Abstract
Background
The development of guidelines by gastroenterology societies increasingly stresses evidence-based endoscopic practice.
Aims
We performed a systematic assessment to determine whether endoscopic video teaching platforms incorporate evidence-based educational strategies and methods in order to disseminate guideline-based endoscopic management strategies.
Methods
Platforms with a video component were systematically identified using the Google search engine, Apple and Android application stores, and searching four major gastroenterology society websites and three known platforms, to identify all relevant platforms. Two video samples from each teaching platform were reviewed independently by two authors and assessed for use of a priori defined principles of evidence-based medicine, as determined by consensus agreement and for the use of simulation.
Results
Fourteen platforms were included in the final analysis, and two videos from each were analyzed. One of the 14 platforms used simulation and incorporated evidence-based medicine principles consistently. Nine of the 14 platforms were not transparent in regard to citation. None of the platforms consistently cited the certainty of evidence or explained how evidence was selected.
Conclusions
Education of guideline-based endoscopic management strategies using principles of evidence-based medicine is under-utilized in endoscopic videos. In addition, the use of cognitive simulation is absent in this arena. There is a paucity of evidence-based cognitive endoscopy simulators designed for fellows that incorporate systematic evaluation, and efforts should be made to create this platform.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10620-022-07558-w.
Keywords: Endoscopy, Education, Guidelines, Simulation
Introduction
Efforts to improve dissemination of and adherence to guidelines and evidence-based practices are of great importance [1, 2]. Decision making based on evidence-based medicine and outcomes compared to decision making based on theory, dogma, or past experience alone improves patient outcomes by providing care that is beneficial [3–5]. While this is true in all fields of medicine, it is increasingly recognized as an important component of cognitive endoscopy.
Cognitive endoscopic skills include the constellation of the appropriate knowledge and reasoning to determine the best approach of applying technical skills to practice. Specific cognitive skills include recognition of abnormalities, identification of pathology, and development of appropriate management decisions based on endoscopic findings [6]. Isolated cognitive endoscopic training primarily exists in the form of endoscopy videos and didactic sessions. As emphasis on evidence-based endoscopic practice increases, there should be a commensurate increase in evidence-based content in cognitive endoscopy education. There are many endoscopy videos readily available online. However, whether these videos employ evidence-based principles has not been studied.
Furthermore, there is evidence that simulation is a useful tool in medical education, particularly in promoting understanding and enhancing content retention [6–9, 11]. Simulation is an attempt to replicate a real-world experience and prompts the learner to react as if they are truly in that experience [7, 11–13]. Recently, a high-fidelity simulation program for endoscopy was noted be an effective learning tool that helped novice endoscopists acquire basic skills of upper endoscopy and successfully apply them to practice [14]. However, high-fidelity simulators are costly and not widely available. Low-fidelity simulation replicates real life to a lesser degree and focuses on forcing the trainee to replicate the emotions and cognitions of the real-life clinical encounter, rather than the physical environment. These simulations may involve computer modules featuring clinical vignettes, or hands on practice with a simple mannequin. Prior studies have found that low-fidelity simulation is non-inferior to high-fidelity simulation, even in procedural training [15]. Therefore, endoscopic video platforms may benefit from the incorporation of simulation as a teaching technique, without incurring additional cost. Whether the currently available endoscopic video teaching platforms employ simulation also has not been studied.
The addition of evidence-based society guidelines into teaching and the use of simulation to existing educational platforms may be a simple and inexpensive way to optimize cognitive endoscopy education. In this systematic evaluation, we assessed all educational platforms readily accessible to trainees with the aim to determine the availability of videos or modules that incorporate evidence-based society guidelines into their teaching and use the technique of simulation to enhance the learning experience.
Methods
Systematic Search to Identify Existing Educational Platforms
A systematic evaluation was conducted to identify currently available online endoscopy learning platforms on April 1, 2020. Platforms that were freely available to the public, and those that were available at no additional cost to members of the American Gastroenterological Association (AGA), American College of Gastroenterology (ACG), American Society of Gastrointestinal Endoscopy (ASGE), and the American Association for the Study of Liver Diseases (AASLD), were included. These sites were selected as many fellowship programs encourage their fellows to become members of these major national societies. A single reviewer (SS or MI), searched the ACG, AGA, ASGE, and AASLD websites for dedicated online endoscopy educational platforms. The Digital Atlas of Video Endoscopy (DAVE) project, Asian Pacific Association of Gastroenterology (APAGE), and World Endoscopy Organization (WEO) were known platforms, so they were also searched.
Subsequently, individual Google searches were conducted using the search terms “gastroenterology education,” “endoscopy simulation,” “virtual endoscopy,” “endoscopy education,” “cognitive endoscopy,” and “learning endoscopy” to identify any platforms that were not part of a major GI society or known platforms. Inclusion criteria were a free platform (or included with basic trainee membership to a society) with a specific aim to teach endoscopy via a video. Additionally, each platform included was assessed to ensure that it was either associated with a medical society or medical personnel. Two reviewers (SS, MI) viewed the first 20 results of each search, excluding advertisement sites, both independently and in duplicate. Twenty results were deemed an adequate portrayal of websites considered widely available, given that less than 2.5% of people performing Google searches click past the tenth position in a Google search [9]. Subsequently, we searched iOS (Apple®) and Android® application (app) stores using the search term “endoscopy.” The first 25 applications of each store were reviewed (for a total of 50 across Android and Apple app stores). As there were limited data on user behavior on finding the desired search in the application store, we extrapolated from data on Google search behavior.
The search results were screened by each reviewer (SS, MI) by assessing the title. Any title that met our inclusion criteria was included for full website/app assessment of educational endoscopy videos. Within each website/app, the random videos were selected using a website that generates a random number [10]. That number was used to select the link within each website/app and had to meet inclusion criteria. If a platform did not have an endoscopic educational video, it was excluded. If there was a disagreement between the two reviewers in regards to excluding or including a website/app, it was automatically included for full assessment. Full website and app assessment was also done in duplicate, and disagreements were handled via discourse. If disagreement could not be resolved through discussion, a third reviewer (RS or MK) was utilized.
Systematic Evaluation of Identified Platforms
Evaluation of whether the video purposely taught evidence-based practices and focused on clinical outcomes-based learning was performed. The transparency and origin of the evidence for each included platform’s teaching was assessed. Specific criteria included whether the platform explicitly cited the evidence for the endoscopic technique it is teaching (either verbally or in writing), whether the platform discussed the quality of this evidence using a systematic methodology or established terminology, whether the platform focused on guideline-based practice, and whether the evidence cited was selected in a systematic manner.
Each identified platform was then evaluated to determine whether it met the definition of simulation. We defined simulation as “a method used in health care education to replace or amplify real performance of endoscopy with scenarios designed to replicate the experience of performing real endoscopic procedures wherein the trainee is required to perform at least some of the tasks they usually would in a real endoscopic procedure, using a computer-based module [2].” Because we hypothesized that many platforms would not employ simulation, the analysis was broadened to also evaluate whether the platform was interactive. Interactivity was defined as, “an instructional method that engages students by inviting the learner to actively participate in the learning process, most commonly via answering questions [11, 13]” (Table 1). Two videos (termed “samples”) from each included website or app were randomly selected for review. If the website or app contained more than one platform, 2 videos from each platform were reviewed. Additionally, whether or not the platform involved an endoscopist in its creation was evaluated.
Table 1.
Definitions of analyzed educational features
| Term | Definition |
|---|---|
| Didactic | Any presentation in which the presenter attempts to explicitly impart information, knowledge, and/or skills to the learner |
| Interactivity | An instructional method that engages students by inviting the learner to actively participate in the learning process, most commonly via answering questions |
| Simulation | A method used in healthcare education to replace or amplify real performance of endoscopy with scenarios designed to replicate the experience of performing real endoscopic procedures wherein the trainee is required to perform at least some of the tasks he/she usually would in a real endoscopic procedure, using a computer-based module |
*For modified definitions, see Supplementary table—Definition of educational features and origins
Results
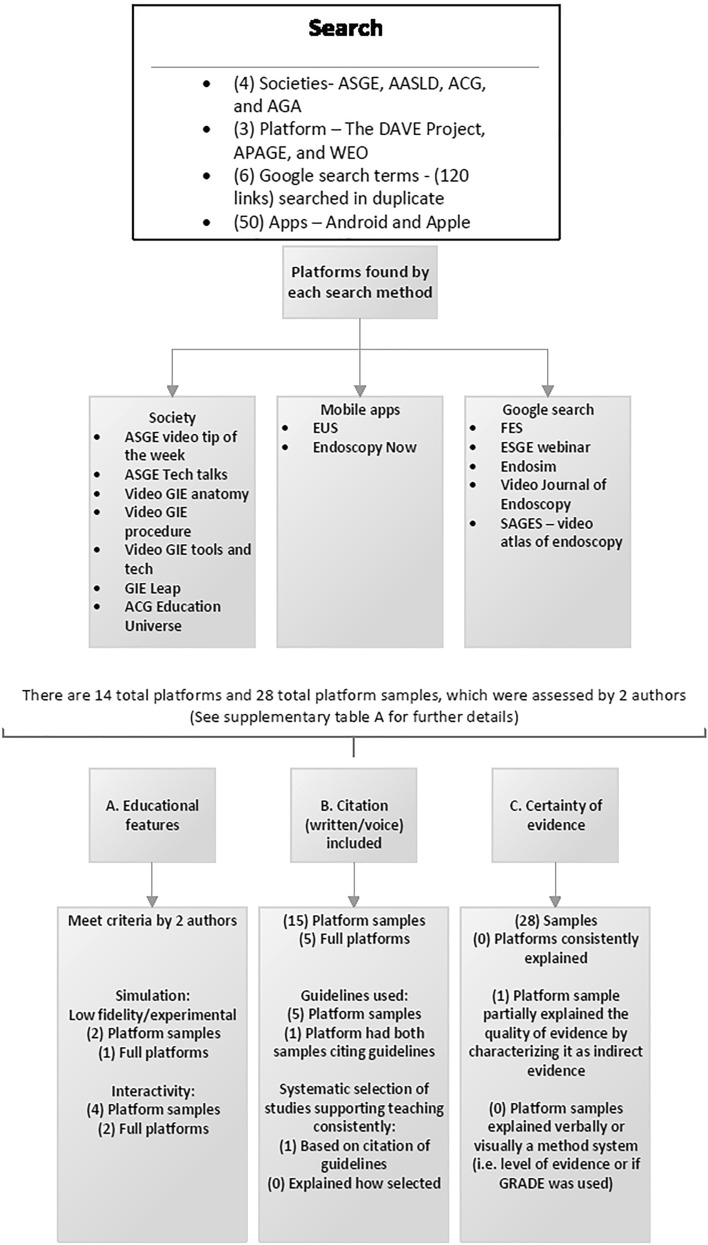
After reviewing the society websites for the AGA, ASGE, ACG AASLD, APAGE, and WEO, seven total platforms that met the inclusion criteria were found. APAGE did not have endoscopy videos. WEO did not have educational endoscopy videos as of April 2020 when the search was completed. After review of 20 Google links each for six search terms, five additional platforms that met our inclusion criteria were extracted. Review of 50 mobile applications revealed two additional mobile apps that met inclusion criteria. The DAVE project was excluded as the website and videos could not be accessed consistently during the time of our review and was therefore not considered to be widely and easily available. Thus, in total, 14 platforms were included. Two videos were sampled from each of the 14 platforms. There were a total of 28 platform samples.
In terms of evidence-based teaching and transparency, 15 of the 28 video samples incorporated verbal citation or written citation of evidence for the practice it was demonstrating. If both samples of a platform met a particular criteria or definition, it was deemed to do this consistently. Five of 14 platforms consistently incorporated voice or written citations. However, only one of 14 platforms used guidelines consistently to cite their teaching. No platforms consistently discussed quality or certainty of evidence. One sample of a platform did discuss how the evidence for their teaching originated from an indirect population, but did not use a method system to describe the certainty of the evidence (e.g., very low, low, moderate, high; using GRADE methodology). Only one platform consistently based their teaching on a systematic approach of selecting the evidence, but no platform explained how the evidence was selected. Overall, only one platform (ESGE) used both simulation and evidence-based teaching according to the pre-defined criteria (Fig. 1 & Supplementary Table—platform results). Only one of 14 platforms (two of 28 video samples) incorporated simulation according to the a priori definition, and two of the 14 platforms (four of 28 video samples) were interactive (Fig. 1 & Supplementary Table—Platform results). All platforms involved an endoscopist in its creation.
Fig. 1.
Results of the systematic search
Discussion
There are a scarcity of data that systematically appraise the widely available online platforms for cognitive endoscopy. We assessed them primarily for their relation to the body of available evidence on the endoscopic technique of their focus. We found that selection of evidence to support teaching of a subject was not universally transparent. More than half of the platforms did not consistently provide an immediate verbal or written citation. Only one platform consistently used a guideline to support its teaching. Although not every topic will have a guideline to support its teaching, there are advantages to ensure dissemination of knowledge is based on the entire body of evidence which includes minimizing bias as this could occur from selection of individual studies [16, 17]. Only one platform explained the certainty of evidence. However, even this platform did not do this consistently or use a method system in their discussion. These issues highlight that there is a deficiency in education of guideline-based endoscopic management strategies.
We also found a paucity of platforms that were interactive, and even fewer platforms that used simulation. Simulation-based learning is associated with more engagement by participants when compared with a traditional video lecture [18]. Similarly, interactivity is supported by evidence as a tool that promotes understanding and retention of content [6–9, 11]. In other areas of medical education, increasing student participation in educational activities has improved examination scores and higher-end cognitive application of the material [19]. These areas in existing platforms can be optimized to create a richer cognitive endoscopy experience.
While one platform met our criteria for simulation, this platform featured videos that were approximately one hour in length. The average adult attention span is 15–20 minutes [20]. Furthermore, trainees prefer shorter-time didactics [21]. Micro-learning, a concept based on short educational sessions and activities to teach a topic, is beneficial in healthcare education [20, 22, 23]. Additionally, surveys of surgical resident trainees suggest an interest in learning evidence-based medicine, but time is an issue [24]. Educational platforms that incorporate brief teaching videos are thus more likely to be utilized and may be more effective than longer presentations.
It is acknowledged that searching for free or included in trainee membership platforms will not encompass all the available platforms for endoscopic education. However, this search was done in a systematic manner and thus is reproducible for future research. In addition, only two random samples from each platform were assessed. However, this assessment was done to identify whether an educational feature was included consistently by a platform. Given the paucity of consistent inclusion of educational features, it was not deemed necessary to sample more videos. Moreover, there are numerous videos placed on social media and streaming platforms such as YouTube® and it was not feasible to sample every subscription in this review. Thus, to mitigate missing any major relevant platform, “Google searches” with defined search terms were performed.
Furthermore, the COVID-19 pandemic’s adverse effects on endoscopic training highlighted the importance of these supplemental forms of endoscopic training and led to several new cognitive endoscopic teaching programs that were created after the time our review was completed [25]. These include new AGA On Demand modules, ASGE Endo Hangouts and the Twitter-based @ScopingSundays, among others, which were not assessed in our study21, 26, 27. Future studies could address how the COVID-19 pandemic has changed the educational landscape.
In conclusion, this systematic evaluation and analysis of available endoscopy teaching platforms at the onset of the COVID-19 pandemic found that education of guideline-based endoscopic management strategies using principles of evidence-based medicine and transparency of citations is under-utilized. As national societies utilize major resources in creating rigorous guidelines, educational platforms could be used to disseminate this knowledge. Also, almost no endoscopy teaching platforms invite the learner to make real-time management decisions in a simulated endoscopy procedure. Few platforms are interactive. These deficiencies represent a void in cognitive endoscopic training which has become even more important during the COVID-19 pandemic and arguably represents substantial needs in a digital, evidence-based era. Incorporation of these tools to existing or similarly designed platforms may fill this void and would be a welcome addition to cognitive endoscopy education.
Supplementary Information
Below is the link to the electronic supplementary material.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Grimshaw JM, Schünemann HJ, Burgers J, et al. Disseminating and implementing guidelines: article 13 in Integrating and coordinating efforts in COPD guideline development. An official ATS/ERS workshop report. Proc Am Thorac Soc. 2012;9(5):298–303. doi: 10.1513/pats.201208-066ST. [DOI] [PubMed] [Google Scholar]
- 2.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003 doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 3.Guyatt GH, Oxman AD, Kunz R, et al. What is "quality of evidence" and why is it important to clinicians? BMJ. 2008;336(7651):995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zaman A, Fennerty MB. Evidence-based medicine: what on earth does it have to do with endoscopy? and is it the new "three-letter" word in endoscopic research? Gastrointest Endosc. 2003;58(6):895–901. doi: 10.1016/s0016-5107(03)02305-8. [DOI] [PubMed] [Google Scholar]
- 5.Strate LL, Liu YL, Syngal S, Aldoori WH, Giovannucci EL. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300(8):907–914. doi: 10.1001/jama.300.8.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Munshi F. In: Low-versus high-fidelity simulations in teaching and assessing clinical skills. Lababidi H, editor. Journal of Taibah University Medical Sciences; 2015. pp. 12–15. [Google Scholar]
- 7.Passiment M. In: Medical simulation in medical education: results of an AAMC survey. Sacks H, editor. Washington: Association of American Medical Colleges; 2011. [Google Scholar]
- 8.McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Med Educ. 2010;44(1):50–63. doi: 10.1111/j.1365-2923.2009.03547.x. [DOI] [PubMed] [Google Scholar]
- 9.Zhang D, Zhou L, Briggs RO, Nunamaker JF., Jr Instructional video in e-learning: assessing the impact of interactive video on learning effectiveness. Inf Manag. 2006;43(1):15–27. doi: 10.1016/j.im.2005.01.004. [DOI] [Google Scholar]
- 10.https://randomwordgenerator.com/number.php. (n.d.). Random Number Generator. Retrieved from Random Number Generator
- 11.Evaluation of Evidence-Based Practices inOnline Learning: A Meta-Analysis andReview of Online Learning Studies. 2010:94.
- 12.Merriam-Webster.com Dictionary. 2020. https://www.merriam-webster.com/
- 13.Morgan S, Martin L, Howard B, Mihalek PH. Active learning: what is it and why should i use it. Dev Bus Simul Exp Learn. 2005;32:219–220. [Google Scholar]
- 14.Soetikno R, Cabral-Prodigalidad PA, Kaltenbach T, Investigators A. Simulation-based mastery learning with virtual coaching: experience in training standardized upper endoscopy to novice endoscopists. Gastroenterology. 2020;159(5):1632–1636. doi: 10.1053/j.gastro.2020.06.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lefor AK, Harada K, Kawahira H, Mitsuishi M. The effect of simulator fidelity on procedure skill training: a literature review. Int J Med Educ. 2020;11:97–106. doi: 10.5116/ijme.5ea6.ae73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pae CU. Why systematic review rather than narrative review? Psychiatry Investig. 2015;12(3):417–419. doi: 10.4306/pi.2015.12.3.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah R, Morgan RL, Falck-Ytter Y, Mustafa RA. Have we not learned from past mistakes? Am J Respir Crit Care Med. 2018;197(11):1499–1500. doi: 10.1164/rccm.201711-2200LE. [DOI] [PubMed] [Google Scholar]
- 18.Courteille O, Fahlstedt M, Ho J, et al. Learning through a virtual patient vs recorded lecture: a comparison of knowledge retention in a trauma case. Int J Med Educ. 2018;9:86–92. doi: 10.5116/ijme.5aa3.ccf2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Starmer DJ, Duquette S, Howard L. Participation strategies and student performance: an undergraduate health science retrospective study. J Chiropr Educ. 2015;29(2):134–138. doi: 10.7899/JCE-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hotelling BA. Considerations when using videos in Lamaze classes. J Perinat Educ. 2012;21(3):189–192. doi: 10.1891/1058-1243.21.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chak A. ASGE endo hangout with GI fellows. United States: American Society of Gastrointestinal Endoscopy; 2020. [Google Scholar]
- 22.De Gagne JC, Park HK, Hall K, Woodward A, Yamane S, Kim SS. Microlearning in health professions education: scoping review. JMIR Med Educ. 2019;5(2):e13997. doi: 10.2196/13997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Narula N, Ahmed L, Rudkowski J. An evaluation of the '5 Minute Medicine' video podcast series compared to conventional medical resources for the internal medicine clerkship. Med Teach. 2012;34(11):e751–e755. doi: 10.3109/0142159X.2012.689446. [DOI] [PubMed] [Google Scholar]
- 24.Kwaan MR, Melton GB. Evidence-based medicine in surgical education. Clin Colon Rectal Surg. 2012;25(3):151–155. doi: 10.1055/s-0032-1322552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah R, Satyavada S, Ismail M, et al. COVID-19 pandemic through the lens of a gastroenterology fellow: looking for the silver lining. Gastrointest Endosc. 2020;92(2):394–398. doi: 10.1016/j.gie.2020.03.3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.@ScopingSundays. In: @ScopingSundays, editor. Twitter 2020.
- 27.Association AG. Appropriate Referral for Endoscopic Polyp Removal. In: Douglas K. Rex M, Dennis J. Yang M, Heiko Pohl M, MD SK, V. Raman Muthusamy M, editors. AGA University2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.