Abstract
After initial strategies targeting inotropism and congestion, the neurohormonal interpretative model of heart failure (HF) pathophysiology has set the basis for current pharmacological management of HF, as most of guideline recommended drug classes, including beta-blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and mineralocorticoid receptor antagonists, blunt the activation of detrimental neurohormonal axes, namely sympathetic and renin–angiotensin–aldosterone (RAAS) systems. More recently, sacubitril/valsartan, a first-in-class angiotensin receptor neprilysin inhibitor, combining inhibition of RAAS and potentiation of the counter-regulatory natriuretic peptide system, has been consistently demonstrated to reduce mortality and HF-related hospitalization. A number of novel pharmacological approaches have been tested during the latest years, leading to mixed results. Among them, drugs acting directly at a second messenger level, such as the soluble guanylate cyclase stimulator vericiguat, or other addressing myocardial energetics and mitochondrial function, such as elamipretide or omecamtiv-mecarbil, will likely change the therapeutic management of patients with HF. Sodium glucose cotransporter 2 inhibitors, initially designed for the management of type 2 diabetes mellitus, have been recently demonstrated to improve outcome in HF, although mechanisms of their action on cardiovascular system are yet to be elucidated. Most of these emerging approaches have shifted the therapeutic target from neurohormonal systems to the heart, by improving cardiac contractility, metabolism, fibrosis, inflammation, and remodeling. In the present paper, we review from a pathophysiological perspective current and novel therapeutic strategies in chronic HF.
Keywords: Heart failure, Pharmacotherapy, Pharmacodynamics, Neurohormonal antagonism, Emerging targets, SGLT2 inhibitors
Introduction
Heart failure (HF) represents a global health issue, as it is estimated to affect 1–2% of the general population, with an even higher prevalence in cohorts of elderly subjects [1]. Several interpretative models have been proposed over the last decades to explain HF pathophysiology. They initially focused on the concomitant impairment of both heart and kidney (cardio-renal model), and later on hemodynamic alterations secondary to pump failure (hemodynamic model) [2]. In the last 30 years, the neurohormonal model has taken a central role, following the demonstration that derangement of neurohormonal activation and of peripheral feedbacks acts as promoter in HF syndrome and represents the pathophysiological basis for the use of most of pharmacological classes with a prognostic benefit [3].
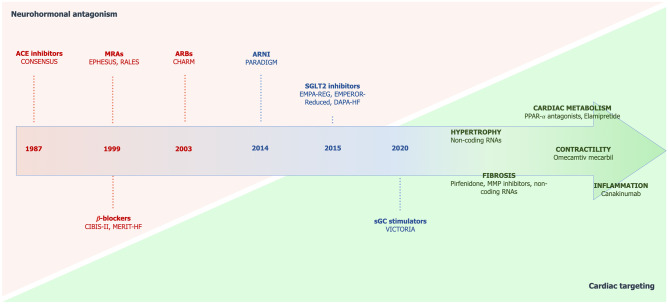
In clinical practice, HF is usually classified based on left ventricular ejection fraction (LVEF) into HF with reduced ejection fraction (HFrEF, LVEF < 40%), HF with preserved ejection fraction (HFpEF, LVEF ≥ 50%), and in the recently proposed category of HF with mid-range ejection fraction (HFmrEF, LVEF 40–49%) [4]. While many pharmacological and non-pharmacological therapies of HFrEF have shown a prognostic benefit, the outcome of patients with HFrEF still remains poor [5]. To date, few evidence-based data are available as concerns treatment of patients with milder degree of LV systolic dysfunction, as the majority of the drugs investigated have failed to demonstrate prognostic benefit in HFpEF [6]. Nevertheless, novel therapies are emerging in latest years, most of them targeting myocardial energetics, shifting the focus back from the periphery to the heart muscle (Fig. 1). Herein, we review the current and novel potential therapeutic strategies in chronic HF from a pathophysiological perspective.
Fig. 1.
Chronologic development of drugs in heart failure, highlighting the shift from neurohormonal antagonism to specific cardiac targeting. Current guideline recommended drugs classes are represented in bold red; drug classes with existing evidence on an outcome benefit in heart failure are represented in bold blue; novel possible targets are represented in green. ACE angiotensin-converting enzyme; ARBs angiotensin receptor blockers; ARNI angiotensin receptor neprilysin inhibitor; MRAs mineralocorticoid receptor antagonists; sGC soluble guanylate cyclase; SGLT2 sodium-glucose cotransporter 2
Current therapeutic targets
Sympathetic nervous system
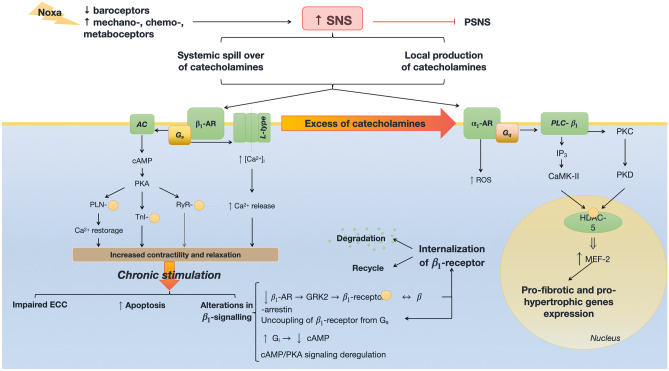
HF is characterized by an imbalance between sympathetic and parasympathetic afferent systems. A blunted baroreflex is usually combined with hyperactive chemo- and ergoreflexes [7, 8]. The final result of this imbalance is an overactivation of the sympathetic nervous system (SNS), initially aimed at restoring the circulatory homeostasis. Chronic stimulation of SNS causes a systemic spill-over of catecholamines, attributed to their increased release and reduced reuptake, and to an excessive intra-myocardial production [9] (Fig. 2).
Fig. 2.
Molecular signaling of sympathetic nervous system (SNS) activation in the cardiomyocyte in heart failure. -AR adrenergic receptor; AC adenylate cyclase; AR adrenergic receptor; CaMK-II calcium-calmodulin kinase type 2; cAMP cyclic adenosine monophosphate; Gi G-protein “i” associated with trans-membrane receptor; Gq G-protein “q” associated with trans-membrane receptor; GRK2 complex G protein-coupled receptor kinase type 2; Gs G-protein “s” associated with trans-membrane receptor; HDAC-5 histone deacetylase type 5; IP3 inositol trisphosphate; L-type L-type calcium channel; MEF-2 myocyte enhancer factor type 2; PKA protein-kinase A; PKC protein-kinase C; PKD protein-kinase D; PLC- phospholipase C-; PLN phospholamban; PSNS parasympathetic nervous system; ROS reactive oxygen species; RyR ryanodine receptor; SR sarcoplasmic reticulum; TnI troponin-I
Stimulation of 1 adrenergic receptor by catecholamines, mainly by norepinephrine, activates GS protein [10]. GS protein in turn stimulates L-type calcium channels with increased calcium conductance, and activates adenylate-cyclase, thus resulting in an increased cyclic adenosine monophosphate (cAMP) production and in protein-kinase A activation. Protein-kinase A regulates phosphorylation of phospholamban, troponin I, and ryanodine receptor, thus improving myocardial contraction and relaxation [11]. Chronic stimulation of adrenergic receptors holds detrimental effects. The role of α1 receptors is less defined, and there is evidence that they may hold important adaptive functions, promoting cardiomyocyte survival and protecting against adverse remodeling [12]. Conversely, persistent activation of 1-adrenergic receptor negatively affects excitation–contraction coupling (ECC) and enhances pro-apoptotic pathways [13] (see also Table 1).
Table 1.
Main molecular pathways involved in heart failure (HF) pathophysiology, therapeutic targets, second messengers, adaptive, and maladaptive effects on the cardiovascular system and related drugs. Entries in italics represent the current guidelines-based drugs for heart failure. Entries in bold represent drugs with demonstrated benefits in the outcome of heart failure, yet not included in guidelines. AC adenylate cyclase; cAMP cyclic adenosine monophosphate; cGMP cyclic guanosine monophosphate; CPT Acetyl-CoA C-acetyl transferase; DAG diacyl-glycerol; ET endothelin receptor; HIF hypoxia inducible factor; HSD hydroxysteroid dehydrogenase; ICAM intercellular adhesion molecule 1; IL interleukin; IP3 inositol triphosphate; JAK/STAT Janus kinase/signal transducer and activator transcription factor; LDLox oxidized LDL; MEF myocyte enhancer factor; MMP metalloproteinases; NADPH nicotinamide-adenine dinucleotide; NO nitric oxide; NP natriuretic peptide; NPR natriuretic peptide-binding receptor; PKA protein kinase A; PKB protein kinase B; PKC protein kinase C; PKG protein kinase G; PLC phospholipase; PlGF placental-derived growth factor; PP- protein phosphatase-; PPAR peroxisome proliferator-activated receptor; PTP phosphotyrosine phosphatase; ROS reactive oxygen species; RyR ryanodine receptor; SERCA sarco/endoplasmic reticulum calcium ATPase; TGF transforming growth factor; TRPV transient receptor potential cation channel subfamily V; vSMCs vascular smooth muscle cells
| Pathway | Receptor/target | Second messenger | Adaptive effects | Maladaptive effects | Drugs |
|---|---|---|---|---|---|
| Sympathetic nervous system | Gs > AC > cAMP > PKA | Increased contractility and relaxation |
Excitation contraction uncoupling Apoptotic pathways Alterations in signals |
Selective blockers (e.g., bisoprolol) | |
|
Gq > PLC- > DAG, IP3, PKC > MEF-2 ROS |
Pro-fibrotic and pro-hypertrophic genes expression | Non-selective blockers (e.g., carvedilol) | |||
| Renin–angiotensin–aldosterone system | AT-1 |
Gq > NADPH oxidase – ROS JAK/STAT > PTK PLC > DAG, IP3, PKC Tyrosine kinase—MAPK |
Vasoconstriction, inflammation, proliferation, atherosclerosis Inflammation, growth, proliferation DAG, IP3 > vasoconstriction Inflammation, growth, proliferation |
ACE inhibitors, AT-1 antagonists (ARBs) | |
| AT-2 |
Bradykinins > NO > cGMP Gq > PP2A, PTP > ↓ MAPK |
Vasodilation, blunt in inflammation, growth and proliferation | ACE inhibitors | ||
| MR |
Tissues with 11--HSD2: Kidney: sodium-water retention vSMCs: galectin-3; PKB; PlGF Endothelium: ICAM. Tissues without 11--HSD2: Cardiomyocytes Macrophages: M1 phenotype |
Increased contractility |
Hypertension Fibrosis; apoptosis; atherosclerosis Leukocytes adhesion Hypertrophy, electric instability, oxidative stress Fibrosis and damage |
MR antagonists (MRAs) | |
| Natriuretic peptides | NPR-A | GC > cGMP > PKG | Vasodilation, diuresis, natriuresis, inhibition of cardiac hypertrophy and remodeling, suppression of ADH, blunt in SNS discharge | Angiotensin receptor/Neprilysin inhibitor | |
| NPR-B | Inhibition of vSMC proliferation, LDLox migration, ET-1 release | ||||
| NPR-C | Internalization of NPs for degradation | Blunt in NPs effects | |||
| Nitric oxide | Guanylate cyclase | cGMP | Vasodilation and muscular relaxation | Soluble guanylate cyclase stimulators (vericiguat) and activators | |
| SGLT-2 | SGLT-2 | Glucose and sodium reabsorption |
Glucose, sodium and water retention Activation of SNS? Oxidative stress? Cardiomyocyte metabolic impairment with usage of unfavorable substrates? |
Empagliflozin, Dapagliflozin | |
| Endothelin | ET-A |
Gq > PLC > DAG, IP3 Gs |
Increased contractility | Fibrosis, arrhythmias, hypertrophy, vasoconstriction | Endothelin receptor antagonists, both selective (-A or -B) or non-selective |
| ET-B |
Gq > PLC > DAG, IP3 Gs |
cGMP-dependent endothelium-mediated vasodilation | Fibrosis, apoptosis, hypertrophy, PKC-dependent vasoconstriction | ||
| Anti-diuretic hormone | V1a | Gq > PLC > DAG, IP3 | Increased contractility | Vasoconstriction, platelets aggregation, hypertrophy | Vaptans |
| V1b | Increased ACTH production | ||||
| V2 | Gs > AC > cAMP > aquaporin 2 | Water reabsorption, hyponatremia | |||
| Mitochondria | PPAR- | Transactivation of genes for -oxidation: CPT-1, MCAD | Induces shift to lipidic metabolism | PPAR- antagonists? | |
| CPT | Stimulation of -oxidation | Trimetazidine | |||
| Cardiolipin | Mitochondrial membrane stabilizer | Efficient mitochondrial respiration | Elamipretide? | ||
| Q10 coenzyme | Efficient mitochondrial respiration | Q10 supplements | |||
| Nox2 ROS | ↓ PP-1 activity | Increased activity of SERCA and RyR | Impairment of the activity of both proteins, due to chronic oxidation |
Antioxidants? Elamipretide? |
|
| Nox4 ROS |
↓ PP-1 activity HIF stabilized |
Angiogenesis | Hypertrophy | ||
| Inflammation | e.g. IL-1 | Canakinumab? | |||
| Fibrosis | TGF- | Cardiac fibrosis | Pirfenidone? | ||
| MMP | MMP inhibitors? | ||||
| Galectin-3 | Antisense RNA? | ||||
| TRPV-4 | TGF- | Calcium | Vasodilation, arteriogenesis | Cardiac fibrosis, pulmonary hypertension, HF-related pulmonary edema | TRPV-4 inhibitors? |
Inhibition of adrenergic receptors is effectively achieved by -blockers, a wide and heterogeneous class of drugs. Their use in HF has been firstly debated because of their negative chronotropic and inotropic effects. Actually, their use has been proved effective, and represents a cornerstone of the pharmacological treatment for HF [14]. Specifically, -blockers cause a reduction in myocardial oxygen consumption and prevent the detrimental consequences of a longstanding adrenergic stimulation [15]. Some molecules can also inhibit adrenergic receptor (non-selective -blockers, such as carvedilol); other can exert a weak agonism to the -receptor (i.e., pindolol), a property known as intrinsic sympathomimetic activity, but none of them has been proven effective in HF. -blockers, particularly non-selective ones, might cause subtype-specific upregulation of adrenergic receptors and therefore should not be withdrawn abruptly [16].
Renin–angiotensin–aldosterone system
Renin and angiotensins
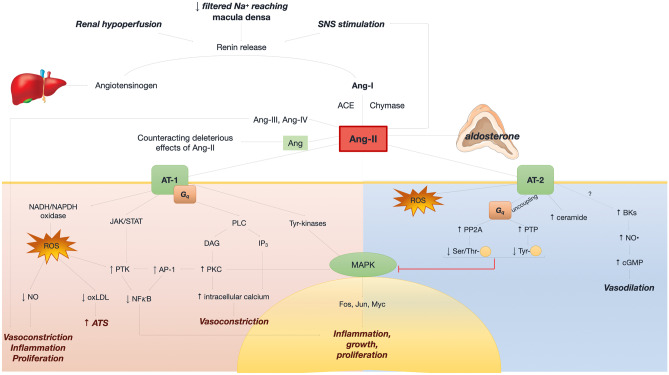
Renin–angiotensin–aldosterone system (RAAS) is one of the main drivers in HF pathophysiology. Renin release from juxtaglomerular apparatus is the first step in the RAAS cascade. SNS activation, together with renal hypoperfusion and reduced filtered sodium levels reaching the macula densa are the main stimuli for renin secretion [13, 17]. Renin converts angiotensinogen—synthetized by the liver—into Ang-I, which is further cleaved into Ang-II by the angiotensin-converting enzyme (ACE), and, to a lesser extent, by other enzymes, such as chymases [18]. Renin, as well as its precursor prorenin, also exists as a cytosolic protein with other non-enzymatic functions [19]. The cytosolic renin exerts different and even opposite functions to those of secretory renin; specifically, whereas secretory renin promotes necrosis and fibrosis, the cytosolic renin variant protects cells from necrotic death. Binding of either secretory renin or prorenin to its (pro)renin receptor triggers downstream intracellular signals leading to the overexpression of pro-fibrotic genes. The interaction between renin and (pro)renin receptor also increases renin cleavage activity at cell surface [20].
Ang-II interacts with angiotensin receptor (AT) 1 and AT-2. Ang-II directly regulates glomerular homeostasis and stimulates aldosterone production in the adrenal gland. Downstream actions following the interaction of Ang-II with AT-1 include nicotinamide-adenine dinucleotide phosphate (NADPH) oxidase activation, JAK-STAT signaling, phospholipase C pathway, and tyrosine kinases activation [21, 22]. NADPH oxidase activation causes ROS production, reduced nitric oxide (NO) concentration, inflammation, and proliferation [23–25]. Ang-II/AT-2 interaction promotes ROS production, increases intracellular ceramide levels, and causes the uncoupling of AT-2 from Gq, leading to a reduction of mitogen-activated protein kinase (MAPK) activity and of inflammatory, proliferative, and growth-related effects [26]. Ang-II is also cleaved into other peptides (Ang-III and Ang-IV), causing vasoconstrictive effects, and Ang peptide 1–7 via ACE isoform 2, counteracting the deleterious effects of Ang-II [27] (Fig. 3). Ang 1–7 also have direct cardioprotective and vasodilatory actions, by inducing the release of NO and prostaglandins and by antagonizing AT-1 [28, 29]. Indeed, preclinical studies have shown that Ang 1–7 blunts ischemia–reperfusion injury and inhibits Ang-II-induced cardiac hypertrophy and remodeling [30, 31]. The latter effect is mostly mediated by the binding to its high selective G-protein coupled Mas receptor [32].
Fig. 3.
Molecular signaling of the renin–angiotensin–aldosterone system in heart failure. Angiotensin receptor 1 (AT-1) as well as many angiotensins (II, III, IV) are responsible for vasoconstriction, inflammation, proliferation and atherosclerosis. AT-2 counteracts these detrimental responses mainly via vasodilation. Ang angiotensin; AP-1 activator protein 1; ATS atherosclerosis, BK bradykinin; cGMP cyclic guanosine monophosphate; DAG diacyl-glycerol; IP3 inositol-triphosphate; JAK/STAT Janus kinase/signal transducer and activator transcription factor; NAD(P)H nicotinamide-adenine dinucleotide (phosphate); NFkB nuclear factor kappa-B; NO nitric oxide; oxLDL oxidized low-density lipoprotein; PKC protein kinase C; PLC phospholipase; PP2A protein phosphatase 2A; PTK phosphotyrosine kinase; PTP phosphotyrosine phosphatase; Ser/Thr serine/threonine; Tyr tyrosine
RAAS blockade plays a key role in the neurohormonal antagonism in HF. Many molecules targeting different steps in the RAAS cascade have been evaluated, with ACE inhibitors, AT-1 receptor blockers (ARBs), and aldosterone antagonists being the most widely tested. ACE inhibitors and ARBs have been introduced in clinical practice as potent vasodilators, but also showed antiremodeling properties in the setting of either ischemic and non-ischemic LV dysfunction [33–35].
Compared to ACE inhibitors, ARBs have a downstream activity as they prevent Ang-II from binding to AT-1. This was hypothesized to contribute to a binding shift of Ang-II to AT-2, thus resulting in additional antifibrotic effects vs. ACE inhibitors. Nonetheless, there is weaker evidence on the clinical efficacy of ARBs compared to ACE inhibitors in HF patients [4]. Although a potential advantage from a double RAAS blockade with a combination of ACE inhibitors and ARBs may be envisaged, such strategy did not prove effective in clinical practice. Further, the direct renin inhibitor aliskiren did not reduce the rates of all-cause and cardiovascular mortality in HF patients [36]. Novel renin inhibitors are currently under investigation and are showing promising results in murine models [37]. Finally, as discussed in a following paragraph, combined angiotensin receptor and neprilysin inhibition has become the first option among drugs acting on RAAS.
Vasodilation as a potential therapeutic target has been addressed also before RAAS inhibition, as hydralazine—an inositol triphosphate inhibitor—reduced mortality by 34% in the V-HeFT trial [38]. Today, it is used especially in the Afro-Americans, as it showed a 47% reduction in mortality in the A-HeFT trial [39].
Aldosterone
Aldosterone is a steroid hormone produced by the adrenal cortex. Aldosterone signaling includes genomic and non-genomic actions, which are mediated by intracellular and membrane mineralocorticoid receptors (MRs), respectively [40]. Although the intracellular receptor is responsible for the potential binding of several molecules, including aldosterone and glucocorticoids, the receptor specificity for aldosterone depends on the presence of 11--hydroxysteroid dehydrogenase 2 [41]. The intracellular MR mediates sodium-water retention in renal epithelial cells of the distal nephron, stimulates fibrosis, apoptosis, and atherosclerosis in vascular smooth muscle cells (vSMCs) and promotes leukocyte adhesion, pro-thrombotic phenotype and epithelial–mesenchymal transition in endothelial cells [42].
The intracellular MR is also present in other non-epithelial tissues, acting in a 11--hydroxysteroid dehydrogenase 2-independent fashion [43]. In macrophages, MR activation promotes M1-phenotype differentiation, thus leading to galectin-3 secretion, fibroblast activation, and deposition of fibrous tissue [44]. In cardiomyocytes, MR usually acts as glucocorticoid receptor, and increases contractility, stimulates hypertrophy, and contributes to electrical remodeling [45].
While MR antagonists (MRAs) were first employed in clinical practice as potassium-sparing diuretics, they have been proven useful in cardiovascular diseases and in HF, mostly due to their antifibrotic and antihypertrophic actions [46]. Currently available molecules have either a steroidal (i.e., spironolactone and eplerenone) or non-steroidal structure (i.e., finerenone). The in-class and between-class differences mainly stand in the selectivity (rather than in the affinity) for MR, as only steroidal MRA can also bind to other steroids receptors. As the founder of this class, spironolactone has a similar structure to both aldosterone and progesterone, whereas eplerenone more specifically binds MR. This results in a reduced incidence of adverse drug reactions related to the binding to sexual hormones receptors [47]. Finerenone shows the highest specificity within this class, and is currently under a phase-III clinical trial evaluation for the treatment of HF [48].
MR blockade, as well as the use of ACE inhibitors and ARBs, has been associated with a rebound increase in circulating aldosterone, named the aldosterone breakthrough [49]. Although the mechanisms underlying this phenomenon are still to be clarified, the ACE-independent synthesis of RAAS effectors has been advocated.
Endothelin
Endothelin plays pleiotropic roles in the cardiovascular system. Synthesis of pre-pro-endothelin is stimulated by several neuro-hormones (i.e., Ang-II, norepinephrine), cytokines (i.e. interleukin-1), hypoxia, acidosis and shear stress [50]. The precursor is then cleaved by proteases into pro-endothelin, which is further processed into endothelin, the biologically active form, by the endothelin-converting enzyme [51].
Endothelin binds to receptors ET-A and ET-B, both expressed in heart and vessels. ET-A plays a major role on cardiomyocytes, mediating hypertrophy, fibrosis, and favoring the onset of arrhythmias; it also exerts a positive inotropic effect by increasing intracellular calcium concentration [52, 53]. In blood vessels, ET-A promotes fibrosis through fibroblast activation and mediates vasoconstriction in vSMCs via Gq-phospholipase C signaling [54]. Furthermore, it has been demonstrated that ET-A is regulated by complex G protein-coupled receptor kinase type 2-mediated phosphorylation that may increase its affinity for arrestins [55]. ET-B expression is higher in fibroblast than in cardiomyocytes, promoting fibrosis, apoptosis, and hypertrophy [56]. In the vasculature, ET-B is responsible for fibrosis, acting synergistically with ET-A, as well as for vasoconstrictive signals in vSMCs via protein kinase C [57].
Despite the role of endothelin in the progression of end-organ damage, many drugs antagonizing ET-A and/or ET-B (i.e., bosentan, sitaxentan) displayed no beneficial effects compared to placebo, while some others were shown to be harmful, both in the settings of acute and chronic HF [58–60].
Antidiuretic hormone
The antidiuretic hormone (ADH) pathway has been considered one of the leading pathophysiological drivers of HF, especially in advanced stages, when hyponatremia is more often observed [61]. Despite this assumption, the main clinical trials targeting ADH system have yielded controversial results, mainly with non-significant improvements in hard endpoints [62].
In physiological conditions, ADH is produced by the supraoptic and paraventricular nuclei in the hypothalamus and then stored in the neurohypophysis. Its release mainly depends on osmotic imbalance, sensed by specific receptors. In patients with HF, ADH secretion is also dependent on non-osmotic mechanisms, especially SNS and RAAS overactivation.
ADH acts on three types of receptors: V1a, V1b, V2 [63]. V1a signaling is mediated by Gq-PLC pathway, thus inducing vSMCs vasoconstriction, platelet aggregation, and myocyte modifications, such as activation of growth factors, synthesis of contractile proteins and positive inotropic effect. The binding of V1b causes an increased production of adrenocorticotropic hormone by the adenohypophysis [64]. Finally, V2 stimulation in the kidney increases the exposure of aquaporin 2 at the plasma membrane, which is in turn is responsible for a higher rate of free water reabsorption, plasma dilution, and hyponatremia [65].
Conivaptan is a non-selective, intravenous V1a and V2 antagonist, whereas tolvaptan is a selective V2 antagonist which has been shown to ameliorate serum sodium levels in acute and chronic HF [66, 67]. Both drugs target free water retention and have been proposed as second-line diuretics [68], whilst conivaptan has further antiremodeling properties. Nevertheless, both these molecules failed to significantly reduce mortality in clinical studies [69].
Natriuretic peptides
The natriuretic peptide system represents the main counterregulatory axis, with diuretic, natriuretic, vasodilative, and antifibrotic actions [70–72]. The main stimulus to the release of natriuretic peptides is the increase in cardiac wall tension. Atrial natriuretic peptide (ANP), produced mainly by atrial cardiomyocytes, is released following acute changes in atrial wall stress, whereas B-type natriuretic peptide (BNP) secretion is finely, transcriptionally regulated by a chronic overload of the left ventricle [73, 74]. Moreover, several cardiac (e.g. atrial fibrillation) or extracardiac co-factors (such as pulmonary comorbidities, renal function, age and body mass index) might affect circulating levels of natriuretic peptide [75].
Pro-ANP, cleaved by pre-pro-ANP, is a peptide precursor enzymatically processed by corin into the inactive fragment N-terminal (NT)-pro-ANP and into the active peptide ANP [76]. ANP release is promoted by a large number of damage systems, including endothelin, Ang-II, and ADH [77]. BNP is produced by the enzymatic cleavage of proBNP (derived from pre-proBNP) by corin and furin. BNP is released with the biologically inactive N-terminal fragment (NT-proBNP) in an equimolar fashion [78]. Both ANP and BNP can bind to two types of membrane receptors: natriuretic peptide receptor (NPR)-A, which is responsible for their biological actions, and NPR-C, which is involved in the internalization and the degradation of natriuretic peptides. BNP can further bind to NPR-B [79]. NPR-A and NPR-B stimulation increases the activity of guanylate cyclase (GC), which turns into an increase in cyclic guanosine monophosphate (cGMP) production and protein-kinase G activation [80]. Following protein kinase G activation, natriuretic peptides induce renal vasodilation, natriuresis, and diuresis via dilation of the afferent and constriction of the efferent arteriole, reduce sodium-water reabsorption and inhibit RAAS and ADH signaling pathways. Other targets include the increase in parasympathetic stimulation and the blunting of sympathetic activity, as well as the inhibition of fibroblasts, macrophages, pro-inflammatory cytokines, and pro-hypertrophic stimuli [71, 72, 77].
C-type natriuretic peptide (CNP) is produced by pre-proCNP following a double enzymatic cleavage in brain, endothelial cells, heart, fibroblasts, and macrophages [75, 81]. CNP binds to NPR-B and, by increasing cGMP levels, inhibits vSMCs proliferation, oxidized low-density lipoprotein accumulation in the arterial walls, endothelin release, phosphorylation of calmodulin kinase, and extracellular signal-regulated kinase [82].
Plasma levels of natriuretic peptides are dependent on both synthesis and clearance processes. NPR-C is the third isoform of natriuretic peptides receptors, whose binding determines the internalization of the ligand-receptor complex and the ligand degradation [83]. Neprilysin is a zinc-dependent endopeptidase, which is able to degrade all natriuretic peptides, although with a higher affinity for ANP than for BNP [84]. Neprilysin has also other substrates, including Ang-II, glucagon, and bradykinin [85].
Despite their important counterbalancing role, natriuretic peptides can fully oppose detrimental drivers only at earlier stages of disease. Along with HF progression, multiple derangements in natriuretic peptide system occur, including a reduced expression of corin and furin leading to low biologically active peptides, an increased dipeptidyl-peptidase IV activity causing the rise in circulating levels of truncated pro-BNP and BNP, a downregulation of NPR-A and NPR-B, a desensitization of NPR-A/GC system and an increase NPR-C-mediated clearance [86].
The first attempt in targeting this system was to administer exogenous natriuretic peptides. Despite initial optimism, the largest trial on nesiritide (a recombinant form of BNP) failed to show a difference in mortality or re-hospitalization rates versus placebo, and disclosed poor tolerability (e.g., hypotension and worsening renal function), leading to approval withdrawal [87, 88]. More stable molecules have been developed and are currently undergoing clinical tests. M-ANP, a natriuretic peptide analogue, was shown to improve natriuresis and glomerular filtration rate as compared with endogenous ANP [89].
Many attempts have been made to test neprilysin inhibitors in HF, but no molecule proved to be effective when used alone. This has been attributed to a blunt in Ang-II breakdown by reduced neprilysin activity, increasing Ang-II concentrations. Therefore, neprilysin inhibitors were first tested in combination with ACE inhibitors, as omapatrilat [90]. This combination proved harmful. In fact, both ACE and neprilysin are responsible for the degradation of bradykinin; hence, their concurrent inhibition led to the rise of bradykinin levels with increased risk of angioedema [91]. Conversely, the association of neprilysin inhibitor and ARB proved effective and safe, and represents the only available neurohormonal modulator to date providing both antagonism of RAAS pathway and potentiation of the natriuretic peptide axis. The Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM) trial was the first study to demonstrate the prognostic benefits of a neprilysin inhibitor (sacubitril) combined with the ARB valsartan over enalapril in a large population with HFrEF [92]. Still, as assessed in the Prospective Comparison of angiotensin receptor–neprilysin inhibitor with ARB Global Outcomes in HF with Preserved Ejection Fraction (PARAGON-HF) trial, the use of sacubitril/valsartan missed the composite primary endpoint of reducing hospitalization and death in HFpEF [93].
Novel therapeutic targets
NO synthase and guanylate cyclase
NO is highly volatile molecule with a short half-life that mediates vasodilation in coronary and non-coronary districts and has positive effects on the myocardium [94]. Once NO is produced in the endothelium and in the endocardium, it spreads to the vSMCs and the myocardium and is responsible for soluble GC activation [95]. The resulting cGMP causes a decrease in intracellular free calcium levels, promoting relaxation, and is then degraded by phosphodiesterase type 5 [95–97]. In HF, NO production is significantly reduced because of multiple mechanisms including downregulation of endothelial NO synthase and inactivation by ROS, especially superoxide anions [98]. This is in turn responsible for vasoconstriction, increased muscular, and vascular stiffness and adverse remodeling [96, 99].
A broad range of molecules targeting the NO-GC system has been developed. Phosphodiesterase 5 inhibitors (such as sildenafil) reduce cGMP degradation [100]. Other drugs directly interact with the soluble form of GC and are classified into activators (cinaciguat) and stimulators (vericiguat and riociguat). GC activators target the oxidized, malfunctioning, NO-unresponsive enzyme by mimicking NO itself. Conversely, GC stimulators act on the reduced, functioning isoform, enhancing soluble GC activity in the presence of the endogenous ligand [101]. Benefits of The SOluble Guanylate Cyclase stimulatoR in heArT failurE patientS With REDUCED EF (SOCRATES-REDUCED) trial showed a reduction in NT-proBNP levels with vericiguat in patients with HFrEF [102, 103]. In the recent Vericiguat Global Study in Subjects with Heart Failure with Reduced Ejection Fraction (VICTORIA) trial, vericiguat reduced the composite end-point of death from any cause or hospitalization for HF compared to placebo among patients with HF at high risk of decompensation [104].
SGLT2 inhibitors
Sodium glucose cotransporter 2 (SGLT2) inhibitors were specifically designed for the management of type 2 diabetes mellitus, as they promote renal glucose excretion by inhibiting reabsorption [105]. Nonetheless, their effects go far beyond their role of glucose-lowering drugs, as they have been proved to be effective in the context of HFrEF, even in the absence of diabetes. Data from large randomized clinical trials with empagliflozin (EMPA-REG, Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes) [106] and dapagliflozin (DECLARE–TIMI 58, Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes) [107] demonstrated a reduction in hospitalization for HF, in cardiovascular and all-cause mortality, in atherosclerosis-related events and in the progression of chronic kidney disease in large cohorts of diabetic patients. These data have been empowered by the results of the EMPEROR-Reduced (EMPagliflozin outcomE tRial in Patients With chrOnic heaRt Failure With Reduced Ejection Fraction) [108] and the DAPA-HF (Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction) [109] trials, which demonstrated a lower risk of cardiovascular death and HF hospitalization with empagliflozin and dapagliflozin as compared to placebo, irrespective of the presence of diabetes mellitus. Moreover, a slower decline in renal function was observed in those treated with empagliflozin. This may infer that the effects on cardiovascular outcomes are at least partially mediated by nephroprotection. As a support, the Dapagliflozin in Patients with Chronic Kidney Disease (DAPA-CKD) [110] demonstrated that dapagliflozin reduced the risk of worsening renal function or death from cardiovascular or kidney disease in patients with chronic kidney disease with and without type 2 diabetes mellitus.
The mechanisms underlying the beneficial effects of SGLT2 inhibitors in HF remain to be elucidated, although some hypotheses have been formulated. As recently reported, SGLT2 inhibitors reduce oxidative stress, inflammation, and fibrosis in the whole cardiovascular system, and mitigate glomerular hypertension, thus preventing shear stress-related renal damage [111–114]. Moreover, they reduced cardiac cytosolic Na+ and Ca2+ concentrations through inhibition of Na+/H+ exchanger, promote weight loss by inducing a fasting-like state with increased production of ketones, an advantageous substrate for the failing heart [115]. Finally, SGLT2 inhibitors may blunt sympathetic activation, as they reduce renal and cardiac levels of tyrosine hydroxylase and norepinephrine, and their hypotensive effect is maintained regardless of renal function worsening [116].
Myocardial contractility
So far, inotropic agents have been predominantly employed in the setting of acute HF. Indeed, molecules most commonly used in clinical practice are burdened by a high rate of adverse effects, especially in end-stage patients, and their use should be limited to the shortest time possible. First-generation inotropes (such as adrenergic agonists, e.g., norepinephrine) are affected by a relevant pro-arrhythmic burden, due to increased oxygen consumption and to the afterdepolarizations caused by calcium overload [117]. With these premises, they are not recommended in the absence of hypotension or hypoperfusion [4]. Glycosides can be used also in the setting of chronic HF, even if they are not associated with improved survival [118]. Levosimendan mainly acts as a calcium-sensitizer, has a more favorable safety profile as compared with adrenergic agonists, and has been shown to have beneficial effects in acute HF [119]. Furthermore, encouraging results came from the Levosimendan Intermittent administration in Outpatients: effects on Natriuretic peptides in advanced chronic HEART failure (LION-HEART) trial, where the intermittent use of levosimendan in patients with advanced HFrEF was associated to a reduction in NT-proBNP levels and in the rate of hospitalization [120].
More recently, new molecules named “myosin motor activators” have been developed, the first-in-class drug being omecamtiv mecarbil. This drug enhances the ATPase activity of myosin, thus favoring the formation and stabilization of cardiomyocyte cross-bridges. This results in an increased force of contraction and in a prolongation of the systolic ejection time, without interfering in calcium transients nor in the velocity of contraction [121, 122]. As compared to “conventional” inotropes, omecamtiv mecarbil improves systolic function without affecting the intracellular concentrations of cAMP and calcium, nor increasing oxygen consumption and ATP demand [123]. Phase II and III trials showed promising results in terms of increase in stroke volume and reduction in end-systolic and end-diastolic diameters. Recently, the GALACTIC-HF trial (A Double-blind, Randomized, Placebo-controlled, Multicenter Study to Assess the Efficacy and Safety of Omecamtiv Mecarbil on Mortality and Morbidity in Subjects With Chronic Heart Failure With Reduced Ejection Fraction) has shown that use of omecamtiv mecarbil was associated with a lower incidence of a composite of a HF event or death from cardiovascular causes compared to placebo [124, 125].
Mitochondria and metabolism
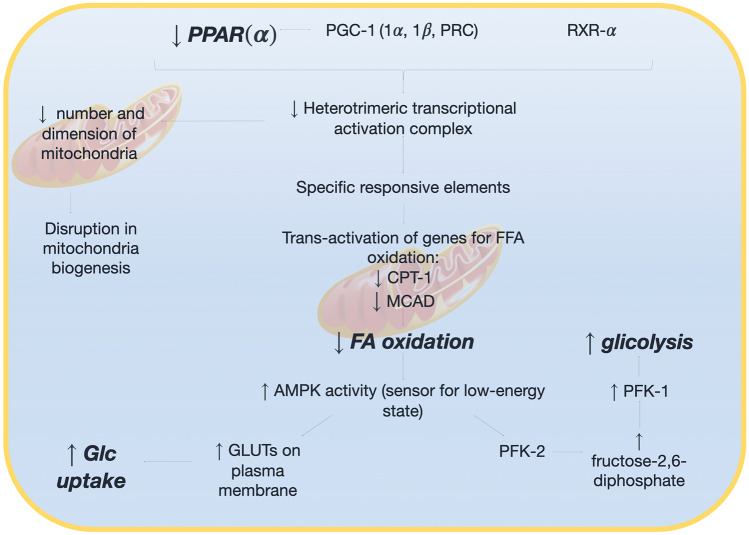
The resting healthy myocardium drains 60–70% of energy from fatty acid oxidation, whereas energy is mostly obtained from glucose catabolism in post-prandial phase or during physical exercise [126]. Glucose and lipid metabolism are tightly inversely regulated in myocytes according to the Randle cycle [127]. A shift from free fatty acids to glucose utilization has been observed in HF [128]. This mechanism plays an adaptive role, since free fatty acid oxidation requires 10–15% more oxygen to obtain the same ATP levels than glucose. The reduction in peroxisome proliferator-activated receptor (PPAR)- leads to reduced a number and dimension of mitochondria and a reduced expression of proteins involved in -oxidation [129]. Moreover, the increased activity of AMP-kinase, a sensor for low-energy state, promotes the expression of glucose transporters on the plasma membrane and the activity of phosphofructokinase-2, thus increasing glycolysis rate [130] (Fig. 4). Adrenergic activation leads to increased lipolysis from adipose tissue and reactive oxygen species (ROS) production, with an impairment of cell respiration, an upregulation of mitochondrial expression of uncoupling proteins 2 and 3 and insulin resistance [131, 132], finally inhibiting the metabolic switch in the heart.
Fig. 4.
Metabolic phenotype of heart failure. The reduction in peroxisome proliferator-activated receptor alpha (PPAR-) leads to a decreased expression of enzymes for fatty acid oxidation. This in turn stimulates glycolysis and glucose uptake via the increase of adenosine monophosphate kinase. AMPK adenosine monophosphate kinase; CPT carnitine palmitoyl transferase; FA fatty acid; Glc glucose; GLUT glucose transporter; MCAD medium-chain acyl-CoA dehydrogenase; PFK phosphofructokinase; PGC peroxisome proliferator-activated receptor gamma coactivator 1-alpha; PPAR peroxisome proliferator-activated receptor; RXR retinoid-X receptor
PPAR- antagonists might favor this glycolytic shift and improve myocardial energetics, but their clinical utility remains to be established [133]. Trimetazidine, a second-line antianginal drug, promotes a shift to glucose metabolism by inhibiting the last reaction of free fatty acid oxidation, catalyzed by acetyl CoA C-acyltransferase [134]. Growing evidence supports its efficacy in chronic HF, even if most of the available data come from meta-analyses of retrospective studies [135–137].
Mitochondrial function also relies on membrane stability, mainly dependent on cardiolipin and coenzyme Q10 [138, 139]. Elamipretide, a cardiolipin-stabilizer, has been first tested on a canine model of HF showing improvements in LVEF and reduction in circulating levels of NT-proBNP, tumor necrosis factor- and C-reactive protein. Although no significant reduction in biomarkers emerged from studies in humans, some positive effects on reverse remodeling were observed [140, 141]. Though, a phase-II clinical trial showed no improvement in left ventricular end-systolic volume after a 4-week treatment [142]. Coenzyme Q10 promotes the synthesis of ATP in the mitochondria by participating in redox reactions within the electron transport chain. Treatment with coenzyme Q10, studied in The Effect of Coenzyme Q10 on Morbidity and Mortality in Chronic Heart Failure (Q-SYMBIO) study, was associated with a lower rate of mortality for both cardiovascular- and all-cause mortality and with a reduced rate of hospitalization. However, studies on larger cohorts are still lacking [143].
The impairment in cellular respiration is also associated to enhanced oxidative stress and inflammation. Patients with chronic HF show higher levels of serum biomarkers associated with inflammation, including high-sensitivity C-reactive protein, interleukin-1β, interleukin-6, inteleukin-8, and tumor necrosis factor [144]. An excess in ROS can modify highly expressed proteins in myocytes, including protein-kinases, myofilaments and other proteins involved in excitation–contraction coupling [145]. In a cohort of high-risk coronary artery disease patients, interleukin-1β blockade was associated with significant reduction in ischemic events and cardiovascular mortality [146]. A post hoc analysisalso detected a reduction in the rate of hospitalization due to HF [147].
Treatments targeting hypertrophy and fibrosis
Beyond antagonists of renin–angiotensin–aldosterone system and beta-blockers that affect cellular hypertrophy [148], current efforts are focusing on the anti-hypertrophic effects of molecules acting directly on the cardiomyocyte, targeting crucial signaling cascades that alter gene expression, protein function, and red149ox imbalance (Fig. 5). These agents include histone deacetylase inhibitors, a wide spectrum of pro-hypertrophic microRNAs and several other small molecules (such as rapamycin, inhibitors of Rho kinase) [149–151].
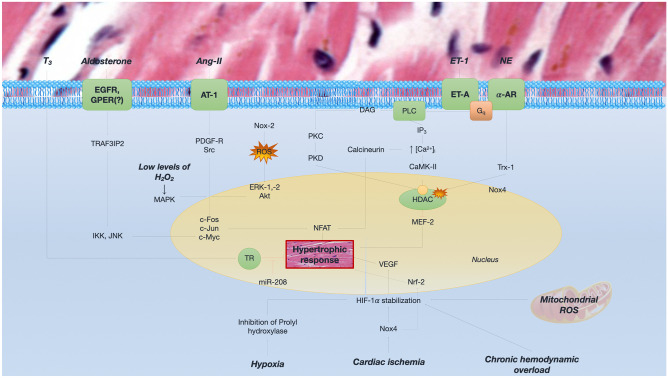
Fig. 5.
Main molecular pathways for cardiac hypertrophy. Hypertrophy may be the consequence of both hemodynamic (chronic overload) and non-hemodynamic factors, namely neuroendocrine systems derangement and reduction in oxygen myocardial delivery. Ang angiotensin; AR adrenergic receptor; AT angiotensin receptor; DAG diacyl-glycerol; EGFR epidermal growth factor receptor; ERK extracellular signal-regulated kinase; ET endothelin; ET-A endothelin receptor A; H2O2 hydrogen peroxide; HDAC histone deacetylase; HIF hypoxia inducible factor; IKK inhibitor of nuclear factor kappa-B kinase; IP3 inositol triphosphate; JNK c-Jun N-terminal kinase; MEF myocyte enhancer factor; NE norepinephrine; NFAT nuclear factor of activated T-cell; Nox NADPH oxidase; PDGF-R receptor of platelet-derived growth factor; PKC protein kinase C; PKD protein kinase D; PLC phospholipase C; Src Rous sarcoma protooncogene; TR thyroid receptor; Trx1 thioredoxin 1; VEGF vascular endothelial growth factor
In contrast to the traditional view in which fibrosis is regarded as a secondary phenomenon, recent evidences indicate a primary role for cardiac fibroblast activity in myocardial disease. Cardiac fibrosis is linked to cardiac dysfunction, increased risk of arrhythmia, and poor outcomes [152]. Despite the use of ACE inhibitors and MRAs, a residual fibrotic activity is still observed in HF. Novel antifibrotic agents are currently under investigation, specifically targeting connective tissue growth factors (e.g., TGF- by pirfenidone), galectin-3 (e.g., by antisense RNA), matrix metalloproteinases, and cell reprogramming via non-coding RNAs [153].
HFpEF: a therapeutic challenge
Unlike in HFrEF, neurohormonal antagonists did not reduce mortality in patients affected by HFpEF. However, when excluding cohorts from Georgia and Russia in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial, the use of spironolactone significantly reduced mortality in this setting [154]. The finding that aldosterone levels are increased in HFpEF may provide a pathophysiological basis for the use of MRA in HFpEF [155].
To date, treatment of risk factors and underlying disease is the only beneficial therapeutic approach for patients with HFpEF. Notably, tafamidis, a pharmacological transthyretin-stabilizer, improved outcome of patients affected by transthyretin-related cardiac amyloidosis, a progressively more recognized clinical phenotype of HFpEF [156].
Future perspectives
Novel therapeutic options are emerging for the treatment of HF. Some of them address well-known pathophysiological mechanisms, such as neurohormonal deregulation and the NO-GC-cGMP system; others, such as SGLT2 inhibitors, hold effects on the cardiovascular system that are still to be fully clarified. Several emerging approaches target cardiac metabolism, inflammation, and remodeling. Specific transient receptor potential cation channel subfamily V (TRPV)-4 blocker, GSK2798745, has shown promising results in a model of chronic HF, possibly by interfering with transforming growth factor (TGF) β-1-induced activation of myofibroblasts [157].
In the future of HF therapy, stem cells, micro-RNA, and epigenetics are likely to become novel cornerstone and to allow a tailored approach. Micro-RNAs have been thoroughly studied in the processes of hypertrophy, apoptosis, and fibrosis. As an example, micro-RNAs-34 family encloses many subtypes of micro-RNAs whom are involved in fibroblast survival and growth factors secretion (i.e., micro-RNA-21) [158] and in the activity of calmodulin kinase (i.e., micro-RNA-1) [159]. As shown in the Randomized Clinical Trial of Intravenous Infusion Umbilical Cord Mesenchymal Stem Cells on Cardiopathy (RIMECARD), the use of umbilical cord stem cells was safe in patients with stable HFrEF under optimal medical treatment, and improvements in LVEF, functional status and quality of life were observed [160].
Conclusions
HF is a complex, multisystemic syndrome with a dramatic social and economic impact. Since decades, HF therapeutics have been following the interpretative pathophysiological models. After initial strategies targeting inotropism and congestion, and neurohormonal antagonism addressing dysregulation of peripheral feedbacks, novel therapeutic approaches have been recently developed, directed to the heart muscle. Drugs acting at a second-messenger levels, such as vericiguat, as well as other drugs acting on myocardial energetics and mitochondrial function, including elamipretide or omecamtiv mecarbil may then represent in the next future some additive, synergistic tools to improve patient outcome. Effective, evidence-based drugs from the fields of stem cells, micro-RNAs, and epigenetic remodulation are awaited in the next decades. In the next future, individual profiling and dissection of the activation of specific pathophysiological pathways of organ damage may represent the base for a tailored treatment of HF.
Abbreviations
- ACE
Angiotensin-converting enzyme
- ADH
Antidiuretic hormone/arginine-vasopressin
- Ang
Angiotensin
- ANP
Atrial natriuretic peptide
- BNP
B-type natriuretic peptide
- cAMP
Cyclic adenosine monophosphate
- cGMP
Cyclic guanosine monophosphate
- CNP
C-type natriuretic peptide
- GC
Guanylate cyclase
- HF
Heart failure
- HFmrEF
Heart failure with mid-range ejection fraction
- HFpEF
Heart failure with preserved ejection fraction
- HFrEF
Heart failure with reduced ejection fraction
- MAPK
Mitogen-activated protein kinase
- MR
Mineralocorticoid receptor
- MRA
Mineralocorticoid receptor antagonists
- NADPH
Nicotinamide-adenine dinucleotide phosphate
- NO
Nitric oxide
- NPR
Natriuretic peptide receptor
- NT
N-terminal
- PPAR
Peroxisome proliferator-activated receptor
- RAAS
Renin-angiotensin-aldosterone system
- SGLT
Sodium glucose cotransporter
- TGF
Transforming growth factor
- TRPV-4
Transient receptor potential cation channel subfamily V member 4
- vSMCs
Vascular smooth muscle cells
Author contribution
Dr. Ghionzoli and Dr. Vergaro conceived the paper. Dr. Ghionzoli performed the literature search, drafted the work and prepared figures. Dr. Vergaro contributed to draft and revise the work. Dr. Gentile, Dr. Del Franco, Dr. Castiglione, Dr. Aimo, Dr. Giannoni, Dr. Burchielli, Prof. Cameli, and Prof. Emdin critically revised the work.
Funding
Open access funding provided by Scuola Superiore Sant'Anna within the CRUI-CARE Agreement.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93:1137–1146. doi: 10.1136/hrt.2003.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mann DL, Bristow MR. Mechanisms and models in heart failure: the biomechanical model and beyond. Circulation. 2005;31(111):2837–2849. doi: 10.1161/CIRCULATIONAHA.104.500546. [DOI] [PubMed] [Google Scholar]
- 3.Packer M. The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol. 1992;20:248–254. doi: 10.1016/0735-1097(92)90167-l. [DOI] [PubMed] [Google Scholar]
- 4.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Rev Esp Cardiol (Engl Ed) 2016;69:1167. doi: 10.1016/j.rec.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Maggioni AP, Dahlström U, Filippatos G, et al (2013) EURObservational research programme: Regional differences and 1-year follow-up results of the heart failure pilot survey (ESC-HF Pilot). Eur J Heart Fail. 15:808–817. 10.1093/eurjhf/hft050 [DOI] [PubMed]
- 6.Ilieșiu AM, Hodorogea AS (2018) Treatment of heart failure with preserved ejection fraction. Adv Exp Med Biol. 1067:67–87. 10.1007/5584_2018_149 [DOI] [PubMed]
- 7.Spyer KM. Annual review prize lecture. Central nervous mechanisms contributing to cardiovascular control. J Physiol. 1994;474:1–19. doi: 10.1113/jphysiol.1994.sp019997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.La Rovere M, Pinna G, Maestri R, Sleight P (2013) Clinical value of baroreflex sensitivity. Netherlands Hear J. 21:61–63. 10.1007/s12471-012-0349-8 [DOI] [PMC free article] [PubMed]
- 9.Floras JS (2009) Sympathetic nervous system activation in human heart failure: clinical implications of an updated model. J Am Coll Cardiol. 54:375–385. 10.1016/j.jacc.2009.03.061 [DOI] [PubMed]
- 10.Feldman DS, Carnes CA, Abraham WT, Bristow MR (2005) Mechanisms of disease: beta-adrenergic receptors—alterations in signal transduction and pharmacogenomics in heart failure. Nat Clin Pract Cardiovasc Med 2:475–483. 10.1038/ncpcardio0309 [DOI] [PubMed]
- 11.MacLennan DH, Kranias EG (2003) Phospholamban: a crucial regulator of cardiac contractility. Nat. Rev. Mol. Cell Biol. 4:566–577. 10.1038/nrm1151 [DOI] [PubMed]
- 12.Lymperopoulos A, Rengo G, Koch WJ. Adrenergic nervous system in heart failure: pathophysiology and therapy. Circ Res. 2013;113:739–753. doi: 10.1161/CIRCRESAHA.113.300308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dodge-Kafka KL, Soughaver J, Pare GC, et al (2005) The protein kinase A anchoring protein mAKAP coordinates two integrated cAMP effector pathways. Nature 437:574–578. 10.1038/nature03966 [DOI] [PMC free article] [PubMed]
- 14.Dargie HJ, Lechat P. The cardiac insufficiency bisoprolol study II (CIBIS-II): A randomised trial. Lancet. 1999;353:9–13. doi: 10.1016/S0140-6736(05)74355-5. [DOI] [PubMed] [Google Scholar]
- 15.Kumakura S, Oshima T. Effects of beta blockers on cardiac function and myocardial oxygen consumption in the isolated supported heart preparation of the dog. Jpn Heart J. 1975;16:592–602. doi: 10.1536/ihj.16.592. [DOI] [PubMed] [Google Scholar]
- 16.Prichard BN, Walden RJ. The syndrome associated with the withdrawal of beta-adrenergic receptor blocking drugs. Br J Clin Pharmacol. 1982;13:337S–343S. doi: 10.1111/j.1365-2125.1982.tb01938.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dendorfer A, Thornagel A, Raasch W, Grisk O, Tempel K, Dominiak P. Angiotensin II induces catecholamine release by direct ganglionic excitation. Hypertension. 2002;40:348–354. doi: 10.1161/01.hyp.0000028001.65341.aa. [DOI] [PubMed] [Google Scholar]
- 18.Urata H, Healy B, Stewart RW, Bumpus FM, Husain A. Angiotensin II-forming pathways in normal and failing human hearts. Circ Res. 1990;66:883–890. doi: 10.1161/01.res.66.4.883. [DOI] [PubMed] [Google Scholar]
- 19.Peters J, Wanka J, Peters B, Hoffmann S. A renin transcript lacking exon 1 encodes for a non-secretory intracellular renin that increases aldosterone production in transgenic rats. J Cell Mol Med. 2008;12:1229–1237. doi: 10.1111/j.1582-4934.2008.00132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peters J. Cytosolic (pro)renin and the matter of intracellular renin actions. Frontiers in Bioscience. 2013;S5:198–205. doi: 10.2741/s366. [DOI] [PubMed] [Google Scholar]
- 21.Berk BC, Corson MA. Angiotensin II signal transduction in vascular smooth muscle: role of tyrosine kinases. Circ Res. 1997;80:607–616. doi: 10.1161/01.res.80.5.607. [DOI] [PubMed] [Google Scholar]
- 22.Ruiz-Ortega M, Lorenzo O, Ruperez M, et al. Angiotensin II activated nuclear transcription factor kappaB through AT(1) and AT(2) in vascular smooth muscle cells: molecular mechanisms. Circ Res. 2000;86:1266–1272. doi: 10.1161/01.res.86.12.1266. [DOI] [PubMed] [Google Scholar]
- 23.Zhang H, Schmeisser A, Garlichs CD, et al. Angiotensin II-induced superoxide anion generation in human vascular endothelial cells: role of membrane-bound NADH/NADPH-oxidases. Cardiovasc Res. 1999;44:215–222. doi: 10.1016/s0008-6363(99)00183-2. [DOI] [PubMed] [Google Scholar]
- 24.Bauersachs J, Bouloumié A, Fraccarollo D, Hu K, Busse R, Ertl G. Endothelial dysfunction in chronic myocardial infarction despite increased vascular endothelial nitric oxide synthase and soluble guanylate cyclase expression: role of enhanced vascular superoxide production. Circulation. 1999;100:292–298. doi: 10.1161/01.cir.100.3.292. [DOI] [PubMed] [Google Scholar]
- 25.Keidar S, Kaplan M, Hoffman A, Aviram M. Angiotensin II stimulates macrophage-mediated oxidation of low density lipoproteins. Atherosclerosis. 1995;115:201–215. doi: 10.1016/0021-9150(94)05514-j. [DOI] [PubMed] [Google Scholar]
- 26.Liu YH, Yang XP, Sharov VG, et al. Effects of angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor antagonists in rats with heart failure. Role of kinins and angiotensin II type 2 receptors. J Clin Invest. 1997;99:1926–1935. doi: 10.1172/JCI119360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Misbah H, Fazli RA. Hypertension regulating angiotensin peptides in the pathobiology of cardiovascular disease. Clin Exp Hypertens. 2018;40:344–352. doi: 10.1080/10641963.2017.1377218. [DOI] [PubMed] [Google Scholar]
- 28.Sampaio WO, Nascimento AA, Santos RA. Systemic and regional hemodynamic effects of angiotensin-(1–7) in rats. Am J Physiol Heart Circ Physiol. 2003;284:H1985–H1994. doi: 10.1152/ajpheart.01145.2002. [DOI] [PubMed] [Google Scholar]
- 29.Pörsti I, Bara AT, Busse R, Hecker M. Release of nitric oxide by angiotensin-(1–7) from porcine coronary endothelium: implications for a novel angiotensin receptor. Br J Pharmacol. 1994;111:652–654. doi: 10.1111/j.1476-5381.1994.tb14787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mercure C, Yogi A, Callera GE, et al. Angiotensin (1–7) blunts hypertensive cardiac remodeling by a direct effect on the heart. Circ Res. 2008;103:1319–1326. doi: 10.1161/CIRCRESAHA.108.184911. [DOI] [PubMed] [Google Scholar]
- 31.Ferreira AJ, Santos RA, Almeida AP. Angiotensin-(1–7) cardioprotective effect in myocardial ischemia/reperfusion. Hypertension. 2001;38:665–668. doi: 10.1161/01.hyp.38.3.665. [DOI] [PubMed] [Google Scholar]
- 32.Iwata M, Cowling RT, Gurantz D, et al. Angiotensin-(1–7) binds to specific receptors on cardiac fibroblasts to initiate antifibrotic and antitrophic effects. Am J Physiol Heart Circ Physiol. 2005;289:H2356–H2363. doi: 10.1152/ajpheart.00317.2005. [DOI] [PubMed] [Google Scholar]
- 33.The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet. 1993;342:821–828. [PubMed] [Google Scholar]
- 34.Konstam MA, Rousseau MF, Kronenberg MW, et al. Effects of the angiotensin converting enzyme inhibitor enalapril on the long-term progression of left ventricular dysfunction in patients with heart failure. Circulation. 1992;86:431–438. doi: 10.1161/01.cir.86.2.431. [DOI] [PubMed] [Google Scholar]
- 35.SOLVD Investigators, Yusuf S, Pitt B, Davis CE, Hood WB Jr, Cohn JN (1992) Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med. 327:685–691. 10.1056/NEJM199209033271003 [DOI] [PubMed]
- 36.Liu H, Luo H, Wang S, Zhang C, Hao J, Gao C (2017) Aliskiren for heart failure: a systematic review and meta-analysis of randomized controlled trials. Oncotarget. 8:88189–88198. 10.18632/oncotarget.21112 [DOI] [PMC free article] [PubMed]
- 37.Tomoya H, Satoshi N, Toshihiro Y. TAK-272 (imarikiren), a novel renin inhibitor, improves cardiac remodeling and mortality in a murine heart failure model. Plos One. 2005;13:e0202176. doi: 10.1371/journal.pone.0202176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N Engl J Med. 1986;314:1547–1552. doi: 10.1056/NEJM198606123142404. [DOI] [PubMed] [Google Scholar]
- 39.Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049–2057. doi: 10.1056/NEJMoa042934. [DOI] [PubMed] [Google Scholar]
- 40.Grossmann C, Benesic A, Krug AW, et al. Human mineralocorticoid receptor expression renders cells responsive for nongenotropic aldosterone actions. Mol Endocrinol. 2005;19:1697–1710. doi: 10.1210/me.2004-0469. [DOI] [PubMed] [Google Scholar]
- 41.Lombes M, Alfaidy N, Eugene E, Lessana A, Farman N, Bonvalet JP. Prerequisite for cardiac aldosterone action. Mineralocorticoid receptor and 11 beta-hydroxysteroid dehydrogenase in the human heart. Circulation. 1995;92:175–182. doi: 10.1161/01.cir.92.2.175. [DOI] [PubMed] [Google Scholar]
- 42.Caprio M, Newfell BG, la Sala A, et al. Functional mineralocorticoid receptors in human vascular endothelial cells regulate intercellular adhesion molecule-1 expression and promote leukocyte adhesion. Circulation Research. 2008;102:1359–1367. doi: 10.1161/CIRCRESAHA.108.174235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rickard AJ, Morgan J, Tesch G, Funder JW, Fuller PJ, Young MJ Deletion of mineralocorticoid receptors from macrophages protects against deoxycorticosterone/salt-induced cardiac fibrosis and increased blood pressure. Hypertension. 2009;54:537–543. doi: 10.1161/HYPERTENSIONAHA.109.131110. [DOI] [PubMed] [Google Scholar]
- 44.Azibani F, Benard L, Schlossarek S, et al. Aldosterone inhibits antifibrotic factors in mouse hypertensive heart. Hypertension. 2012;59:1179–1187. doi: 10.1161/HYPERTENSIONAHA.111.190512. [DOI] [PubMed] [Google Scholar]
- 45.Ouvrard-Pascaud A, Sainte-Marie Y, Bénitah JP, et al. Conditional mineralocorticoid receptor expression in the heart leads to life-threatening arrhythmias. Circulation. 2005;111:3025–3033. doi: 10.1161/CIRCULATIONAHA.104.503706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Farquharson CA, Struthers AD. Spironolactone increases nitric oxide bioactivity, improves endothelial vasodilator dysfunction and suppresses vascular angiotensin I/angiotensin II conversion in patients with chronic heart failure. Circulation. 2000;101:594–597. doi: 10.1161/01.cir.101.6.594. [DOI] [PubMed] [Google Scholar]
- 47.Ménard J. The 45-year story of the development of an antialdosterone more specific than spironolactone. Mol Cell Endocrinol. 2004;217:45–52. doi: 10.1016/j.mce.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 48.Pitt B, Anker SD, Böhm M, et al. Rationale and Design of MinerAlocorticoid Receptor Antagonist Tolerability Study-Heart Failure (ARTS-HF): a randomized study of finerenone vs. eplerenone in patients who have worsening chronic heart failure with diabetes and/or chronic kidney disease. Eur J Heart Fail. 2015;17:224–232. doi: 10.1002/ejhf.218. [DOI] [PubMed] [Google Scholar]
- 49.Vergaro G, Fatini C, Sticchi E, et al. Refractory hyperaldosteronism in heart failure is associated with plasma renin activity and angiotensinogen polymorphism. J Cardiovasc Med (Hagerstown) 2015;16:416–422. doi: 10.2459/JCM.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 50.Miyauchi T, Masaki T. Pathophysiology of endothelin in the cardiovascular system. Annu Rev Physiol. 1999;61:391–415. doi: 10.1146/annurev.physiol.61.1.391. [DOI] [PubMed] [Google Scholar]
- 51.Kaddoura S, Firth JD, Boheler KR, Sugden PH, Poole-Wilson PA. Endothelin-1 is involved in norepinephrine-induced ventricular hypertrophy in vivo. Acute effects of bosentan, an orally active, mixed endothelin ETA and ETB receptor antagonist. Circulation. 1996;93:2068–2079. doi: 10.1161/01.cir.93.11.2068. [DOI] [PubMed] [Google Scholar]
- 52.Duru F, Barton M, Lüscher TF, Candinas R. Endothelin and cardiac arrhythmias: do endothelin antagonists have a therapeutic potential as antiarrhythmic drugs? Cardiovasc Res. 2001;49:272–280. doi: 10.1016/s0008-6363(00)00263-7. [DOI] [PubMed] [Google Scholar]
- 53.Teerlink JR. Endothelins: pathophysiology and treatment implications in chronic heart failure. Curr Heart Fail Rep. 2005;2:191–197. doi: 10.1016/s0008-6363(00)00263-7. [DOI] [PubMed] [Google Scholar]
- 54.Berk BC. Vascular smooth muscle growth: autocrine growth mechanisms. Physiol Rev. 2001;81:999–1030. doi: 10.1152/physrev.2001.81.3.999. [DOI] [PubMed] [Google Scholar]
- 55.Morris GE, Nelson CP, Standen NB, Challiss RA, Willets JM. Endothelin signalling in arterial smooth muscle is tightly regulated by G protein-coupled receptor kinase 2. Cardiovasc Res. 2010;85:424–433. doi: 10.1093/cvr/cvp310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mayet J, Hughes A. Cardiac and vascular pathophysiology in hypertension. Heart. 2003;89:1104–1109. doi: 10.1136/heart.89.9.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gray GA, Löffler BM, Clozel M. Characterization of endothelin receptors mediating contraction of rabbit saphenous vein. Am J Physiol. 1994;266:H959–H966. doi: 10.1152/ajpheart.1994.266.3.H959. [DOI] [PubMed] [Google Scholar]
- 58.Coletta AP, Cleland JGF. Clinical trials update: highlights of the Scientific Sessions of the XXIII Congress of the European Society of Cardiology— WARIS II, ESCAMI, PAFAC, RITZ-1 and TIME. Eur J Heart Fail. 2001;3:747–750. doi: 10.1016/s1388-9842(01)00210-0. [DOI] [PubMed] [Google Scholar]
- 59.Packer M, Caspi A, Charlon V. Multicenter, double-blind, placebo-controlled study of long-term endothelin blockade with bosentan in chronic heart failure: results of the REACH-1 trial. Circulation. 1998;98:S12. [Google Scholar]
- 60.Fonarow GC. Oral endothelin antagonist worsens clinical status in chronic heart failure. Best of the ACC Scientific Session. Rev Cardiovasc Med. 2001;2:144–145. [Google Scholar]
- 61.Ron M. Oren Hyponatremia in Congestive Heart Failure. Am J Cardiol. 2005;95:2B–7B. doi: 10.1016/j.amjcard.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 62.Vishram-Nielsen JK, Gustafsson F. Vasopressin and vasopressin antagonists in heart failure. Handb Exp Pharmacol. 2017;243:307–328. doi: 10.1007/164_2017_28. [DOI] [PubMed] [Google Scholar]
- 63.Goldsmith SR. The role of vasopressin in congestive heart failure. Cleve Clin J Med. 2006;73:S19–S23. doi: 10.3949/ccjm.73.suppl_3.s19. [DOI] [PubMed] [Google Scholar]
- 64.Lee CR, Watkins ML, Patterson JH, et al. Vasopressin: a new target for the treatment of heart failure. Am Heart J. 2003;146:9–18. doi: 10.1016/S0002-8703(02)94708-3. [DOI] [PubMed] [Google Scholar]
- 65.Goldsmith SR, Francis GS, Cowley AW, Jr, Levine TB, Cohn JN. Increased plasma arginine vasopressin levels in patients with congestive heart failure. J Am Coll Cardiol. 1983;1:1385–1390. doi: 10.1016/s0735-1097(83)80040-0. [DOI] [PubMed] [Google Scholar]
- 66.Shanmugam E, Doss CR, George M, et al. Effect of tolvaptan on acute heart failure with hyponatremia – a randomized, double blind, controlled clinical trial. Indian Heart J. 2016;68(Suppl 1):S15–21. doi: 10.1016/j.ihj.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Peri A. Clinical review: the use of vaptans in clinical endocrinology. J Clin Endocrinol Metab. 2013;98:1321–1332. doi: 10.1210/jc.2012-4082. [DOI] [PubMed] [Google Scholar]
- 68.Vidic A, Shuster JE, Goff ZD, et al. Vasopressin antagonism for decompensated right-sided heart failure. Int J Cardiol. 2019;274:245–247. doi: 10.1016/j.ijcard.2018.08.036. [DOI] [PubMed] [Google Scholar]
- 69.Rossi J, Bayram M, Udelson JE, et al. Improvement in hyponatremia during hospitalization for worsening heart failure is associated with improved outcomes: insights from the Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Chronic Heart Failure (ACTIV in CHF) trial. Acute Card Care. 2007;9:82–86. doi: 10.1080/17482940701210179. [DOI] [PubMed] [Google Scholar]
- 70.Sosa RE, Volpe M, Marion DN, et al. Relationship between renal hemodynamic and natriuretic effects of atrial natriuretic factor. Am J Physiol. 1986;250:F520–F524. doi: 10.1152/ajprenal.1986.250.3.F520. [DOI] [PubMed] [Google Scholar]
- 71.Chartier L, Schiffrin E, Thibault G, Garcia R. Atrial natriuretic factor inhibits the stimulation of aldosterone secretion by angiotensin II, ACTH and potassium in vitro and angiotensin II-induced steroidogenesis in vivo. Endocrinology. 1984;115:2026–2028. doi: 10.1210/endo-115-5-2026. [DOI] [PubMed] [Google Scholar]
- 72.Fujita S, Shimojo N, Terasaki F, et al. Atrial natriuretic peptide exerts protective action against angiotensin II-induced cardiac remodeling by attenuating inflammation via endothelin-1/endothelin receptor A cascade. Heart Vessels. 2013;28:646–657. doi: 10.1007/s00380-012-0311-0. [DOI] [PubMed] [Google Scholar]
- 73.de Bold AJ, de Bold ML, Sarda IR. Functional-morphological studies on in vitro cardionatrin release. J Hypertens Suppl. 1986;4:S3–S7. [PubMed] [Google Scholar]
- 74.Edwards BS, Zimmerman RS, Schwab TR, Heublein DM, Burnett JC., Jr Atrial stretch, not pressure, is the principal determinant controlling the acute release of atrial natriuretic factor. Circ Res. 1988;62:191–195. doi: 10.1161/01.res.62.2.191. [DOI] [PubMed] [Google Scholar]
- 75.Gentile F, Sciarrone P, Zamora E, et al (2020) Body mass index and outcomes in ischaemic versus non-ischaemic heart failure across the spectrum of ejection fraction [published online ahead of print, 2020 Jun 2]. Eur J Prev Cardiol. 2047487320927610. 10.1177/2047487320927610 [DOI] [PubMed]
- 76.Yan W, Wu F, Morser J, Wu Q. Corin, a transmembrane cardiac serine protease, acts as a pro-atrial natriuretic peptide-converting enzyme. Proc Natl Acad Sci USA. 2000;97:8525–8529. doi: 10.1073/pnas.150149097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lachance D, Garcia R, Gutkowska J, Cantin M, Thibault G. Mechanisms of release of atrial natriuretic factor. I. Effect of several agonists and steroids on its release by atrial minces. Biochem Biophys Res Commun. 1986;135:1090–1098. doi: 10.1016/0006-291x(86)91040-5. [DOI] [PubMed] [Google Scholar]
- 78.Mukoyama M, Nakao K, Hosoda K, et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J Clin Invest. 1991;87:1402–1412. doi: 10.1172/JCI115146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Potter LR, Abbey-Hosch S, Dickey DM. Natriuretic peptides, their receptors, and cyclic guanosine monophosphate-dependent signaling functions. Endocr Rev. 2006;27:47–72. doi: 10.1210/er.2005-0014. [DOI] [PubMed] [Google Scholar]
- 80.Lohmann SM, Vaandrager AB, Smolenski A, Walter U, De Jonge HR. Distinct and specific functions of cGMP-dependent protein kinases. Trends Biochem Sci. 1997;22:307–312. doi: 10.1016/s0968-0004(97)01086-4. [DOI] [PubMed] [Google Scholar]
- 81.Totsune K, Takahashi K, Ohneda M, Itoi K, Murakami O, Mouri T. C-type natriuretic peptide in the human central nervous system: distribution and molecular form. Peptides. 1994;15:37–40. doi: 10.1016/0196-9781(94)90167-8. [DOI] [PubMed] [Google Scholar]
- 82.Furuya M, Yoshida M, Hayashi Y, et al. C-type natriuretic peptide is a growth inhibitor of rat vascular smooth muscle cells. Biochem Biophys Res Commun. 1991;177:927–931. doi: 10.1016/0006-291x(91)90627-j. [DOI] [PubMed] [Google Scholar]
- 83.Atlas S, Maack T (1992) Atrial natriuretic factor. Handbook of physiology: renal physiology. Renal physiology. New York: Oxford University Press 1577–1673
- 84.Vanneste Y, Michel A, Dimaline R, Najdovski T, Deschodt-Lanckman M. Hydrolysis of alpha-human atrial natriuretic peptide in vitro by human kidney membranes and purified endopeptidase-24.11. Evidence for a novel cleavage site. Biochem J. 1988;254:531–537. doi: 10.1042/bj2540531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bayes-Genis A, Barallat J, Richards AM. A test in context: neprilysin: function, inhibition, and biomarker. J Am Coll Cardiol. 2016;68:639–653. doi: 10.1016/j.jacc.2016.04.060. [DOI] [PubMed] [Google Scholar]
- 86.Mangiafico S, Costello-Boerrigter LC, Andersen IA, Cataliotti A, Burnett JC., Jr Neutral endopeptidase inhibition and the natriuretic peptide system: an evolving strategy in cardiovascular therapeutics. Eur Heart J. 2013;34:886–893. doi: 10.1093/eurheartj/ehs262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.O'Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;7(365):32–43. doi: 10.1056/NEJMoa1100171. [DOI] [PubMed] [Google Scholar]
- 88.Sackner-Bernstein JD, Skopicki HA, Aaronson KD. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation. 2005;111:1487–1491. doi: 10.1161/01.CIR.0000159340.93220.E4. [DOI] [PubMed] [Google Scholar]
- 89.McKie PM, Cataliotti A, Huntley BK, Martin FL, Olson TM, Burnett JC., Jr A human atrial natriuretic peptide gene mutation reveals a novel peptide with enhanced blood pressure-lowering, renal-enhancing, and aldosterone-suppressing actions. J Am Coll Cardiol. 2009;54:1024–1032. doi: 10.1016/j.jacc.2009.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kaplan AP. Angioedema World Allergy Organ J. 2008;1:103–113. doi: 10.1097/WOX.0b013e31817aecbe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.McClean DR, Ikram H, Garlick AH, Richards AM, Nicholls MG, Crozier IG. The clinical, cardiac, renal, arterial and neurohormonal effects of omapatrilat, a vasopeptidase inhibitor, in patients with chronic heart failure. J Am Coll Cardiol. 2000;36:479–486. doi: 10.1016/s0735-1097(00)00741-5. [DOI] [PubMed] [Google Scholar]
- 92.McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004. doi: 10.1056/NEJMoa1409077. [DOI] [PubMed] [Google Scholar]
- 93.Solomon SD, McMurray JJV, Anand IS, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381:1609–1620. doi: 10.1056/NEJMoa1908655. [DOI] [PubMed] [Google Scholar]
- 94.Furchgott RF, Zawadzki JV. The obligatory role of the endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature. 1980;288:373–376. doi: 10.1038/288373a0. [DOI] [PubMed] [Google Scholar]
- 95.Mohan P, Brutsaert DL, Paulus WJ, Sys SU. Myocardial contractile response to nitric oxide and cGMP. Circulation. 1996;93:1223–1229. doi: 10.1161/01.cir.93.6.1223. [DOI] [PubMed] [Google Scholar]
- 96.Buys ES, Sips P, Vermeersch P, et al. Gender-specific hypertension and responsiveness to nitric oxide in sGCalpha1 knockout mice. Cardiovasc Res. 2008;79:179–186. doi: 10.1093/cvr/cvn068. [DOI] [PubMed] [Google Scholar]
- 97.Paulus WJ, Bronzwaer JG. Nitric oxide’s role in the heart: control of beating or breathing? Am J Physiol Heart Circ Physiol. 2004;287:H8–13. doi: 10.1152/ajpheart.01147.2003. [DOI] [PubMed] [Google Scholar]
- 98.Gheorghiade M, Marti CN, Sabbah HN, et al. Soluble guanylate cyclase: a potential therapeutic target for heart failure. Heart Fail Rev. 2013;18:123–134. doi: 10.1007/s10741-012-9323-1. [DOI] [PubMed] [Google Scholar]
- 99.Franssen C, Chen S, Unger A, et al. Myocardial microvascular inflammatory endothelial activation in heart failure with preserved ejection fraction. JACC Heart Fail. 2016;4:312–324. doi: 10.1016/j.jchf.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 100.Rotella DP. Phosphodiesterase 5 inhibitors: current status and potential applications. Nat Rev Drug Discov. 2002;1:674–682. doi: 10.1038/nrd893. [DOI] [PubMed] [Google Scholar]
- 101.Evgenov OV, Pacher P, Schmidt PM, Hasko G, Schmidt HH, Stasch JP. NO-independent stimulators and activators of soluble guanylate cyclase: discovery and therapeutic potential. Nat Rev Drug Discov. 2006;5:755–768. doi: 10.1038/nrd2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gheorghiade M, Greene SJ, Butler J, et al. Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. JAMA. 2015;314:2251–2262. doi: 10.1001/jama.2015.15734. [DOI] [PubMed] [Google Scholar]
- 103.Bonderman D, Ghio S, Felix SB, et al. Riociguat for patients with pulmonary hypertension caused by systolic left ventricular dysfunction: a phase IIb double-blind, randomized, placebo-controlled, dose-ranging hemodynamic study. Circulation. 2013;128:502–511. doi: 10.1161/CIRCULATIONAHA.113.001458. [DOI] [PubMed] [Google Scholar]
- 104.Armstrong PW, Pieske B, Anstrom KJ, et al. Vericiguat in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2020;382:1883–1893. doi: 10.1056/NEJMoa1915928. [DOI] [PubMed] [Google Scholar]
- 105.Wright EM, Turk E. The sodium/glucose cotransport family SLC5. Pflugers Arch. 2004;447:510–518. doi: 10.1007/s00424-003-1063-6. [DOI] [PubMed] [Google Scholar]
- 106.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 107.Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380:347–357. doi: 10.1056/NEJMoa1812389. [DOI] [PubMed] [Google Scholar]
- 108.Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;8(383):1413–1424. doi: 10.1056/NEJMoa2022190. [DOI] [PubMed] [Google Scholar]
- 109.McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008. doi: 10.1056/NEJMoa1911303. [DOI] [PubMed] [Google Scholar]
- 110.Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–1446. doi: 10.1056/NEJMoa2024816. [DOI] [PubMed] [Google Scholar]
- 111.Ye Y, Bajaj M, Yang HC, Perez-Polo JR, Birnbaum Y. SGLT-2 inhibition with dapagliflozin reduces the activation of the Nlrp3/ASC inflammasome and attenuates the development of diabetic cardiomyopathy in mice with type 2 diabetes. Further augmentation of the effects with saxagliptin, a DPP4 inhibitor. Cardiovasc Drugs Ther. 2017;31:119–132. doi: 10.1007/s10557-017-6725-2. [DOI] [PubMed] [Google Scholar]
- 112.El-Daly M, Pulakazhi Venu VK, Saifeddine M, et al. Hyperglycaemic impairment of PAR2-mediated vasodilation: prevention by inhibition of aortic endothelial sodium-glucose-co-transporter-2 and minimizing oxidative stress. Vascul Pharmacol. 2018;109:56–71. doi: 10.1016/j.vph.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 113.Cherney DZ, Perkins BA, Soleymanlou N, et al. The effect of empagliflozin on arterial stiffness and heart rate variability in subjects with uncomplicated type 1 diabetes mellitus. Cardiovasc Diabetol. 2014;13:28. doi: 10.1186/1475-2840-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Woods TC, Satou R, Miyata K, et al. Canagliflozin prevents intrarenal angiotensinogen augmentation and mitigates kidney injury and hypertension in mouse model of type 2 diabetes mellitus. Am J Nephrol. 2019;49:331–342. doi: 10.1159/000499597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Horton JL, Davidson MT, Kurishima C, et al. The failing heart utilizes 3-hydroxybutyrate as a metabolic stress defense. JCI Insight. 2019;4:12407. doi: 10.1172/jci.insight.124079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Scheen AJ. Effect of SGLT2 inhibitors on the sympathetic nervous system and blood pressure. Curr Cardiol Rep. 2019;21:70. doi: 10.1007/s11886-019-1165-1. [DOI] [PubMed] [Google Scholar]
- 117.Fozzard HA. Afterdepolarizations and triggered activity. Basic Res Cardiol. 1992;87:105–113. doi: 10.1007/978-3-642-72477-0_10. [DOI] [PubMed] [Google Scholar]
- 118.Digitalis Investigation Group The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–533. doi: 10.1007/978-3-642-72477-0_10. [DOI] [PubMed] [Google Scholar]
- 119.Russ MA, Prondzinsky R, Christoph A, et al. Hemodynamic improvement following levosimendan treatment in patients with acute myocardial infarction and cardiogenic shock. Critical Care Medicine. 2007;35:2732–2739. doi: 10.1097/01.CCM.0000287524.17358.48. [DOI] [PubMed] [Google Scholar]
- 120.Comín-Colet J, Manito N, Segovia-Cubero J, et al. Efficacy and safety of intermittent intravenous outpatient administration of levosimendan in patients with advanced heart failure: the LION-HEART multicentre randomised trial. Eur J Heart Fail. 2018;20:1128–1136. doi: 10.1002/ejhf.1145. [DOI] [PubMed] [Google Scholar]
- 121.Malik FI, Morgan BP. Cardiac myosin activation part 1: from concept to clinic. J Mol Cell Cardiol. 2011;51:454–461. doi: 10.1016/j.yjmcc.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 122.Swenson AM, Tang W, Blair CA, et al. Omecamtiv mecarbil enhances the duty ratio of human β-cardiac myosin resulting in increased calcium sensitivity and slowed force development in cardiac muscle. J Biol Chem. 2017;292:3768–3778. doi: 10.1074/jbc.M116.748780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mamidi R, Gresham KS, Li A, dos Remedios CG, Stelzer JE. Molecular effects of the myosin activator omecamtiv mecarbil on contractile properties of skinned myocardium lacking cardiac myosin binding protein-C. J Mol Cell Cardiol. 2015;85:262–272. doi: 10.1016/j.yjmcc.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Teerlink JR, Diaz R, Felker GM, et al. Omecamtiv mecarbil in chronic heart failure with reduced ejection fraction: rationale and design of GALACTIC-HF. JACC Heart Fail. 2020;8:329–340. doi: 10.1016/j.jchf.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 125.Teerlink JR, Diaz R, Felker GM, et al. Cardiac myosin activation with omecamtiv mecarbil in systolic heart failure. N Engl J Med. 2020;384:105–116. doi: 10.1056/NEJMoa2025797. [DOI] [PubMed] [Google Scholar]
- 126.Bayeva M, Gheorghiade M, Ardehali H. Mitochondria as a therapeutic target in heart failure. J Am Coll Cardiol. 2013;61:599–610. doi: 10.1016/j.jacc.2012.08.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Randle PJ, Garland PB, Hales CN, Newsholme EA. The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet. 1963;1:785–789. doi: 10.1016/s0140-6736(63)91500-9. [DOI] [PubMed] [Google Scholar]
- 128.Rajabi M, Kassiotis C, Razeghi P, Taegtmeyer H. Return to the fetal gene program protects the stressed heart: a strong hypothesis. Heart Fail Rev. 2007;12:331–343. doi: 10.1007/s10741-007-9034-1. [DOI] [PubMed] [Google Scholar]
- 129.Karbowska J, Kochan Z, Smolenski RT. Peroxisome proliferator-activated receptor α is downregulated in the failing human heart. Cell Mol Biol Lett. 2003;8:49–53. [PubMed] [Google Scholar]
- 130.Beauloye C, Bertrand L, Horman S, Hue L. AMPK activation, a preventive therapeutic target in the transition from cardiac injury to heart failure. Cardiovasc Res. 2011;90:224–233. doi: 10.1093/cvr/cvr034. [DOI] [PubMed] [Google Scholar]
- 131.Hesselink MK, Schrauwen P. Uncoupling proteins in the failing human heart: friend or foe? Lancet. 2005;365:385–386. doi: 10.1016/S0140-6736(05)17823-4. [DOI] [PubMed] [Google Scholar]
- 132.Tsutsui H, Kinugawa S, Matsushima S. Oxidative stress and heart failure. Am J Physiol Heart Circ Physiol. 2011;301:H2181–H2190. doi: 10.1152/ajpheart.00554.2011. [DOI] [PubMed] [Google Scholar]
- 133.Aubert G, Vega RB. Kelly DP (2013) Perturbations in the gene regulatory pathways controlling mitochondrial energy production in the failing heart. Biochim Biophys Acta. 2013;1833:840–847. doi: 10.1016/j.bbamcr.2012.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kantor PF, Lucien A, Kozak R, Lopaschuk GD. The antianginal drug trimetazidine shifts cardiac energy metabolism from fatty acid oxidation to glucose oxidation by inhibiting mitochondrial long-chain 3-ketoacyl coenzyme A thiolase. Circ Res. 2000;86:580–588. doi: 10.1161/01.res.86.5.580. [DOI] [PubMed] [Google Scholar]
- 135.Fragasso G, Rosano G, Baek SH, et al. Effect of partial fatty acid oxidation inhibition with trimetazidine on mortality and morbidity in heart failure: results from an international multicentre retrospective cohort study. Int J Cardiol. 2013;163:320–325. doi: 10.1016/j.ijcard.2012.09.123. [DOI] [PubMed] [Google Scholar]
- 136.Vitale C, Wajngaten M, Sposato B, et al. Trimetazidine improves left ventricular function and quality of life in elderly patients with coronary artery disease. Eur Heart J. 2004;25:1814–1821. doi: 10.1016/j.ehj.2004.06.034. [DOI] [PubMed] [Google Scholar]
- 137.Fragasso G, Palloshi A, Puccetti P, et al. A randomized clinical trial of trimetazidine, a partial free fatty acid oxidation inhibitor, in patients with heart failure. J Am Coll Cardiol. 2006;48:992–998. doi: 10.1016/j.jacc.2006.03.060. [DOI] [PubMed] [Google Scholar]
- 138.Paradies G, Paradies V, De Benedictis V, Ruggiero FM, Petrosillo G. Functional role of cardiolipin in mitochondrial bioenergetics. Biochim Biophys Acta. 2014;1837:408–417. doi: 10.1016/j.bbabio.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 139.Bentinger M, Brismar K, Dallner G. The antioxidant role of coenzyme Q. Mitochondrion. 2007;7:S41–50. doi: 10.1016/j.mito.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 140.Sabbah HN, Gupta RC, Kohli S, Wang M, Hachem S, Zhang K. Chronic therapy with elamipretide (MTP-131), a novel mitochondria-targeting peptide, improves left ventricular and mitochondrial function in dogs with advanced heart failure. Circ Heart Fail. 2016;9:e002206. doi: 10.1161/CIRCHEARTFAILURE.115.002206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Daubert MA, Yow E, Dunn G, et al. Novel mitochondria-targeting peptide in heart failure treatment: a randomized, placebo-controlled trial of elamipretide. Circ Heart Fail. 2017;10:e004389. doi: 10.1161/CIRCHEARTFAILURE.117.004389. [DOI] [PubMed] [Google Scholar]
- 142.Butler J, Khan MS, Anker SD, et al. Effects of elamipretide on left ventricular function in patients with heart failure with reduced ejection fraction: the PROGRESS-HF phase 2 trial. J Card Fail. 2020;26:429–437. doi: 10.1016/j.cardfail.2020.02.001. [DOI] [PubMed] [Google Scholar]
- 143.Mortensen SA, Rosenfeldt F, Kumar A, et al. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC Heart Fail. 2014;2:641–649. doi: 10.1016/j.jchf.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 144.Ueland T, Gullestad L, Nymo SH, Yndestad A, Aukrust P, Askevold ET. Inflammatory cytokines as biomarkers in heart failure. Clin Chim Acta. 2015;443:71–77. doi: 10.1016/j.cca.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 145.Ferdinandy P, Danial H, Ambrus I, Rothery RA, Schulz R. Peroxynitrite is a major contributor to cytokine-induced myocardial contractile failure. Circ Res. 2000;87:241–224. doi: 10.1161/01.res.87.3.241. [DOI] [PubMed] [Google Scholar]
- 146.Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 147.Ridker PM, MacFadyen JG, Everett BM, Libby P, Thuren T, Glynn RJ. Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomised controlled trial. Lancet. 2018;391:319–328. doi: 10.1016/S0140-6736(17)32814-3. [DOI] [PubMed] [Google Scholar]
- 148.Bisping E, Wakula P, Poteser M, Heinzel FR. Targeting cardiac hypertrophy: toward a causal heart failure therapy. J Cardiovasc Pharmacol. 2014;64:293–305. doi: 10.1097/FJC.0000000000000126. [DOI] [PubMed] [Google Scholar]
- 149.Dian JC, Zhao VW, Pavan KB, et al. Histone deacetylase (HDAC) inhibitors attenuate cardiac hypertrophy by suppressing autophagy. Proc Natl Acad Sci USA. 2011;108:4123–4128. doi: 10.1073/pnas.1015081108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Thum T, Condorelli G. Long noncoding RNAs and MicroRNAs in cardiovascular pathophysiology. Circ Res. 2015;116:751–762. doi: 10.1161/CIRCRESAHA.116.303549. [DOI] [PubMed] [Google Scholar]
- 151.McKinsey TA, Kass DA. Small-molecule therapies for cardiac hypertrophy: moving beneath the cell surface. Nat Rev Drug Discov. 2007;6:617–635. doi: 10.1038/nrd2193. [DOI] [PubMed] [Google Scholar]
- 152.González A, Schelbert EB, Díez J, Butler J. Myocardial interstitial fibrosis in heart failure. J Am Coll Cardiol. 2018;71:1696–1706. doi: 10.1016/j.jacc.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 153.Aimo A, Cerbai E, Bartolucci G, et al. Pirfenidone is a cardioprotective drug: Mechanisms of action and preclinical evidence. Pharmacol Res. 2020;155:104694. doi: 10.1016/j.phrs.2020.104694. [DOI] [PubMed] [Google Scholar]
- 154.Pitt B, Pfeffer MA, Assmann SF, et al. TOPCAT Investigators. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383–1392. doi: 10.1056/NEJMoa1313731. [DOI] [PubMed] [Google Scholar]
- 155.Vergaro G, Aimo A, Prontera C, et al. Sympathetic and renin-angiotensin-aldosterone system activation in heart failure with preserved, mid-range and reduced ejection fraction. Int J Cardiol. 2019;296:91–97. doi: 10.1016/j.ijcard.2019.08.040. [DOI] [PubMed] [Google Scholar]
- 156.Maurer MS, Schwartz JH, Gundapaneni B, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379:1007–1016. doi: 10.1056/NEJMoa1805689. [DOI] [PubMed] [Google Scholar]
- 157.Adapala RK, Thoppil RJ, Luther DJ, et al. TRPV4 channels mediate cardiac fibroblast differentiation by integrating mechanical and soluble signals. J Mol Cell Cardiol. 2013;54:45–52. doi: 10.1016/j.yjmcc.2012.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Thum T, Gross C, Fiedler J, et al. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature. 2008;456:980–984. doi: 10.1038/nature07511. [DOI] [PubMed] [Google Scholar]
- 159.Lin Z, Murtaza I, Wang K, Jiao J, Gao J, Li PF. miR-23a functions downstream of NFATc3 to regulate cardiac hypertrophy. Proc Natl Acad Sci USA. 2009;106:12103–12108. doi: 10.1073/pnas.0811371106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bartolucci J, Verdugo FJ, González PL, et al. Safety and efficacy of the intravenous infusion of umbilical cord mesenchymal stem cells in patients with heart failure: a phase 1/2 randomized controlled trial (RIMECARD Trial [Randomized Clinical Trial of Intravenous Infusion Umbilical Cord Mesenchymal Stem Cells on Cardiopathy]) Circ Res. 2017;27:1192–1204. doi: 10.1161/CIRCRESAHA.117.310712. [DOI] [PMC free article] [PubMed] [Google Scholar]