doi: 10.1146/annurev.ps.44.020193.000245. [DOI] [PubMed] [Google Scholar]
- 16.Endler N.S., Parker J.D. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990;58(5):844–854. doi: 10.1037/0022-3514.58.5.844. [DOI] [PubMed] [Google Scholar]
- 17.Park C.L., Russell B.S., Fendrich M., Finkelstein-Fox L., Hutchison M., Becker J. Americans' COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020;35(8):2296–2303. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saalwirth C., Leipold B. Well-being and sleep in stressful times of the COVID-19 pandemic: relations to worrying and different coping strategies. Stress Health. 2021 doi: 10.1002/smi.3057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Budimir S., Probst T., Pieh C. Coping strategies and mental health during COVID-19 lockdown. J Ment Health. 2021;30(2):156–163. doi: 10.1080/09638237.2021.1875412. [DOI] [PubMed] [Google Scholar]
- 20.Golemis A., Voitsidis P., Parlapani E., Nikopoulou V.A., Tsipropoulou V., Karamouzi P., et al. Young adults' coping strategies against loneliness during the COVID-19-related quarantine in Greece. Health Promot Int. 2022;37(1) doi: 10.1093/heapro/daab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neuhann F., Buess M., Wolff A., Pusch L., Kossow A., Winkler M., et al. Softwareentwicklung zur Unterstützung der Prozesse im Gesundheitsamt der Stadt Köln in der SARS-CoV-2-Pandemie Digitales Kontaktmanagement (DiKoMa) Epidemiol Bull. 2020;(23):3–11. [Google Scholar]
- 22.Joisten C., Kossow A., Book J., Broichhaus L., Daum M., Eisenburger N., et al. How to manage quarantine-adherence, psychosocial consequences, coping strategies and lifestyle of patients with COVID-19 and their confirmed contacts: study protocol of the CoCo-Fakt surveillance study, Cologne, Germany. BMJ Open. 2021;11(4) doi: 10.1136/bmjopen-2020-048001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betsch C., Wieler L.H., Habersaat K. Monitoring behavioural insights related to COVID-19. Lancet. 2020;395(10232):1255–1256. doi: 10.1016/S0140-6736(20)30729-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lampert T., Kroll L.E., Müters S., Stolzenberg H. Messung des sozioökonomischen Status in der Studie "Gesundheit in Deutschland aktuell" (GEDA) Bundesgesundheitsblatt - Gesundheitsforsch - Gesundheitsschutz. 2013;56(1):131–143. doi: 10.1007/s00103-012-1583-3. [DOI] [PubMed] [Google Scholar]
- 25.Lange C., Jentsch F., Allen J., Hoebel J., Kratz A.L., von der Lippe E., et al. Data resource profile: German health update (GEDA)—the health interview survey for adults in Germany. Int J Epidemiol. 2015;44(2):442–450. doi: 10.1093/ije/dyv067. [DOI] [PubMed] [Google Scholar]
- 26.Fragebogen Welle 4, 24.03.-25.03.2020 [questionnaire wave 4, 24 March 2020-25 March 2020]. [July 24, 2021]; Available from: https://dfncloud.uni-erfurt.de/s/Cmzfw8fPRAgzEpA#pdfviewer.
- 27.Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 28.Hautzinger M., Bailer M., Hofmeister D., Keller F. 2nd ed. Prag; Göttingen, Bern, Wien, Paris, Oxford: 2012. ADS: manual. Toronto, Cambridge, MA, Amsterdam, Kopenhagen, Stockholm: Hogrefe. [Google Scholar]
- 29.Reime B., Steiner I. Ausgebrannt oder depressiv?: Eine empirische Studie zur Konstruktvalidität von Burnout in Abgrenzung zur Depression. Psychother Psychosom Med Psychol. 2001;51(8):304–307. doi: 10.1055/s-2001-15996. [DOI] [PubMed] [Google Scholar]
- 30.Maercker A., Schützwohl M. IES-R; 1998. Erfassung von psychischen Belastungsfolgen: die Impact of Event Skala-revidierte Version. [Google Scholar]
- 31.Muris P., Meesters C., Eijkelenboom A., Vincken M. The self-report version of the Strengths and Difficulties Questionnaire: its psychometric properties in 8- to 13-year-old non-clinical children. Br J Clin Psychol. 2004;43(Pt 4):437–448. doi: 10.1348/0144665042388982. [DOI] [PubMed] [Google Scholar]
- 32.Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 33.Kunzler A.M., Chmitorz A., Bagusat C., Kaluza A.J., Hoffmann I., Schäfer M., et al. Construct validity and population-based norms of the German brief resilience scale (BRS) Eur J Health Psychol. 2018;25(3):107–117. doi: 10.1027/2512-8442/a000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Satici B., Saricali M., Satici S.A., Griffiths M.D. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int J Ment Health Addiction. 2020:1–12. doi: 10.1007/s11469-020-00305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patton M.Q. 3rd ed. Sage; Thousand Oaks, Calif: 2009. Qualitative research & evaluation methods. [Google Scholar]
- 36.Glaser B.G., Strauss A.L. Routledge; London, New York: 2017. The discovery of grounded theory: strategies for qualitative research. [Google Scholar]
- 37.Fetters M.D., Curry L.A., Creswell J.W. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48(6 Pt 2):2134–2156. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maertl T., Bock F de, Huebl L., Oberhauser C., Coenen M., Jung-Sievers C., et al. Physical activity during COVID-19 in German adults: analyses in the COVID-19 snapshot monitoring study (COSMO) Int J Environ Res Publ Health. 2021;18(2) doi: 10.3390/ijerph18020507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singh N., Kumar S., Rathore P., Vig S., Vallath N., Mohan A., et al. Concerns and coping strategies of persons under institutional quarantine during SARS-CoV-2 pandemic. Indian J Palliat Care. 2020;26(Suppl 1):S99–S105. doi: 10.4103/IJPC.IJPC_176_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ressourcen und Belastungen COSMO [resources and strain COSMO]. [August 11, 2021]; Available from: https://projekte.uni-erfurt.de/cosmo2020/web/topic/vertrauen-zufriedenheit-ressourcen/20-belastungen/#umgang-mit-der-situation-stand-09.03.21.
- 41.Iddi S., Obiri-Yeboah D., Aboh I.K., Quansah R., Owusu S.A., Enyan N.I.E., et al. Coping strategies adapted by Ghanaians during the COVID-19 crisis and lockdown: a population-based study. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0253800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cincidda C., Pizzoli S.F.M., Oliveri S., Pravettoni G. Regulation strategies during Covid-19 quarantine: the mediating effect of worry on the links between coping strategies and anxiety. Eur Rev Appl Psychol. 2021:100671. doi: 10.1016/j.erap.2021.100671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beato A.F., da Costa L.P., Nogueira R. "Everything is gonna Be alright with me": the role of self-compassion, affect, and coping in negative emotional symptoms during coronavirus quarantine. Int J Environ Res Publ Health. 2021;18(4) doi: 10.3390/ijerph18042017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sebri V., Cincidda C., Savioni L., Ongaro G., Pravettoni G. Worry during the initial height of the COVID-19 crisis in an Italian sample. J Gen Psychol. 2021;148(3):327–359. doi: 10.1080/00221309.2021.1878485. [DOI] [PubMed] [Google Scholar]
- 45.Li G., Miao J., Wang H., Xu S., Sun W., Fan Y., et al. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J Neurol Neurosurg Psychiatry. 2020;91(8):895–897. doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- 46.Jeong H., Yim H.W., Song Y.-J., Ki M., Min J.-A., Cho J., et al. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets used and/or analysed in the present study are not publicly available due to the inclusion of sensitive personal data.