Abstract
PURPOSE
Researchers aimed to describe general practitioners’ understanding of appropriate ultrasound use, to record actual scanning practices of early adopters in general practice, and to identify differences between attitudes and actual practice via a mixed methods analysis.
METHODS
This study was part of a larger multistage mixed methods research framework exploring the use of ultrasound in general practice in Denmark. We used an exploratory sequential approach in the data collection with initial qualitative findings from an interview study applied to building a quantitative questionnaire utilized in a cohort study. In addition, we merged the qualitative and quantitative data using joint display analysis to compare and contrast the results from the 2 stages of the study.
RESULTS
In the interviews, general practitioners described appropriate ultrasound use as point-of-care examinations with a clear purpose and limited to predefined specific conditions within delimited anatomic areas. They stated that general practitioners should receive formalized ultrasound training and be skilled in the examinations they perform. In the cohort study, general practitioners performed ultrasound examinations of anatomic areas with or without a defined clinical suspicion. Some performed ultrasound examinations for which they had no previous training or skills.
CONCLUSIONS
We found a difference between the ideas about the appropriate uses for ultrasound in general practice and the actual use by early adopters in clinical practice. Our findings suggest a need for evidence-based guidelines to support general practitioners in choosing which examinations to perform and strategies for developing and maintaining scanning competency.
Key words: family practice, general practice, primary health care, point-of-care systems, ultrasonography
INTRODUCTION
Point-of-care ultrasonography (POCUS) is performed by a frontline clinician and integrated into the examination of the patient.1 Despite lack of evidence-based guidelines, POCUS use is growing in general practice,2 although in Denmark, where this study was conducted, POCUS is not widely used. This may be an example of Rogers’ diffusion of an innovation,3 where the technology has been adopted by innovators and early adopters within the general practice community. Potentially, POCUS may lead to faster and more precise diagnoses and referrals.4,5 Introducing a diagnostic test entails potential unintended harms, however: misdiagnosis,6,7 over or underdiagnosis,8 and overtreatment.9,10 Point-of-care ultrasonography is used for a variety of conditions in general practice,2,4 but general practitioners (GPs) cannot achieve the same breadth and depth of experience as imaging specialists. Hence, defining the boundaries of POCUS in general practice seems necessary to guide appropriate practice.
Clinical guidelines should be developed from a thorough evaluation of the actual use of POCUS in general practice and based on best available evidence,11 but also include GPs’ perspectives on the type of examinations and competencies needed. This complex issue calls for mixed methods research, where integration of qualitative and quantitative approaches enables a more complete understanding by drawing on strengths of both methodologies12 with new inferences generated from their integration.13,14
This study is part of a larger, multistage mixed methods framework14 exploring the use of POCUS in general practice through several studies2,15,16 (Supplemental Appendix 1). Using previously unreported data, this study aims to describe general practitioners’ understanding of appropriate ultrasound use, record actual scanning practices of early adopters in general practice, and identify differences between attitudes and actual practice through a mixed methods analysis.
METHODS
Design
Prior to this study, data were collected using an exploratory sequential mixed methods approach13 where initial qualitative findings from the interview stage15 informed subsequent quantitative data collection in the cohort stage.16 In this study, mixed methods integration was achieved through merging13 as we gave equal emphasis to the qualitative themes from the interview stage and quantitative information from the cohort stage to compare and contrast the results13 (Supplemental Appendix 1).
Setting and Participants
Denmark has a tax-financed health care system, where patients are listed with a GP.17 The GPs provide primary health care in smaller clinics and act as gatekeepers for secondary health care. GPs have a post-graduate specialization in family medicine. They are self-employed and paid by the Danish regions through a combination of remuneration and fee-for-service. The use of gynecological/obstetric POCUS during hospital residency has been part of GP training for several years. General practitioners are not paid for performing POCUS in primary care, and relatively few GPs perform POCUS. Participants in the interview (n = 24) and cohort (n = 20) stages were recruited from the same population of GPs. Five GPs participated in both stages (Table 1).
Table 1.
Participating Physician Demographics
| Interview Stage | Cohort Stage | Overall Populationa | ||
|---|---|---|---|---|
| Characteristic | Nonusers (n = 11) |
US users (n = 13) |
US Users (n = 20) |
GPs in Denmark (n = 3,402) |
| Age, y | ||||
| <40 | 2 | 0 | 2 | ... |
| 40-50 | 1 | 6 | 14 | ... |
| 51-60 | 5 | 4 | 3 | ... |
| 61-70 | 3 | 3 | 1 | ... |
| Mean age, y | 52.4 | 52.2 | 46.2 | 52.2 |
| Gender, No. | ||||
| Male | 7 | 11 | 14 | 1,605 |
| Female | 4 | 2 | 6 | 1,797 |
| Experience as a general practitioner,b y | ||||
| <10 | 3 | 4 | ... | ... |
| 10-20 | 3 | 6 | ... | ... |
| >20 | 5 | 3 | ... | ... |
| Experience using POCUS in general practice, y | ||||
| <2 | ... | 7 | 6 | ... |
| 2-5 | ... | 4 | 11 | ... |
| >5 | ... | 2 | 3 | ... |
| Type of POCUS training, No. | ||||
| No training | 4 | 0 | 0 | ... |
| Residency | 6 | 1 | 0 | ... |
| Course | 0 | 5 | 4 | ... |
| Course and residency | 1 | 7 | 16 | ... |
| Practice community character, No. | ||||
| Urban | 5 | 8 | 12 | ... |
| Mixed | 5 | 5 | 6 | ... |
| Rural | 1 | 0 | 2 | ... |
| Practice region, No. | ||||
| North Denmark region | 3 | 2 | 4 | 301 |
| Central Denmark region | 4 | 4 | 3 | 807 |
| Region of Southern Denmark | 1 | 2 | 7 | 782 |
| Region Zealand | 1 | 0 | 2 | 460 |
| Capital region of Denmark | 2 | 5 | 4 | 1,052 |
| Practice size, No. of patients | ||||
| <2,000 | 2 | 4 | 3 | ... |
| 2,000-5,000 | 5 | 4 | 10 | ... |
| >5,000 | 4 | 5 | 7 | ... |
| Type of practice,c No. | ||||
| Partnership | 9 | 9 | 17 | ... |
| Solo | 1 | 2 | 1 | 929 |
| Collaboration | 1 | 2 | 2 | ... |
GP = general practitioner; POCUS = point-of-care ultrasonography; US = ultrasonography.
Data available from the Danish Medical Association (PLO faktaark 2018).
Becoming a GP in Demark requires a 6-year post-graduate specialization in family medicine. A few GPs may have been working or received training in other specialties before they entered family medicine training but there is no formal sub-specialization of Danish GPs.
Partnership practice is defined as a clinic owned and administrated by more than 1 GP. Solo practice is a clinic owned and administrated by just 1 GP. Collaboration practice is a clinic owned by 1 GP or several GPs, but administrated in collaboration with other GP clinics.
Qualitative Interview Stage
From August 2016 through March 2017, we sampled and interviewed POCUS users and nonusers aiming for maximum variation in the GPs’ characteristics (Table 1).15 Recruitment of both groups was done purposively, one at a time, based on the concept of information power,18 and stopped when no new information emerged in the semistructured interviews. We used an interview guide, transcribed interviews verbatim, and analyzed text using Systematic Text Condensation.19 The analysis included: developing an overall impression, identifying and sorting meaning units, condensing, and synthesizing. For the present study, we included the analytic themes “appropriate use of ultrasound in general practice” and “the need for regulations” (Supplemental Appendix 2).
Quantitative Cohort Stage
The prospective cohort study (Clinical trials registration number: NCT03375333) included 18 GP practices with 20 POCUS users and 574 patients.16 The GPs were enrolled from January 2018 through July 2018. Each GP recruited patients examined with POCUS during 1 month. Data were collected during the consultation using an online registration before and after the use of POCUS. The GPs provided background information through a questionnaire at baseline. A POCUS skills assessment of each participant was completed 1 to 2 weeks before they enrolled patients, using an adapted version of the generic Objective Structured Assessment of Ultrasound Skills assessment tool.20
We conducted a subanalysis of individual POCUS users to examine the extent that they restricted their use of POCUS. Specifically, we looked at (1) the proportion of focused vs exploratory examinations and (2) the number of different anatomic areas evaluated. We further examined individual users’ restrictions in terms of their own ultrasound competencies by calculating the proportion of ultrasound scans performed in anatomic areas in which (3) the GP had received formal training and (4) the GP had been assessed as skilled (Supplemental Appendix 3).
Mixed Methods Merging Stage
We used joint display analysis.21 First, we identified links between qualitative themes and quantitative constructs in relation to the (1) purpose of the examination, (2) anatomic area evaluated, (3) GP’s ultrasound training, and (4) GP’s ultrasound skills. Second, we organized and reorganized data in tables, developing different iterations as new understandings emerged. After developing 4 joint displays illustrating the order in the data collection, origin of data, and links between the 2 data sets, we interpreted the data collectively and drew meta-inferences from the 4 points of comparison.
RESULTS
Interview Qualitative Findings
Use of POCUS was described as appropriate and recommended for use in the context of general practice, but as something distinct from the traditional ultrasound examinations performed in secondary care. The GPs explained that POCUS should match the working conditions and patient encounters in general practice. As such, GPs talked about 4 dimensions of appropriate use of POCUS: the purpose of examination, the type of examination, the GP’s training, and the GP’s skills. Inappropriate use was described, not as the contrary, but as experimental or too extensive use, in which GPs exceeded their own abilities.
Both POCUS nonusers and users described general practice as a diverse field of medicine with the hallmark of unregulated subspecialization for GPs with areas of special interest. These GPs described the professional norm to be self-regulation guided by their moral responsibilities and awareness of their own competencies that entails providing patient care up to a certain level before referring patients to specialists.
Overall, nonusers described a clear distinction in scope between appropriate and inappropriate use of POCUS in general practice. In contrast, POCUS users defined appropriate use in less definitive terms and, for some, described appropriate uses were not in line with their actual use.
Purpose of POCUS in General Practice
All participants stated that POCUS in general practice should be used for focused examinations with a clear clinical purpose aimed to address specific clinical questions in symptomatic patients (Figure 1). Some participants even proposed that POCUS in general practice should be limited to rule-in examinations leaving it to imaging specialists to conduct detailed examinations and to rule out disease.
Figure 1.
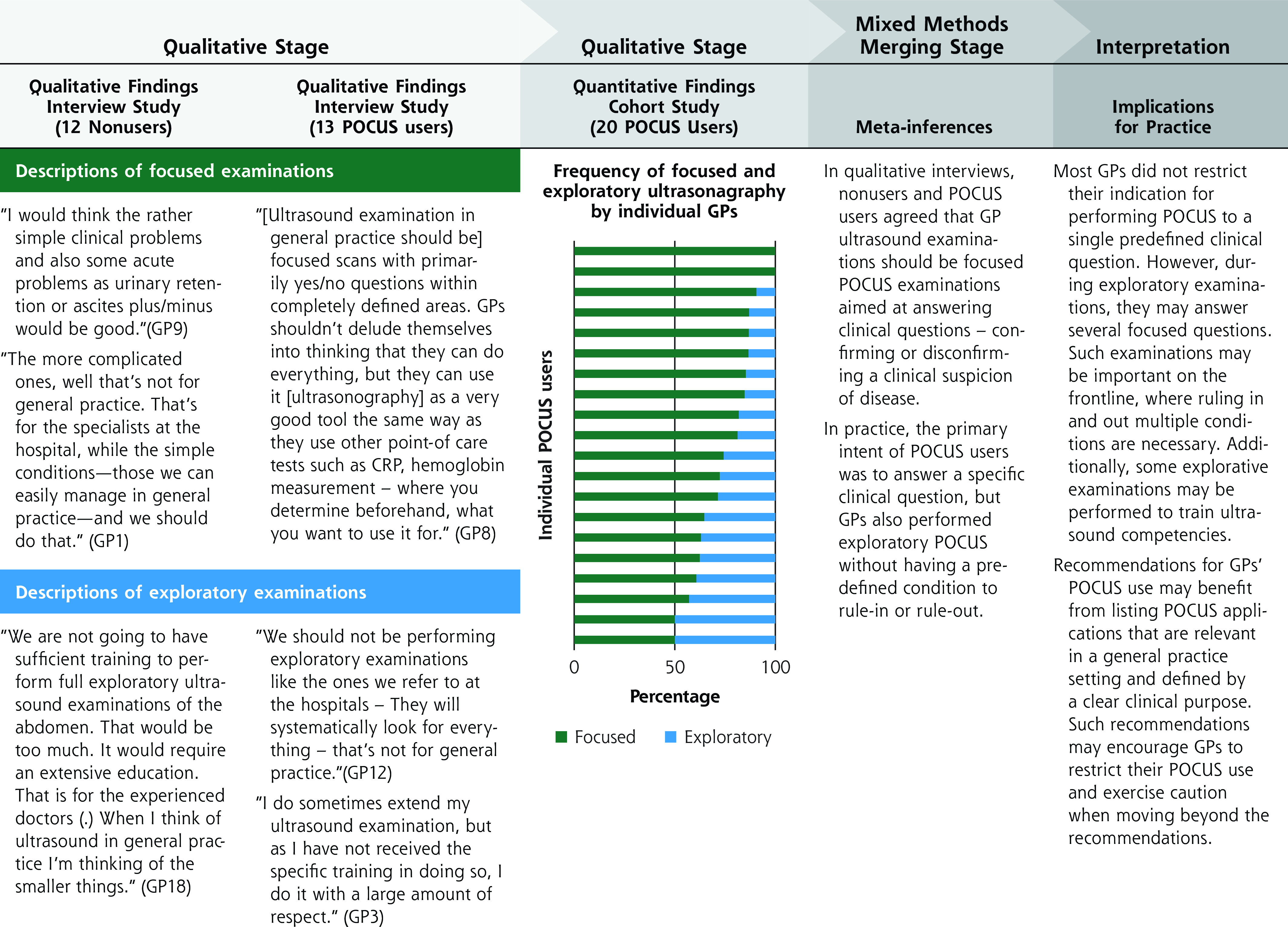
Mixed methods findings on the purpose of POCUS in general practice.
GP = general practitioner; Nonuser = a GP who is not using POCUS; POCUS = point-of-care ultrasonography; POCUS user = a GP who uses POCUS.
Nonusers described exploratory examinations motivated by the GP’s curiosity or fascination with the technology as highly inappropriate. In contrast, POCUS users found some exploratory examinations appropriate as long as the GP exercised caution in drawing conclusions.
Application of POCUS in General Practice
The participants agreed that only some POCUS examinations should be performed by GPs, but they did not agree on which examinations. Some nonusers called for a restricted set of examinations that only included relevant and common conditions within a few anatomic areas. The POCUS users, however, talked about an individual’s application with a stepwise addition of POCUS (Figure 2) resulting in a POCUS portfolio based on individual GP’s interests, patient population, clinical routines, and competencies. Several of them opposed regulations limiting the use of POCUS in general practice as they feared their freedom to select applications in areas of interest would be reduced.
Figure 2.
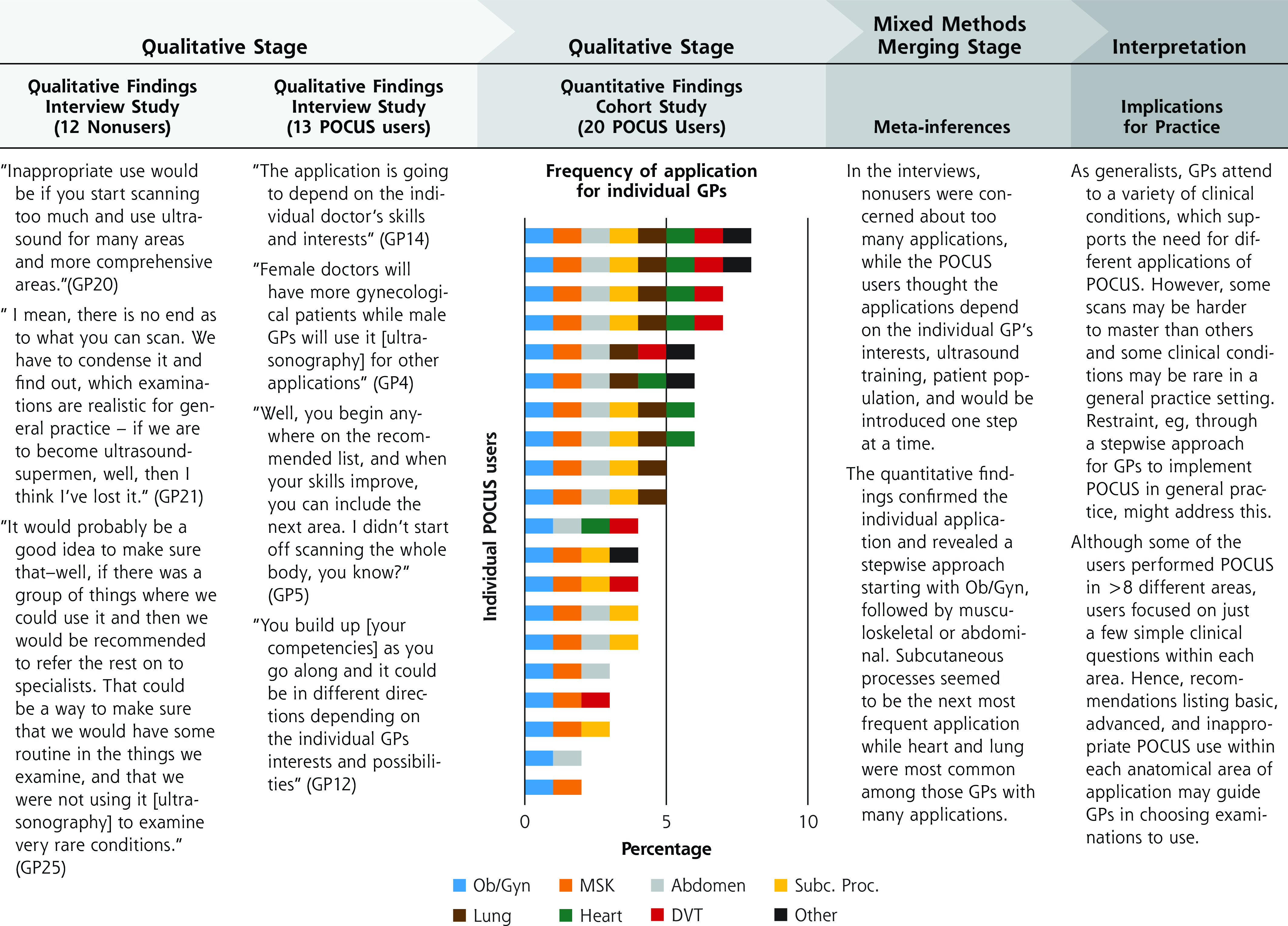
Mixed methods findings for the anatomical areas of POCUS examinations in general practice.
DVT = deep vein thrombosis; GP = general practitioner; MSK = musculoskeletal; Nonuser = a GP who is not using POCUS; Ob/Gyn = obstetrics and/or gynecology; POCUS = point-of-care ultrasonography; POCUS user = a GP who uses POCUS; Subc Proc= subcutaneous processes.
GP Ultrasound Training
All participants stated that appropriate use of POCUS required GPs to have ultrasonography knowledge obtained through formal training. They explained that some POCUS examinations would be easy to learn and master, while others would require more education and practice. They firmly believed that GPs could obtain the necessary competency. Several nonusers, however, questioned whether competence could be maintained with the low frequency of POCUS use in general practice. Nonusers believed that GPs should restrict themselves to only perform POCUS examinations for which they had formal training. Users described individual learning strategies such as unstructured study and practice of scanning competencies as appropriate and an inevitable part of POCUS in general practice. While nonusers talked about restricting the application of POCUS in general practice to avoid required extensive or continuous training programs, users talked about continuous POCUS education including a constant addition of more applications (Figure 3).
Figure 3.
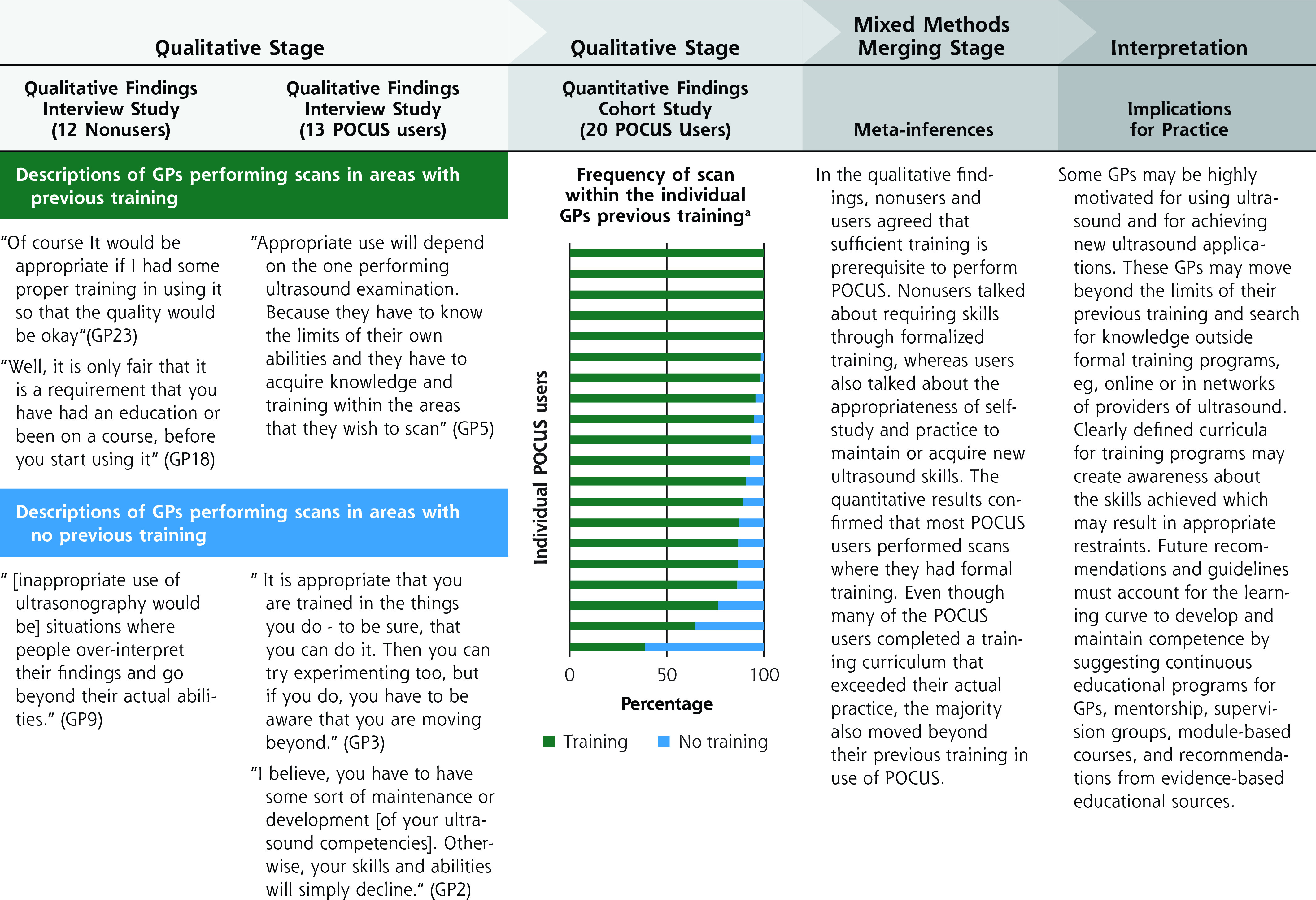
Mixed methods findings for GPs POCUS training and competencies.
GP = general practitioner; Nonuser = a GP who is not using POCUS; POCUS = point-of-care ultrasonography; POCUS user = a GP who uses POCUS.
a All GPs had all participated in formalized training in the use of POCUS. Ten GPs had participated in musculoskeletal POCUS courses, 3 in abdominal courses, and 2 in gynecological/obstetric courses. Fifteen GPs had participated in an extensive 12-month POCUS course targeting general practice. Nine of these GPs had also taken additional courses. Finally, 5 GPs had previous experience with using more advanced ultrasonography in a hospital setting; 2 in cardiology and 3 in gynecology.
GP Ultrasound Skills
All participants described how the appropriate scope of POCUS depended on GPs staying within the limits of their own abilities. The nonusers believed that GPs should only perform POCUS examinations for which they had sufficient skills and that GPs should be careful to not expand POCUS examinations into areas where they were not able to interpret the ultrasound images (Figure 4). The users agreed, but they also described cautious expansion of the application of POCUS to gain new skills.
Figure 4.
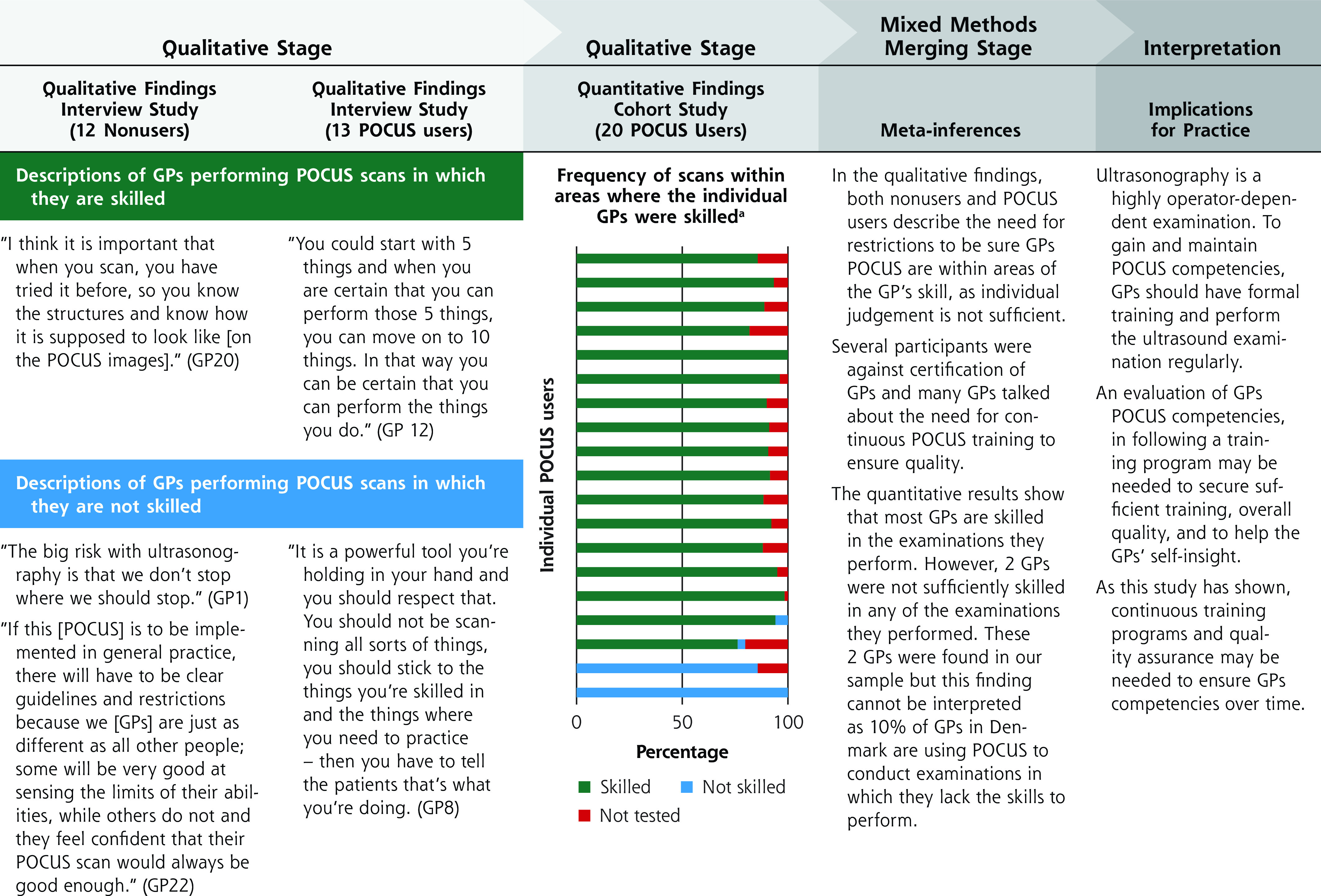
Mixed methods findings about GPs POCUS skills.
GP = general practitioner; nonuser = a GP who is not using POCUS; POCUS = point-of-care ultrasonography; POCUS user = a GP who uses POCUS.
a Skills were assessed using an adapted version of the generic Objective Structured Assessment of Ultrasound Skills assessment tool (Supplemental Appendix 2).
Some users and nonusers described how appropriate use and GP skills could be secured through POCUS certification, but the majority of participants opposed this. Having to be certified to perform an examination in general practice was deemed nontraditional and they feared that agreeing to certification in one area of competence could lead to similar requirements in other areas.
Cohort Quantitative Findings
Focused vs Exploratory POCUS Examinations
The mean proportion of focused examinations was 75.4% (95% CI, 68.3-83.0) (Figure 1). Among the 18 GPs who reported performing exploratory examinations, the mean proportion was 24.5% (95% CI, 17.3-13.6). No demographic characteristics distinguished outliers or the GPs above and below average.
Types of POCUS Applications
POCUS use ranged from 2 to more than 8 different applications with gynecological/obstetric scans being most common (Figure 2). The GPs using POCUS for most applications were the GPs with the most extensive training, and the 2 GPs using only 2 applications had training from a previous hospital employment supplemented with 1 or 2 day-courses.
POCUS Applications and Formal Training
Five of the 20 GPs only performed POCUS within areas that they had previously received formal training (Figure 3). These 5 GPs were among the GPs with the fewest anatomic areas of application (2 to 4 areas). The other 15 GPs performed examinations outside anatomic areas where they had previously received training.
POCUS Applications and GP Skills
The users’ ultrasound skills varied (Supplemental Appendix 4). Most participants, however, only performed ultrasound examination in anatomic areas where they were skilled (Figure 4). Four GPs performed POCUS examinations in anatomic areas where they had been assessed to be unskilled. No demographic characteristics distinguished these from the other GPs.
Findings From Mixed Methods Data Merging
In study interviews, nonusers and users all talked about normative use of POCUS. The nonusers exhibited a more rigid understanding of the boundaries of appropriate use, whereas the POCUS users had vaguer descriptions including accounts of deviating behavior. The cohort study confirmed such deviations. The mixed methods analysis revealed that although most POCUS users primarily scanned according to general perspectives on appropriate use, they also performed exploratory examinations and few restricted their use to limited anatomic areas of application. Most POCUS users performed examinations that were beyond their previous formal training and a few performed examinations in anatomic areas where they were unskilled (Figure 1-4).
DISCUSSION
This study revealed important differences between GPs’ attitudes and their actual use of POCUS.
The sequential design of this study made it possible to explore and quantify the qualitative findings from the interviews. Comparison was limited, however, to the outcomes measured in the cohort study. Hence, other factors characterizing the extent of POCUS in general practice, for example, the scanning protocols used, were not explored.
Generalizability of our results is limited by the low number of participants and self-reported outcomes. In addition, the studies were conducted in Denmark where POCUS is not widely used, and the users are most likely a select group of innovative GPs. The organization and regulation of Danish general practice, including the lack of fee for performing POCUS, differs from other countries.17 This potentially limits external validity. The aim of this study, however, was to gain a deeper understanding on how POCUS is used in general practice when there are no guidelines or recommendations. Our findings included fundamental professional considerations for general practice rather than national organizational aspects of primary care. Furthermore, the GPs were not driven by financial incentives, but used POCUS because they found it relevant to their general practice. Hence, our findings are likely to be transferable and could, therefore, guide relevant POCUS use in other primary care situations and countries.
In the interviews, all GPs talked about appropriate use of POCUS as restricted use. Previous studies have pointed out the importance of regulation for other procedures used in general practice.22,23 The lack of evidence-based clinical guidelines and regulations on POCUS in general practice may foster the opportunistic, individualized, and less restricted applications found in the cohort study. It remains unknown if this leads to negative effects on patient outcomes.
The POCUS users’ deviation from fundamental professional considerations for appropriate use may be understood with Rogers’ theory of diffusion of innovations.3 According to Rogers, early adopters, like the GPs in this study, are innovators, who venture into new areas, adapt new technology, and have a willingness to take risks. Later adopters of technology tend to wait for recommendations and be less adventurous.
A few attempts have been made to guide GP use of POCUS,5,24,25 but evidence from in-hospital settings does not account for the different epidemiology of illnesses in general practice (especially the low pre-test probability of disease), or national differences in primary care organization and working conditions. Applications for rare conditions such as ocular ultrasound for detached retina24 or chest ultrsasound for pneumothorax,25 and applications that require extensive training, such as, cardiac ultrasound,4,5 have been recommended for GPs. This and previous studies,2,16 however, suggest that such applications may not be very useful in general practice. Other medical specialties26,27 have listed suitable POCUS applications and defined the purpose for POCUS with a clinical question. Some guidelines have defined a scanning protocol that includes the extent of the examinations.28,29 Such guidelines may reduce the individual applications of POCUS revealed in this study and create awareness of basic, advanced, and discouraged applications of POCUS.
Our findings confirm that achieving and maintaining POCUS competence requires continuous use and practice. A recent review30 described skills assessments after short training programs for GPs, but how busy GPs will be able to maintain and develop their skills over time is an area ripe for scientific investigation. Reports have emphasized visual knowledge in relation to skills development31,32 and international recommendations for continuous training under supervision.6,33,34 In countries like Denmark, however, opportunities for supervision are sparse, frequency of POCUS use is low,2,16 and no skills assessment or accreditation is required.5 This study showed that some GPs do not have the recommended skills despite having participated in POCUS training.
There is a need for studies to explore skill acquisition strategies for GPs, identify which competences are needed, and determine how GPs can develop competence and maintain skills over time.
Developments in ultrasound technology provide new diagnostic opportunities for primary care physicians and this study may carry implications beyond POCUS. Despite scant evidence, the POCUS use in general practice is increasing.36 Given the discrepancy between the GPs’ perspectives on appropriate use and their actual practice, efforts to guide GPs venturing into POCUS use are needed. Patients seem to appreciate the use of POCUS,37,38 but questions remain regarding the reliability and diagnostic accuracy of a GP POCUS scan30 and the challenges of evaluating and monitoring technology based in the community.39,40 Until data is available for developing evidence-based guidelines11 about appropriate and inappropriate POCUS use in general practice, interim experience-based recommendations based on basic ethical clinical principles, eg, primum non nocere (first, do no harm), may guide and encourage prudence among GPs (Figures 1-4).
Including the 4 dimensions of appropriate use of POCUS described in this study in future guideline development11 and research strategies may help determine the normative boundaries between appropriate and inappropriate use of POCUS in general practice. Hence, future research should focus on exploring diagnostic precision of different GP-performed POCUS examinations and patient prognosis following POCUS use in general practice.
Supplementary Material
Acknowledgments
The authors would like to thank the participating GPs for their participation in this study. The collaboration of Drs Guetterman and Fetters was possible through the Mixed Methods Program in the Department of Family Medicine at the University of Michigan, USA.
Footnotes
Conflicts of interest: authors report none.
Funding support: This study is independent research funded by Center for General Practice at Aalborg University, Denmark and the Danish Committee of Multipractice Studies in General Practice.
References
- 1.Moore CLCJ, Copel JA.. Point-of-care ultrasonography. N Engl J Med. 2011; 364(8): 749-757. 10.1056/NEJMra0909487 [DOI] [PubMed] [Google Scholar]
- 2.Andersen CA, Holden S, Vela J, Rathleff MS, Jensen MB.. Point-of-care ultrasound in general practice: a systematic review. Ann Fam Med. 2019; 17(1): 61-69. 10.1370/afm.2330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rogers EM. Evolution: diffusion of innovations. International Encyclopedia of Social & Behavioral Sciences. 2001; 8: 4982-4986. [Google Scholar]
- 4.Steinmetz P, Oleskevich S.. The benefits of doing ultrasound exams in your office. J Fam Pract. 2016; 65(8): 517-523. [PubMed] [Google Scholar]
- 5.Bhagra A, Tierney DM, Sekiguchi H, Soni NJ.. Point-of-care ultrasonography for primary care physicians and general internists. Mayo Clin Proc. 2016; 91(12): 1811-1827. 10.1016/j.mayocp.2016.08.023 [DOI] [PubMed] [Google Scholar]
- 6.Education and Practical Standards Committee, European Federation of Societies for Ultrasound in Medicine and Biology . Minimum training recommendations for the practice of medical ultrasound. Ultraschall Med. 2006; 27(1): 79-105. 10.1055/s-2006-933605 [DOI] [PubMed] [Google Scholar]
- 7.Dietrich CF, Goudie A, Chiorean L, et al. Point of care ultrasound: A WFUMB position paper. Ultrasound Med Biol. 2017; 43(1): 49-58. 10.1016/j.ultrasmedbio.2016.06.021 [DOI] [PubMed] [Google Scholar]
- 8.O’Sullivan JW, Albasri A, Nicholson BD, et al. Overtesting and undertesting in primary care: a systematic review and meta-analysis. BMJ Open. 2018; 8(2): e018557. 10.1136/bmjopen-2017-018557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin JS, Bowles EJA, Williams SB, Morrison CC.. Screening for thyroid cancer: Updated evidence report and systematic review for the US preventive services task force. JAMA. 2017; 317(18): 1888-1903. 10.1001/jama.2017.0562 [DOI] [PubMed] [Google Scholar]
- 10.Shabanzadeh DM, Sørensen LT, Jørgensen T.. A prediction rule for risk stratification of incidentally discovered gallstones: results from a large cohort study. Gastroenterology. 2016; 150(1): 156-167.e1. 10.1053/j.gastro.2015.09.002 [DOI] [PubMed] [Google Scholar]
- 11.Brozek JL, Akl EA, Alonso-Coello P, et al. ; GRADE Working Group . Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009; 64(5): 669-677. 10.1111/j.1398-9995.2009.01973.x [DOI] [PubMed] [Google Scholar]
- 12.Guetterman TC, Fetters MD, Creswell JW.. Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Ann Fam Med. 2015; 13(6): 554-561. 10.1370/afm.1865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Creswell JW, Plano Clark VL.. Designing and Conducting Mixed Methods Research. 2ed. SAGE Publications; 2011. [Google Scholar]
- 14.Fetters MD, Curry LA, Creswell JW.. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013; 48(6 Pt 2): 2134-2156. 10.1111/1475-6773.12117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andersen CA, Davidsen AS, Brodersen J, Graumann O, Jensen MB.. Danish general practitioners have found their own way of using point-of-care ultrasonography in primary care: a qualitative study. BMC Fam Pract. 2019; 20(1): 89. 10.1186/s12875-019-0984-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andersen CA, Brodersen J, Davidsen AS, et al. Use and impact of point-of-care ultrasonography in general practice: a prospective observational study. BMJ Open. 2020; 10: e037664. 10.1136/bmjopen-2020-037664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pedersen KM, Andersen JS, Søndergaard J.. General practice and primary health care in Denmark. J Am Board Fam Med. 2012; 25(Suppl 1): S34-S38. 10.3122/jabfm.2012.02.110216 [DOI] [PubMed] [Google Scholar]
- 18.Malterud K, Siersma VD, Guassora AD.. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016; 26(13): 1753-1760. 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- 19.Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012; 40(8): 795-805. 10.1177/1403494812465030 [DOI] [PubMed] [Google Scholar]
- 20.Tolsgaard MG, Todsen T, Sorensen JL, et al. International multispecialty consensus on how to evaluate ultrasound competence: a Delphi consensus survey. PLoS One. 2013; 8(2): e57687. 10.1371/journal.pone.0057687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fetters MD. Mixed Methods Research Workbook - Activities for Designing, Implementing and Publishing Projects. SAGE Publications; 2020. [Google Scholar]
- 22.Córdoba G, Holm A, Sørensen TM, et al. Use of diagnostic tests and the appropriateness of the treatment decision in patients with suspected urinary tract infection in primary care in Denmark - observational study. BMC Fam Pract. 2018; 19(1): 65. 10.1186/s12875-018-0754-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Ravesteijn H, van Dijk I, Darmon D, et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012; 86(1): 3-8. 10.1016/j.pec.2011.02.003 [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Family Physicians (AAFP) . Recommended curriculum guidelines for family medicine residents; point of care ultrasound. Published Dec 2016. Accessed Oct 28, 2019. https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf
- 25.The Danish College of General Practitioners (DSAM), Ultrasound interest group . Common trunk. Published 2015. Accessed Oct 28, 2019. https://www.dsam.dk/flx/organisation/udvalg_og_interessegrupper/ultralyd_i_almen_praksis/common_trunk/
- 26.Olgers TJ, Azizi N, Blans MJ, Bosch FH, Gans ROB, Ter Maaten JC.. Point-of-care Ultrasound (PoCUS) for the internist in acute medicine: a uniform curriculum. Neth J Med. 2019; 77(5): 168-176. [PubMed] [Google Scholar]
- 27.Ma IWY, Arishenkoff S, Wiseman J, et al. ; Canadian Internal Medicine Ultrasound (CIMUS) Group . Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) group. J Gen Intern Med. 2017; 32(9): 1052-1057. 10.1007/s11606-017-4071-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Via G, Hussain A, Wells M, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014; 27(7): 683.e-683.e33. 10.1016/j.echo.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 29.Volpicelli G, Elbarbary M, Blaivas M, et al. ; International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS) . International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012; 38(4): 577-591. 10.1007/s00134-012-2513-4 [DOI] [PubMed] [Google Scholar]
- 30.Andersen CA, Hedegård HS, Løkkegaard T, et al. Education of general practitioners in the use of point-of-care ultrasonography: a systematic review. Fam Pract. 2020. Dec 26: cmaa140. 10.1093/fampra/cmaa140 [DOI] [PubMed] [Google Scholar]
- 31.Bezemer J. Visual research in clinical education. Med Educ. 2017; 51(1): 105-113. 10.1111/medu.13163 [DOI] [PubMed] [Google Scholar]
- 32.Nicholls D, Sweet L, Muller A, Hyett J.. Teaching psychomotor skills in the twenty-first century: Revisiting and reviewing instructional approaches through the lens of contemporary literatures. Med Teach. 2016. Oct; 38(10): 1056-1063. 10.3109/0142159X.2016.1150984 [DOI] [PubMed] [Google Scholar]
- 33.Atkinson P, Bowra J, Lambert M, Lamprecht H, Noble V, Jarman B.. International Federation for Emergency Medicine point of care ultrasound curriculum. CJEM. 2015; 17(2): 161-170. 10.1017/cem.2015.8 [DOI] [PubMed] [Google Scholar]
- 34.The Royal College of Radiologists . Ultrasound training recommendations for medical and surgical specialities. Third edition. Published Jun 2017. Accessed on Jun 2019. https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr173_ultrasound_training_med_surg.pdf
- 35.Mengel-Jørgensen T, Jensen MB.. Variation in the use of point-of-care ultrasound in general practice in various European countries. Results of a survey among experts. Eur J Gen Pract. 2016; 22(4): 274-277. 10.1080/13814788.2016.1211105 [DOI] [PubMed] [Google Scholar]
- 36.Myklestul HC, Skonnord T, Brekke M.. Point-of-care ultrasound (POCUS) in Norwegian general practice. Scand J Prim Health Care. 2020; 38(2): 219-225. 10.1080/02813432.2020.1753385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Andersen CA, Brodersen J, Rudbæk TR, Jensen MB.. Patients’ experiences of the use of point-of-care ultrasound in general practice - a cross-sectional study. BMC Fam Pract. 2021; 22(1): 116. 10.1186/s12875-021-01459-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pertierra-Galindo N, Salvo-Donangelo L, Salcedo-Joven MI, Román-Crespo B, Froilán Torres MC.. [Study of patient satisfaction when performing an ultrasound in Primary Care]. Semergen. 2019; 45(4): 239-250. 10.1016/j.semerg.2018.08.007 [DOI] [PubMed] [Google Scholar]
- 39.Chavannes N, Schermer T, Akkermans R, et al. Impact of spirometry on GPs’ diagnostic differentiation and decision-making. Respir Med. 2004; 98(11): 1124-1130. 10.1016/j.rmed.2004.04.004 [DOI] [PubMed] [Google Scholar]
- 40.Wagenvoort LME, Willemsen RTA, Konings KTS, Stoffers HEJH.. Interpretations of and management actions following electrocardiograms in symptomatic patients in primary care: a retrospective dossier study. Neth Heart J. 2019; 27(10): 498-505. 10.1007/s12471-019-01306-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


