Abstract
Background
Older patients (65+) with mild cognitive impairment (MCI) receive less guideline-concordant care for cardiovascular disease (CVD) and other conditions than patients with normal cognition (NC). One potential explanation is that patients with MCI want less treatment than patients with NC; however, the treatment preferences of patients with MCI have not been studied.
Objective
To determine whether patients with MCI have different treatment preferences than patients with NC.
Design
Cross-sectional survey conducted at two academic medical centers from February to December 2019
Participants
Dyads of older outpatients with MCI and NC and patient-designated surrogates.
Main Measures
The modified Life-Support Preferences-Predictions Questionnaire score measured patients’ preferences for life-sustaining treatment decisions in six health scenarios including stroke and acute myocardial infarction (range, 0–24 treatments rejected with greater scores indicating lower desire for treatment).
Key Results
The survey response rate was 73.4%. Of 136 recruited dyads, 127 (93.4%) completed the survey (66 MCI and 61 NC). The median number of life-sustaining treatments rejected across health scenarios did not differ significantly between patients with MCI and patients with NC (4.5 vs 6.0; P=0.55). Most patients with MCI (80%) and NC (80%) desired life-sustaining treatments in their current health (P=0.99). After adjusting for patient and surrogate factors, the difference in mean counts of rejected treatments between patients with MCI and patients with NC was not statistically significant (adjusted ratio, 1.08, 95% CI, 0.80–1.44; P=0.63).
Conclusion
We did not find evidence that patients with MCI want less treatment than patients with NC. These findings suggest that other provider and system factors might contribute to patients with MCI getting less guideline-concordant care.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06839-w.
KEY WORDS: aging, Alzheimer’s, cardiovascular disease, health services research
INTRODUCTION
More than 5.4 million Americans—up to 20% of older adults (65+)—have mild cognitive impairment (MCI),1 and this number might triple by 2050.2 MCI is characterized by measurable cognitive impairment that does not significantly impair daily functioning.3 Dementia is not inevitable in patients with MCI.4 While some patients diagnosed with MCI develop dementia (3–15% per year), others remain stable or revert to normal cognition (NC) (14–55%).5–8 Many patients with MCI live up to a decade on average,9,10 with good quality of life,11,12 and face aging health risks including cardiovascular disease (CVD), the leading cause of death and disability in patients with MCI and NC.10,13 Clinical practice guidelines recommend that all older patients receive guideline-concordant care for CVD unless they have advanced dementia or limited life expectancy.14–16 Nevertheless, evidence suggests patients with MCI receive fewer guideline-concordant treatments for CVD and other conditions than patients with NC.17–20
The reasons that patients with MCI get fewer guideline-concordant treatments are unclear though some physicians believe patients with MCI, compared with patients with NC, want less intensive care.21,22 The extent to which treatment preferences differ between patients with MCI and NC is unknown. Exploring the association between patient MCI diagnosis and treatment preferences in Black and White patients is important because Black patients, compared with White patients, are more likely to have MCI.1 However, some studies have suggested Black patients tend to have less understanding of dementia and perceive themselves as having a lower dementia risk.23–25
We conducted a multi-center survey study of older patients to determine how patient MCI diagnosis influences treatment preferences in several clinical scenarios, including two CVD events, acute myocardial infarction (AMI) and stroke. We hypothesized that patients with MCI would prefer less treatment than patients with NC because patients with MCI might overestimate their dementia risk. We based this hypothesis on research showing people tend to overestimate the risk of rare events and underestimate the risk of common events,26 and patients with lower cognitive function have greater worry about dementia.27
METHODS
Study Population
We recruited patients and their self-designated surrogates by mail and telephone at two academic medical centers (University of Michigan [U-M] and Duke University [Duke]). The Online Appendix 1 has details. We included surrogates defined as a friend or family member involved in the patients’ medical care because patients with MCI and NC frequently involve friends or family members in their care. We contacted participants from the available rosters with a goal of recruiting a sample that had approximately equal numbers of Black and White dyads by cognitive status group within each site.
We recruited patients with MCI and surrogates from cognitive/memory disorders clinics, geriatric clinics, medical records, and/or active cognition studies. We recruited patients with NC and their surrogates from established registries and active studies at U-M and Duke. Eligible patients were required to be 65 or older, have a diagnosis of MCI or NC within the past 12 months, read and speak English, self-identify as having Black or White race, and have a self-designated surrogate 18 or older who reads and speaks English. At both sites, the diagnosis of MCI was based on cognitive testing, clinical examinations, and expert clinician diagnosis following the 2011 National Institute on Aging—Alzheimer’s Association (NIA-AA) diagnostic guidelines for MCI.28 We aimed to recruit 100 patient-surrogate dyads (50 dyads per site) based on pre-survey power calculations (Online Appendix 1). Patients and surrogates provided written consent before completing the paper survey and received a $50 incentive. The U-M and Duke institutional review boards approved this study.
Survey Data Collection
We refined surveys based on two rounds of cognitive interviews with 28 individuals (8 with MCI) to ensure understanding in the target population. Online Appendices 2 and 3 have the full surveys. We obtained missing survey data by telephone, as possible.29
Primary Outcome
The primary outcome was the Life-Support Preferences-Predictions Questionnaire (LSPQ).30 The LSPQ is a validated measure of treatment preferences in patients and surrogates across a broad spectrum of realistic life-sustaining treatment decisions.30,31 We used a modified version of the LSPQ that had six health scenarios: (1) the patient’s current health; (2) emphysema; (3) stroke; (4) metastatic colon cancer; (5) heart attack with heart failure; and (6) dementia (Online Appendix 1). Patients were asked to imagine themselves in each scenario and indicate their preference for receiving each of 4 life-sustaining medical treatments chosen to vary in invasiveness: (1) antibiotics for life-threatening pneumonia; (2) cardiopulmonary resuscitation for cardiac arrest; (3) emergency gall bladder surgery for life-threatening gallbladder infection; and (4) artificial nutrition and hydration for inability to take food or water. The modified LSPQ had high reliability (Cronbach’s alpha of 0.96 in patients with MCI and NC and their surrogates), comparable to the previous LSPQ version.32
Patients indicated their treatment preferences using a 5-point Likert scale (probably want treatment, definitely want treatment, unsure, probably do not want treatment, and definitely do not want treatment).30 Surrogates imagined the patient in each illness scenario and indicated the treatments they would want for the patient using the same scale. To calculate LSPQ total scores, we summed the probably/definitely “do not want treatment” responses across the 24 questions (6 health scenarios times 4 life-sustaining treatments/scenario) resulting in values ranging from zero to 24. Based on previous research,30,33 we categorized “unsure” responses with “want treatment” because the clinical default in most scenarios is to provide treatment unless specifically refused.
Secondary Outcomes
We assessed patients’ and surrogates’ preferences for shared decision-making (SDM) with clinicians in general using the Control Preferences Scale.34 We also assessed patients’ SDM preferences for specific AMI and ischemic stroke treatments varying in invasiveness and settings across the treatment spectrum from acute treatment to rehabilitation to secondary prevention using a 5-point Likert scale ranging from “definitely do not want to be involved” to “definitely want to be involved.” The four treatments after AMI included coronary angioplasty, coronary artery bypass graft surgery, outpatient cardiac rehabilitation, and cholesterol medicine. The four treatments after ischemic stroke included intravenous tissue plasminogen activator (IV t-PA), carotid endarterectomy, inpatient rehabilitation, and anticoagulation for atrial fibrillation. Surrogates imagined the patient in each AMI and stroke scenario and indicated their own preferences for being involved in the treatment decisions using the same scale.
Covariates
Patients and surrogates self-reported covariates. Demographic variables included age, gender, race, marital status, and education level. Health experience variables included health status, medical history (stroke, heart disease, chronic lung disease, cancer, and arthritis),35 depressive symptoms,36 functional limitations in basic activities of daily living (ADLs),35 presence of a close family member/friend with dementia, AMI, and stroke,35 and social support/structure.37–39 To adjust for patients’ global cognitive performance, patients with MCI and NC completed the Montreal Cognitive Assessment (MoCA) test at a routine clinic or research study visit during the 12 months before the survey. Surrogates separately reported patient’s functional abilities using the Dementia Severity Rating Scale (DSRS),40 relationship to the patient, duration of the relationship, and type/frequency of contact with the patient.
Statistical Analysis
We compared descriptive characteristics by patient cognitive status (MCI vs. NC) using Mood’s median tests for continuous variables and χ2 tests or Fisher’s exact tests for categorical variables. A high proportion of patients and surrogates had LSPQ scores of 0, indicating they would reject zero life-sustaining treatments and want every life-sustaining treatment in every scenario. We examined associations between LSPQ score (dependent variable) and patient cognitive status using zero-inflated negative binomial (ZINB) regression, a method used to model over-dispersed count data with excessive zeros.
The ZINB model consisted of two complementary sub-models. The regression sub-model had a dichotomous outcome with categories LSPQ=0 and LSPQ>0 pertaining to a hypothetical (latent) subpopulation of patients “at risk” of having an LSPQ score equal to 0. The negative binomial regression sub-model had a continuous outcome of LSPQ score with values ranging from 0 to 24 pertaining to a hypothetical subpopulation of patients “not at risk” of having an LSPQ score equal to 0. To allow for direct interpretation of the model coefficients in terms of overall effects associated with the entire population, we assumed that the probability of belonging to the first subpopulation did not depend on any covariates.41 Consequently, we present the ZINB model results in terms of regression coefficients obtained from the negative binomial regression sub-model. We present and interpret the ZINB model coefficients in terms of ratios of mean counts representing a relative increase/decrease of patient-surrogate responses expressing no desire for life-sustaining treatments attributed to a one-unit increase in a value of a corresponding covariate. We found no significant association between a race * MCI interaction term and the patient- or surrogate-reported LSPQ scores. We examined differences in secondary outcomes by patient cognitive status; however, insufficient cell sizes in some response categories precluded significance testing. The analytic code is publicly available (https://github.com/deblevine/MCI-DeM_LSPQ).
RESULTS
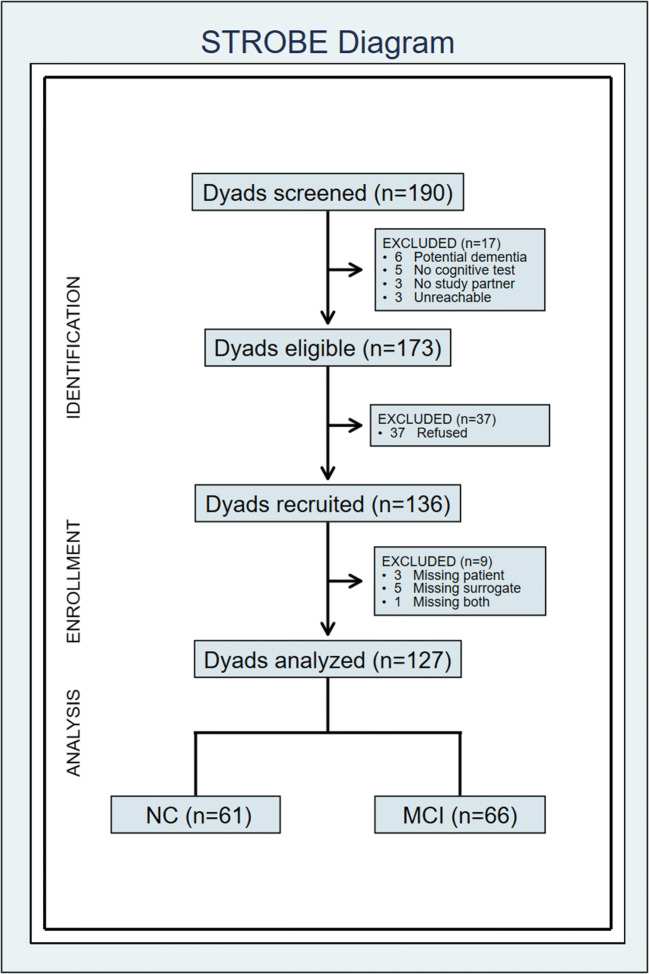
Figure 1 presents a flow diagram. Of 190 screened dyads, 173 dyads were eligible. Of the 173 eligible dyads, we recruited 136 dyads, and 127 dyads (66 MCI, 61 NC) completed the surveys (final analytic sample). The response rate was 73.4% (127/173). The completion rate was 93.4% (127/136).
Figure 1.
STROBE diagram. Abbreviations: MCI, mild cognitive impairment; NC, normal cognition.
Table 1 presents descriptive characteristics by patient cognitive status. Patients with MCI (42.4% Black, 60.6% female, median [IQR] age: 74.0 [69.0, 78.0] years), compared to patients with NC (47.5% Black, 62.3% female, median [IQR] age: 71.0 [69.0, 76.0] years), had lower cognitive performance (median MoCA scores, 23 vs 27 points; P<0.001), higher functional dependence due to cognitive impairment (median DSRS scores, 5.5 vs 1 points; P<0.001), greater indication of depression (40.9% vs 19.7%; P=0.01), and longer relationships with their surrogates (52 vs 43 years; P=0.04).
Table 1.
Patient, Surrogate, and Dyad Characteristics, by Patient’s MCI Status
| Variable | Patient MCI status | P | |
|---|---|---|---|
| No MCI (n=61) | MCI (n=66) | ||
| Patient characteristics | |||
| Age, years: median (IQR) | 71.0 (69.0, 76.0) | 74.0 (69.0, 78.0) | 0.66 |
| MoCA, points: median (IQR) | 27.0 (26.0, 28.0) | 23.0 (21.0, 25.0) | <0.001 |
| DSRS*, points: median (IQR) | 1.0 (0.0, 2.0) | 5.5 (1.0, 10.0) | <0.001 |
| Race, Black: no. (%) | 29 (47.5) | 28 (42.4) | 0.56 |
| Gender, female: no. (%) | 38 (62.3) | 40 (60.6) | 0.85 |
| Education: no. (%) | 0.09 | ||
| No college | 3 (4.9) | 11 (16.7) | |
| Some college | 23 (37.7) | 17 (25.8) | |
| 4-Year degree | 9 (14.8) | 14 (21.2) | |
| Graduate degree | 26 (42.6) | 24 (36.4) | |
| Marital status: no. (%) | 0.27 | ||
| Single | 28 (45.9) | 24 (36.4) | |
| Married/partner | 33 (54.1) | 42 (63.6) | |
| Has children: no. (%) | 56 (91.8) | 62 (93.9) | 0.74 |
| Lives with child: no. (%) | 9 (14.8) | 5 (7.7) | 0.26 |
| Child within 30 miles: no. (%) | 34 (55.7) | 43 (68.3) | 0.15 |
| Self-rated health: no. (%) | 0.43 | ||
| Fair | 3 (4.9) | 9 (13.6) | |
| Good | 31 (50.8) | 30 (45.5) | |
| Very good | 21 (34.4) | 21 (31.8) | |
| Excellent | 6 (9.8) | 6 (9.1) | |
| Depression: no. (%) | 0.010 | ||
| No indication | 49 (80.3) | 39 (59.1) | |
| Some indication | 12 (19.7) | 27 (40.9) | |
| Difficulty with ADLs: no. (%) | 14 (23.0) | 13 (19.7) | 0.65 |
| Disease history: no. (%) | |||
| Stroke | 4 (6.6) | 6 (9.1) | 0.75 |
| Lung disease | 9 (14.8) | 3 (4.5) | 0.07 |
| Heart disease | 15 (24.6) | 15 (22.7) | 0.80 |
| Cancer | 14 (23.0) | 18 (27.3) | 0.58 |
| Arthritis | 47 (77.0) | 43 (65.2) | 0.14 |
| Contact history: no. (%) | |||
| Dementia | 39 (63.9) | 49 (74.2) | 0.21 |
| Stroke | 41 (67.2) | 38 (57.6) | 0.26 |
| Heart attack | 42 (68.9) | 36 (54.5) | 0.10 |
| Surrogate characteristics | |||
| Age, years: median (IQR) | 69.0 (62.0, 72.0) | 70.0 (64.0, 77.0) | 0.61 |
| Race, Black: no. (%) | 30 (49.2) | 28 (42.4) | 0.45 |
| Gender, female: no. (%) | 42 (68.9) | 43 (65.2) | 0.66 |
| Education: no. (%) | 0.31 | ||
| No college | 4 (6.6) | 9 (13.6) | |
| Some college | 26 (42.6) | 19 (28.8) | |
| 4-Year degree | 10 (16.4) | 11 (16.7) | |
| Graduate degree | 21 (34.4) | 27 (40.9) | |
| Marital status: no. (%) | 0.06 | ||
| Single | 21 (34.4) | 13 (19.7) | |
| Married/partner | 40 (65.6) | 53 (80.3) | |
| Self-rated health: no. (%) | 0.88 | ||
| Fair | 4 (6.6) | 7 (10.6) | |
| Good | 20 (32.8) | 22 (33.3) | |
| Very good | 29 (47.5) | 29 (43.9) | |
| Excellent | 8 (13.1) | 8 (12.1) | |
| Depression: no. (%) | 0.58 | ||
| No indication | 47 (77.0) | 48 (72.7) | |
| Some indication | 14 (23.0) | 18 (27.3) | |
| Difficulty with ADLs: no. (%) | 12 (19.7) | 13 (19.7) | 0.99 |
| Disease history: no. (%) | |||
| Stroke | 1 (1.6) | 3 (4.5) | 0.62 |
| Lung disease | 6 (9.8) | 5 (7.6) | 0.76 |
| Heart disease | 10 (16.4) | 15 (22.7) | 0.37 |
| Cancer | 12 (19.7) | 18 (27.3) | 0.31 |
| Arthritis | 29 (47.5) | 37 (56.1) | 0.34 |
| Contact history: no. (%) | |||
| Dementia | 39 (63.9) | 43 (65.2) | 0.89 |
| Stroke | 37 (60.7) | 39 (59.1) | 0.86 |
| Heart attack | 45 (73.8) | 41 (62.1) | 0.16 |
| Dyad characteristics | |||
| Relationship length, years: median (IQR) | 43.0 (28.0, 53.0) | 51.5 (40.0, 60.0) | 0.04 |
| Site: no. (%) | 0.72 | ||
| U-M | 36 (59.0) | 41 (62.1) | |
| DU | 25 (41.0) | 25 (37.9) | |
| Relationship type: no. (%) | 0.19 | ||
| Spouse | 33 (54.1) | 40 (60.6) | |
| Child | 10 (16.4) | 8 (12.1) | |
| Friend | 14 (23.0) | 8 (12.1) | |
| Other | 4 (6.6) | 10 (15.2) | |
| Physical interaction: no. (%) | 0.66 | ||
| Daily | 38 (62.3) | 45 (68.2) | |
| Several times per week | 10 (16.4) | 11 (16.7) | |
| Once per week or less | 13 (21.3) | 10 (15.2) | |
| Verbal interaction: no. (%) | 0.39 | ||
| Daily | 42 (68.9) | 47 (71.2) | |
| Several times per week | 11 (18.0) | 15 (22.7) | |
| Once per week or less | 8 (13.1) | 4 (6.1) | |
P values were obtained using the following1: Mood’s median tests, for continuous variables2; χ2 tests, for categorical variables with expected cell counts >5; and3 Fisher’s exact tests, for categorical variables with expected cell counts ≤5. Abbreviations: MCI, mild cognitive impairment; NC, normal cognition; IQR, interquartile range; MoCA, Montreal Cognitive Assessment; DSRS, Dementia Severity Rating Scale; ADL, activity of daily living; U-M, University of Michigan; DU, Duke University
*Provided by the surrogate
Primary Outcome: Patients’ Preferences For life-Sustaining Treatments
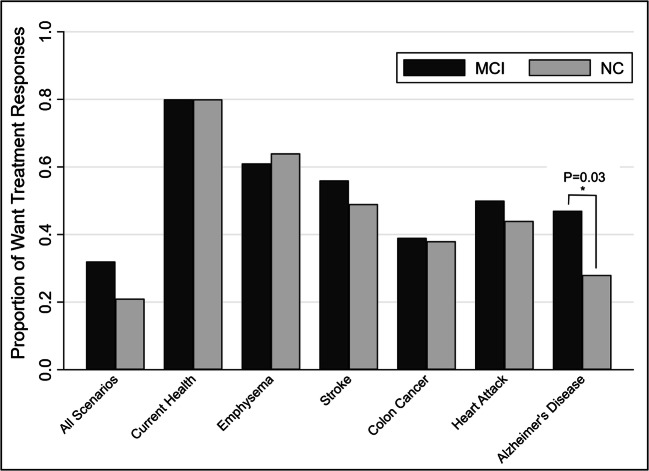
The median number of life-sustaining treatments rejected across the six health scenarios was not significantly different between patients with MCI and those with NC (rejected treatments, 4.5 vs 6.0; P=0.55) (Table 2). Figure 2 presents the proportion of desired life-sustaining treatments by patients’ cognitive status and health scenario. Differences in the proportions of patients with MCI and NC who desired life-sustaining treatments in individual health scenarios were not statistically significant, except patients with MCI desired more life-sustaining treatments than patients with NC in the Alzheimer’s disease scenario (P=0.03) (Fig. 2). Most patients with MCI (80%) and NC (80%) desired life-sustaining treatments in their current health (P=0.99).
Table 2.
Medical Decision-making Preferences, by Patient’s MCI Status
| Variable | Patient responses | Surrogate responses* | ||||
|---|---|---|---|---|---|---|
| Patient MCI status | Patient MCI status | |||||
| NC (n=61) | MCI (n=66) | P | NC (n=61) | MCI (n=66) | P | |
| LSPQ score† | ||||||
| Number of rejected treatments: median (IQR) | 6.0 (1.0, 13.0) | 4.5 (0.0, 13.0) | 0.55 | 0.0 (0.0, 5.0) | 1.0 (0.0, 7.0) | 0.12 |
| Zero treatments rejected: no. (%) | 13 (21.3) | 21 (31.8) | 0.18 | 38 (62.3) | 32 (48.5) | 0.12 |
| Control Preferences Scale: no. (%) | 0.76 | 0.94 | ||||
| I make all medical decisions | 5 (8.2) | 6 (9.1) | 4 (6.6) | 4 (6.1) | ||
| I make final medical decisions | 36 (59.0) | 36 (54.5) | 38 (62.3) | 37 (56.1) | ||
| My doctor and I make joint medical decisions | 18 (29.5) | 18 (27.3) | 17 (27.9) | 22 (33.3) | ||
| My doctor makes final medical decisions | 2 (3.3) | 4 (6.1) | 1 (1.6) | 2 (3.0) | ||
| My doctor makes all medical decisions | 0 (0.0) | 2 (3.0) | 1 (1.6) | 1 (1.5) | ||
| Desired involvement in treatment decisions | ||||||
| Scenario: acute MI: no. (%)‡ | ||||||
| Coronary angioplasty | 59 (96.7) | 63 (95.5) | 0.99 | 56 (91.8) | 63 (95.5) | 0.48 |
| Coronary artery bypass graft surgery | 60 (98.4) | 64 (97.0) | 0.99 | 56 (91.8) | 64 (97.0) | 0.26 |
| Cardiac rehabilitation | 60 (98.4) | 62 (93.9) | 0.37 | 59 (96.7) | 65 (98.5) | 0.61 |
| Cholesterol medication | 60 (98.4) | 63 (95.5) | 0.62 | 54 (88.5) | 63 (95.5) | 0.19 |
| Scenario: stroke: no. (%)‡ | ||||||
| Intravenous tissue plasminogen activator | 57 (93.4) | 61 (92.4) | 0.99 | 58 (95.1) | 60 (90.9) | 0.49 |
| Carotid endarterectomy | 58 (95.1) | 62 (93.9) | 0.99 | 58 (95.1) | 61 (92.4) | 0.72 |
| Inpatient stroke rehabilitation | 61 (100.0) | 64 (97.0) | 0.50 | 59 (96.7) | 62 (93.9) | 0.37 |
| Anticoagulation for atrial fibrillation | 59 (96.7) | 64 (97.0) | 0.99 | 56 (91.8) | 62 (93.9) | 0.99 |
P values were obtained using Mood’s median tests, for continuous variables, and Fisher’s exact tests, for categorical variables. Abbreviations: MCI, mild cognitive impairment; NC, normal cognition; LSPQ, Life-Support Preferences-Predictions Questionnaire; IQR, inter quartile range
*All surrogate responses are provided in reference to the patient’s treatment, with the exception of control preferences
†Life-Support Preferences-Predictions Questionnaire scores are counts of subject responses expressing no desire for life-sustaining treatment and range 0 to 24. Higher scores indicate a lower desire for treatment. Zero treatments rejected means the participant would want all life-sustaining treatments in all health scenarios
‡Representing participants who prefer to be involved in treatment decisions, compared with those who do not
Figure 2.
Patient preferences for medical treatment, by patient’s MCI status and health scenario. Differences between MCI and NC patients: all scenarios (P=0.23), current health (P=0.99), emphysema (P=0.72), stroke (P=0.48), colon cancer (P=0.86), heart attack (P=0.60), Alzheimer’s disease (P=0.03). Abbreviations: MCI, mild cognitive impairment; NC, normal cognition.
Patients’ preferences for life-sustaining treatments did not differ significantly by patient MCI diagnosis before and after adjustment for patient and surrogate factors (Table 3). After adjustment, the difference in mean counts of rejected treatments between patients with MCI and patients with NC was not statistically significant (adjusted ratio, 1.00, 95% CI, 0.71–1.41; P=0.99). Mean counts of rejected treatments across health scenarios were lower in Black patients (adjusted ratio, 0.33, 95% CI, 0.20–0.55, P<0.001), male patients (ratio, 0.58, 95% CI, 0.39–0.84; P=0.005), and male surrogates (adjusted ratio, 0.55, 95% CI, 0.36–0.84; P=0.005). Patients having a family member or friend with stroke had higher counts of rejected treatments across health scenarios (adjusted ratio, 1.41, 95% CI, 1.01–1.95; P=0.04).
Table 3.
Unadjusted and Adjusted Analysis of Patient-Reported Number of Treatments Rejected Across Health Scenarios
| Covariate | Ratio of average counts of rejecting treatment across health scenarios | ||
|---|---|---|---|
| Ratio | 95% CI | P | |
| Unadjusted model | |||
| Patient: MCI vs NC | 1.06 | 0.79, 1.42 | 0.69 |
| Adjusted model | |||
| Patient: MCI vs NC | 1.00 | 0.71, 1.41 | 0.99 |
| Patient: age, per 1-year increase | 1.00 | 0.98, 1.03 | 0.76 |
| Patient: Black vs White | 0.33 | 0.20, 0.55 | <0.001 |
| Patient: education | |||
| Some college vs no college | 1.17 | 0.64, 2.13 | 0.61 |
| 4-year degree vs no college | 1.42 | 0.71, 2.84 | 0.32 |
| Graduate degree vs no college | 1.54 | 0.86, 2.76 | 0.15 |
| Patient: male vs female | 0.58 | 0.39, 0.84 | 0.005 |
| Surrogate: male vs female | 0.55 | 0.36, 0.84 | 0.005 |
| Patient: contact vs no contact with stroke* | 1.41 | 1.01, 1.95 | 0.04 |
Unadjusted and adjusted models were tested using zero-inflated negative binomial regression. Abbreviations: CI, confidence interval; MCI, mild cognitive impairment; NC, normal cognition
*Close family member or friend has history of stroke
Secondary Outcomes
Surrogates’ preferences for the patients to receive life-sustaining treatments across health scenarios did not differ significantly by patient MCI diagnosis, before and after adjustment for patient and surrogate factors. There was no statistically significant difference in the median number of life-sustaining treatments rejected between surrogates of patients with MCI and surrogates of those with NC (rejected treatments, 0.0 vs 1.0; P=0.12) (Table 2). After adjusting for patient and surrogate factors, the difference in mean counts of rejected life-sustaining treatments on the LSPQ between surrogates of patients with MCI and surrogates of patients with NC was not significantly different (adjusted ratio, 1.06, 95% CI, 0.71=1.57, P=0.77) (Table 4). Mean counts of rejected treatments across health scenarios were lower in Black surrogates (adjusted ratio, 0.52, 95% CI, 0.30–0.92; P=0.02). Surrogates having a history of stroke had higher counts of rejected treatments across health scenarios (adjusted ratio, 2.80, 95% CI, 1.68–4.68; P<0.001).
Table 4.
Unadjusted and Adjusted Analysis of Surrogate-Reported Number of Treatments Rejected Across Health Scenarios
| Covariate | Ratio of average counts of rejecting treatment across health scenarios | ||
|---|---|---|---|
| Ratio | 95% CI | P | |
| Unadjusted model | |||
| Patient: MCI vs NC | 1.20 | 0.79, 1.82 | 0.40 |
| Adjusted model | |||
| Patient: MCI vs NC | 1.06 | 0.71, 1.57 | 0.77 |
| Surrogate: age, years | 1.00 | 0.97, 1.02 | 0.69 |
| Surrogate: Black vs White | 0.52 | 0.30, 0.92 | 0.02 |
| Surrogate: male vs female | 0.92 | 0.59, 1.43 | 0.70 |
| Surrogate: education | |||
| Some college vs no college | 0.56 | 0.28, 1.13 | 0.11 |
| 4-year degree vs no college | 1.08 | 0.51, 2.28 | 0.85 |
| Graduate degree vs no college | 0.79 | 0.41, 1.53 | 0.49 |
| Surrogate: history vs no history of stroke | 2.80 | 1.68, 4.68 | <0.001 |
Unadjusted and adjusted models were tested using zero-inflated negative binomial regression. Abbreviations: CI, confidence interval; MCI, mild cognitive impairment; NC, normal cognition
Based on the Control Preferences Scale responses, the majority of patients wanted to make final or all medical decisions for themselves; fewer patients wanted SDM. Patients’ preferences for SDM for specific AMI and stroke treatments did not differ significantly by patient MCI diagnosis (Table 2). Most patients (92.4–100%) wanted to be involved in making specific AMI and stroke treatment decisions. The majority of surrogates preferred to make final or all medical decisions for themselves based on the Control Preferences Scale. Most surrogates wanted to be involved in making AMI and stroke treatment decisions for the patient.
DISCUSSION
We found no evidence that older patients with MCI, compared to those with NC, have different preferences for life-sustaining treatments except they desire more treatment in Alzheimer’s disease. Similar to patients with NC, most patients with MCI (80%) desired life-sustaining treatments in their current health. We also found no evidence that patients’ preferences for SDM generally and in AMI and stroke treatment decisions differed significantly by patient MCI diagnosis. In general, the majority of patients with MCI and NC wanted to make final medical decisions themselves. In the event of the patient having an AMI or stroke, most patients with MCI and NC wanted to participate in treatment decision-making.
Little research has compared patients’ treatment preferences between patients with MCI and NC. Prior studies suggest that physicians assume that patients with MCI, compared to patients with NC, prefer less treatment.21,22 Yet, we found no evidence that patients with MCI prefer less life-sustaining treatment than patients with NC in our study, contrary to our hypothesis. There was no evidence that patient MCI diagnosis modified the differences in treatment preferences between Black and White individuals, though our results show that Black patients and surrogates desired more treatment than White patients and surrogates, consistent with previous studies.42 We also found evidence that patients with a close family member/friend with stroke and surrogates with stroke were more likely to reject life-sustaining treatments in the health scenarios suggesting that stroke disability would decrease the desire for life-sustaining treatment.
Few studies have compared SDM preferences between patients with MCI and NC. A hypothetical scenario study suggested that older patients prefer increased family involvement in cancer treatment decision-making as their cognitive function worsens.43 We found no evidence that patients with MCI and NC have different patient-clinician SDM preferences generally and for specific AMI and stroke treatments. We were surprised that, in general, patients with MCI and NC preferred to make decisions (patient-driven decision-making) more frequently than patient-clinician SDM. We expected patient-clinician SDM to be the most common response. For that reason, we did not give the option of patients making the decisions for the AMI and stroke treatments. When having an AMI or stroke, most MCI and NC patients would prefer patient-clinician SDM to clinician-driven decision-making. Our results are consistent with research showing that people with MCI frequently want to participate in making medical decisions for themselves.44
We found surrogates’ preferences for patients’ treatment and SDM (generally and for AMI and stroke treatments) did not differ between patients with MCI and NC. Surrogates frequently participate in clinical visits of older adults with MCI, though their involvement can create communication challenges.45 Physicians also report more frequently involving surrogates in treatment decisions in patients with MCI than in those with NC.22 Some physicians assume that patients with MCI, compared to patients with NC, have impaired independent decision-making and cannot communicate their treatment preferences.21,22 Our results suggest that many patients with MCI can communicate their treatment preferences. Studies also show that many patients with MCI can participate in treatment decision-making.44 Research is needed to identify effective communication strategies and decision aids for clinicians, patients with MCI, and their surrogates.46
Our study had several strengths. The survey had a high response rate. We used validated measures of patient and surrogate treatment preferences and SDM. We confirmed that patients with MCI and NC and their surrogates could understand the survey using cognitive interviews. We included Black and White individuals in two different geographic regions of the country. Patients received MCI and NC diagnosis based on cognitive testing within 12 months, so it is unlikely that their cognitive status changed.
Our study had potential limitations. Results might not be generalizable to other populations, e.g., non-academic settings and non-volunteer populations. The LSPQ has hypothetical clinical scenarios, and how treatment preferences in hypothetical situations correlate to those in real-life situations including CVD events is unclear. We did not examine patient-surrogate concordance in treatment decision-making because studies43 have found low patient-surrogate concordance in treatment decision-making in patients with cognitive impairment. We did not assess religious beliefs or how respondents interpreted the impact of treatment decisions on survival and quality of life, factors that may be important to consider in future work. It is possible we were underpowered to detect clinically meaningful differences in LSPQ score between patients with MCI and NC.
Our study has clinical and policy implications. Patients with MCI should receive the guideline-concordant care they would want if adequately informed. Nevertheless, evidence suggests that patients with MCI get less guideline-concordant care for CVD and other conditions than patients with NC.17–19 We found no evidence that patients with MCI want less life-sustaining care than patients with NC. Our findings suggest that other provider and system factors (e.g., disparities and access to care issues) might contribute to patients with MCI getting less guideline-concordant care. Some preliminary evidence suggests that physicians recommend less care for CVD and other conditions to patients with MCI than to patients with NC.21,47 We are now performing a larger-scale national survey of physicians’ recommendations for CVD treatments in patients with NC, MCI, and dementia. In the meantime, our results suggest that clinicians should know that patients with MCI want the same treatment as patients with NC and patients are more likely to prefer patient-driven decision-making than patient-clinician SDM.
CONCLUSIONS
We did not find evidence that patients with MCI and their surrogates have different treatment preferences than patients with NC and their surrogates. These findings suggest that other provider and system factors rather than patient and surrogate treatment preferences might contribute to patients with MCI getting less guideline-concordant care than patients with NC.
Supplementary Information
(PDF 688 kb)
Acknowledgments
The authors appreciate the help of Ari Bhaumik, BA, and Theresa Gierzynski, LLMSW, in recruiting patients and surrogates, and the patients and surrogates who participated in the study.
Funding
Research reported in this publication was supported by the National Institute On Aging of the National Institutes of Health under Award Number R01AG051827 (Levine DA, PI).
All authors receive National Institutes of Health funding. Dr. Fagerlin receives American Heart Association funding. Dr. Galecki was supported by the National Institutes of Health/National Institute on Aging grant P30 AG024824 (R01 AG051827).
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Prior Presentations
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, et al. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148(6):427–34. doi: 10.7326/0003-4819-148-6-200803180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alzheimer’s Association 2020 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2020;16(3):391–460. doi: 10.1002/alz.12068. [DOI] [Google Scholar]
- 3.Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312(23):2551–61. doi: 10.1001/jama.2014.13806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med. 2014;275(3):214–28. doi: 10.1111/joim.12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farias ST, Mungas D, Reed BR, Harvey D, DeCarli C. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66(9):1151–7. doi: 10.1001/archneurol.2009.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia--meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119(4):252–65. doi: 10.1111/j.1600-0447.2008.01326.x. [DOI] [PubMed] [Google Scholar]
- 7.Fisk JD, Merry HR, Rockwood K. Variations in case definition affect prevalence but not outcomes of mild cognitive impairment. Neurology. 2003;61(9):1179–84. doi: 10.1212/01.WNL.0000089238.07771.C7. [DOI] [PubMed] [Google Scholar]
- 8.Larrieu S, Letenneur L, Orgogozo JM, Fabrigoule C, Amieva H, Le Carret N, et al. Incidence and outcome of mild cognitive impairment in a population-based prospective cohort. Neurology. 2002;59(10):1594–9. doi: 10.1212/01.WNL.0000034176.07159.F8. [DOI] [PubMed] [Google Scholar]
- 9.Yaffe K, Lindquist K, Vittinghoff E, Barnes D, Simonsick EM, Newman A, et al. The effect of maintaining cognition on risk of disability and death. J Am Geriatr Soc. 2010;58(5):889–94. doi: 10.1111/j.1532-5415.2010.02818.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sachs GA, Carter R, Holtz LR, Smith F, Stump TE, Tu W, et al. Cognitive impairment: an independent predictor of excess mortality: a cohort study. Ann Intern Med. 2011;155(5):300–8. doi: 10.7326/0003-4819-155-5-201109060-00007. [DOI] [PubMed] [Google Scholar]
- 11.Barrios H, Narciso S, Guerreiro M, Maroco J, Logsdon R, de Mendonca A. Quality of life in patients with mild cognitive impairment. Aging Ment Health. 2013;17(3):287–92. doi: 10.1080/13607863.2012.747083. [DOI] [PubMed] [Google Scholar]
- 12.Ready RE, Ott BR, Grace J. Patient versus informant perspectives of quality of life in mild cognitive impairment and alzheimer’s disease. Int J Geriatr Psychiatry. 2004;19(3):256–65. doi: 10.1002/gps.1075. [DOI] [PubMed] [Google Scholar]
- 13.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 14.Watson K, Fung CH, Budoff M. Quality indicators for the care of ischemic heart disease in vulnerable elders. J Am Geriatr Soc. 2007;55(Suppl 2):S366–72. doi: 10.1111/j.1532-5415.2007.01344.x. [DOI] [PubMed] [Google Scholar]
- 15.Cheng EM, Fung CH. Quality indicators for the care of stroke and atrial fibrillation in vulnerable elders. J Am Geriatr Soc. 2007;55(Suppl 2):S431–7. doi: 10.1111/j.1532-5415.2007.01352.x. [DOI] [PubMed] [Google Scholar]
- 16.Wenger NS, Solomon DH, Amin A, Besdine RK, Blazer DG, Cohen H, et al. Application of assessing care of vulnerable elders-3 quality indicators to patients with advanced dementia and poor prognosis. J Am Geriatr Soc. 2007;55(Suppl 2):S457–63. doi: 10.1111/j.1532-5415.2007.01375.x. [DOI] [PubMed] [Google Scholar]
- 17.Levine DA, Langa KM, Galecki A, Kabeto M, Morgenstern LB, Zahuranec DB, et al. Mild cognitive impairment and receipt of treatments for acute myocardial infarction in older adults. J Gen Intern Med. 2020;35(1):28–35. doi: 10.1007/s11606-019-05155-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gharacholou SM, Reid KJ, Arnold SV, Spertus J, Rich MW, Pellikka PA, et al. Cognitive impairment and outcomes in older adult survivors of acute myocardial infarction: findings from the translational research investigating underlying disparities in acute myocardial infarction patients’ health status registry. Am Heart J. 2011;162(5):860–9. doi: 10.1016/j.ahj.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stagg BC, Ehrlich JR, Choi H, Levine DA. Association of cognitive impairment and dementia with receipt of cataract surgery among community-dwelling Medicare beneficiaries. JAMA Ophthalmol. 2019;137(1):114–7. doi: 10.1001/jamaophthalmol.2018.5138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bagai A, Chen AY, Udell JA, Dodson JA, McManus DD, Maurer MS, et al. Association of cognitive impairment with treatment and outcomes in older myocardial infarction patients: A Report From the NCDR Chest Pain-MI Registry. J Am Heart Assoc. 2019;8(17):e012929. doi: 10.1161/JAHA.119.012929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levine DA, Langa KM, Fagerlin A, Morgenstern LB, Nallamothu BK, Forman J, et al. Physician decision-making and recommendations for stroke and myocardial infarction treatments in older adults with mild cognitive impairment. PLoS One. 2020;15(3):e0230446. doi: 10.1371/journal.pone.0230446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blair EM, Zahuranec DB, Langa KM, Forman J, Reale BK, Kollman C, et al. Impact of patient mild cognitive impairment on physician decision-making for treatment. J Alzheimers Dis. 2020;78(4):1409–17. doi: 10.3233/JAD-200700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maust DT, Solway E, Langa KM, Kullgren JT, Kirch M, Singer DC, et al. Perception of dementia risk and preventive actions among US adults aged 50 to 64 years. JAMA Neurol. 2020;77(2):259–62. doi: 10.1001/jamaneurol.2019.3946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roberts JS, Connell CM, Cisewski D, Hipps YG, Demissie S, Green RC. Differences between African Americans and whites in their perceptions of Alzheimer disease. Alzheimer Dis Assoc Disord. 2003;17(1):19–26. doi: 10.1097/00002093-200301000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Connell CM, Scott Roberts J, McLaughlin SJ, Akinleye D. Racial differences in knowledge and beliefs about Alzheimer disease. Alzheimer Dis Assoc Disord. 2009;23(2):110–6. doi: 10.1097/WAD.0b013e318192e94d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kahneman D. Thinking, Fast and Slow. New York: Farrar, Straus and Giroux; 2011. [Google Scholar]
- 27.Ostergren JE, Heeringa SG, Leon CFM, Connell CM, Roberts JS. The Influence of psychosocial and cognitive factors on perceived threat of Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2017;32(5):289–99. doi: 10.1177/1533317517714552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dillman DA. Mail and Internet surveys. The tailored design method-2007 update with new Internet, visual, and mixed-mode guide. Hoboken, New Jersey: John Wiley & Sons; 2011. [Google Scholar]
- 30.Ditto PH, Danks JH, Smucker WD, Bookwala J, Coppola KM, Dresser R, et al. Advance directives as acts of communication: a randomized controlled trial. Arch Intern Med. 2001;161(3):421–30. doi: 10.1001/archinte.161.3.421. [DOI] [PubMed] [Google Scholar]
- 31.Coppola KM, Ditto PH, Danks JH, Smucker WD. Accuracy of primary care and hospital-based physicians’ predictions of elderly outpatients’ treatment preferences with and without advance directives. Arch Intern Med. 2001;161(3):431–40. doi: 10.1001/archinte.161.3.431. [DOI] [PubMed] [Google Scholar]
- 32.Coppola KM, Bookwala J, Ditto PH, Lockhart LK, Danks JH, Smucker WD. Elderly adults’ preferences for life-sustaining treatments: the role of impairment, prognosis, and pain. Death Stud. 1999;23(7):617–34. doi: 10.1080/074811899200803. [DOI] [PubMed] [Google Scholar]
- 33.Seckler AB, Meier DE, Mulvihill M, Paris BE. Substituted judgment: how accurate are proxy predictions? Ann Intern Med. 1991;115(2):92–8. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]
- 34.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997;29(3):21–43. [PubMed] [Google Scholar]
- 35.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: the Health and Retirement Study (HRS) Int J Epidemiol. 2014;43(2):576–85. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 37.Piette JD, Rosland AM, Silveira M, Kabeto M, Langa KM. The case for involving adult children outside of the household in the self-management support of older adults with chronic illnesses. Chronic Illn. 2010;6(1):34–45. doi: 10.1177/1742395309347804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choi H, Schoeni RF, Langa KM, Heisler MM. Older adults’ residential proximity to their children: changes after cardiovascular events. J Gerontol B Psychol Sci Soc Sci. 2015;70(6):995–1004. doi: 10.1093/geronb/gbu076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choi H, Schoeni RF, Langa KM, Heisler MM. Spouse and child availability for newly disabled older adults: socioeconomic differences and potential role of residential proximity. J Gerontol B Psychol Sci Soc Sci. 2015;70(3):462–9. doi: 10.1093/geronb/gbu015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clark CM, Ewbank DC. Performance of the Dementia Severity Rating Scale: a caregiver questionnaire for rating severity in Alzheimer disease. Alzheimer Dis Assoc Disord. 1996;10(1):31–9. [PubMed] [Google Scholar]
- 41.Albert JM, Wang W, Nelson S. Estimating overall exposure effects for zero-inflated regression models with application to dental caries. Stat Methods Med Res. 2014;23(3):257–78. doi: 10.1177/0962280211407800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Orlovic M, Smith K, Mossialos E. Racial and ethnic differences in end-of-life care in the United States: evidence from the Health and Retirement Study (HRS) SSM Popul Health. 2019;7:100331. doi: 10.1016/j.ssmph.2018.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shin DW, Cho J, Roter DL, Kim SY, Park JH, Yang HK, et al. Patient’s cognitive function and attitudes towards family involvement in cancer treatment decision making: a patient-family caregiver dyadic analysis. Cancer Res Treat. 2018;50(3):681–90. doi: 10.4143/crt.2017.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Daly RL, Bunn F, Goodman C. Shared decision-making for people living with dementia in extended care settings: a systematic review. BMJ Open. 2018;8(6):e018977. doi: 10.1136/bmjopen-2017-018977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vick JB, Amjad H, Smith KC, Boyd CM, Gitlin LN, Roth DL, et al. "Let him speak:" a descriptive qualitative study of the roles and behaviors of family companions in primary care visits among older adults with cognitive impairment. Int J Geriatr Psychiatry. 2018;33(1):e103–e12. doi: 10.1002/gps.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Green AR. How can we optimize care and outcomes for patients with mild cognitive impairment and acute myocardial infarction? J Gen Intern Med. 2020;35(1):5–7. doi: 10.1007/s11606-019-05484-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Grant EV, Summapund J, Matlock DD, Vaughan Dickson V, Iqbal S, Patel S, et al. Patient and cardiologist perspectives on shared decision making in the treatment of older adults hospitalized for acute myocardial infarction. Med Decis Making. 2020;40(3):279–88. doi: 10.1177/0272989X20912293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 688 kb)