Abstract
Background
Extracorporeal shock wave therapy (ESWT) is a modern physiotherapeutic method that is useful for treating musculoskeletal conditions. There are still limited data from well-designed studies evaluating the clinical efficiency of ESWT in low back pain (LBP). Therefore, this study aimed to assess the effectiveness of the focused ESWT (fESWT) in reducing pain and improving the functional status of patients with chronic LBP.
Material/Methods
The study involved 40 patients with L5-S1 discopathy with chronic LBP pain who were randomized into 2 groups: group A (n=20, mean age of 42.3±13.1 years) and group B (n=20, mean age of 45.4±14 years). Group A was an experimental group treated with an fESWT at the lumbar and sacral spine (0.15 mJ/mm2, 1000 pulses, 4 Hz). Group B was a control group, treated with a sham fESWT. The treatment protocol in both groups included identical stabilization training (45 minutes, once a day, 5 days a week). Study outcomes included subjective pain with a visual analog scale (VAS) and Laitinen Pain Scale (LPS), and functional status using the Oswestry Disability Index (ODI). Measurements were made before and after treatments, as well as follow-up observations at 1 and 3 months following ESWT. The study was prospectively registered at the ISRCTN registry platform (no. ISRCTN13785224).
Results
There was a significant analgesic effect (VAS and LPS) in both groups; however, it was significantly greater in the experimental group compared to the sham group (P<0.05). A more significant decrease in the perceived pain (VAS and LPS) was observed immediately after the active fESWT therapy. In follow-up observations (after 1 and 3 months), there were no significant between-group differences (P>0.05). Also, there was a significant effect in terms of functional state (ODI) for both groups (P<0.05); however, between-group comparisons revealed no statistically significant differences (P>0.05).
Conclusions
Focused ESWT with an exercise program can be effective in patients with chronic LBP. ESWT allows reducing pain, although it does not seem to significantly improve a patient’s functional state.
Keywords: Chronic Pain, Extracorporeal Shockwave Therapy, Functional Status, Low Back Pain, Physical Therapy Modalities, Randomized Controlled Trial
Background
Extracorporeal shock wave (ESWT) is a modern physiotherapeutic method which is useful for musculoskeletal conditions. Despite some evidence from recent systematic reviews, meta-analyses [1–4], and the Cochrane recommendations [5], there are still inconclusive results on ESWT. Moreover, the literature on ESWT in low back pain (LBP) treatment in the Web of Science Core Collection, PubMed, and MEDLINE databases is limited. There are only 6 randomized clinical trials (RCTs) showing the effect of ESWT on LBP [6–11] that went through methodological quality analysis using the Physiotherapy Evidence Database (PEDro) score (Table 1). Based on objective data, levels of methodological quality of these randomized clinical trials vary from medium to low. Furthermore, most studies did not meet the essential criteria of Evidence-Based Physiotherapy (no Cochrane recommendation and PEDro indexation), suggesting that this topic still requires in-depth investigation. Therefore, in practice, it is not easy to objectively analyze the clinical effectiveness of such procedures, together with precise recommendations regarding doses, treatment parameters, duration of the procedure, and other relevant aspects of the treatment protocol. For example, it is unclear how to evaluate radial vs focused techniques.
Table 1.
A randomized clinical trial addressing the treatment of LBP using ESWT.
| Researchers | PEDro score | Study limitations |
|---|---|---|
| Taheri et al 2021 [6] | 4/10 | No random allocation No baseline comparability No blinded subjects No blinded therapists No blinded assessors No adequate follow-up |
| Walewicz et al 2019 [7] | 7/10 | No concealed allocation No blinded therapists No blinded assessors |
| Moon et al 2017 [8] | 7/10 | No blinded therapists No adequate follow-up No intention-to-treat analysis |
| Schneider 2018 [9] | 6/10 | No concealed allocation No blinded subjects No blinded therapists No blinded assessors |
| Notarnicola et al 2018 [10] | 3/10 | No concealed allocation No baseline comparability No blinded subjects No blinded therapists No adequate follow-up No intention-to-treat analysis No point estimates and variability |
| Han et al 2015 [11] | 3/10 | No sham therapy No placebo No blinded subjects No blind therapists No blinded assessors No adequate follow-up No intention-to-treat analysis |
PEDro – Physiotherapy Evidence Database.
The radial method (rESWT) is based on pneumatic technology, using the principle of accelerated cartridge impact by compressed air under high pressure. In this way, the shock wave penetrates the body with a radiated beam, and its energy decreases with the depth of penetration. The pulse lasts a maximum of 5 ms, and the pressure reached by the wave does not exceed 1 MPa [12]. The focused technique (fESWT) is characterized by a stronger stimulus, having a more intense effect on the tissues. Unlike the radial method, the focused technique uses electroacoustic technology. Under the influence of high voltage, an acoustic shock wave is created in the applicator, forming a focused stimulus using a special lens. This stimulus with special coupling attachments is introduced into the patient’s body at an appropriate depth, at the assumed pressure of up to 100 MPa, and the pulse duration up to 0.2 μs [13,14].
In 2020, our research team published clinical data on radial ESWT in treating patients with chronic LBP [15] that had the methodologically highest level (9/10 points) according to PEDro score. Our results showed that the ESWT technique might be especially used in maintaining remission of symptoms and preventing recurrence of disease. Therefore, our team has decided to examine an fESWT, which theoretically might have greater technological possibilities than the radial technique. Thus, the study aimed to assess the effectiveness of focused ESWT in reducing pain intensity and improving functional efficiency in patients with chronic LBP.
Material and Methods
Study Design
The research was carried out in the Clinical Research Laboratory of the Institute of Health Sciences of the University of Opole. The study was conducted in cooperation with the Department of Physiotherapy of the Wrocław Medical University in Poland. The local and independent Bioethics Committee of the University of Opole approved the study protocol (no. KB/90/FI/2018). The study was prospectively registered at the International Standard Randomized Controlled Trial Number (ISRCTN) registry database (no. ISRCTN13785224). Each participant provided their written informed consent prior to the study. The studies were conducted in accordance with the Helsinki Declaration and Good Clinical Practice guidelines.
Randomization and Blinding
Patients were selected for this randomized and single-blinded project by an internist, radiologist, neurologist, neurosurgeon, orthopedist, and physiotherapist. After a positive qualifying procedure, participants were randomly assigned to real or sham ESWT treatments using a computer random number generator (www.random.com). Both groups also performed basic central spine stabilization exercises. The allocation to the group did not depend on the research staff implementing the therapy and analyzing the results. The same therapist conducted all tests and surveys. One physiotherapist performed all treatments and stabilization exercises.
Participants
Patients with L5-S1 discopathy, chronic pain, and no spinal surgical intervention were qualified. The participants were of legal age and had current magnetic resonance imaging (MRI) scans confirming the LBP syndrome – type 3 changes in section L5-S1 according to Modic classification (MC), which describes vertebral endplate lesions.
The exclusion criteria were: discopathy beyond the L5-S1 (MC type 1 and 2), no pain and reduced mobility in the lumbosacral segment, other spinal conditions (fractures, tumors, spondylolisthesis, rheumatic diseases, cauda equina syndrome), pregnancy or ovulation, neurological deficits, implanted cardiac pacemaker, blood coagulation disorders, metal implants within the application site, sensory disturbances, mental disorders, cancer, skin lesions within the treatment site, viral and bacterial infections, painkillers, and anti-inflammatory drugs.
The study involved 40 patients with L5-S1 discopathy of the spine with chronic pain lasting at least 12 weeks. Patients were randomized into 2 groups: group A (n=20) with a mean age of 42.3±13.1 years and group B (n=20) with a mean age of 45.4±14 years. The groups were homogeneous regarding demographic characteristics (Table 2) and initial pain and functional status assessments. Following the Consolidated Standards of Reporting Trials (CONSORT) guidelines for registered randomized clinical trials, the patient flow over the entire period of the study is shown in Figure 1. In both groups, all participants completed treatment. All patients were assessed 1 month later and 3 months after the end of the study. It should be noted that 1 person in group A (business trip at the time of taking the measurements) and 2 people in group B (taking painkillers) were excluded from the statistical analysis.
Table 2.
Characteristics of the study groups.
| Variable | Experimental fESWT group | Control fESWT group | P value | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ̄ | Me | Min | Max | Q1 | Q3 | SD | χ̄ | Me | Min | Max | Q1 | Q3 | SD | ||
| Age [years] | 4.3 | 43.0 | 18.0 | 64.0 | 33.0 | 49.0 | 13.1 | 45,4 | 49.0 | 22.0 | 76.0 | 36.0 | 55.0 | 14.0 | 0.490 |
| Body weight [kg] | 72.8 | 73.0 | 57.0 | 90.0 | 61.0 | 83.0 | 11.6 | 74.5 | 77.0 | 55.0 | 87.0 | 72.0 | 81.0 | 9.2 | 0.989 |
| Body height [cm] | 172.6 | 173.0 | 156,0 | 186.0 | 164.0 | 178.0 | 7.9 | 168.1 | 170.0 | 150.0 | 182.0 | 163.5 | 172.0 | 8.8 | 0.068 |
| BMI [kg/m2] | 24.3 | 23.6 | 18.3 | 30.5 | 21.8 | 27.8 | 3.9 | 26.5 | 27.1 | 22.0 | 32.0 | 24.3 | 27.8 | 3.0 | 0.102 |
| Disease duration [months] | 57.5 | 48.0 | 3.0 | 204.0 | 24.0 | 84.0 | 50.9 | 61.8 | 60.0 | 3.0 | 180.0 | 24.0 | 72.0 | 53.1 | 0.989 |
| Sex | F – n=10; 50.0% M – n=10; 50.0% |
F – n=10; 50.0% M – n=10; 50.0% |
1.000 | ||||||||||||
fESWT – focused extracorporeal shock wave; n – number of individuals; χ̄ – mean; Me – median; Min – minimum value; Max – maximum value; Q1 – lower quartile; Q3 – upper quartile; SD – standard deviation; F – female; M – male.
U-Mann-Whitney;
Chi-square test.
Figure 1.
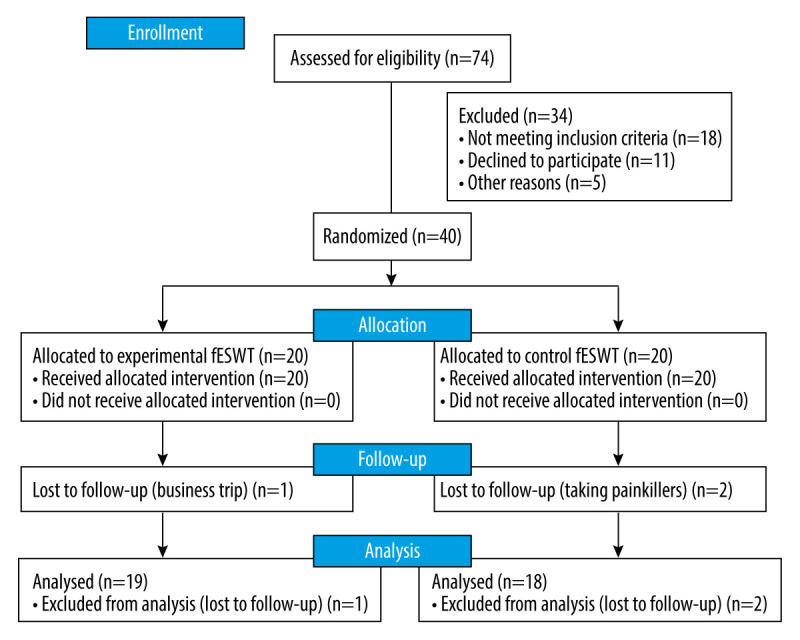
CONSORT flow chart of study participants. fESWT – focused extracorporeal shock wave.
Treatment
Group A was an experimental group treated with an fESWT shockwave using the Duolith SD1 Tower device (Storz Medical, Switzerland; Figures 2, 3). Each procedure was performed using the contact method at the lumbar and sacral spine level in the area of greatest pain indicated by the patient (Figure 4). The following parameters were used for the therapy: energy flux density 0.15 mJ/mm2 (1000 pulses), frequency 4 Hz. An ultrasound gel was used as a coupling substance between the applicator and the patient’s skin to reduce tissue resistance. Treatments were performed twice a week (Monday and Thursday) for 5 weeks (10 treatments in total). The therapy was conducted under ultrasound guidance.
Figure 2.
Duolith SD1 Tower device for high-energy fESWT.
Figure 3.

fESWT applicator used in this study.
Figure 4.

Treatment session using the fESWT applicator.
Group B was a control group, treated with a sham fESWT. Stimulation took place using a special polyethylene insert mounted on the top of the applicator, which absorbed energy and limited its spread in the tissue. The treatment procedure was identical to condition A in terms of the audible signals and the technical parameters used in the actual procedure.
The treatment protocol in both groups included identical stabilization training (45 minutes, once a day, 5 days a week, Monday to Friday) with myofascial relaxation of the extensors of the spine, activation of the lumbo-sacro-pelvic complex and deep muscles, stimulation of proper breathing, and dynamic postural exercises.
Measurement
Therapeutic progress was assessed by analyzing subjective pain sensations using a visual analog scale (VAS), on which the patient-rated the symptoms on a numerical scale from 0 to 10 (0 indicated no pain, 10 indicated the strongest pain).
The Laitinen Pain Scale (LPS) was also used, which measures 4 criteria of pain: its intensity, frequency of its occurrence, use of painkillers, and limitation of motor activity. Patients assigned points from 0 to 4 (0 – no pain, 4 – severe pain) to each of the determined indicators.
Functional fitness was assessed using the Oswestry Disability Index (ODI), which consists of 10 sections, with 8 related to activities of daily living and 2 related to pain concerns; responses are graded from 0 to 5, and the total ODI score is presented on a scoring system of 0–50 or a percentage system of 0–100% indicating the degree of disability.
Tests and questionnaires were administered in both groups at the beginning, after treatment, and during follow-up visits after 1 and 3 months. During this time, the patients were not receiving any other treatment.
Sample Size
The sample size was based on group differences in primary outcomes (means and standard deviations of pain experience), estimated at 26 participants (13 in each group). A 20% loss to follow-up was allowed for in calculations. The decreasing sample size also applied to historical information from our unit because 45% of patients offered conservative management (physical therapy agents) for LBP opted for ESWT within 6 months.
Statistical Analysis
Statistical analysis was performed using the Statistica 13 program (TIBCO, Inc., USA). Arithmetic means, medians, standard deviations, quartiles, and the range of variability (extreme values) were calculated for measurable variables. For qualitative variables, the frequencies were calculated (the results were given as percentages). Quantitative variables were subjected to the Shapiro-Wilk test to determine the normality of distribution. Comparisons between groups were made using the chi-square test (χ2). Within-group comparisons for measurement conditions 1, 2, 3, and 4 were performed by Friedman’s analysis of variance and a post hoc test (Dunn’s test). Finally, the comparison between the experimental and placebo groups was assessed using the Mann-Whitney U test. The level for statistical significance was α=0.05.
Results
Table 3 presents comparisons of pain (VAS) in both groups. There was a significant effect in both groups (P<0.05). The strongest analgesic effect was observed in the group treated with ESWT – by 5.7 points immediately after therapy, 5.5 points after 1 month, and 5.2 points after 3 months. In the sham ESWT (control) group, a significant decrease of 4.4 points occurred after therapy, then 4.2 points after 1 month, and 4.3 points after 3 months.
Table 3.
VAS scores in both groups.
| Variable | Measure | Experimental fESWT group | Control fESWT group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ̄ | Me | Min | Max | Q1 | Q3 | SD | χ̄ | Me | Min | Max | Q1 | Q3 | SD | ||
| VAS score | Before | 7.2 | 8.0 | 4.0 | 10.0 | 5.0 | 8.5 | 1.9 | 7.3 | 7.0 | 5.0 | 10.0 | 6.0 | 9.0 | 1.7 |
| After | 1.5 | 1.0 | 1.0 | 3.0 | 1.0 | 2.0 | 0.6 | 2.9 | 3.0 | 1.0 | 6.0 | 2.0 | 3.0 | 1.3 | |
| 1 month FU | 1.7 | 1.0 | 1.0 | 5.0 | 1.0 | 2.0 | 1.1 | 3.1 | 3.0 | 1.0 | 7.0 | 2.0 | 4.0 | 1.7 | |
| 3 months FU | 2.0 | 1.5 | 1.0 | 5.0 | 1.0 | 3.0 | 1.2 | 3.3 | 3.0 | 1.0 | 8.0 | 2.0 | 4.0 | 1.9 | |
| P value (main effect*) | <0.001 | <0.001 | |||||||||||||
| p-value (multiple comparisons**) | Before vs after: p<0.001 Before vs 1 month: p<0.001 Before vs 3 months: p<0.001 After vs 1 month: p=1.000 After vs 3 months: p=1.000 1 month vs 3 months: p=1.000 |
Before vs after: p<0.001 Before vs 1 month: p<0.001 Before vs 3 months: p<0.001 After vs 1 month: p=1.000 After vs 3 months: p=1.000 1 month vs 3 months: p=1.000 |
|||||||||||||
fESWT – focused extracorporeal shock wave; n – number of individuals; χ̄ – mean; Me – median; Min – minimum value; Max – maximum value; Q1 – lower quartile; Q3 – upper quartile; SD – standard deviation; FU – follow-up.
Friedman’s ANOVA;
Dunn’s test.
Comparing pain between the groups (using the VAS scale showed differences immediately after treatment and 1 month after the end of treatment (Figure 5). For the ESWT group, there was a significantly greater improvement in VAS scores compared to the sham group (P<0.05 for all values), suggesting a clinical superiority of ESWT over the other group. There were no differences in the 3-month follow-up (P>0.05); however, the patients in the experimental ESWT group had greater improvement compared to the control group. The results confirmed the effectiveness of the analgesic effect immediately after treatment and a favorable outcome in long-term follow-up despite the slow recurrence of symptoms.
Figure 5.
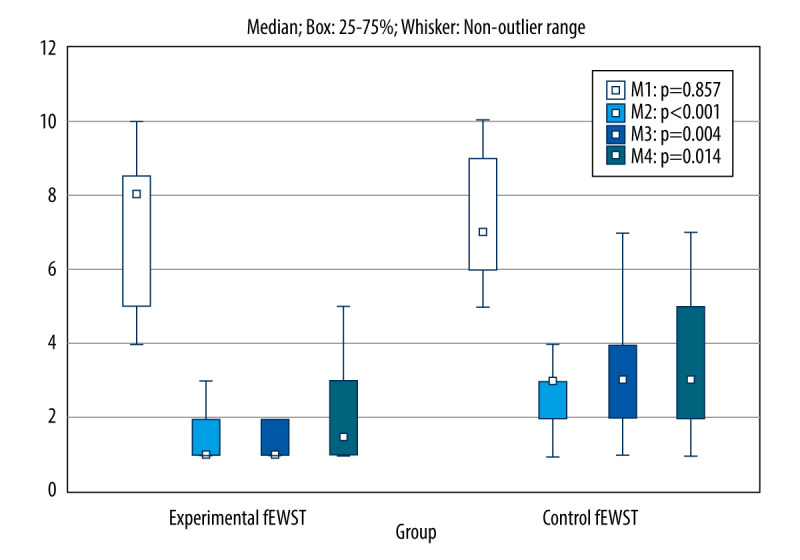
Comparison of VAS scores obtained in 4 measurements between the experimental and control group. fESWT – focused extracorporeal shock wave; M1 – before, M2 – after, M3 – after 1 month, M4 – after 3 months.
Table 4 shows the comparisons of perceived pain according to LPS in 4 measurements between the experimental and control groups. The mean pain scores changed significantly in both groups (main effect: P<0.05). A significant decrease in the perceived pain was observed immediately after the therapy by 6.9 points, after 1 month by 6.4 points, after 3 months by 6 points. However, in the control group, there was a significant decrease after the therapy by 4 points, after one month by 3.8 points, after 3 months by 3.4 points.
Table 4.
LPS scores in both groups.
| Variable | Measure | Experimental fESWT group | Control fESWT group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ̄ | Me | Min | Max | Q1 | Q3 | SD | χ̄ | Me | Min | Max | Q1 | Q3 | SD | ||
| LPS score | Before | 8.8 | 8.0 | 4.0 | 15.0 | 7.0 | 11.0 | 3.2 | 7.1 | 6.0 | 4.0 | 12.0 | 5.0 | 9.0 | 2.6 |
| After | 1.9 | 2.0 | 0.0 | 4.0 | 0.0 | 3.0 | 1.5 | 3.1 | 3.5 | 0.0 | 7.0 | 2.0 | 4.0 | 2.0 | |
| 1 month FU | 2.4 | 2.0 | 0.0 | 7.0 | 0.0 | 3.5 | 2.2 | 3.3 | 3.0 | 0.0 | 7.0 | 2.5 | 4.5 | 2.1 | |
| 3 months FU | 2.8 | 3.0 | 0.0 | 5.0 | 1.0 | 5.0 | 2.0 | 3.7 | 4.0 | 0.0 | 8.0 | 2.5 | 5.5 | 2.4 | |
| P value (main effect*) | <0.001 | <0.001 | |||||||||||||
| p-value (multiple comparisons**) | Before vs after: p<0.001 Before vs 1 month: p<0.001 Before vs 3 months: p=0.001 After vs 1 month: p=1.000 After vs 3 months: p=0.193 1 month vs 3 months: p=1.000 |
Before vs after: p<0.001 Before vs 1 month: p<0.001 Before vs 3 months: p=0.016 After vs 1 month: p=1.000 After vs 3 months: p=1.000 1 month vs 3 months: p=1.000 |
|||||||||||||
fESWT – focused extracorporeal shock wave; n – number of individuals; χ̄ – mean; Me – median; Min – minimum value; Max – maximum value; Q1 – lower quartile; Q3 – upper quartile; SD – standard deviation; FU – follow-up.
Friedman’s ANOVA;
Dunn’s test.
Patients from the experimental group differed from the control group immediately after treatment, indicating remission of pain (P<0.05). In follow-up observations (after 1 and 3 months), there were no significant differences (P>0.05) (Figure 6), although the trend for therapeutic advantage was still maintained.
Figure 6.
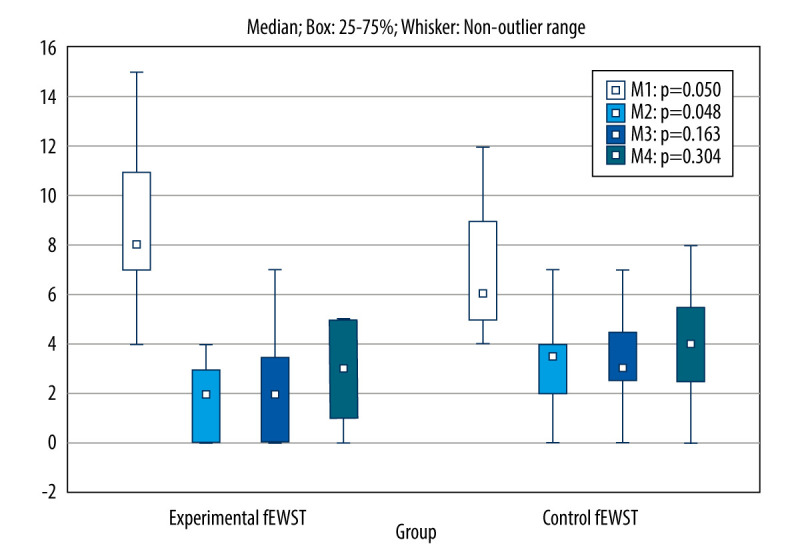
Comparison of LPS scores obtained in 4 measurements between the experimental and control group. fESWT – focused extracorporeal shock wave; M1 – before, M2 – after, M3 – after 1 month, M4 – after 3 months.
Table 5 shows the between-group comparisons of functional assessments taken with the ODI under 4 measurement conditions. There was a significant effect for both groups (significant effect: P<0.05). After the end of treatment in the experimental group, there was a decrease by 15.1 points, after 1 month by 16.1 points, and after 3 months by 15.1 points. The ESWT results suggested a stable clinical effect, taking into account the functional assessment of patients. On the other hand, there was a decrease after therapy by 13 points in the control group and conditions 1 month after, 13.8 points, and 3 months after 12.6 points. However, between-group comparisons revealed no statistically significant differences (Figure 7).
Table 5.
ODI scores in both groups.
| Variable | Measure | Experimental fESWT group | Control fESWT group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ̄ | Me | Min | Max | Q1 | Q3 | SD | χ̄ | Me | Min | Max | Q1 | Q3 | SD | ||
| ODI score | Before | 33.4 | 34.0 | 25.0 | 47.0 | 30.0 | 38.0 | 6.3 | 32.5 | 29.5 | 23.0 | 54.0 | 28.0 | 33.5 | 8.6 |
| After | 18.3 | 16.0 | 9.0 | 31.0 | 12.0 | 24.5 | 7.5 | 19.5 | 20.0 | 10.0 | 35.0 | 15.5 | 23.0 | 6.5 | |
| 1 month FU | 17.3 | 14.0 | 9.0 | 31.0 | 12.0 | 23.0 | 7.1 | 18.7 | 19.0 | 10.0 | 32.0 | 14.0 | 21.0 | 6.6 | |
| 3 months FU | 18.3 | 16.0 | 11.0 | 31.0 | 12.0 | 24.5 | 6.8 | 19.9 | 19.0 | 10.0 | 36.0 | 15.5 | 23.5 | 7.4 | |
| P value (main effect*) | <0.001 | <0.001 | |||||||||||||
| p-value (multiple comparisons**) | Before vs after: p<0.001 Before vs 1 month: p<0.001 Before vs 3 months: p<0.001 After vs 1 month: p=1.000 After vs 3 months: p=1.000 1 month vs 3 months: p=1.000 |
Before vs after: p<0.001 Before vs 1 month: p<0.001 Before vs 3 months: p<0.001 After vs 1 month: p=1.000 After vs 3 months: p=1.000 1 month vs 3 months: p=1.000 |
|||||||||||||
fESWT – focused extracorporeal shock wave; n – number of individuals; χ̄ – mean; Me – median; Min – minimum value; Max – maximum value; Q1 – lower quartile; Q3 – upper quartile; SD – standard deviation; FU – follow-up.
Friedman’s ANOVA;
Dunn’s test.
Figure 7.
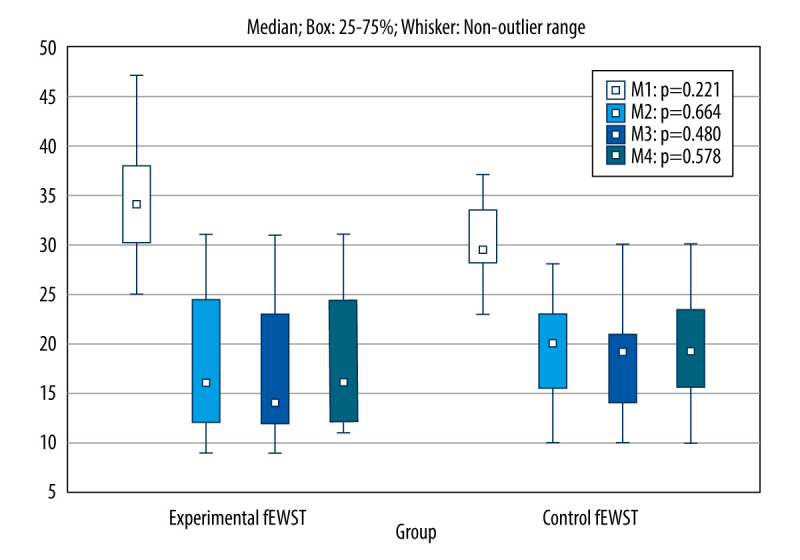
Comparison of ODI scores obtained in 4 measurements between the experimental and control group. fESWT – focused extracorporeal shock wave; M1 – before, M2 – after, M3 – after 1 month, M4 – after 3 months.
Discussion
Our experience with using rESWT [7,15] in LBP treatment procedures is far-reaching. Previous clinical studies have shown the high effectiveness of the procedure in reducing pain, enhancing the functional state of patients, and improving the stabilization of body posture. Notably, both publications showed that the therapeutic effect was maintained in long-term observation and was associated with longer remission of disease symptoms compared to standard physiotherapeutic methods.
However, the results of the present randomized clinical trial are not very promising. The analgesic effect was evident, but there was no strong improvement in functional status over the control group. Certainly, a more detailed analysis is needed, based on other research tools and scales of physical fitness, while maintaining the highest methodological levels (over 7 points on the PEDro scale).
There is only 1 previous report like the present results. In an Iranian study, Taheri et al [6] (only 4/10 points on the PEDro scale) verified the effectiveness of focus shock waves in combination with oral medications and exercise in reducing pain in LBP patients. Ultimately, 38 people were randomly assigned to 2 groups. In the first group, ESWT was used with energy flux density 0.15 mJ/mm2; 1500 pulses, frequency 4 Hz, patients received 1 treatment weekly for 4 weeks); painkillers and exercise were also employed. The second group received a sham and standard therapy as the first group.
As in the above report, our study used ESWT with an energy flux density of 0.15 mJ/mm2 (1000 pulses), frequency 4 Hz, and patients received a total of 10 treatments over a period of 5 weeks (twice a week). Taheri et al evaluated the therapy by measuring patients’ pain using the VAS scale and assessing disability with the ODI scale. Control measurements were taken before treatment, 1 month, and 3 months later. Our study used the same length of follow-up (1 and 3 months). However, the Iranian study showed that the VAS and ODI parameters improved significantly in both groups. Researchers indicated that their shock wave therapy effectively treated LBP, combined with drug treatment and exercise. Still, interestingly, the beneficial outcomes did not apply to ODI, as in our project. It seems that usage of oral pharmacotherapy was the weakness of the present work. Notably, it was difficult to estimate to what extent pain reduction is due to the physical method or resulted from the biochemical action of the drug and analgesia. This observation certainly diminishes the credibility of our findings. Our participants used only physiotherapeutic methods.
In turn, Moon et al [8] compared the single application of ESWT and sham surgery in patients with LBP without complete treatment, as was the case in the present study. The ESWT group received 2000 pulses during the procedure with the maximum energy level tolerated by the patient (energy flux density=0.09–0.25 mJ/mm2), and the probe was positioned perpendicular to the posterior lumbar line and moved up and down along the connecting line. Therapeutic progress was assessed 1 and 4 weeks after surgery using the 10-cm numerical rating scale (NRS) and the ODI. At the end of the study, pain reduction and functional improvement were found, and there was a conclusion that ESWT may be suitable for therapy in reducing LBP. In addition, the study received 7/10 points on the PEDro scale, although the obtained results are challenging to apply to a complete treatment program.
Schneider’s [9] study, with a PEDro of 6/10 points showed that manual myofascial (MT) therapy in combination with ESWT increased the physiotherapeutic efficacy in the management of chronic LBP. The studies of 2 groups compared the MT treatments combined with ESWT (1st group) with the MT treatment condition (2nd group). The therapy was carried out twice a week for 3 weeks, and there was no follow-up. Nevertheless, the short-term results were promising. Similar conclusions were reported by Notarnicola et al [10] and Han et al [11], whose short-term observations showed favorable analgesic effects and improvements in aspects of quality of life. However, these studies had low methodological PEDro levels (3/10 points).
In summary, focused ESWT can be effective in the analgesic effect in patients with LBP. Furthermore, the method can contribute to remission and lasting analgesia. However, despite some positive evidence, it is premature to reach a conclusion regarding the effectiveness of the focused technique in improving the functional state of patients. In this respect, our findings are not as promising and seem to be less convincing than outcomes from a less technologically advanced radial wave technique. However, this finding would require a single comparative analysis in joint clinical development for both methods.
Study Limitations
Future research should use other objective measurement methods (eg, stabilometric platform, surface electromyography) and include more participants over a longer period. Also, it is important to establish uniform treatment parameters that can be verified by other researchers. In subsequent studies, the questionnaire assessment of disability should be extended.
Conclusions
Focused ESWT in conjunction with an exercise program can be effective in patients with chronic LBP, both short- and long-term. In addition, focused ESWT allows reducing pain, although it does not seem to improve a patient’s functional state significantly. Thus, ESWT cannot be a key enrichment method for a standard rehabilitation program at this stage. Therefore, further clinical trials should be conducted, especially regarding patient functional evaluation after applying focused ESWT.
Acknowledgments
There were no other contributors than the authors listed, and we received no assistance in writing our paper.
Footnotes
Conflict of interest: None declared
Department and Institution Where Work Was Done
Clinical Research Laboratory of the Institute of Health Sciences of the University of Opole, Opole, Poland.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: This research was funded by the University of Opole in Poland and the Academy of Physical Education in Katowice subventions according to the number of FIZ/3/2022. Also, the study was supported by the Ministry of Health subventions according to the number of SUBZ.E060.22.099 from the IT Simple system of the Wrocław Medical University in Poland
References
- 1.Korakakis V, Whiteley R, Tzavara A, Malliaropoulos N. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: A systematic review including quantification of patient-rated pain reduction. Br J Sports Med. 2018;52:387–407. doi: 10.1136/bjsports-2016-097347. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Q, Fu C, Huang L, et al. Efficacy of extracorporeal shockwave therapy on pain and function in myofascial pain syndrome of the trapezius: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2020;101:1437–46. doi: 10.1016/j.apmr.2020.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Ma H, Zhang W, Shi J, et al. The efficacy and safety of extracorporeal shockwave therapy in knee osteoarthritis: A systematic review and meta-analysis. Int J Surg Lond Engl. 2020;75:24–34. doi: 10.1016/j.ijsu.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 4.Tengku Yusof TNB, Seow D, Vig KS. The musculoskeletal applications of extracorporeal shockwave therapy for foot and ankle disorders: A systematic review and meta-analysis. J Am Podiatr Med Assoc. 2021:18–191. doi: 10.7547/18-191. [DOI] [PubMed] [Google Scholar]
- 5.Surace SJ, Deitch J, Johnston RV, Buchbinder R. Shock wave therapy for rotator cuff disease with or without calcification. Cochrane Database Syst Rev. 2020;3:CD008962. doi: 10.1002/14651858.CD008962.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taheri P, Khosrawi S, Ramezani M. Extracorporeal shock wave therapy combined with oral medication and exercise for chronic low back pain: A randomized controlled trial. Arch Phys Med Rehabil. 2021;102:1294–99. doi: 10.1016/j.apmr.2020.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Walewicz K, Taradaj J, Rajfur K, et al. The effectiveness of radial extracorporeal shock wave therapy in patients with chronic low back pain: A prospective, randomized, single-blinded pilot study. Clin Interv Aging. 2019;14:1859–69. doi: 10.2147/CIA.S224001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moon YE, Seok H, Kim SH, et al. Extracorporeal shock wave therapy for sacroiliac joint pain: A prospective, randomized, sham-controlled short-term trial. J Back Musculoskelet Rehabil. 2017;30:779–84. doi: 10.3233/BMR-150405. [DOI] [PubMed] [Google Scholar]
- 9.Schneider R. Effectiveness of myofascial trigger point therapy in chronic back pain patients is considerably increased when combined with a new, integrated, low-frequency shock wave vibrotherapy (Cellconnect Impulse): A two-armed, measurement repeated, randomized, controlled pragmatic trial. J Back Musculoskelet Rehabil. 2018;31:57–64. doi: 10.3233/BMR-169662. [DOI] [PubMed] [Google Scholar]
- 10.Notarnicola A, Maccagnano G, Gallone MF, et al. Extracorporeal shockwave therapy versus exercise program in patients with low back pain: Short-term results of a randomised controlled trial. J Biol Regul Homeost Agents. 2018;32:385–89. [PubMed] [Google Scholar]
- 11.Han H, Lee D, Lee S, et al. The effects of extracorporeal shock wave therapy on pain, disability, and depression of chronic low back pain patients. J Phys Ther Sci. 2015;27:397–99. doi: 10.1589/jpts.27.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foldager CB, Kearney C, Spector M. Clinical application of extracorporeal shock wave therapy in orthopedics: Focused versus unfocused shock waves. Ultrasound Med Biol. 2012;38:1673–80. doi: 10.1016/j.ultrasmedbio.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 13.van der Worp H, van den Akker-Scheek I, van Schie H, Zwerver J. ESWT for tendinopathy: Technology and clinical implications. Knee Surg Sports Traumatol Arthrosc. 2013;21:1451–58. doi: 10.1007/s00167-012-2009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Opara J, Taradaj J, Walewicz K, et al. The current state of knowledge on the clinical and methodological aspects of extracorporeal shock waves therapy in the management of post-stroke spasticity-overview of 20 years of experiences. J Clin Med. 2021;10:E261. doi: 10.3390/jcm10020261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walewicz K, Taradaj J, Dobrzyński M, et al. Effect of radial extracorporeal shock wave therapy on pain intensity, functional efficiency, and postural control parameters in patients with chronic low back pain: A randomized clinical trial. J Clin Med. 2020;9:568. doi: 10.3390/jcm9020568. [DOI] [PMC free article] [PubMed] [Google Scholar]


