Abstract
This study aims to determine the resilience level and its influence on anxiety among Chinese lumbar disc herniation (LDH) patients, and to determine the critical psychological and non-psychological predictors of resilience among LDH patients. Twenty hundred and fifty LDH patients from a tertiary hospital in Jinzhou, China were included in this survey to answer the Resilience Scale-14 (RS-14), Zung Self-Rating Anxiety Scale (SAS), Herth Hope Index (HHI), Revised Life Orientation Test (LOT-R), Multidimensional Scale of Perceived Social Support (MSPSS), Perceived Stress Scale-10 (PSS-10). The mean resilience level of LDH patients was 61.96 ± 12.37. Resilience was negatively correlated with anxiety (χ2 = 32.603, p < 0.001), accompanied by a significant linear trend (χ2 = 28.567, p < 0.001). Hope, stress, social support, and medical payment type accounted for 48.7% resilience variance. This study reveals that Chinese LDH patients had low resilience level, and that lower level of resilience was closely associated with higher anxiety level. The predictors for resilience among LDH patients include hope, stress, social support, as well as medical payment types. These findings provide local government and related health-care professionals with a basis for development of targeted mental health management of Chinese LDH patients, and will also help to devise appropriate health intervention strategies for promoting the mental health status of LDH patients.
Keywords: Lumbar disc herniation, Resilience, Anxiety, Hope, Social support
Lumbar disc herniation; Resilience; Anxiety; Hope; Social support.
1. Introduction
Lumbar disc herniation (LDH) is the most common spinal disc herniation, accounting for 50% of low back pain (LBP) (Engel-Yeger et al., 2018). LDH may cause physical distress and the affected individuals would feel pain in the leg, foot, lower back, and/or buttock. They would also experience numbness, weakness, and/or tingling in the leg and/or foot. Severe LDH even triggers the loss of bladder and bowel control, leads to serious physical impairment, and greatly decreased the quality of life of the victims (Kose and Hatipoglu, 2012; Yao et al., 2020). In addition to physical disabilities, mental distress also represents a major aspect of the decreased quality of life (QOL) of LDH patients (Engel-Yeger et al., 2018). The patients are supposed to experience frequent mental distress. In a recent study conducted in China, it was shown that the prevalence of depression and anxiety among LDH was 33.3% and 37.6%, respectively (Mu et al., 2019). Studies elsewhere likewise suggested that emotional distress, depression, and anxiety are the common psychological problems in LDH patients (Boakye et al., 2013; Chen and Tsai, 2013; Lebow et al., 2012). Notably, Batya et al. suggested that mental distress might play a more important role in impaired QOL of LDH patients (Engel-Yeger et al., 2018). Thus, effectively addressing and responding to psychological distress in LDH patients would reasonably benefit the improvement of their QOL.
Mental resilience, or resilience in short, is an extremely important psychological feature in individuals and can be defined as an individual's ability to properly handle tragedy, trauma, adversity, or other life- and workplace-related unfavorable events (Jia et al., 2020). Generally, patients with higher level of resilience show better psychological adaptation and have higher QOL (Mohlin et al., 2021). As such, resilience improvement is considered as an effective strategy for improving psychological symptoms among patients with various chronic diseases. Studies showed that resilience level was negatively or positively influenced by many psychological and non-psychological factors, such as assets, resources, family, hope, stress, optimism, and support system, etc (Gao et al., 2019; Zhong et al., 2016). As of now, however, little information is available regarding resilience among LDH patients.
In the current work, we aim to evaluate the resilience status in LDH patients with varied sociodemographic characteristics, and to address its influence on anxiety severity in LDH patients. Besides, the relationship between resilience level and other psychological variables, including hope, social support, stress, and optimism was also analyzed in LDH patients. Through these analyses, we hope to identify predictors of resilience so as to help provide a basis for effective management of the mental health level of LDH patients.
2. Methods
2.1. Participants
A cross-sectional study was conducted among 250 LDH patients recruited from a tertiary hospital in Jinzhou, Liaoning Province, Northeast China between January 2020 and June 2021. All the participants were informed beforehand regarding the purpose and process of this investigation. After they agreed to participate in this study and provided their written informed consent, investigators assigned the questionnaires to them. They were also informed to complete the questionnaires voluntarily and anonymously and have the right to withdraw from this survey at any time out of any reason. Inclusion criteria included: aged 18 years or over; LDH diagnosed for the first time during the past one to five years; aware of their own diagnosis but without a history of previous treatment; speaking and understanding mandarin (standard spoken Chinese). Patients having psychiatric history or cognitive deficits, with previous back surgery, having other osteoarthropathies, or not sufficiently literate were excluded from this study. This study was reviewed and approved by the Ethics Committee of Jinzhou Medical University, China. All procedures met the 1964 Helsinki declaration and its later amendments.
2.2. Measurement of resilience
Patients' resilience was assessed by the Resilience Scale-14 (RS-14) (Tian and Hong, 2013). Each item adopted a 7-point Likert rating method ranging from “strongly disagree” to “strongly agree”. Higher RS-14 scoring means better resilience level. The participants with RS-14 scoring ≤63, between 64–73, and ≥74 were regarded as lowly, moderately, and highly resilient, respectively as demonstrated in previous reports (Gao et al., 2019). RS-14 showed satisfactory reliability and validity in the Chinese cultural context (Chen et al., 2020; Gao et al., 2019; Tian and Hong, 2013). In this survey, Cronbach's α coefficient of internal consistency of this scale was 0.941.
2.3. Measurement of hope
The Herth Hope Index (HHI) (Herth, 1991) was applied to measure hope among LDH patients. This 12-item scale measures three different domains of hope: temporality and future, positive readiness and expectancy, and interconnectedness. Each item was scored ranging from 1 to 4, with higher scores indicating higher level of hope. HHI had been widely used and showed good reliability and validity in China (Gao et al., 2019; Li et al., 2018; Wang et al., 2019; Zhong et al., 2021). In this survey, Cronbach's α coefficient of internal consistency of this scale was 0.816.
2.4. Measurement of perceived social support
The level of social support of the participants was evaluated using the Multidimensional Scale of Perceived Social Support (MSPSS) (Dahlem et al., 1991). This scale contained 12 items measuring perceived social support from family, friends and significant others. Each item was rated from 1 (very strongly disagree) to 7 (very strongly agree). The total score ranged from 12 to 84 with higher indicating higher level of social support. The Chinese version of MSPSS exhibited good reliability and validity (Li et al., 2020, 2021b; Yang et al., 2020). In this survey, Cronbach's α coefficient of internal consistency of this scale was 0.949.
2.5. Measurement of optimism
The Revised Life Orientation Test (LOT-R) (He et al., 2013; Zhang et al., 2020) was used for measurement of optimism. This scale consists of 6 items, with 3 items measuring individual differences in dispositional optimism, and 3 items measuring pessimism. Each item was rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). A higher total score means a higher level of optimism. LOT-R showed good reliability and validity in the Chinese cultural context (Tang et al., 2020). In this survey, Cronbach's α coefficient of internal consistency of this scale was 0.739.
2.6. Measurement of perceived stress
Perceived stress of the participants during the last month was evaluated using Perceived Stress Scale-10 (PSS-10) (Wang et al., 2011). The items were rated on a 5-point Likert scale and the composite score ranged from 0 to 40. Higher PSS-10 total score means greater level of perceived stress. The Chinese version of PSS-10 demonstrated satisfactory reliability and validity (Liu et al., 2021; Wang et al., 2021a; Zhang et al., 2021). In this survey, Cronbach's α coefficient of internal consistency of this scale was 0.722.
2.7. Measurement of anxiety symptoms
The prevalence and severity of anxiety was assessed by the Zung Self-Rating Anxiety Scale (SAS) (Zung, 1971) among the recruited LDH patients. Each item was scored on a 4-point Likert scale. The total raw score was transformed into the standardized score int (1.25 × raw score) for subsequent analysis, with higher scoring indicating more severe anxiety symptom. Based on previous studies, standardized score between 50-59, between 60-69, and ≥70 represented mild, moderate, and severe anxiety level, respectively (Zhu et al., 2021). The Chinese version of SAS showed good reliability and validity (Gao et al., 2012; Li et al., 2021a; Wang et al., 2021b). In this survey, Cronbach's α coefficient of internal consistency of this scale was 0.840.
2.8. Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Science (SPSS, version 20.0). Descriptive statistics for sociodemographic variables and distribution of different level of anxiety are presented as frequencies and percentages. Continuous variables that measure various psychological indexes were shown as mean (SD, standard deviation). Student's t-test and one-way analysis of variance (ANOVA) were used for comparison of resilience level in subjects with different sociodemographic characteristics. Pearson's correlation analysis was conducted for examination of the correlation among continuous variables. Hierarchical linear regression was used for predicting resilience with sociodemographic variables significant in univariate analysis as control variables, and psychological factors as independent variables. Kruskal-Wallis H test was conducted for determining whether patients with different level of resilience had different anxiety severity. In addition, the linear trend between resilience and anxiety was analyzed by Cochran-Mantel-Haenszel test.
3. Results
3.1. Descriptive statistics and resilience level comparison
As shown in Table 1, of the 250 invited LDH patients, 109 (43.6%) were males, and 208 (83.2%) were under 60 years. Mean age was 44.24 years (SD = 15.36, rang 19–83). 76 (30.4%) of all patients reported at least one comorbid chronic disease. Resilience was significantly different among participants with varied demographic characteristics including marriage (F = 4.474, p = 0.004), body mass index (BMI) (F = 7.667, p = 0.001), education (F = 6.202, p < 0.001), job status (F = 3.949, p = 0.009), income (F = 5.271, p = 0.002), residence (t = -2.881, p = 0.005), medical payment types (t = 3.021, p = 0.003), and with comorbid chronic diseases (t = 3.250, p = 0.001).
Table 1.
Sociodemographic characteristics and the level of resilience among patients with lumbar disc herniation (n = 250).
| Variables | N (%) | Resilience |
||
|---|---|---|---|---|
| Mean (SD) | t/F | P | ||
| Age | 1.112 | 0.267 | ||
| <60 years | 208 (83.2) | 62.35 (12.61) | ||
| ≥60 years | 42 (16.8) | 60.02 (11.08) | ||
| Gender | 0.560 | 0.576 | ||
| Male | 109 (43.6) | 62.46 (12.78) | ||
| Female | 141 (56.4) | 61.57 (12.08) | ||
| Marriage | 4.474 | 0.004 | ||
| Married | 139 (55.6) | 63.40 (11.01) | ||
| Single | 69 (27.6) | 62.81 (13.02) | ||
| Divorced | 25 (10.0) | 56.68 (15.24) | ||
| Widowed | 17 (6.8) | 54.53 (11.98) | ||
| BMI | 7.667 | 0.001 | ||
| <18.5 | 18 (7.2) | 52.33 (14.43) | ||
| 18.5–23.9 | 169 (67.6) | 63.54 (11.54) | ||
| ≥24 | 63 (25.2) | 60.48 (12.68) | ||
| Education | 6.202 | <0.001 | ||
| Primary school | 13 (5.2) | 52.85 (13.71) | ||
| Junior high school | 53 (21.2) | 58.79 (11.49) | ||
| High school | 100 (40.0) | 61.83 (11.18) | ||
| College or university | 84 (33.6) | 65.52 (12.96) | ||
| Job status | 3.949 | 0.009 | ||
| Employee | 143 (57.2) | 63.69 (12.69) | ||
| Retirement | 60 (24.0) | 60.15 (10.26) | ||
| Unemployed | 14 (5.6) | 53.00 (14.32) | ||
| Other | 33 (13.2) | 61.58 (12.04) | ||
| Income | 5.271 | 0.002 | ||
| <2000 | 19 (7.6) | 54.84 (11.81) | ||
| 2000–3000 | 117 (46.8) | 60.57 (11.18) | ||
| 3001–4000 | 94 (37.6) | 63.78 (12.26) | ||
| >4000 | 20 (8.0) | 68.30 (15.97) | ||
| Residence | -2.881 | 0.005 | ||
| Urban | 195 (78.0) | 63.29 (11.45) | ||
| Rural | 55 (22.0) | 57.24 (14.36) | ||
| Smoking | 0.252 | 0.801 | ||
| No | 134 (53.6) | 61.78 (11.17) | ||
| Yes | 116 (46.4) | 62.17 (13.68) | ||
| Drinking alcohol | -1.485 | 0.139 | ||
| No | 150 (60.0) | 62.91 (11.97) | ||
| Yes | 100 (40.0) | 60.54 (12.88) | ||
| Family history | 1.957 | 0.051 | ||
| No | 190 (76.0) | 62.82 (12.49) | ||
| Yes | 60 (24.0) | 59.25 (11.67) | ||
| Medical payments types | 3.021 | 0.003 | ||
| Insurance | 209 (83.6) | 62.99 (11.75) | ||
| Self-pay | 41 (16.4) | 56.71 (14.20) | ||
| Comorbid chronic disease | 3.250 | 0.001 | ||
| Without | 174 (69.6) | 63.61 (11.58) | ||
| With | 76 (30.4) | 58.18 (13.34) | ||
Figures in bold represent being statistically significant (P < 0.05).
3.2. Correlation analysis
Table 2 presented the correlation between resilience, hope, perceived social support, optimism, and perceived stress. Resilience had negative association with perceived stress (r = -0.450, p < 0.01), and positive association with hope (r = 0.576, p < 0.01), perceived social support (r = 0.653, p < 0.01), and optimism (r = 0.265, p < 0.01).
Table 2.
Descriptive statistics and correlations among continuous variables (n = 250).
| Variables | Mean | SD | Resilience | Hope | Social support | Optimism |
|---|---|---|---|---|---|---|
| Resilience | 61.96 | 12.37 | 1 | |||
| Hope | 34.92 | 4.88 | 0.576∗∗ | 1 | ||
| Perceived social support | 58.24 | 11.20 | 0.653∗∗ | 0.662∗∗ | 1 | |
| Optimism | 20.65 | 3.61 | 0.265∗∗ | 0.396∗∗ | 0.198∗∗ | 1 |
| Perceived stress | 18.38 | 5.23 | -0.450∗∗ | -0.495∗∗ | -0.447∗∗ | -0.339∗∗ |
∗∗P < 0.01 (two-tailed).
3.3. Hierarchical linear regression analysis
Table 3 showed that hope (β = 0.142, p = 0.039), perceived stress (β = -0.117, p = 0.034), and perceived social support (β = 0.458, p < 0.001) significantly related to the resilience level of LDH patients. These three variables, alongside with medical payment types accounted for 48.7% resilience variance, with 36.1% (48.7% minus 12.6%) were explained by the psychological variables.
Table 3.
Hierarchical linear regression analysis for the predictors of resilience (n = 250).
| Variables | Resilience |
|||
|---|---|---|---|---|
| β | P | β | P | |
| Step 1 | ||||
| Marriage | -0.104 | 0.114 | -0.043 | 0.398 |
| Education | 0.132 | 0.056 | 0.063 | 0.235 |
| Job status | 0.079 | 0.201 | 0.056 | 0.250 |
| Income | 0.146 | 0.036 | -0.028 | 0.608 |
| Residence | 0.079 | 0.217 | 0.036 | 0.471 |
| BMI | 0.038 | 0.536 | -0.047 | 0.326 |
| Medical payments types | -0.133 | 0.031 | -0.116 | 0.015 |
| Comorbid chronic diseases | -0.101 | 0.121 | -0.059 | 0.235 |
| Step 2 | ||||
| Hope | 0.142 | 0.039 | ||
| Perceived stress | -0.117 | 0.034 | ||
| Optimism | 0.082 | 0.119 | ||
| Perceived social support | 0.458 | <0.001 | ||
| F value | 5.507 | 20.736 | ||
| p value | 0.000 | 0.000 | ||
| R2 | 0.155 | 0.512 | ||
| Adjusted R2 | 0.126 | 0.487 | ||
Figures in bold represent being statistically significant (P < 0.05).
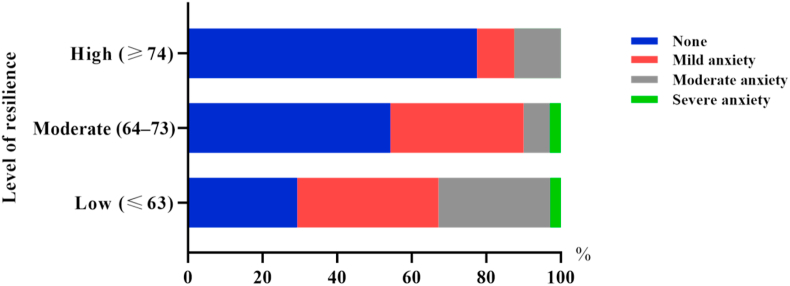
3.4. Influence of resilience on anxiety among LDH patients
Kruskal-Wallis H test was conducted for examining the potential impact of resilience on anxiety among LDH patients. As shown in Figure 1, 56.0% (140/250) LDH patients reported mild to severe anxiety symptoms. Notably, the data revealed that anxiety level of the participants differed with different resilience levels. In the low, moderate, and high resilience groups, the prevalence of anxiety was 70.7%, 45.7%, and 22.5%, respectively (χ2 = 32.603, p < 0.001). In addition, a significant linear tendency between resilience and anxiety was revealed by the Cochran-Mantel-Haenszel test among the LDH participants (χ2 = 28.567, p < 0.001).
Figure 1.
Degree of anxiety among patients with different levels of resilience (n = 250).
4. Discussion
In this survey, we have for the first time presented data regarding the resilience level and its predictors among Chinese LDH patients. Chinese LDH patients had low level of resilience, and less resilient LDH patients reported higher level of anxiety. Demographical variables including marriage, BMI, education, job status, income, residence, medical payment types, and whether having comorbid chronic diseases were significantly related to resilience. In addition, it was found that resilience was positively associated with hope, social support, optimism, and negatively with stress. Hope, stress, social support, and medical payment types independently predicted the resilience level in LDH patients.
Chinese LDH patients reported a resilience mean score of 61.96 ± 12.37, demonstrating a low level of resilience among LDH patients as per the previously determined cutoff scores (Tian and Hong, 2013). Although the impaired psychological state has been commonly documented in previous studies (Yüksel et al., 2021), this, as far as we know, might be the first report revealing resilience level among LDH patients. Since resilience-promoting strategies can help individuals overcome adversity, stress, and setbacks (Luo et al., 2021; Muniandy et al., 2021), we thus reasonably argue that increasing the resilience level would represent a highly effective avenue to improvement of the mental health of LDH patients based on the negative correlation between resilience and anxiety in LDH patients as revealed in the present study.
Previously it was reported that patients with disc herniation experienced high level of psychological stress, including anxiety (Cici and Özkan, 2021). Our findings regarding the correlation between anxiety and resilience levels in LDH patients herein showed that anxiety among LDH patients were inversely correlated with resilience, demonstrating that high resilience level might have better psychological adaption when confronted with this disorder. Similarly, the inverse correlation between resilience and anxiety has also been revealed in patients with other types of diseases (Gao et al., 2019). Obviously, resilience can be regarded as a common protection against psychological distress among diverse chronic conditions. In this sense, we argue that promoting resilience might represent a useful intervention for the alleviation of anxiety level among LDH patients. Actually, existing data have strongly advocated the incorporation of resilience-promoting intervention into the management of psychological well-being when confronted with diverse adversities (Luo et al., 2021).
This study demonstrated that hope, stress, social support, as well as medical payment types were major predictive factors for the resilience level of LDH patients. These four variables explained 48.7% resilience variance in total. Among the four significant predictors, social support exhibited the highest association with resilience (β = 0.458, P < 0.001). As far as we know, this is the first report regarding the analysis of potential influencing factors of resilience among LDH patients, which may have theoretical and clinical implications for the mental health management of LDH patients.
The close association between social support and resilience in LDH was also seen in other disease types. For example, a recent study showed that social support system and inclusive environment are important external factors contributing to resilience among youths (Shahram et al., 2021). In another report, it was shown that social support functioned as an important protective factor predicting child resilience in a community-based cohort facing flood as natural disaster (Arshad et al., 2020). The protection of adequate social support on resilience and against behavioral problems was also documented in 6∼8-years-old children (Cabaj et al., 2014). In view of the foremost predictive contribution of perceived social support to resilience as demonstrated in our study, strategies to foster social support are strongly suggested to be preferentially included in resilience-promoting intervention.
The association between hope and resilience has been seen in patients diagnosed with oral cancer, although no significant correlation was found between perceived stress and resilience among these patients (Gao et al., 2019). However, in bladder and renal cancer patients, psychological stress had a significant prediction on resilience (Li and Wang, 2016). As for our study, we found these two psychological variables both had a certain degree of predictive effect on resilience level of LDH patients. Based on this finding, promoting hope level and alleviating psychological stress might represent effective avenues to improved resilience and mental health level.
In our present study, medical payment type was the only significant sociodemographic variable for resilience level prediction among LDH patients. LDH/LBP patient are generally subjected to enormous economic burden (Scaturro et al., 2020; Sconza et al., 2021), which inevitably would decrease their resilience level, and thereby provoke anxiety symptoms. Based on our data, Healthcare services should pay more attention to those LDH patients without medical insurance, as this subgroup might have lower resilience and correspondingly higher anxiety level.
There exist several major limitations in this study. Firstly, the research design was cross-sectional, and any causal relationship cannot be drawn from our data. Future longitudinal and intervention studies are warranted to further confirm our conclusion. Secondly, in the future more psychological variables should be included in this study so as to more fully identify the predictors of resilience of LDH patients. In addition, a lager-sample size and multicenter studies are needed to decrease bias. The study, albeit these limitations, does provide valuable information regarding the resilience status and associated predictors of resilience among Chinese LDH patients, which would help develop precise and effective intervention strategies so as to improve anxiety severity among LDH patients.
5. Conclusion
The present study showed that overall Chinese LDH patients had low level of resilience, which was closely associated with higher anxiety level. The predictors for resilience among LDH patients include hope, stress, social support, as well as medical payment types. These findings provide local government and related health-care professionals with a basis for development of targeted mental health management of Chinese LDH patients, and will also help to devise appropriate health intervention strategies for promoting the mental health status of LDH patients.
Declarations
Author contribution statement
Yuqiang Zhang: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Hongliang Dai: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Yuying Chu: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Xue Wang; Chunguang Liang; Suyan Wang; Wenhui Li: Performed the experiments; Contributed reagents, materials, analysis tools or data.
Guizhi Jia: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This work was supported by Project of Scientific Research Funding of Department of Education of Liaoning Province (No. JYTJCZR2020079), and the School-Enterprise Partnership Program of Jinzhou Medical University (No. 2021004).
Data availability statement
Data included in article/supplementary material/referenced in article.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We thank all the participants taking part in this survey.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Arshad M., Mughal M.K., Giallo R., Kingston D. Predictors of child resilience in a community-based cohort facing flood as natural disaster. BMC Psychiatr. 2020;20(1):543. doi: 10.1186/s12888-020-02944-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boakye M., Moore R., Kong M., Skirboll S.L., Arrigo R.T. Health-related quality-of-life status in Veterans with spinal disorders. Qual. Life Res. 2013;22(1):45–52. doi: 10.1007/s11136-012-0121-y. [DOI] [PubMed] [Google Scholar]
- Cabaj J.L., McDonald S.W., Tough S.C. Early childhood risk and resilience factors for behavioural and emotional problems in middle childhood. BMC Pediatr. 2014;14:166. doi: 10.1186/1471-2431-14-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H.N., Tsai Y.F. A predictive model for disability in patients with lumbar disc herniation. J. Orthop. Sci. 2013;18(2):220–229. doi: 10.1007/s00776-012-0354-1. [DOI] [PubMed] [Google Scholar]
- Chen W., Xie E., Tian X., Zhang G. Psychometric properties of the Chinese version of the resilience scale (RS-14): preliminary results. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0241606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cici R., Özkan M. Altern Ther Health Med; 2021. Effects on Anxiety and Vital Signs of the Emotional Freedom Technique and Music before Surgery for Lumbar Disc Hernia. AT6442. Online ahead of print. [PubMed] [Google Scholar]
- Dahlem N.W., Zimet G.D., Walker R.R. The multidimensional scale of perceived social support: a confirmation study. J. Clin. Psychol. 1991;47(6):756–761. doi: 10.1002/1097-4679(199111)47:6<756::aid-jclp2270470605>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Engel-Yeger B., Keren A., Berkovich Y., Sarfaty E., Merom L. The role of physical status versus mental status in predicting the quality of life of patients with lumbar disk herniation. Disabil. Rehabil. 2018;40(3):302–308. doi: 10.1080/09638288.2016.1253114. [DOI] [PubMed] [Google Scholar]
- Gao Y., Yuan L., Pan B., Wang L. Resilience and associated factors among Chinese patients diagnosed with oral cancer. BMC Cancer. 2019;19(1):447. doi: 10.1186/s12885-019-5679-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Y.Q., Pan B.C., Sun W., Wu H., Wang J.N., Wang L. Anxiety symptoms among Chinese nurses and the associated factors: a cross sectional study. BMC Psychiatr. 2012;12:141. doi: 10.1186/1471-244X-12-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He F., Cao R., Feng Z., Guan H., Peng J. The impacts of dispositional optimism and psychological resilience on the subjective well-being of burn patients: a structural equation modelling analysis. PLoS One. 2013;8(12) doi: 10.1371/journal.pone.0082939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herth K. Development and refinement of an instrument to measure hope. Sch. Inq. Nurs. Pract. 1991;5(1):39–51. discussion 53-36. [PubMed] [Google Scholar]
- Jia G., Li X., Chu Y., Dai H. Function of family of origin and current quality of life: exploring the mediator role of resilience in Chinese patients with type 2 diabetes. Int. J. Diabetes Dev. Ctries. 2020;41(9):1–8. [Google Scholar]
- Kose G., Hatipoglu S. The effect of low back pain on the daily activities of patients with lumbar disc herniation: a Turkish military hospital experience. J. Neurosci. Nurs. 2012;44(2):98–104. doi: 10.1097/JNN.0b013e3182478e57. [DOI] [PubMed] [Google Scholar]
- Lebow R., Parker S.L., Adogwa O., Reig A., Cheng J., Bydon A., McGirt M.J. Microdiscectomy improves pain-associated depression, somatic anxiety, and mental well-being in patients with herniated lumbar disc. Neurosurgery. 2012;70(2):306–311. doi: 10.1227/NEU.0b013e3182302ec3.. [DOI] [PubMed] [Google Scholar]
- Li L., Wu X.L., Xu L. Factors affecting self-perceived participation and autonomy among patients with burns: a follow-up study. Burns. 2018;44(8):2064–2073. doi: 10.1016/j.burns.2018.07.008. [DOI] [PubMed] [Google Scholar]
- Li M., Wang L. The associations of psychological stress with depressive and anxiety symptoms among Chinese bladder and renal cancer patients: the mediating role of resilience. PLoS One. 2016;11(4) doi: 10.1371/journal.pone.0154729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T., Sun S., Liu B., Wang J., Zhang Y., Gong C., Duan J. Prevalence and risk factors for anxiety and depression in patients with COVID-19 in wuhan, China. Psychosom. Med. 2021;83(4):368–372. doi: 10.1097/PSY.0000000000000934. [DOI] [PubMed] [Google Scholar]
- Li X.Y., Wang J., Zhang R.X., Chen L., He C.K., Wang C.Y., Ke J.J., Wang Y.L., Zhang Z.Z., Song X.M. Psychological status among anesthesiologists and operating room nurses during the outbreak period of COVID-19 in wuhan, China. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.574143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Zhang W., Ye M., Zhou L. Perceived participation and autonomy post-stroke and associated factors: an explorative cross-sectional study. J. Adv. Nurs. 2021;77(3):1293–1303. doi: 10.1111/jan.14670. [DOI] [PubMed] [Google Scholar]
- Liu Y., Chen H., Zhang N., Wang X., Fan Q., Zhang Y., Huang L., Hu B., Li M. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J. Affect. Disord. 2021;278:144–148. doi: 10.1016/j.jad.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y.H., Xia W., He X.L., Zhang J.P., Li H.C.W. Psychological interventions for enhancing resilience in parents of children with cancer: a systematic review and meta-analysis. Support. Care Cancer. 2021;29(11):7101–7110. doi: 10.1007/s00520-021-06344-0. [DOI] [PubMed] [Google Scholar]
- Mohlin Å., Bendahl P.O., Hegardt C., Richter C., Hallberg I.R., Rydén L. Psychological resilience and health-related quality of life in 418 Swedish women with primary breast cancer: results from a prospective longitudinal study. Cancers. 2021;13(9):2233. doi: 10.3390/cancers13092233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mu W., Shang Y., Zhang C., Tang S. Analysis of the depression and anxiety status and related risk factors in patients with lumbar disc herniation. Pakistan J. Med. Sci. 2019;35(3):658–662. doi: 10.12669/pjms.35.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muniandy M., Richdale A.L., Arnold S.R.C., Trollor J.N., Lawson L.P. Inter-relationships between trait resilience, coping strategies, and mental health outcomes in autistic adults. Autism Res. 2021;14(10):2156–2168. doi: 10.1002/aur.2564. [DOI] [PubMed] [Google Scholar]
- Scaturro D., Asaro C., Lauricella L., Tomasello S., Varrassi G., Letizia Mauro G. Combination of rehabilitative therapy with ultramicronized palmitoylethanolamide for chronic low back pain: an observational study. Pain Ther. 2020;9(1):319–326. doi: 10.1007/s40122-019-00140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sconza C., Braghetto G., Respizzi S., Morenghi E., Kon E., Di Matteo B. Ultrasound-guided periradicular oxygen-ozone injections as a treatment option for low back pain associated with sciatica. Int. Orthop. 2021;45(5):1239–1246. doi: 10.1007/s00264-021-04975-w. [DOI] [PubMed] [Google Scholar]
- Shahram S.Z., Smith M.L., Ben-David S., Feddersen M., Kemp T.E., Plamondon K. Promoting "Zest for life": a systematic literature review of resiliency factors to prevent youth suicide. J. Res. Adolesc. 2021;31(1):4–24. doi: 10.1111/jora.12588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang L., Li Z., Pang Y. The differences and the relationship between demoralization and depression in Chinese cancer patients. Psycho Oncol. 2020;29(3):532–538. doi: 10.1002/pon.5296. [DOI] [PubMed] [Google Scholar]
- Tian J., Hong J.S. Validation of the Chinese version of the resilience scale and its cutoff score for detecting low resilience in Chinese cancer patients. Support. Care Cancer. 2013;21(5):1497–1502. doi: 10.1007/s00520-012-1699-x. [DOI] [PubMed] [Google Scholar]
- Wang C., Lin S., Ma Y., Wang Y. The mediating effect of social support on the relationship between perceived stress and quality of life among shidu parents in China. Health Qual. Life Outcome. 2021;19(1):104. doi: 10.1186/s12955-021-01726-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Xu W., Ren L., Wang W., Wang Y. The relationship between hope and post-traumatic stress disorder in Chinese shidu parents: the mediating role of perceived stress. J. Affect. Disord. 2019;251:23–30. doi: 10.1016/j.jad.2019.03.049. [DOI] [PubMed] [Google Scholar]
- Wang X., Tao J., Zhu Q., Wu X., Li T., Zhao C., Yang W., Wang X., Zhang J., Guan N. Depression and anxiety symptoms to COVID-19 outbreak among the public, medical staff and patients during the initial phase of the pandemic: an online questionnaire survey by a WeChat Mini Program. BMJ Open. 2021;11(6) doi: 10.1136/bmjopen-2020-046350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Chen J., Boyd J.E., Zhang H., Jia X., Qiu J., Xiao Z. Psychometric properties of the Chinese version of the perceived stress scale in policewomen. PLoS One. 2011;6(12) doi: 10.1371/journal.pone.0028610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C., Zhou Y., Xia M. How resilience promotes mental health of patients with DSM-5 substance use disorder? The mediation roles of positive affect, self-esteem, and perceived social support. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.588968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao M., Xu B.P., Li Z.J., Zhu S., Tian Z.R., Li D.H., Cen J., Cheng S.D., Wang Y.J., Guo Y.M., Cui X.J. A comparison between the low back pain scales for patients with lumbar disc herniation: validity, reliability, and responsiveness. Health Qual. Life Outcome. 2020;18(1):175. doi: 10.1186/s12955-020-01403-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yüksel A., Çetinkaya F., Karakoyun A. The effect of mindfulness-based therapy on psychiatric symptoms, psychological well-being, and pain beliefs in patients with lumbar disk herniation. Psychiatr. Care. 2021;57(1):335–342. doi: 10.1111/ppc.12568. [DOI] [PubMed] [Google Scholar]
- Zhang T., Wei Q., Ma S.Y., Li H.P. The relationship between optimism and job satisfaction for Chinese specialist nurses: a serial-multiple mediation model. Jpn. J. Nurs. Sci. 2020;17(3) doi: 10.1111/jjns.12334. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Cui C., Wang L., Yu X., Wang Y., Wang X. The mediating role of hope in the relationship between perceived stress and post-traumatic stress disorder among Chinese patients with oral cancer: a cross-sectional study. Cancer Manag. Res. 2021;13:393–401. doi: 10.2147/CMAR.S281886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong G.Q., Lin B.H., Xiao C.X. Hope levels and resilience in patients with severe novel coronavirus pneumonia: the current situation and a correlation analysis. Int. J. Gen. Med. 2021;14:1959–1965. doi: 10.2147/IJGM.S301128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong X., Wu D., Nie X., Xia J., Li M., Lei F., Lim H.A., Kua E.H., Mahendran R. Parenting style, resilience, and mental health of community-dwelling elderly adults in China. BMC Geriatr. 2016;16:135. doi: 10.1186/s12877-016-0308-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Su L., Zhou Y., Qiao J., Hu W. The effect of nationwide quarantine on anxiety levels during the COVID-19 outbreak in China. Brain Behav. 2021;11(1) doi: 10.1002/brb3.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zung W.W. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supplementary material/referenced in article.