ABSTRACT
The translation of scientific evidence into guidelines and advice is a fundamental aspect of scientific communication within nutrition and dietetics. For communication to be effective for all patients, health literacy (HL) must be considered, i.e. an individual’s capacity to obtain, comprehend and utilise information to empower decision-making and promote their own health. HL levels are varied and difficult to judge on an individual basis and have not been quantified, thus not giving a population mean HL competency indication. It has been evidenced that most of the working age population in England cannot comprehend healthcare materials due to complexity, thereby promoting a need for agreed readability thresholds for written healthcare information. A wide range of modalities within dietetics are used to communicate to a varied audience with the primary form written, e.g. journal articles, plain language summaries and leaflets. Audio/visual and digital communications are increasing in dietetic care and welcomed by patients; however, the effectiveness of such approaches has not been studied thoroughly and digital exclusion remains a concern. Communication considering a patient’s HL level leads to empowerment which is key to effective management of chronic diseases with a high treatment burden. Therefore; this review will focus on the importance of modalities used to communicate science in nutrition to ensure they are appropriate in relation to Health Literacy.
Keywords: cystic fibrosis (CF), effective communication, health literacy, readability, scientific communication
INTRODUCTION
Scientific communication (SC) is defined as scientific information transmission to a specialised/non-specialist audience by methods such as verbal explanation, writing, lectures and digital means [1]. Effective SC is important when securing research funding, in media communication and informing policy. Within healthcare, SC is vital, especially as the final stakeholders for health-related research are patients, thereby directly impacting their health [2].
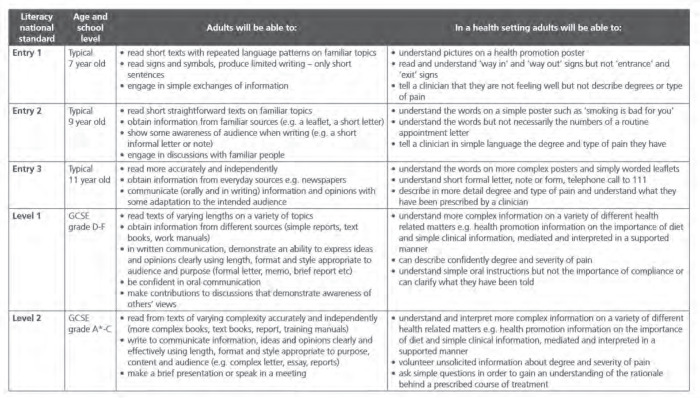
It is recognised that low patient literacy has been linked to poorer health outcomes, affecting how clinicians deliver healthcare [3]. Literacy is the extent of ability to read, write and have the skills to recognise words and understand text [4]. Health literacy (HL) extends this definition, further including comprehension of scientific knowledge, and having accessibility and skills to make appropriate health-related decisions [5]. In effective communication, information is given by methods appropriate to the patient’s HL level. DeWalt and colleagues noted that clinicians are generally poor judges of patient HL levels and so developed a HL universal precautions (HLUP) toolkit to help deliver healthcare information at a low HL level in a General Practice [6]. It has been shown that as many as four in 10 adults in the UK struggle to understand and use typical medical information designed for the public [7], where such low HL has been linked to a range of problems, including poor general health, inappropriate use of health services and reduced life expectancy [7]. The majority of adults in England are in the 11-14 year old reading age group [8] and Table 1 shows the levels of literacy related to age and understanding in a health setting [8].
Table 1.
Levels of literacy related to age and understanding in a health setting [Taken from “Health Literacy “How to” Guide: NHS Health Education England (Available at https://library.nhs.uk/wp-content/uploads/sites/4/2020/08/Health-literacy-how-to-guide.pdf)]
Dietitians must not only understand the scientific mechanisms behind nutrition and grasp the research methods needed to critically appraise the evidence, but they must also communicate appropriate information clearly at patients’ understanding levels. Thus, dietetics has been described as both an art and a science [9]. Dietitians artfully communicate scientific findings through varied modalities at a populationally understandable level to promote health, prevent disease and manage conditions. Therefore, the aim of this article is to discuss communication approaches and modalities which influence HL both within healthcare and specifically dietetics, in order to improve and promote HL in patients.
Health Literacy
The concept of HL, originally only alluded to functional literacy, i.e. the ability to read, understand and follow health information and advice, has evolved extensively [11] (Table 2). HL is a dynamic concept, as over a patient’s lifetime their HL capacity can change, with degree of cognitive and physical health altering with age or disease stage [23].
Table 2.
The evolving concept of health literacy: a selection of health literacy definitions in chronological order
| Source and Year [Reference] | Definition |
|---|---|
| Nutbeam (1998) [11] | “The cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health.” |
| American Medical Association (AMA) (1999) [12] | “The constellation of skills, including the ability to perform basic reading and numeral tasks required to function in the healthcare environment.” |
| Nutbeam (2000) [13] | “The personal, cognitive and social skills which determine the ability of individuals to gain access to, understand, and use information to promote and maintain good health.” |
| Institute of Medicine (2004) [14] | “The individuals’ capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.” |
| Zarcadoolas et al. (2005) [15] | “The wide range of skills, and competencies that people develop to seek out, comprehend, evaluate and use health information and concepts to make informed choices, reduce health risks and increase quality of life.” |
| Stocks et al. (2009) [16] | “The ability to understand and interpret the meaning of health information in written, spoken or digital form and how this motivates people to embrace or disregard actions relating to health.” |
| Freedman et al. (2009) [17] | “The degree to which individuals and groups can obtain, process, understand, evaluate, and act upon information needed to make public health decisions that benefit the community.” |
| Healthy People (2010) [18] | “The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” |
| Sørensen et al. (2012) [19] | “Health literacy is linked to literacy and entails people’s knowledge, motivation and competencies to access, understand, appraise and apply information to make judgements and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain and improve quality of life during the life course.” |
| Dodson et al. (2015) [20] | “The personal characteristics and social resources needed for individuals and communities to access, understand, appraise and use information and services to make decisions about health. Health literacy includes the capacity to communicate, assert and enact these decisions.” |
As a result of the association between low HL and poorer health outcomes [4], much research explores the possible link between poor chronic disease management and low HL. An adequate level of HL is needed to empower individuals to take charge of their own health or care for another, especially when they are critically involved in disease management e.g. diabetes [24].
A range of interventions to improve health knowledge in people with lower HL levels has been systematically reviewed by Pignone and colleagues [25], however, consistent differences in health knowledge pre and post intervention were not found. Intra-intervention differences were too various to draw firm conclusions and the studies reviewed often did not compare high and low literacy groups. Although HL can be measured using tools such as Rapid Estimate of Adult Literacy in Medicine, health outcome indications are limited to survey results with few longitudinal studies, thereby providing a limited evidence-base of prolonged health outcomes [25].
Although populational HL level in the UK has not been gauged, a key HL observational study investigated the relationship between health materials and literacy abilities of the English working-age-population (16-65 years). Several healthcare professionals (HCPs), including dietitians, judged representativeness of a national health booklets sample and a threshold comprehension level was found to be level 2 (5 GCSE’s A* to C), representing 73% of health brochures. When compared to populational literacy data from a survey sample of 7230 people [26], 40% of participants were below the comprehension threshold [27]. Literacy competency multivariate analyses demonstrated that sex (Adjusted Odds Ratio (AOR) = 1.25), age (1.44), ethinicity (1.43), English as first language 2.03), qualification level (2.38), job grade (1.40 – 1.88), income (1.41) and home ownership (1.32) were statistically significant, whereas nativity (i.e. born/not born in UK) (AOR=1.07) and employment (i.e. employed/not employed) (AOR=1.05) were not significant [27]. It must be noted that these results were produced from a small sample, not accounting for verbal communication or individual’s material interaction. The population data is somewhat dated and limited, neglecting non-working-age HL levels and did not include all HL aspects, like accessibility and comprehension. Nevertheless, the results underline a need for health literature to target lower HL levels.
Plain Language Summaries (PLSs)
A prevalent communication mode is written text, including journal articles, Plain Language Summaries (PLS), health information leaflets and Patient Information Leaflets, relating to pharmaceutical medicines. Journal articles communicate scientific research findings to similarly skilled professionals; the language is complex and discipline-specific preventing general public understanding. Therefore, PLSs of scientific findings are devised and are in widespread use, increasing science accessibility to those with lower HL. Although they have been criticised for formatting and length inconsistency, [28] they are nevertheless useful to communicate research findings. One example of innovation has been when a scientific or medical journal takes a positive action to also include a Lay or Plain Language Summary. One example of such practice is the Publication, Cystic Fibrosis Research News, which is a relative rarity in respiratory peer-review publishing, as it mirrors the papers published in its sister journal, the Journal of Cystic Fibrosis (JCF). CF Research News aims to foster enhanced knowledge by patients, their families and other members of the lay community about research advances published in JCF and to provide an opportunity for authors to write summaries of their Original Articles and Short Communications published in JCF.
Cochrane Reviews, provide vital, rigorous and reputable evidence, however authors lack consistent adherence to the ‘Plain Language Expectations for Authors of Cochrane Summaries’ [29]. Points of author criticism are the continued technical jargon presence and only 23% of PLSs analysed being within the word count [30]. Locating PLSs online has also been highly criticised [31], highlighting the need for inter-discipline standardised practice.
The gold standard for assessing healthcare information readability is the Simple Measure of Gobbledegook [32] (Table 3). Various people such as original scientific authors, freelance writers and lay-people may be involved in writing a PLS. In most medical PLSs, the author writes corresponding PLS, helping thought continuity [31]. White and colleagues piloted a second year undergraduate PLS writing course, with adherence criteria including a Flesh-Kincaid readability score of between grades 8 – 10 (age 13-16 years). Students described it as “tedious”, having difficulty in preserving integral research meaning whilst keeping reading level low [36]. Furthermore, Brownell and colleagues confirmed the need for university training to build SC into the curriculum, with multiple opportunities for practice, feedback and revision [37].
Table 3.
A selection of the various metrics used to assess readability of written text
| Readability Index Name | Summary | Score Example | Age equivalent | Formula |
|---|---|---|---|---|
| Simple Measure of Gobbledygook (SMOG) | Estimates comprehension in terms of years of education needed. The first, middle and last 10 sentences should be sampled to calculate SMOG. It involves counting words with 3+ syllables. [32] | SMOG US grade 8 score | 13-14 years | 3 + square root √ [number of polysyllabic words x (30 ÷ number of sentences)] |
| The Gunning Fog Index (GFI) | Similar to SMOG except it estimates first time readability comprehension in terms of years of education needed. The scale is from 6-17. [33] | GFI US grade 7-8 score | 13-14 years | 0.4 x [(words ÷ sentences) + 100 x (complex words ÷ total words)] |
| Flesch-Kincaid Grade Score (FKG) | Usually used in education and assesses readability whilst weighting heavily on syllable count. [34] | FKG US grade 8 score | 13-14 years | 0.39 (total words/total sentences) + 11.8 (total syllables/total words) – 15.59 |
| Flesch Reading Ease Score (FRES) | English text on a scale of 100, with a higher number indicating easier comprehension. [35] | FRES score of 60-70 | 13 years | [206.835 – (1.015 x (total words ÷ total sentences)) – (84.6 x (total syllables ÷ total words))] |
Visual Aids (VA)
VA found on posters, brochures, websites and social media can promote health messages and include pictures, infographics, figures, charts and pictographs. Results from a randomised study found that when presenting risk probability (e.g. 2/100), graphically for low literacy groups, pictographs were more effective for denominators <100-1000 and bar charts for >1000 [38]. Pictographs with text have been found to reduce error of drug dosage administration to children among parents with low HL [39]. Pictures improve information recall, grab attention and promote health information understanding; especially simpler cartoon pictures complementing text [41]. To maximise effectiveness, they should be accompanied by captions to prevent erroneous interpretation and illustrate written communication; not distracting from the information.
Audio Visual (AV) techniques
Although little evidence has shown learning outcome differences based on a target learning styles teaching approach [41]; preferences may influence information delivery choice, whether visual, kinaesthetic or auditory. AV communication synthesises such preferences together forming videos. The effectiveness of healthcare AV communication has not been widely studied, although certain patient groups have indicated a desire for video-based education [42]. One area that has used AV Digital Communication (DC) to promote health is for handwashing in infection control (IC). Particularly, Stanford University published a wordless AV graphic animation illustrating SARS-CoV-2 spread and preventative measures, which will form part of a randomised trial comparing differences in behavioural intent after watching it, compared to placebo and control [43]. Benefits of AV communication include its deliverability without physical contact and it can be re-watched and potentially inform without language barriers.
Digital Communication (DC)
There has been accelerated DC use to promote health messages with increasing telehealth replacing clinics. Previously HCPs have resisted engagement with some DC forms, e.g. social media, due to medicolegal and ethical issues [44]. Valdez and colleagues have cautioned rapid DC acceptance by stating that the existent digital exclusion divide among many groups, but especially those with certain disabilities could exacerbate health access inequalities [45]. Common digital inclusion barriers found in a rapid review included; physical access, usage skills and fearful attitudes [46]. DC has significant reachability; however, barriers must be considered for long-term patient care, and HCP burden.
A specific DC ethical concern of the adolescent patient-clinician relationship is maintaining professionalism. Patients with chronic diseases felt that increased communication with HCPs produced a trusting relationship and better health knowledge, however, clinicians thought it blurred lines between consent and duty of care limits which were being stretched to out-of-office hours [47]. More guidance and clarity are necessary for HCPs effective navigation of digital health communication.
The importance of Health Literacy and Communication in Nutrition and Dietetics
The communication method and HL knowledge underpins effective nutrition and dietetic communication. One estimation of patient HL in primary care is the newest vital sign (NVS) measure, in which a clinician asks six comprehension questions from an ice-cream label, with the number of correct answers indicating likelihood of HL level [48]. In a study by Caldwell (2020) NVS scores indicated that adolescents’ HL increased with age, suggesting HL intra-age-group variation [49]. Age and comprehension level will affect a dietitian’s communication approach clinically and in devising written materials, with the target audience informing communication style, information and complexity.
The varied audience with which dietitians must effectively communicate outside a patient counselling role; (carers, families and HCPs within the multidisciplinary team (MDT)) promoted a pilot workplace-based communication programme for Australian dietitians. It was rated very beneficial for those practicing <5 years, indicating significantly higher benefit than those working >5 years, highlighting that reflective learning experiences improve communication [50]. Recent focus has been on the HL knowledge of students training as HCPs because of the potential teaching impact on shaping future clinician’s communication skills. Results have been unequivocal, finding lower than desired HL and a need for student training in HL communication [51-53].
‘Good communication skills’ is also a theme associated with Dietetic patient centred care (PCC) [54]. Based on 27 reviewed studies, communication skills valued by patient and dietitian included verbal and non-verbal, such as active listening, rewording and asking questions. All modes focused on patients’ value and promoted understanding and patient-enablement contributing to the overall “collaborative partnership” as a HL output. This aforementioned review focused only on patient-clinician relationships, neglecting other modes of dietetic communication, such as active enteral feeding demonstrations, DC or written materials.
CONCLUSION
In conclusion; without acknowledgement of the individual’s HL level, abilities and access, dietetic communication will be sub-optimal. Verbal and active communications in patient-clinician relationships are important. Written SC is currently largely aimed at too high a reading and HL level, indicating the need for a standardised readability testing approach to evaluate healthcare material suitability. The addition of VA is helpful in communication for people with low HL and although there are gaps in the research regarding effectiveness of DC and target patient populations, prevalence is likely to increase. All communication approaches must be used selectively in PCC, in order to negotiate treatment plans, educate verbally, create resources to improve condition manageability and ultimately patient healthcare empowerment.
ACKNOWLEDGEMENTS
This project was a product of the Cystic Fibrosis Study Buddies Programme designed to enable improved health literacy and essential skills for life and employability in young CF adults. Author Hannah L. Anderson was a CF Study Buddy, supporting young people with cystic fibrosis. This project was supported by a Charitable Grant from Vertex Pharmaceuticals Inc., USA. (CG-2017-106614). Vertex Pharmaceuticals did not play any role in project conceptualisation, design, execution, analysis, nor any editorial role in manuscript writing or approval.
Footnotes
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Jucan MS, Jucan CN. The power of science communication. Procedia Soc Behav Sci. 2014;149:461–6. doi: 10.1016/j.sbspro.2014.08.288. [DOI] [Google Scholar]
- 2.Orritt R, Powell P. Getting the word out: how to talk to the public about your research. Breathe (Sheff) 2020;16(2):1–7. doi: 10.1183/20734735.0008-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Storr T, Maher J, Swanepoel E. Online nutrition information for pregnant women: a content analysis. Matern Child Nutr. 2017;13(2):e12315. doi: 10.1111/mcn.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nutbeam D. Defining and measuring health literacy: what can we learn from literacy studies? Int J Public Health. 2009;54(5):303–5. doi: 10.1007/s00038-009-0050-x. [DOI] [PubMed] [Google Scholar]
- 5.Neter E, Brainin E. Association between health literacy, ehealth literacy, and health outcomes among patients with long-term conditions. [Internet] Eur Psychol. 2019;24(1):68–81. [Google Scholar]
- 6.DeWalt DA, Broucksou KA, Hawk V, Brach C, Hink A et al. Developing and testing the health literacy universal precautions toolkit. Nurs Outlook. 2011;59(2):85–94. doi: 10.1016/j.outlook.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NHS Digital Service Manual. [Internet] Content Style Guide: Health literacy. [cited 2021 Dec 7]. Available from: https://service-manual.nhs.uk/content/health-literacy .
- 8.NHS Health Education England. [Internet] Health literacy “how to“ guide. [cited 2021 Dec 7]. Available from: https://library.nhs.uk/wp-content/uploads/sites/4/2020/08/Health-literacy-how-to-guide.pdf .
- 9.Mantzioris E. The science and art of dietetics: why science needs to underpin our practice. Nutr Diet. 2018;75(3):247–9. doi: 10.1111/1747-0080.12445. [DOI] [PubMed] [Google Scholar]
- 10.Frisch AL, Camerini L, Diviani N, Schulz PJ. Defining and measuring health literacy: how can we profit from other literacy domains? Health Promot Int. 2012;27(1):117–26. doi: 10.1093/heapro/dar043. [DOI] [PubMed] [Google Scholar]
- 11.Nutbeam D, Kickbusch I. Health promotion glossary. Health Promot Int. 1998;13(4):349–64. [Google Scholar]
- 12.Health literacy: report of the council on scientific affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs American Medical Association. JAMA. 1999;281(6):552–7. [PubMed] [Google Scholar]
- 13.Nutbeam D. Health literacy as a public goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259–67. [Google Scholar]
- 14.Institute of Medicine (US) Committee on Health Literacy. Health literacy: a prescription to end confusion. Washington (DC): National Academies Press; 2004. [PubMed] [Google Scholar]
- 15.Zarcadoolas C, Pleasant A, Greer DS. Understanding health literacy: an expanded model. Health Promot Int. 2005;20(2):195–203. doi: 10.1093/heapro/dah609. [DOI] [PubMed] [Google Scholar]
- 16.Adams RJ, Stocks NP, Wilson DH, Hill CL, Gravier S, Kickbusch L, et al. Health literacy - a new concept for general practice? Aust Fam Physician. 2009;38(3):144–6. [PubMed] [Google Scholar]
- 17.Freedman DA, Bess KD, Tucker HA, Boyd DL, Tuchman AM, Wallston KA. Public health literacy defined. Am J Prev Med. 2009;36(5):446–51. doi: 10.1016/j.amepre.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services. Healthy People 2010 Understanding and improving health. 2nd ed. Washington, [DC]: Department of Health and Human Services, National Networks of Libraries of Medicine; 2010. [Google Scholar]
- 19.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dodson S, Good S, Osborne R. New Delhi: World Health Organization; 2015. [cited 2020 Dec 5]. [Internet]. Health literacy toolkit for low and of middle-income countries: a series of information sheets to empower communities and strengthen health systems. Available from: https://apps.who.int/iris/bitstream/handle/10665/205244/B5148.pdf?sequence=1&isAllowed=y . [Google Scholar]
- 21.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. 2010;15(Suppl 2):9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 22.Okan O, Bauer U, Levin-Zamir D, Pinheiro P, Sørensen K. International handbook of health literacy: research, practice and policy across the lifespan. Bristol: Policy Press; 2019. [cited 2020 Dec 5]. Available from: https://library.oapen.org/handle/20.500.12657/24879 . [Google Scholar]
- 23.Parnell TA, Stichler JF, Barton AJ, Loan LA, Boyle DK, Allen PE. A concept analysis of health literacy. Nurs Forum. 2019;54(3):315–27. doi: 10.1111/nuf.12331. [DOI] [PubMed] [Google Scholar]
- 24.Bailey SC, Brega AG, Crutchfield TM, Elasy T, Herr H, Kaphingst K, Karter AJ, et al. Update on health literacy and diabetes. Diabetes Educ. 2014;40(5):581–604. doi: 10.1177/0145721714540220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pignone M, DeWalt DA, Sheridan S, Berkman N, Lohr KN. Interventions to improve health outcomes for patients with low literacy: a systematic review. J Gen Intern Med. 2005;20(2):185–92. doi: 10.1111/j.1525-1497.2005.40208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Department for Business Innovation and Skills. London: Business Innovation & Skills; 2012. [cited 2020 Dec 5]. The 2011 skills for life survey: a survey of literacy, numeracy and ICT levels in England. BIS Research Paper Number 81. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/36000/12-p168-2011-skills-for-life-survey.pdf. [Google Scholar]
- 27.Rowlands G, Protheroe J, Winkley J, Richardson M, Seed PT, Rudd R. A mismatch between population health literacy and the complexity of health information: an observational study. Br J Gen Pract. 2015;65(635):e379–e386. doi: 10.3399/bjgp15X685285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shailes S. Plain language summaries of research, something for everyone. [Internet] ELife. 2017;6:e25411. doi: 10.7554/eLife.25411. Available from: https://elifesciences.org/articles/25411 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chanler J, Churchill R, Higgins J, Lasserson T, Tovey D. London: The Cochrane Collaboration; 2013. Methodological expectations of cochrane intervention reviews (MECIR). Methodological standards for the conduct of new Cochrane Intervention Reviews. version 2013;2. Available from: https://consumers.cochrane.org/sites/consumers.cochrane.org/files/public/uploads/pleacs_2019.pdf. [Google Scholar]
- 30.Kadic AJ, Fidahic M, Vujcic M, Saric F, Propadalo I, Marelja I, et al. Cochrane plain language summaries are highly heterogeneous with low adherence to the standards. BMC Med Res Methodol. 2016;16(61) doi: 10.1186/s12874-016-0162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.FitzGibbon H, King K, Piano C, Wilk C, Gaskarth M. Where are biomedical research plain-language summaries? Health Sci Rep. 2020;3(3):e175. doi: 10.1002/hsr2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fitzsimmons PR, Michael BD, Hulley JL, Scott GO. A readability assessment of online Parkinson’s disease information. J R Coll Physicians Edinb. 2010;40(4):292–6. doi: 10.4997/JRCPE.2010.401. [DOI] [PubMed] [Google Scholar]
- 33.Keogh CJ, McHugh SM, Moloney M, Hannigan A, Healy DA, Burke PE, et al. Assessing the quality of online information for patients with carotid disease. Int J Surg. 2014;12(3):205–8. doi: 10.1016/j.ijsu.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 34.Worrall AP, Connolly MJ, O’Neill A, O’Doherty M, Thornton KP, McNally C, et al. Readability of online COVID-19 health information: a comparison between four English speaking countries. BMC Public Health. 2020;20(1):1–12. doi: 10.1186/s12889-020-09710-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hansberry DR, Agarwal N, Baker SR. Health literacy and online educational resources: an opportunity to educate patients. AJR Am J Roentgenol. 2015;204(1):111–6. doi: 10.2214/AJR.14.13086. [DOI] [PubMed] [Google Scholar]
- 36.White WB, Nelson CR, Henderson FC. Developing lay summaries as a bidirectional learning opportunity for authors and undergraduate scholars: the Jackson heart study. Pedagogy Health Promot. 2019;6(2):137–41. [Google Scholar]
- 37.Brownell SE, Price JV, Steinman L. Science communication to the general public: why we need to teach undergraduate and graduate students this skill as part of their formal scientific training. J Undergrad Neurosci Educ. 2013;12(1):e6–e10. PMID: 24319399. [PMC free article] [PubMed] [Google Scholar]
- 38.McCaffery KJ, Dixon A, Hayen A, Jansen J, Smith S, Simpson JM. The influence of Graphic Display Format on the interpretations of quantitative risk information among adults with lower education and literacy: a randomized experimental study. Med Decis Making. 2011;10;32(4):532–44. doi: 10.1177/0272989X11424926. [DOI] [PubMed] [Google Scholar]
- 39.Yin HS, Mendelsohn AL, Fierman A, van Schaick L, Bazan IS, Dreyer BP. Use of a pictographic diagram to decrease parent dosing errors with infant acetaminophen: a health literacy perspective. Acad Pediatr. 2011;11(1):50–7. doi: 10.1016/j.acap.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 40.Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61(2):173–90. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 41.Kirschner PA. Stop propagating the learning styles myth. Comput Educ. 2017;106:166–71. [Google Scholar]
- 42.Cooley L, Hudson J, Potter E, Raymond KF, George C, Georgiopoulos AM. Clinical communication preferences in Cystic Fibrosis and strategies to optimize care. Pediatr Pulmonol. 2020;55(4):948–58. doi: 10.1002/ppul.24655. [DOI] [PubMed] [Google Scholar]
- 43.Vandormael A, Adam M, Greuel M, Bärnighausen T. A short, animated video to improve good COVID-19 hygiene practices: a structured summary of a study protocol for a randomized controlled trial. Trials. 2020;21(1):469. doi: 10.1186/s13063-020-04449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.George DR, Rovniak LS, Kraschnewski JL. Dangers and opportunities for social media in medicine. Clin Obstet Gynecol. 2013;56(3):453–62. doi: 10.1097/GRF.0b013e318297dc38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Valdez RS, Rogers CC, Claypool H, Trieshmann L, Frye O, Wellbeloved-Stone C, et al. Ensuring full participation of people with disabilities in an era of telehealth. J Am Med Inform Assoc. 2020;28(2):389–92. doi: 10.1093/jamia/ocaa297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Borg K, Boulet M, Smith L, Bragge P. Digital inclusion and health communication: a rapid review of literature in nutrition to promote and improve health literacy. Health Commun. 2019;34(11):1320–28. doi: 10.1080/10410236.2018.1485077. [DOI] [PubMed] [Google Scholar]
- 47.Ignatowicz A, Slowther AM, Elder P, Bryce C, Hamilton K, Huxley C, et al. Ethical implications of digital communication for the patient-clinician relationship: analysis of interviews with clinicians and young adults with long term conditions (the LYNC study) BMC Med Ethics. 2018;19(1):11. doi: 10.1186/s12910-018-0250-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shealy KM, Threatt TB. Utilization of the newest vital sign (NVS) in practice in the United States. J Health Commun. 2015;31(6):679–87. doi: 10.1080/10410236.2014.990079. [DOI] [PubMed] [Google Scholar]
- 49.Caldwell EP. Health literacy in adolescents with sickle cell disease: the influence of caregiver health literacy. J Spec Pediatr Nurs. 2019;25(2):e12284. doi: 10.1111/jspn.12284. [DOI] [PubMed] [Google Scholar]
- 50.Notaras S, Mak M, Wilson N. Advancing practice in dietitians’ communication and nutrition counselling skills: a workplace education program. J Hum Nutr Diet. 2018;31(6):725–33. doi: 10.1111/jhn.12569. [DOI] [PubMed] [Google Scholar]
- 51.Mullan J, Burns P, Weston K, McLennan P, Rich W, Crowther S, et al. Health literacy amongst health professional university students: a study using the health literacy questionnaire. Educ Sci. 2017;7(2):54–65. [Google Scholar]
- 52.Rueda-Medina B, Gómez-Urquiza JL, Tapia-Haro R, Casas-Barragán A, Aguilar-Ferrándiz ME, Correa-Rodríguez M. Assessing health science students’ health literacy and its association with health behaviours. Health Soc Care Community. 2020;28(6):2134–9. doi: 10.1111/hsc.13024. [DOI] [PubMed] [Google Scholar]
- 53.Uysal N, Ceylan E, Koç A. Health literacy level and influencing factors in university students. Health Soc Care Community. 2019;28(2):505–11. doi: 10.1111/hsc.12883. [DOI] [PubMed] [Google Scholar]
- 54.Sladdin I, Ball L, Bull C, Chaboyer W. Patient-centred care to improve dietetic practice: an integrative review. J Hum Nutr Diet. 2017;30(4):453–70. doi: 10.1111/jhn.12444. [DOI] [PubMed] [Google Scholar]