Abstract
In order to expand the promise of regenerative medicine using allogeneic induced pluripotent stem cells (iPSCs), precise and efficient genome editing of human leukocyte antigen (HLA) genes would be advantageous to minimize the immune rejection caused by mismatches of HLA type. However, clinical-grade genome editing of multiple HLA genes in human iPSC lines remains unexplored. Here, we optimized the protocol for good manufacturing practice (GMP)-compatible CRISPR-Cas9 genome editing to deplete the three gene locus (HLA-A, HLA-B, and CIITA genes) simultaneously in HLA homozygous iPSCs. The use of HLA homozygous iPSCs has one main advantage over heterozygous iPSCs for inducing biallelic knockout by a single gRNA. RNA-seq and flow cytometry analyses confirmed the successful depletion of HLAs, and lineage-specific differentiation into cardiomyocytes was verified. We also confirmed that the pluripotency of genome-edited iPSCs was successfully maintained by the three germ layers of differentiation. Moreover, whole-genome sequencing, karyotyping, and optical genome mapping analyses revealed no evident genomic abnormalities detected in some clones, whereas unexpected copy number losses, chromosomal translocations, and complex genomic rearrangements were observed in other clones. Our results indicate the importance of multidimensional analyses to ensure the safety and quality of the genome-edited cells. The manufacturing and assessment pipelines presented here will be the basis for clinical-grade genome editing of iPSCs.
Keywords: CRISPR-Cas9, human iPSCs, HLA-A, HLA-B, CIITA, GMP
Graphical abstract
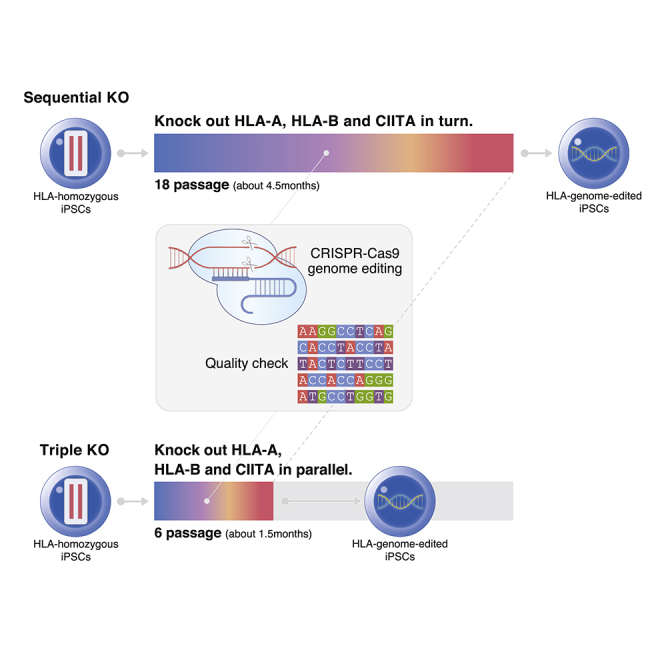
In this manuscript, corresponding authors and colleagues report the process of manufacturing and quality evaluation of the clinical-grade CRISPR-Cas9 genome-edited human iPS cell lines targeting multiple HLA genes. These results indicate the importance of multidimensional analyses due to the complex genomic rearrangement, especially for cells that have been edited simultaneously.
Introduction
Since the invention of human induced pluripotent stem cells (iPSCs) in 2007,1,2 many physicians and researchers worldwide have considered the potential application of iPSCs in regenerative medicine to restore functionally impaired tissues or organs and have been working vigorously toward the realization of this goal. Several leading projects have already come to the stage of clinical trials for diseases such as age-related macular degeneration, Parkinson’s disease and dilated cardiomyopathy,3, 4, 5 and further clinical trials for many other diseases are under development, just as iPS cell-derived CAR-NK therapy is being adapted for tumors.6,7
To expand the applicability of iPSC-mediated cell therapy, the allogeneic transplantation setting is advantageous in terms of its lower manufacturing costs and readiness for patients as an off-the-shelf cell therapy product. However, immune rejection caused by mismatches of human leukocyte antigens (HLAs) between donor and recipient is a hurdle for the development of allogeneic cell therapy.8 To overcome this issue, we have established iPSC stocks derived from healthy donors who are homozygous for HLA genes. To ensure the quality and safety of iPSC stocks, we have applied stringent selection criteria for established iPSC lines to reduce the risk of tumorigenicity due to genomic mutations, and these iPSC stocks have already been used in some of the aforementioned clinical trials.9 It is, however, estimated that more than 140 lines of iPSCs that are homozygous for HLA-A, HLA-B, and HLA-DR will be needed to cover 90% of the Japanese population.10 To cover multiethnic populations, the number of required lines would be even greater.11 Thus, in addition to the establishment of HLA homozygous iPSC lines, an alternative strategy is expected to avoid the immune rejection issue.
Recent progress in genome-editing technologies has revolutionized our ability to edit the genomic sequence of iPS cells at will. In fact, several groups have demonstrated that HLA or HLA-related genes (such as the B2M gene) can be removed or inserted to modulate T cell- or NK cell-mediated immunity against iPS cells.12, 13, 14 Accordingly, we recently developed a new strategy for the reduction of immune rejection using CRISPR-Cas9 genome editing to selectively knockout the HLA-A and HLA-B genes while retaining HLA-C and other non-classical HLAs.15 If necessary, the CIITA (class II, major histocompatibility complex, transactivator) gene can also be knocked out to suppress the expression of HLA class II genes. Such HLA genome-edited iPSCs could escape from both killer T cells and NK cells by deleting HLA-A, HLA-B, and all class II HLAs. The retained HLA-C with a haplotype mismatch can therefore be an antigen for T cells.16 Hence, we propose to match the HLA-C haplotype with donors. Due to the lower diversity of the HLA-C haplotypes compared with that of HLA-A or HLA-B genes, we estimated that seven lines of HLA-edited iPSCs would thus cover >95% of the Japanese population, while 12 lines would cover >90% of multiethnic populations.15
At the same time, however, it is reported that CRISPR genome editing may induce unintended genomic mutations at off-target sites,17,18 or unexpected large deletions at on-target sites.19 The CRISPR system uses a guide RNA (gRNA) to recognize the target site; however, some mismatches can be tolerated. Hence, when a similar target sequence with one or more mismatch bases exists elsewhere in the human genome, such off-target sites may be cleaved and a mutation might be induced. There is also a risk of chromosomal translocation when double-strand breaks are introduced into different chromosomes.20,21 Multiplexed gene disruption is necessary for the generation of hypoimmunogenic iPSCs. In addition, the DNA sequences of the HLA genes are highly similar to each other, hence the risk of off-target mutagenesis or chromosomal rearrangement could be higher than when targeting another gene locus. The risk associated with the clinical translation of multiplexed HLA gene editing remains to be explored.
To translate this HLA editing strategy for clinical applications, we established the manufacturing procedures for CRISPR-Cas9 genome editing in iPSCs under good manufacturing practice (GMP)-compliant conditions. Since HLA genes are highly variable among individuals and between the two alleles, it is technically challenging to design a proper gRNA that can target both alleles of the HLA gene, while avoiding the risk of off-target binding. To this end, we took advantage of our HLA homozygous iPSC lines originating from clinical-grade cell lines that we previously established, as the genomic sequences of both HLA alleles are almost identical in HLA homozygous donors. Hence, a single gRNA is sufficient for targeting both alleles, and we could avoid using multiple gRNAs for targeting a single HLA gene. For clinical-grade CRISPR-Cas9 genome editing, we used GMP-compatible 4D-Nucleofector to electroporate the complex of current GMP (cGMP)-grade Cas9 protein and chemically synthesized gRNAs into HLA homozygous iPSCs. After confirming the bulk knockout efficiency of HLA proteins by flow cytometry, we isolated subclones and performed stringent genomic integrity tests and cellular functional assays, including lineage-specific differentiation. We found that genome editing at the HLA loci could cause unexpected copy number loss, chromosomal translocation, and complex genomic rearrangement in multiple clones assessed by whole-genome sequencing (WGS), karyotyping, and optical genome mapping analyses. Our results highlight the challenges in targeting the HLA gene locus with the CRISPR-Cas9 system for future clinical applications. Therefore, we would like to propose the importance of stringent selection tests based on multidimensional assays, including rigorous genomic integrity tests, to translate the promise of hypoimmunogenic iPSCs for upcoming clinical applications.
Results
Generation of hypoimmunogenic iPSCs by CRISPR-Cas9 genome editing
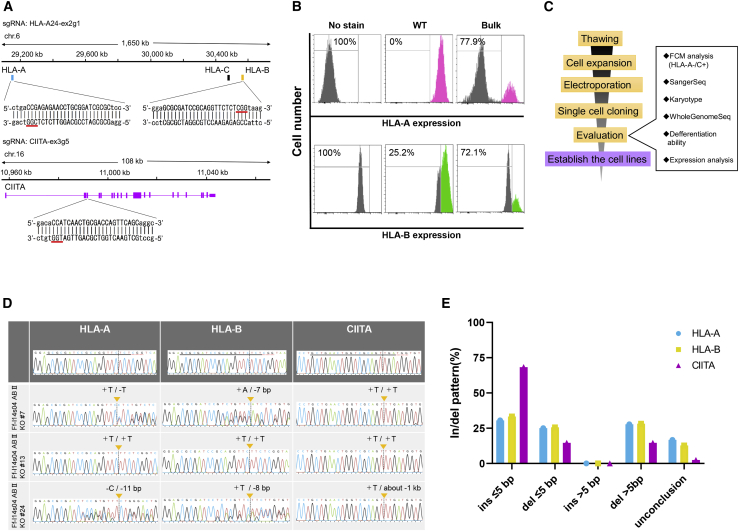
To establish standard operation protocols for the generation of clinical-grade hypoimmunogenic iPSCs, we started the selection of parental iPSC lines. We selected an iPSC line named Ff-I14s04, which was previously generated from peripheral blood mononuclear cells provided by a donor (ID: QHJI) carrying homozygous HLA alleles (A∗24:02, B∗52:01, DR∗15:02), which are most common in the Japanese population.9 In terms of the gRNA design, we used our internal genome sequence data for this cell line in order to verify the on-target specificity of a given gRNA. Due to the high homology between the HLA-A and HLA-B genes, we found that simultaneous genome editing of HLA-A and HLA-B genes using a single gRNA could be feasible (Table S1). Therefore, we designed one gRNA (HLA-A24-ex2g1) that targets both the HLA-A and HLA-B genes on chromosome 6, and another gRNA (CIITA-ex3g5) that targets the CIITA gene on chromosome 16 (Figure 1A). After optimization of the electroporation conditions, we electroporated the Cas9 protein and two gRNAs (HLA-A24-ex2g1 and CIITA-ex3g5) into the Ff-I14s04 clone by using 4D-Nucleofector. The knockout efficiency of the HLA-A and HLA-B protein in the bulk cell population was confirmed by HLA-A or B antibody staining and flow cytometry (FCM), after interferon (IFN)-γ stimulation for 2 days. The results showed that 77.9% of the cells were negative for the cell surface expression of HLA-A protein and 72.1% were negative for HLA-B protein, suggesting that biallelic knockout was achieved (Figure 1B).
Figure 1.
Generation and evaluation of simultaneous knockout of the HLA-A, HLA-B, and CIITA genes in iPSCs by CRISPR-Cas9
(A) The design of a gRNA (HLA-A24-ex2g1) to simultaneously target the HLA-A and HLA-B genes, and another gRNA (CIITA-ex3g5) to target the CIITA gene. The genomic coordinate is based on hg19. (B) Histograms of the immunoreactivity intensity of the anti-HLA-A and anti-HLA-B antibodies for bulk genome-edited iPSCs. (C) The workflow of the production of genome-edited iPSC clones and their evaluation. (D) Sanger sequencing of the genome-edited iPSCs after single-cell cloning. Insertions or deletions at the target sites in the genome-edited iPSC clones were confirmed by electropherograms. (E) Size distribution of insertions or deletions at each target gene locus.
Furthermore, to examine the insertion or deletion (indel) efficiency of HLA-A, HLA-B, and CIITA target sites in more detail, target-site cloning and sequencing were performed. Approximately 80% of target sites had indel mutations (Figure S1A and Table S2). The fact that the efficiency of biallelic knockout obtained from FCM, and indel induction obtained from the genomic DNA sequences of each of the three genes were almost comparable suggested that success or failure of the genome editing against the three loci by two gRNAs in each cell were synchronized rather than independent. Next, we performed limiting dilution of the bulk edited cells and seeded cells into multiple 96-well plates at a density of 0.25 cells/well. After isolation and expansion of the single-cell-derived clones up to 6-well plates, we assessed the HLA-A protein expression by flow cytometry of each clone after IFN-γ treatment. According to a flow cytometry experiment using an HLA-A antibody after cloning, we selected 30 clones of HLA-A knockout (KO) iPSCs from 41 analyzed clones (73.1%). We further subjected these clones to Sanger sequencing, karyotyping, WGS, RNA and protein expression analyses, and assessment of differentiation potential (Figure 1C). When we first tried to amplify the HLA-A, HLA-B, and CIITA regions of 30 subclones by PCR, we either could not obtain PCR products, or we obtained PCR products that differed greatly from the predicted product size in 11 clones (Figure S1B). We found chimeric sequences involving HLA-A and HLA-B in four clones (Figure S1C). These results suggested the existence of global genomic rearrangement involving the targeted loci.
Sanger sequencing of the HLA-A, HLA-B, and CIITA regions revealed that 19 iPSC clones among the above 30 clones had indel mutations, not only at the HLA-A locus but also at the HLA-B and CIITA loci, and six clones had an in-frame mutation in at least one of the HLA-A or HLA-B loci (Figures 1D and S1D). Among these mutations, almost half of the iPSC clones had indels of 5 base pairs (bp) or longer in the HLA loci, whereas 80% of the clones had indels of less than 5 bp in the CIITA locus (Figure 1E). Therefore, the sizes of the indel mutations may be affected by the sequences of the gRNAs or target regions.22,23 The predicted amino acid sequences of the genome-edited iPSC clones—with the exception of clones possessing in-frame mutations—were shortened by the induction of premature stop codons within exons 2 to 4 (Table S3).
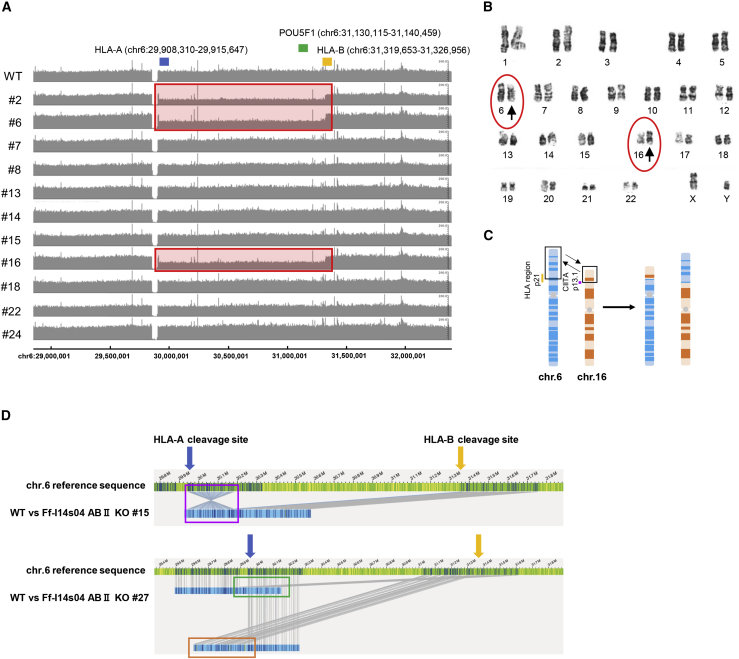
Comprehensive analysis of genetic mutations caused by the CRISPR-Cas9 system
To reveal the mutations that occurred during the genome editing and clonal isolation process, we conducted short read-based WGS, karyotyping, and optical genome mapping using genome-edited iPSC clones. First, we compared the aligned sequences obtained from genome-edited iPSC clones with their parental (wild-type) iPSCs after WGS. The copy number analysis indicated that three (Ff-I14s04 ABII KO #2, #6 and #16) of 11 randomly selected iPSC clones that were subjected to WGS harbored hemizygous large deletions of approximately 1.4 Mbp between the HLA-A and HLA-B loci (Figure 2A). In addition to these three iPSC clones, we identified chimeric sequence reads in three iPSC clones (Ff-I14s04 ABII KO #8, #18 and #22) at the HLA-A and HLA-B loci, indicating that unexpected genomic rearrangement occurred in the process of repair after genomic digestion by the CRISPR-Cas9 system. Among the other mutations found in the copy number analysis, a mutation located on chromosome (chr)3 in Ff-I14s04 ABII KO #2 might have been included in a possible CIITA gRNA off-target region, which was defined by an interval of 1 kbp around the sequences, allowing for 5 bp of mismatches and/or gaps and including the RPN1 gene, which was listed among known cancer-related genes (referred to in COSMIC census version 88, https://cancer.sanger.ac.uk/cosmic/census, Table S4, Data S1 and S2). We further investigated small mutations, including single nucleotide variants (SNVs) and small indels, by comparing genome-edited iPSCs with wild-type iPSCs. The selected SNVs and indels potentially affected amino acid sequences that were not located in either genes related to cancer (other than the HLA-A and CIITA genes) or predicted off-target regions (Table S5).
Figure 2.
Genomic integrity of genome-edited iPSC clones
(A) A copy number analysis from whole-genome sequencing at the HLA class I gene cluster on the chromosome (chr) 6. The locations of HLA-A (blue), HLA-B (orange), and POU5F1 (green) are indicated above. Out of 11 clones analyzed, three clones showed a copy number loss between HLA-A and HLA-B genes (chr6: 29,911,740–31,327,897), indicated by a red box. (B) A karyotype analysis by G-banding of the genome-edited iPSCs. (C) The diagram shows a model of translocation between chr 6 and chr 16, which was found in seven iPSC clones among the 30 clones we tested. (D) Complicated genomic rearrangements were observed in optical genome mapping. Blue bars show the mutated chromosome regions. The genomic coordinate is hg38.
Next, the karyotyping results demonstrated that seven genome-edited iPSC clones among the 30 clones showed chromosomal translocations between chr6 (HLA locus) and chr16 (CIITA locus) (Figures 2B and 2C). For a more detailed analysis, we subjected nine genome-edited iPSC clones, including wild-type iPSCs (as controls) to optical genome mapping. The results of this analysis indicated that Ff-I14s04 ABII KO #8 and #12 presented chromosomal translocations between HLA-A or HLA-B and CIITA sites (Figure S2), which were consistent with the results of the karyotyping test, whereas Ff-I14s04 ABII KO #15 and #27 harbored complex mutations that included partial translocation and inversion near the HLA-A and HLA-B cleavage sites (Figure 2D). All of these comprehensive genetic analyses revealed the frequent occurrence of unexpected genomic rearrangement caused by simultaneous triple gene editing of HLA-A, HLA-B, and CIITA.
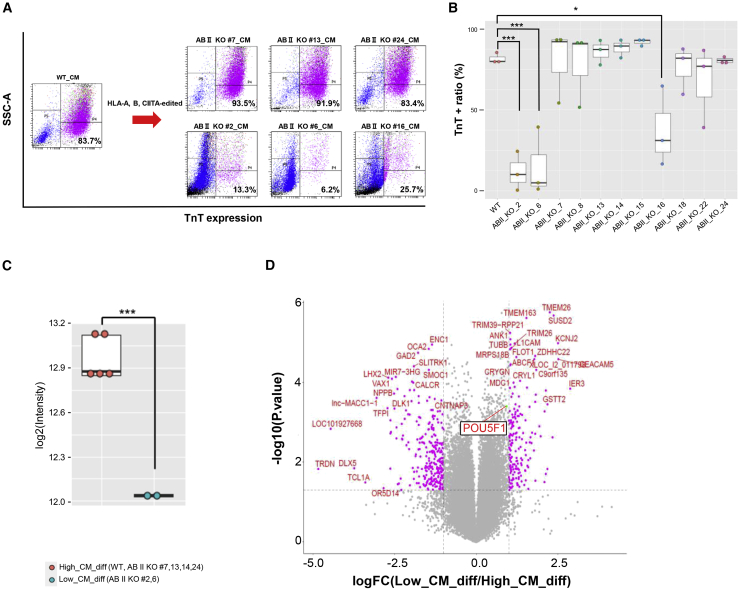
Evaluation of the differentiation potential of genome-edited iPSC clones
Next, to confirm whether genome-edited iPSC clones retained similar differentiation potential to the original iPSC clones, we examined the efficacy of cardiomyocyte differentiation. After the induction of cardiomyocytes though embryo body (EB) formation and a three-stage stepwise differentiation protocol for 15 days, the percentage of troponin T (TnT)-positive cells was measured by FCM (Figures 3A and S3A). The original iPSC clone and eight of the 11 whole-genome-analyzed HLA-edited iPSC clones that were subjected to differentiation assays showed a >50% TnT-positive cell percentage after the induction of differentiation, whereas the other three clone Ff-I14s04 ABII KO #2, #6, and #16 showed a low TnT-positive cell ratio (Figure 3B). As shown in Figure 2A, these three iPSC clones have hemizygous large deletions between the HLA-A and HLA-B loci. More than 30 genes are located between the HLA-A and HLA-B loci, including the POU5F1 (alternatively OCT3/4) gene, which is one of the most important genes for the maintenance of pluripotency. The expression analysis of these genome-edited iPSCs using microarrays revealed that the POU5F1 expression levels in the Ff-I14s04 ABII KO #2 and #6 clones were reduced by approximately half in comparison with those in the wild-type and other genome-edited iPSC clones (Figure 3C). No significant differences were observed in the expression of other pluripotent marker genes between the clones (Figure S3B). Although the expression of many other genes was altered to a greater extent than that of POU5F1 (Figure 3D), the most plausible cause of the loss of the cardiomyocyte differentiation potential in these clones was likely the deletion of the region including POU5F1. Changes in the transcriptional profile, including the decreased expression of POU5F1, could have a large effect on the myocardial differentiation efficiency. In addition, differentiation assays of three germ layers were performed using the STEMdiff Trilineage Differentiation Kit. Immunocytochemistry and FCM were performed on the wild-type, genome-edited iPSC clones (#7, 13, 24), and those with reduced a POU5F1 expression (#2, 6, 16) to assess the differentiation status (Figure S4). There were no significant differences in the potential to differentiate into the early stage of three germ layers among wild-type and genome-edited iPSC clones or genome-edited iPSC clones with and without reduced expression of POU5F1. The down-regulation of the POU5F1 expression did not affect early differentiation, but it did significantly reduce the myocardial differentiation potential. Therefore, genome-edited iPSC lines with the deletion of the HLA-A/HLA-B intergenic region should be excluded from further analyses.
Figure 3.
Evaluation of the cardiomyocyte differentiation potential of the genome-edited iPSCs
(A) Scatterplots of the FCM analysis examining the proportion of troponin T (TnT)+ cells at 15 days after the induction of cardiomyocyte differentiation. The results of the original (wild-type) and typical results of each three clones showing high or low cardiomyocyte differentiation potential. The results of other clones are shown in Figure S3A. The horizontal axis indicates the fluorescence intensities of fluorophores conjugated with the TnT antibody. The vertical axis indicates side scatter. (B) A boxplot showing the proportion of TnT+ cells in cardiomyocyte differentiation assays that were performed on three biological replicates. Asterisks indicate statistical significance: ∗∗∗p < 0.001; ∗p < 0.05. (C) A boxplot of microarray data showing the differential expression of POU5F1 in iPSC clones showing high (orange) or low (cyan) cardiomyocyte differentiation potential. Each dot shows a clone. Asterisks indicate statistical significance: ∗∗∗p < 0.001. (D) A volcano plot of the microarray analysis showing the differentially expressed genes between iPSC clones with high or low cardiomyocyte differentiation potential.
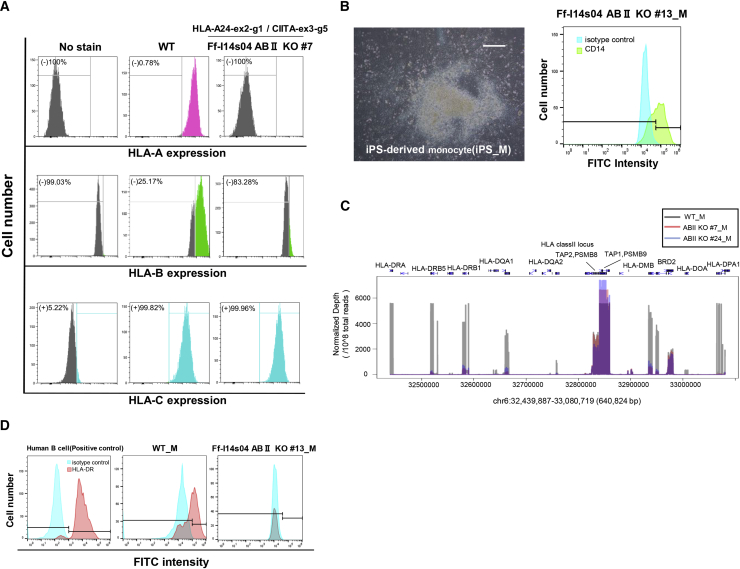
RNA expression analysis of class I and class II HLA genes in genome-edited iPSC clones
Since the genome-edited iPSC clones harbored frameshift indel mutations (Table S3), the immunoreactivity of the HLA-A antibody toward them was lost due to the destruction of the HLA-A antibody epitope, whereas that of the anti-HLA-C antibody was retained as intended (Figure 4A). With respect to HLA-B, antibody reactivity was also reduced (Figure 4A). Next, to confirm the effect HLA-A, HLA-B, and CIITA gene editing on the HLA gene expression, wild-type and genome-edited iPSCs were differentiated into CD14+ monocytes, which are known to express both HLA class I and class II genes. After the stepwise differentiation, the percentage of CD14+ monocytes was confirmed by FCM using an anti-CD14 antibody (Figure 4B). Then, we examined the RNA expression by RNA sequencing (RNA-seq) and the expression of the HLA-DR cell surface protein by FCM. The normalized gene expression, represented by transcripts per million values, was reduced for HLA-A, HLA-B, and classⅡ HLA, but not for HLA-C, HLA-E, HLA-F, HLA-G, or CIITA in CD14+ monocytes derived from genome-edited iPSC clones (Figures S5A and S5B). The read mappings in the regions of the CIITA genes indicated that indel mutations induced by genome editing did not greatly affect the expression or maintenance of these transcripts (Figure S5B). CIITA is a transcriptional activator that up-regulates the HLA class II expression. To investigate the impact of CIITA KO, we assessed the expression of the HLA class II genes (HLA-DR, HLA-DQ, HLA-DP) and that were greatly reduced in comparison with the original non-edited CD14+ monocytes (Figure 4C). In addition, the cell surface presentation of the HLA-DR protein was lost in genome-edited iPSC-derived monocytes but not in wild-type monocytes (Figure 4D). Taken together, these results suggested that the function of the HLA-A, HLA-B, and CIITA genes was lost in genome-edited iPSC clones.
Figure 4.
Validation of the expression profiles of the HLA genes in differentiated CD14+ monocytes derived from genome-edited iPSCs
(A) Flow cytometry of the original (wild-type [WT]) and clone #7, as a typical example, stained with the -HLA-A (upper panels), HLA-B (middle panels) or HLA-C (lower panels) antibodies after IFN-γ treatment. (B) Monocyte differentiation derived from the genome-edited iPSCs (clone #13, randomly selected). Scale bar, 200 μm. Flow cytometry of the cells stained with FITC-conjugated anti-CD14 antibody (green on the right panel). The same cells stained with the FITC-conjugated isotype control antibody are indicated in cyan. (C) RNA-seq data of the HLA class II locus in differentiated monocytes derived from the original (WT, gray) and genome-edited iPSC clones (#7, red and #24, blue). The normalized sequence depth (transcriptional level) from the RNA-seq data corresponding to each gene position is shown. In comparison with WT cells, HLA class II genes (HLA-DRA, DRB5, DRB1, DQA2, DMB, DOA, and DPA1) were expressed at much lower levels in genome-edited iPSC clones (#7 and #24), whereas non-HLA genes (TAP2, PSMB8, PSMB9, BRD2) were largely unchanged. (D) After monocyte differentiation of the original (WT) and genome-edited iPSCs (clone #13), flow cytometry was performed by staining with FITC-conjugated anti-class II HLA (HLA-DR, red) or FITC-conjugated isotype control antibodies after IFN-γ treatment. Human B cells were used as a positive control for HLA-DR staining.
Discussion
In this study, we demonstrated the manufacturing of hypoimmunogenic iPSCs and a detailed evaluation of their quality. Since we used iPSCs with homozygous HLA genes, the number of gRNAs required for gene editing targeting multiple loci could be reduced, irrespective of the genetic variability in this region (Figure 1A). This could be advantageous not only for the simplification of the production process but also for the reduction of genetic mutations caused by off-target effects of gRNAs. Among the identified small mutations, including SNVs and indels, which may affect amino acid sequences, the genome-edited iPSCs that we generated in this study did not show mutations either in cancer-related genes other than the target genes (including HLA-A, HLA-B, and CIITA) or in the neighboring predicted off-target sequences (Table S5; Data S1 and S2). Such effects would be more severe in cases in which a greater number of gRNAs were used.
On the other hand, we found that more complicated mutations, such as large deletions at the intervening sequence between HLA-A and HLA-B (Figure 2A) and chromosomal translocations between the locus of HLA on chr6 and that of CIITA on chr16, often occurred in genome-edited iPSCs (Figures 2B and 2C). This might have been due to the simultaneous triple gene editing targeting HLA-A, HLA-B, and CIITA. Although step-by-step genome-editing approaches targeting individual genes at a time might reduce such mutations, it would require a longer culture period and multiple rounds of subcloning processes. In addition, repeated introduction of gRNAs and Cas9 gene or protein could be stressful for cells. Such prolonged culturing might lead to spontaneous mutagenesis that could affect the cellular characteristics. Since the detection of genome-wide low-frequency mutations in a rare cell population is technically challenging,24 avoiding long-term culturing is desirable to reduce the risk. On the other hand, with the simultaneous targeting approach, distinctive mutations could be accurately detected by multiple genomic analyses, including optical genome mapping (Figures 2D and S2). As a result, we could avoid using iPSCs that harbor such mutations. As each genome-editing pipeline has advantages and disadvantages, the genome-editing strategy should be designed to maximize the safety of the therapeutic application.
Next, we examined whether the genome-edited iPSCs retained cardiomyocyte differentiation potential and found that the iPSCs with hemizygous large deletions at the intervening sequence between HLA-A and HLA-B (Ff-I14s04 ABII KO #2, #6, and #16) lost their differentiation potential, whereas the other iPSCs retained it (Figures 3A, 3B, and S3A). This was likely due to the hemizygous loss of alleles, including the POU5F1 gene, located between HLA-A and HLA-B (Figure S3B). POU5F1 (alternatively OCT3/4) is well known to be an important factor for the reprogramming of somatic cells.25 Previous knockdown experiments targeting POU5F1 in human embryonic stem cells (hESCs) revealed that the reduced expression of POU5F1 led to the loss of self-renewal capacity and ectoderm or extraembryonic differentiation, but not mesoderm or endoderm differentiation.26 In our experiment, iPSCs with the hemizygous loss of alleles, including POU5F1, could maintain their proliferation for at least 10 passages, and we could not identify any obvious characteristic morphological features of these iPSC clones, even though the POU5F1 expression levels in these iPSC clones were reduced by half (Figure S6). Although these iPSCs lost their cardiomyocyte differentiation potential, it may be possible for the iPSCs to differentiate into other cells, such as neuronal lineages, as shown in the previous report. In fact, the reduced expression of POU5F1 did not seem to affect differentiation up to the early stage of the three germ layers (Figure S4). The situation is not exactly comparable to our iPSCs with the hemizygous loss of alleles, including POU5F1, or previous knockdown experiments in hESCs because an extremely small difference in gene expression levels can lead to different phenotypes.27 Thus, the development of genome-editing technologies will be indispensable for the quality management of cell products for regenerative therapies. Since genome-editing technologies continue to advance rapidly, it is currently possible to precisely design experiments not only for the disruption of a gene but also for the insertion of donor sequences.28,29 These technologies will contribute to the production of “designer cells” whose functions are modified or newly acquired from original cells other than hypoimmunogenic iPSCs.30
Finally, we evaluated the expression of HLA genes in CD14+ monocytes differentiated from genome-edited iPSCs at the mRNA or protein level. Frameshift indel mutations that induced a premature termination codon in CIITA did not elicit an active degradation mechanism, so-called nonsense-mediated decay (Figure S5B). Due to our incomplete understanding of the regulatory mechanisms of RNA processing and degradation, we should consider that the predicted functions after the introduction of mutations are not necessarily accurate.31 Combinations of other assays are therefore necessary to ensure the loss of function of these genes. Regarding the CIITA gene, the expression levels of class II HLA genes, such as HLA-DRA and HLA-DRB1, were drastically reduced in CD14+ monocytes derived from genome-edited iPSCs, suggesting the loss of function of this gene (Figure 4B). In protein expression assays using FCM, we confirmed the loss of immunoreactivity of anti-HLA-A in genome-edited iPSCs and anti-HLA-DR in the antigen-presenting CD14+ monocytes derived from genome-edited iPSCs, whereas the immunoreactivity of anti-HLA-C was retained in these iPSCs (Figures 4A and 4D). Although the antibody reactivity of HLA-B was not sufficient (Figure 4A), the decrease of antibody response was certainly confirmed in genome-edited iPSCs. Furthermore, a previous study revealed that mutations that induced a premature stop codon at the α-chain of HLA molecules resulted in the loss of the HLA protein function.32 Therefore, the HLA-B function is expected to be lost in genome-edited iPSCs with nonsense mutations in the α-chain region of HLA-B (Table S3). Here, we mainly discussed the triple gene editing approach, as we need to manage the mismatches from both class I and class II HLAs. However, caution is necessary for the CIITA knockout because CIITA is known to be involved in the transcriptional regulation for not only the class II HLAs but also other immunological genes.33, 34, 35 Hence, when there is a concern regarding the possibility of side effects due to the loss of the CIITA, retention of the CIITA gene can be an option for some applications. Previously, Gornalusse et al.12 reported the method that could reduce “missing-self” immune rejection response caused by NK cells. Although the overexpression of single-chain HLA-E fused with B2M could suppress NKG2A (alternatively KLRC1)+ NK cells, this approach is difficult to suppress KIR2DL1–4+ NK cell populations, as they are suppressed through HLA-C or HLA-G binding. In addition, the single-chain HLA-E fused with B2M has no antigen-presentation ability. On the other hand, our HLA-A/B knockout strategy can suppress both NKG2A+ and KIR2DL1-4+ NK cells by endogenous HLA-C or HLA-G expression. By our strategy, we started with the evaluation of 40 genome-edited iPSC clones and finally obtained only three clones that satisfied all criteria with regard to their functions and genetic mutations (Figure S7). This success rate was much lower than our initial expectation. Nonstandard products were obtained as a result of mutations that occurred due to the inappropriate repair of the digested sites introduced by simultaneous triple gene editing. As mentioned above, this may be somewhat unavoidable if we prioritize a simplified process and avoid the repetitive burden of the induction of exogenous genes. Therefore, the detailed evaluation of genome-edited cell products is important for ensuring the safety of regenerative therapies.
Materials and methods
Cell culture and generation of HLA-A, HLA-B, and CIITA genome-edited iPSCs
The generation of iPSCs derived from a donor who provided their informed consent and the genetic recombination experiments were approved by Kyoto University. Ff-I14s04 clones were previously generated from the peripheral blood-derived mononuclear cells of a homozygous HLA donor.9 The culture of iPSCs under feeder-free, xeno-free conditions was performed according to the methods of a previous study.36 The methods of gene editing targeting the HLA-A/HLA-B/CIITA genes were described in a previous study, with a few modifications.15 Briefly, 0.3 × 106 iPSCs were transfected with an RNP (ribonucleoprotein) complex of 5 μg of GMP-grade recombinant Cas9 (Takara-bio, Shiga, Japan) and 1.25 μg of chemical synthesized gRNA (Ajinomoto Bio-Pharma) in 20 μL of Primary P3 buffer and electroporation condition program CA-137. For single-cell cloning, genome-edited iPSCs were plated on a 96-well plate by limiting dilution at 0.25 cells/well. Forty colonies that grew from single cells were picked and expanded for the following analyses.
Differentiation into the three germ layers
The differentiation of iPSCs into three germ layers was conducted using the STEMdiff Trilineage kit (STEMCELL Technologies) according to the manufacturer’s protocol.
Differentiation into cardiomyocytes
Cardiomyocyte differentiation was conducted according to a previous paper with a few modifications.37 In brief, undifferentiated iPSCs were detached and dissociated into single cells by 5-min incubation with TrypLE Select (Gibco). The cells were then suspended in StemPro34 medium supplemented with 10 μL/mL GlutaMax (Gibco), 50 μg/mL ascorbic acid, 4 × 10−4 M monothioglycerol, 150 μg/mL transferrin, 10 μM Y-27632 (WAKO, Japan), 0.5% Matrigel, and 2 ng/mL human recombinant BMP4 (R&D Systems, Minneapolis, MN) and allowed to form EBs by being placed into a low-attachment 6-well dish and cultivated for 24 hours. On day 1, media, which included human recombinant activin A (R&D Systems), BMP4, and basic fibroblast growth factor (bFGF) (R&D Systems), were added into the wells. The final concentrations were as follows: activin A, 6 ng/mL; BMP4, 9 ng/mL; and bFGF, 5 ng/mL. On day 3, the media were changed to StemPro 34 media supplemented with 10 ng/mL vascular endothelial growth factor (VEGF) (R&D Systems), 5.4 nM SB431542, 0.06 μM Dorsomorphin, and 1 μM IWP-3, a Wnt inhibitor (Stemgent, Cambridge, MA). On day 7, the media were changed to StemPro 34 media supplemented with 10 μL/mL GlutaMax, 50 μg/mL ascorbic acid, 4 × 10−4 M monothioglycerol, 150 μg/mL transferrin, and 5 ng/mL VEGF. For the maintenance of iPSC-CMs, the culture media were refed every 2 to 3 days. On the day of cell injection, EBs were dissociated by collagenase I for 3 to 6 hours and Accumax for 10 minutes.
Differentiation into CD14+ monocytes
The differentiation of iPSCs into CD14+ monocytes was conducted using the STEMdiff monocyte kit (STEMCELL Technologies) according to the manufacturer’s protocol.
Flow cytometry
The cultured iPSCs were detached from plates by adding 0.5× TripLE Select (Thermo Fisher Scientific) and 0.25 mM EDTA (Nacalai Tesque, Kyoto, Japan), after which they were washed appropriately. The iPSCs were mixed with the following diluted antibodies: anti-HLA-A24 (Clone 17A10, MBL, Japan), anti-HLA-B (Clone 0.L.6, LS Bio, USA), and anti-HLA-C (Clone DT-9, BD Biosciences, USA). iPSCs with the induction of three germ layer differentiation were fixed in 4% paraformaldehyde, permeabilized with 0.5% Triton X-100, and blocked in Blocking One (Nacalai Tesque, Kyoto, Japan). Cells were incubated with primary antibodies: anti-Nestin (Clone 10C2, CST, USA), anti-PAX6 (Clone D3A9V, CST, USA), anti-NCAM (Clone 123C3, CST, USA), anti-Brachyury (Clone D2Z3J, CST, USA), anti-FOXA2 (Clone 7E6, Abcam, UK), and anti-SOX17 (Clone D1T8M, CST, USA). They were then washed and incubated with secondary antibodies: anti-Mouse IgG Alexa Fluor Plus 555 (Thermo Fisher Scientific), anti-Mouse IgG Alexa Fluor 488 (Thermo Fisher Scientific), and anti-Rabbit IgG CF®640R (BIOTIUM). Cells after myocardial induction were fixed and permeabilized as described above, and incubated with primary antibody anti-ToroponinT (Clone 13-11; Thermo Fisher Scientific), washed, and incubated with Alexa Fluor secondary antibody described above. iPS-derived monocytes were washed appropriately, and mixed with the following diluted antibodies: anti-CD14 (Clone MEM-15, Abcam, UK) and anti-HLA-DR (Clone REA805, Miltenyi Biotec, Germany). After passing the cells through a 45-μm cell strainer (BD Japan), stained cells were applied to an SA3800 cell analyzer (SONY, Tokyo, Japan).
Immunofluorescence cell staining
iPSCs with the induction of three germ layer differentiation were prepared as described above. After incubating with the antibodies, the cells were washed three times with TBS and images were immediately captured using a Keyence microscope BZ-X810.
Target site cloning
For the analysis of mutation efficiency corresponding to each target site, genomic DNA of genome-edited bulk-iPSCs was first amplified using the HLA-A, HLA-B, and CIITA primer pairs (Table S6). Then, the PCR products were placed into the cloning site of TOPO vector by a Zero Blunt TOPO PCR cloning kit for sequencing (Thermo Fisher Scientific) and transformed into E. coli. More than 10 colonies of each group were checked by PCR, and Sanger sequence was performed with the M13 primers.
Sanger sequencing
Genomic DNA was used for PCR and Sanger sequencing to analyze indel patterns, which were carried out with the PCR primers shown in Table S6. Nested PCR was conducted to precisely amplify the target HLA-A, HLA-B, and HLA-C loci. The obtained amplicons were used for Sanger sequencing, which was conducted by Macrogen Japan Corp or Azenta Life Sciences.
Karyotyping analyses
(G-banding) was conducted by SRL (Tokyo, Japan).
Whole-genome sequencing
Library preparation for WGS was conducted using the KAPA HyperPrep PCR-free kit for Illumina (Roche) in accordance with the manufacturer’s protocol. WGS was conducted using an Illumina NovaSeq6000 system. After trimming the sequence reads using fastp 0.20.1,38 they were mapped to the human reference genome (hg19) by BWA MEM v0.7.15.39 All samples were within 1.6 to 2.3 billion sequenced reads, a 75.0% to 79.2% mapping rate, and 60.3 to 82.3 average depth at the genome region. The analysis of SNVs and small indels that were introduced into the iPSCs during the genome editing and the cloning process, was conducted by comparison of genome-edited iPSCs and parental iPSCs using the Genomon pipeline v2.3.0.40 A copy number analysis was conducted using Delly 0.7.3.41 and VarScan2 2.4.2.42 Images of mapped reads were obtained using IGV43 and Genome Jack (Mitsubishi Space Software, Tokyo, Japan).
Optical genome mapping
Optical genome mapping using Saphyr (Bionano genomics) was conducted by AS ONE Bioscience (Osaka, Japan). Bionano optical genome mapping was performed according to the manufacturer’s instructions. Briefly, ultra-high molecular weight (UHMW) genomic DNA was isolated from 1.5 × 106 cells using the Bionano Prep SP Blood and Cell Culture DNA Isolation Kit (Bionano Genomics, San Diego, CA, #80030). DNA quantification was performed using the Qubit dsDNA BR assay kit (Thermo Fisher Scientific) with a Qubit 4.0 Fluorometer (Thermo Fisher Scientific). A total of 750 ng of UHMW DNA was labeled using the Bionano Prep Direct Label and Stain Kit (Bionano Genomics, #80005), according to the manufacturer’s protocol. DNA quantification of the labeled UHMW DNA was performed using the Qubit dsDNA HR assay kit (Thermo Fisher Scientific) with a Qubit 4.0 Fluorometer. Labeled DNA at a concentration of 4 to 15 ng/μL was then loaded onto the Saphyr Chip G2.3 (Bionano Genomics, #20366) and run on a Bionano Saphyr instrument (Bionano Genomics), targeting 100× or 300× human genome coverage by collecting 400 GB or 1,300 GB of data per sample, respectively. De novo assembly and variant annotation pipeline were applied using Bionano Solve version 3.6.1 with GRCh38 as a reference. Only DNA molecules with a minimum length of 150 kbp were used for the bioinformatics analysis, along with a minimum of nine labels per molecule. SV data were visualized with Bionano Access version 1.6.1. SVs were further filtered to eliminate variants observed in the Bionano control samples.
Possible off-target sites of genome editing
These were searched using GGGenome (https://gggenome.dbcls.jp/en/) with the setting allowing for 5 bp of mismatches and/or gaps.
Amino acid sequence prediction
The HLA-A, HLA-B, and CIITA amino acid sequences of the original and genome-edited iPSC clones were translated using ApE (https://jorgensen.biology.utah.edu/wayned/ape/). The translated sequences were subjected to multiple alignments using Clustal Omega (https://www.ebi.ac.uk/Tools/msa/clustalo/).
Microarray analysis
The microarray analysis was conducted using a customized SurePrint G3 human GE microarray 8 × 60K v3.0 (Design ID:083470, Agilent) in accordance with the manufacturer’s protocol.
RNA-seq
TruSeq Stranded Total RNA Prep Gold (Illumina) was used for library preparation. Sequencing of the RNA-seq library was conducted on a NovaSeq6000 platform. All samples were within 335 to 445 million sequenced reads and an 83.3% to 84.7% mapping rate, as calculated by STAR. The obtained sequences were analyzed via the ENCODE long-rna-seq pipeline v2.3.4 (https://github.com/ENCODE-DCC/long-rna-seq-pipeline). The comparison of the expression among iPSCs was conducted using R v3.6.3 (https://cran.r-project.org/).
Statistical analysis
Statistical analyses were conducted using GraphPad Prism 9 and R. In the three germ layer differentiation assays, cardiomyocyte differentiation assay, and comparison of doubling time, a one-way ANOVA with Dunnett’s multiple comparison test was performed by setting the original (wild-type) as a control. In the expression analysis, a two-tailed Student’s t test with Benjamin-Hochberg multiple testing correction was used (Data S3).
Study approval
The iPS cell line (Ff-I14s04) used in this study was generated under written consent with approval by CiRA, Kyoto University.
Acknowledgments
We are grateful to Dr. Hirofumi Harashima (AS ONE) for providing technical assistance with the genomic analysis. We thank Dr. Shin Kaneko (CiRA, Kyoto University) and Dr. Peter Gee (CiRA, Kyoto University and MaxCyte Inc.) for their helpful advice. We thank Mr. Masaya Todani (CiRA, Kyoto University) for helping in the preparation of the Graphical abstract. This work was supported by a research center network for the realization of regenerative medicine of the Japan Agency for Medical Research and Development (AMED) under Grant Number JP20bm0104001h0108.
Author contributions
Y.K., M.U., H.X, A.H., N.T., and M.T. conceived the study design. Y.K., S.N., A.U., K.T., A.K., and H.O. conducted cell culture, and molecular and immunocytochemical experiments. Y.K., T.M.K., and M.N. conducted genomic analysis. T.M.K. conducted expression analysis. Y.K. and T.M.K. wrote the manuscript.
Declaration of interests
The authors declare no competing interests.
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.omtm.2022.05.010.
Supplemental information
References
- 1.Takahashi K., Tanabe K., Ohnuki M., Narita M., Ichisaka T., Tomoda K., et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Yu J., Vodyanik M.A., Smuga-Otto K., Antosiewicz-Bourget J., Frane J.L., Tian S., Nie J., Jonsdottir G.A., Ruotti V., Stewart R., et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 3.Mandai M., Watanabe A., Kurimoto Y., Hirami Y., Morinaga C., Daimon T., Fujihara M., Akimaru H., Sakai N., Shibata Y., et al. Autologous induced stem-cell–derived retinal cells for macular degeneration. N. Engl. J. Med. 2017;376:1038–1046. doi: 10.1056/nejmoa1608368. [DOI] [PubMed] [Google Scholar]
- 4.Takahashi J. Clinical trial for Parkinson's disease gets a green light in the US. Cell Stem Cell. 2021;28:182–183. doi: 10.1016/j.stem.2021.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Deinsberger J., Reisinger D., Weber B. Global trends in clinical trials involving pluripotent stem cells: a systematic multi-database analysis. NPJ Regenerative Med. 2020;5:15. doi: 10.1038/s41536-020-00100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyd N.R., Tiedemann M., Cartledge K., Cao M., Evtimov V., Shu R., Nguyen T., Nguyen N., Nisbet I., Boyd R., Trounson A. Off-the-shelf ipsc derived car-nk immunotherapy for solid tumors. Cytotherapy. 2020;22:S199. doi: 10.1016/j.jcyt.2020.04.067. [DOI] [Google Scholar]
- 7.Ueda T., Kumagai A., Iriguchi S., Yasui Y., Miyasaka T., Nakagoshi K., Nakane K., Saito K., Takahashi M., Sasaki A., et al. Non-clinical efficacy, safety and stable clinical cell processing of induced pluripotent stem cell-derived anti-glypican-3 chimeric antigen receptor-expressing natural killer/innate lymphoid cells. Cancer Sci. 2020;111:1478–1490. doi: 10.1111/cas.14374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamanaka S. Pluripotent stem cell-based cell therapy-promise and challenges. Cell Stem Cell. 2020;27:523–531. doi: 10.1016/j.stem.2020.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Umekage M., Sato Y., Takasu N. Overview: an iPS cell stock at CiRA. Inflamm. Regen. 2019;39:17. doi: 10.1186/s41232-019-0106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okita K., Matsumura Y., Sato Y., Okada A., Morizane A., Okamoto S., Hong H., Nakagawa M., Tanabe K., Tezuka K.-i., et al. A more efficient method to generate integration-free human iPS cells. Nat. Methods. 2011;8:409–412. doi: 10.1038/nmeth.1591. [DOI] [PubMed] [Google Scholar]
- 11.Taylor C.J., Peacock S., Chaudhry A.N., Bradley J.A., Bolton E.M. Generating an iPSC bank for HLA-matched tissue transplantation based on known donor and recipient HLA types. Cell Stem Cell. 2012;11:147–152. doi: 10.1016/j.stem.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Gornalusse G.G., Hirata R.K., Funk S.E., Riolobos L., Lopes V.S., Manske G., Prunkard D., Colunga A.G., Hanafi L.-A., Clegg D.O., et al. HLA-E-expressing pluripotent stem cells escape allogeneic responses and lysis by NK cells. Nat. Biotechnol. 2017;35:765–772. doi: 10.1038/nbt.3860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deuse T., Hu X., Gravina A., Wang D., Tediashvili G., De C., Thayer W.O., Wahl A., Garcia J.V., Reichenspurner H., et al. Hypoimmunogenic derivatives of induced pluripotent stem cells evade immune rejection in fully immunocompetent allogeneic recipients. Nat. Biotechnol. 2019;37:252–258. doi: 10.1038/s41587-019-0016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han X., Wang M., Duan S., Franco P.J., Kenty J.H.-R., Hedrick P., Xia Y., Allen A., Ferreira L.M.R., Strominger J.L., et al. Generation of hypoimmunogenic human pluripotent stem cells. Proc. Natl. Acad. Sci. U. S. A. 2019;116:10441–10446. doi: 10.1073/pnas.1902566116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu H., Wang B., Ono M., Kagita A., Fujii K., Sasakawa N., et al. Targeted disruption of HLA genes via CRISPR-Cas9 generates iPSCs with enhanced immune compatibility. Cell Stem Cell. 2019;24:566–578.e7. doi: 10.1016/j.stem.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Blais M.E., Dong T., Rowland-Jones S. HLA-C as a mediator of natural killer and T-cell activation: spectator or key player? Immunology. 2011;133:1–7. doi: 10.1111/j.1365-2567.2011.03422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fu Y., Foden J.A., Khayter C., Maeder M.L., Reyon D., Joung J.K., Sander J.D. High-frequency off-target mutagenesis induced by CRISPR-Cas nucleases in human cells. Nat. Biotechnol. 2013;31:822–826. doi: 10.1038/nbt.2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cradick T.J., Fine E.J., Antico C.J., Bao G. CRISPR/Cas9 systems targeting β-globin and CCR5 genes have substantial off-target activity. Nucleic Acids Res. 2013;41:9584–9592. doi: 10.1093/nar/gkt714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kosicki M., Tomberg K., Bradley A. Repair of double-strand breaks induced by CRISPR-Cas9 leads to large deletions and complex rearrangements. Nat. Biotechnol. 2018;36:765–771. doi: 10.1038/nbt.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi P.S., Meyerson M. Targeted genomic rearrangements using CRISPR/Cas technology. Nat. Commun. 2014;5:3728. doi: 10.1038/ncomms4728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ghezraoui H., Piganeau M., Renouf B., Renaud J.-B., Sallmyr A., Ruis B., Oh S., Tomkinson A.E., Hendrickson E.A., Giovannangeli C., et al. Chromosomal translocations in human cells are generated by canonical nonhomologous end-joining. Mol. Cell. 2014;55:829–842. doi: 10.1016/j.molcel.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bae S., Kweon J., Kim H.S., Kim J.-S. Microhomology-based choice of Cas9 nuclease target sites. Nat. Methods. 2014;11:705–706. doi: 10.1038/nmeth.3015. [DOI] [PubMed] [Google Scholar]
- 23.van Overbeek M., Capurso D., Carter M.M., Thompson M.S., Frias E., Russ C., et al. DNA repair profiling reveals nonrandom outcomes at Cas9-mediated breaks. Mol. Cell. 2016;63:633–646. doi: 10.1016/j.molcel.2016.06.037. [DOI] [PubMed] [Google Scholar]
- 24.Yoshihara M., Hayashizaki Y., Murakawa Y. Genomic instability of iPSCs: challenges towards their clinical applications. Stem Cell Rev. Rep. 2017;13:7–16. doi: 10.1007/s12015-016-9680-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim K.P., Wu Y., Yoon J., Adachi K., Wu G., Velychko S., MacCarthy C.M., Shin B., Röpke A., Arauzo-Bravo M.J., et al. Reprogramming competence of OCT factors is determined by transactivation domains. Sci. Adv. 2020;6:eaaz7364. doi: 10.1126/sciadv.aaz7364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Z., Oron E., Nelson B., Razis S., Ivanova N. Distinct lineage specification roles for NANOG, OCT4, and SOX2 in human embryonic stem cells. Cell Stem Cell. 2012;10:440–454. doi: 10.1016/j.stem.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 27.Veitia R.A., Bottani S., Birchler J.A. Gene dosage effects: nonlinearities, genetic interactions, and dosage compensation. Trends Gen. 2013;29:385–393. doi: 10.1016/j.tig.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 28.Li P.P., Margolis R.L. Use of single guided Cas9 nickase to facilitate precise and efficient genome editing in human iPSCs. Sci. Rep. 2021;11:9865. doi: 10.1038/s41598-021-89312-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hyodo T., Rahman M.L., Karnan S., Ito T., Toyoda A., Ota A., Wahiduzzaman M., Tsuzuki S., Okada Y., Hosokawa Y., Konishi H. Tandem paired nicking promotes precise genome editing with scarce interference by p53. Cell Rep. 2020;30:1195–1207.e7. doi: 10.1016/j.celrep.2019.12.064. [DOI] [PubMed] [Google Scholar]
- 30.Guilak F., Pferdehirt L., Ross A.K., Choi Y.-R., Collins K., Nims R.J., Katz D.B., Klimak M., Tabbaa S., Pham C.T.N. Designer stem cells: genome engineering and the next generation of cell-based therapies. Orthopaedic Research Society. 2019;37:1287–1293. doi: 10.1002/jor.24304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tuladhar R., Yeu Y., Tyler Piazza J., Tan Z., Rene Clemenceau J., Wu X., Barrett Q., Herbert J., Mathews D.H., Kim J., et al. CRISPR-Cas9-based mutagenesis frequently provokes on-target mRNA misregulation. Nat. Commun. 2019;10:4056. doi: 10.1038/s41467-019-12028-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elsner H.-A., Blasczyk R. Immunogenetics of HLA null alleles: implications for blood stem cell transplantation. Tissue Antigens. 2004;64:687–695. doi: 10.1111/j.1399-0039.2004.00322.x. [DOI] [PubMed] [Google Scholar]
- 33.Nagarajan U.M., Bushey A., Boss J.M. Modulation of gene expression by the MHC class II transactivator. J. Immunol. 2002;169:5078–5088. doi: 10.4049/jimmunol.169.9.5078. [DOI] [PubMed] [Google Scholar]
- 34.Devaiah B.N., Singer D.S. CIITA and its dual roles in MHC gene transcription. Front. Immunol. 2013;4:476. doi: 10.3389/fimmu.2013.00476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bruchez A., Sha K., Johnson J., Chen L., Stefani C., McConnell H., Gaucherand L., Prins R., Matreyek K.A., Hume A.J., et al. MHC class II transactivator CIITA induces cell resistance to Ebola virus and SARS-like coronaviruses. Science. 2020;370:241–247. doi: 10.1126/science.abb3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nakagawa M., Taniguchi Y., Senda S., Takizawa N., Ichisaka T., Asano K., Morizane A., Doi D., Takahashi J., Nishizawa M., et al. A novel efficient feeder-free culture system for the derivation of human induced pluripotent stem cells. Sci. Rep. 2014;4:3594. doi: 10.1038/srep03594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Funakoshi S., Miki K., Takaki T., Okubo C., Hatani T., Chonabayashi K., Nishikawa M., Takei I., Oishi A., Narita M., et al. Enhanced engraftment, proliferation and therapeutic potential in heart using optimized human iPSC-derived cardiomyocytes. Sci. Rep. 2016;6 doi: 10.1038/srep19111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen S., Zhou Y., Chen Y., Gu J. fastp: an ultra-fast all-in-one FASTQ preprocessor. Bioinformatics. 2018;34:i884–i890. doi: 10.1093/bioinformatics/bty560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li H., Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shiraishi Y., Sato Y., Chiba K., Okuno Y., Nagata Y., Yoshida K., Shiba N., Hayashi Y., Kume H., Homma Y., et al. An empirical Bayesian framework for somatic mutation detection from cancer genome sequencing data. Nucleic Acids Res. 2013;41:e89. doi: 10.1093/nar/gkt126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rausch T., Zichner T., Schlattl A., Stütz A.M., Benes V., Korbel J.O. DELLY: structural variant discovery by integrated paired-end and split-read analysis. Bioinformatics. 2012;28:i333–i339. doi: 10.1093/bioinformatics/bts378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koboldt D.C., Zhang Q., Larson D.E., Shen D., McLellan M.D., Lin L., Miller C.A., Mardis E.R., Ding L., Wilson R.K. VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 2012;22:568–576. doi: 10.1101/gr.129684.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thorvaldsdóttir H., Robinson J.T., Mesirov J.P. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Briefings Bioinf. 2013;14:178–192. doi: 10.1093/bib/bbs017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.