Abstract
Introduction
Spine surgery is challenging in hemodialysis (HD)-dependent patients owing to their poor general condition. However, postoperative complications and the mortality and survival rates have not been specifically evaluated in a wide series. This study aimed to elucidate postoperative complications and the survival rate in cervical spine surgery in HD patients.
Methods
This study included 109 HD patients (70 men, 39 women) who had undergone cervical spine surgery between July 1996 and May 2018. Based on radiological diagnosis, we divided them into the destructive spondyloarthropathy (DSA) and non-DSA groups. We investigated the causes of hemodialysis, postoperative complications, postoperative inpatient mortality rate, and survival rate.
Results
The DSA and non-DSA groups included 100 surgeries in 89 patients and 21 surgeries in 20 patients, respectively. The mean age at surgery was 62.9 years for the DSA and 55.9 years for the non-DSA group (P=0.97). The DSA group had a shorter hemodialysis period at surgery compared with the non-DSA group (21.7 vs. 26.5 years, P<0.05). The two most common causes of HD in both groups were chronic glomerulonephritis (DSA, 45%; non-DSA, 57.1%) and diabetes (DSA, 11%; non-DSA, 14.5%). Postoperative complications were observed in 23% (23/100) and 19% (4/21) of surgeries in the DSA and non-DSA groups, respectively (P=0.782). The total in-hospital mortality rate was 2.5% (3/121). The 1-, 3-, 5-, and 10-year postoperative survival rates of all patients were 89.6%, 75.5%, 67.1%, and 44.7%, respectively. The survival rates did not depend on the group (DSA vs. non-DSA), pre- and postoperative Japanese Orthopedic Association score for cervical myelopathy, hemodialysis period, sex, and age (P>0.05). However, significantly low survival rates were observed in HD caused by diabetes compared with that by chronic glomerulonephritis (P<0.001) and other causes (P<0.001).
Conclusions
Cervical spine surgery in HD patients is associated with postoperative complications. The postoperative survival rate was found to be low if the cause of hemodialysis was diabetes.
Keywords: hemodialysis, cervical spine, destructive spondyloarthropathy, complication, survival rate, chronic glomerulonephritis, diabetes
Introduction
Since the first report on destructive spondyloarthropathy (DSA) by Kuntz et al., spine lesions have been well recognized in hemodialysis (HD) patients1). The cervical spine is the most common site for HD-related lesions. Cervical DSA may cause serious myelopathy and require surgical treatment2-5). Apart from DSA, long-term HD patients may also develop spinal canal stenosis due to amyloid deposition and calcification in the spinal canal with scarce X-ray changes3,6,7). In addition, several reports have described upper cervical lesions in long-term HD patients8-11). The upper cervical lesions include periodontoid pseudotumor and atlantoaxial or occipitoatlantal DSA8-11). Periodontoid pseudotumor causes myelopathy or radiculopathy, and DSA causes myelopathy or posterior neck pain. Odontoid process fracture with consequent severe instability in the upper cervical spine has also been reported in patients with atlantoaxial DSA. For the cervical spine lesions in long-term HD patients, conservative treatment is not effective, and surgical treatment is often required8-11). However, surgical treatment in long-term HD patients may cause serious postoperative complications, including death, given that the general conditions of these patients are usually poor12-15). Several reports have described the clinical surgical outcomes of HD patients with cervical spine lesions2-5,7). However, previous studies on the postoperative complications and survival rate in cervical spine surgeries were of limited power as they were based on very small case series. Therefore, in this study, we analyzed the postoperative complications and survival rate in cervical spine surgeries of more than 100 patients with long-term HD from a single institution.
Materials and Methods
This study included 121 surgeries in 109 HD patients who had undergone surgery for HD-related lesions of the cervical spine at our hospital between July 1996 and May 2018. Those who had undergone cervical spine surgery for other diseases, such as ossification of the posterior longitudinal ligament, spondylosis, and rheumatoid arthritis, were excluded from this study. All patients underwent cervical spine X-ray, magnetic resonance imaging (MRI), and computed tomography (CT) imaging preoperatively. Diagnosis of DSA was made via X-ray. The patients were categorized as the DSA group if the X-ray findings indicated that the vertebral endplates and intervertebral disc spaces were of Grades II and III based on the classification reported by Chin et al. (distinct bony erosion or radiolucent lesions in endplates and narrowed intervertebral disc space - grade II; absence of the intervertebral disc space - grade III)16). Instability of the cervical spine was defined as more than 3 mm of spondylolisthesis in the lateral flexion and extension X-ray. The upper cervical DSA indicated the existence of cysts or destruction at the occipitoatlantal or atlantoaxial joints or instability in these joints8,9). Patients with cervical spinal stenosis observed on MRI due to amyloid deposition without DSA changes on X-ray and CT were categorized as the non-DSA group. On the DSA group, we performed en bloc laminoplasty (LP) for the cases with lordotic alignment and without instability on X-ray17). Posterior spinal fusion with lateral mass or pedicle screws was performed in addition to LP for patients with instability. Local kyphosis that was not reduced on extension X-ray required anterior spinal fusion (ASF) with a plate, in addition to LP. For the upper cervical DSA, atlantoaxial fusion with transarticular screws and Brooks' procedure was performed if the DSA change was restricted to the atlantoaxial joints. Occipitocervical fusion was performed in patients with atlanto-occipital DSA. For the non-DSA group, LP was performed in patients with lordotic alignment on X-ray, whereas ASF was performed if the alignment was kyphotic.
The patients' characteristics, HD causes, surgeries performed, pre- and postoperative Japan Orthopedic Association (JOA) scores for cervical myelopathy, postoperative complications, postoperative mortality, and postoperative survival rate were noted. The modified (m) JOA score could be 14 as a maximum, because 3 points were deducted from the original maximum score of 17 due to difficulty in evaluating bladder function in HD patients. For patients who had undergone several surgeries, the postoperative complications were evaluated for each surgery. The survival rate was investigated using medical records of our institute and hospitals where the patients died. The survival rate of patients who underwent multiple surgeries was counted from the time of the first surgery.
Continuous data were expressed as mean±standard deviation for normally distributed data and as median (interquartile range) for non-normally distributed data. Between-group comparisons were performed using the t-test for normally distributed variables and the Mann-Whitney U test for non-normally distributed variables. Categorical data were expressed as number and percentage (%), and intergroup differences were analyzed using Fisher's exact probability test. P values less than or equal to 0.05 were considered statistically significant. These analyses were conducted in SPSS version 22.0 for Windows (IBM Japan, Tokyo, Japan). Log-rank tests for survival rate analysis were based on the Kaplan-Meier method using R version 3.5.2 (R Foundation for Statistical Computing, Vienna, Austria).
The study was approved by the review board of our institute (No. 5801). In this study, the medical records of patients who have undergone a specific procedure for clinical purposes were retrospectively reviewed. Therefore, this study is of no more than minimal risk to subjects; thus, the need for informed consent has been waived by the IRB.
Results
The DSA group included 100 surgeries in 89 patients, whereas the non-DSA group included 21 surgeries in 20 patients (Table 1). The male-to-female ratio was not significantly different between the groups (P=0.333; Table 1). The mean age at surgery was 62.9±7.5 years in DSA group and 59.9±6.8 years in the non-DSA group (P=0.097). The most common cause of HD in both groups was chronic glomerulonephritis (CGN), followed by diabetes mellitus (DM) (P=0.587, Table 1). The operative time was significantly longer in the DSA than in the non-DSA (P<0.05) group, whereas intraoperative blood loss was lower in the DSA than in the non-DSA (P<0.05) group. The mean preoperative and postoperative mJOA scores were not significantly different between the groups (P=0.448 and P=0.246, respectively). Likewise, the mean recovery score was not significantly different between the groups (P=0.557) (Table 2). The types of surgery performed in both groups are presented in Table 3.
Table 1.
Patients’ Characteristics.
| DSA group
(n=100) |
Non-DSA group
(n=21) |
P | |
|---|---|---|---|
| Sex (male:female) | 64:36 | 11:10 | 0.333a |
| Age (yr) | 62.9±7.5 | 59.9±6.8 | 0.097b |
| Dialysis period (yr) | 21.7±8.2 | 26.5±8.4 | 0.018*b |
| Cause of dialysis | 0.383a | ||
| Chronic glomerulonephritis | 45 (45%) | 21 (57.1%) | |
| Diabetes | 11 (11%) | 3 (14.3%) | |
| Toxemia of pregnancy | 4 (4%) | 2 (9.5%) | |
| Nephrotic syndrome | 4 (4%) | 2 (9.5%) | |
| Polycystic kidney disease | 4 (4%) | 0 | |
| Nephrosclerosis | 3 (3%) | 0 | |
| Others | 8 (8%) | 1 (4.8%) | |
| Unknown | 21 (21%) | 1 (4.8%) |
Data expression: n, %
P-value: a, Fisher’s exact test; b, unpaired t-test, *, statistically significant
Table 2.
Surgical Results.
| DSA group
(n=100) |
Non-DSA group
(n=21) |
P | |
|---|---|---|---|
| Operative time (min) | 196.8±86.0 | 155.7±56.4 | 0.039*b |
| Blood loss (mL) | 443.6±469.1 | 792.9±871.9 | 0.011*b |
| mJOA score | |||
| Preoperative | 4.4±2.9 | 3.9±2.0 | 0.448b |
| Postoperative | 8.9±3.3 | 8.0±3.0 | 0.246b |
| Recovery | 4.5±2.9 | 4.1±2.8 | 0.557b |
mJOA, modified Japanese Orthopaedic Association
Data expression: n, %
P-value: b, unpaired t-test, *, statistically significant
Table 3.
Types of Surgery Performed.
| Surgery | DSA
(n=100) |
Non-DSA
(n=21) |
P |
|---|---|---|---|
| 0.436a | |||
| Laminoplasty | 49 (49%) | 19 (90.5%) | |
| Laminoplasty+ASF | 12 (12%) | 0 | |
| Laminoplasty+posterior fusion (LM) | 10 (10%) | 0 | |
| Laminoplasty+posterior fusion (PS) | 10 (10%) | 0 | |
| ASF | 9 (9%) | 1 (4.8%) | |
| Occipito-cervical fusion | 3 (3%) | 0 | |
| MB+laminoplasty | 3 (3%) | 0 | |
| Others | 4 (4%) | 1 (4.8%) |
ASF, anterior spinal fusion, LM, lateral mass screw, PS, pedicle screw, MB, Magerl and Brooks procedure
Data expression: n, %
P-value: a, Fisher’s exact test
Postoperative complications were observed in 23% (23/100) of surgeries in the DSA group and 19% (4/21) in the non-DSA group (P=0.782) (Table 4). Three individuals in the DSA group and none from the non-DSA group died in the hospital. The in-hospital mortality rate was 2.5% (3/121) in all cases. The causes of death were aspiration pneumonia in one case and gastrointestinal perforation in two cases. No surgical site infection was observed. We also compared the surgical results between patients on HD for more than 21 years and those on HD for less than 20 years. No significant difference was observed in the postoperative complications between the two groups (Table 5).
Table 4.
Postoperative Complications.
| Complications | DSA
(n=100) |
Non-DSA
(n=21) |
P |
|---|---|---|---|
| Gastrointestinal dysfunction | 6 (6%) | 2 (9.5%) | 0.626 |
| Coronary artery disease | 2 (2%) | 1 (4.8%) | 0.439 |
| Pneumonia | 3 (3%) | 0 | >0.999 |
| Neurological deterioration | 2 (2%) | 1 (4.8%) | 0.439 |
| Hyperkalemia | 2 (2%) | 0 | >0.999 |
| Consciousness disorder | 2 (2%) | 0 | >0.999 |
| Others | 8 (8%) | 2 (9.5%) | 0.684 |
| Total | 23 (23%) | 4 (19%) | 0.782 |
| Inpatient mortality | 3 (3%) | 0 | >0.999 |
Data expression: n, %
P-value: Fisher’s exact test
Table 5.
Comparison of Surgical Results between Patients on Hemodialysis for More than 21 Years and Those on Hemodialysis for Less than 20 Years.
| HD<20years
(n=47) |
HD>21years
(n=74) |
P-value | |
|---|---|---|---|
| Sex (male:female) | 32:15 | 43:31 | 0.338a |
| Age (yr) | 65.8±7.6 | 60.2±6.5 | <0.001*b |
| Dialysis period (yr) | 13.8±4.8 | 28.1±4.5 | - |
| Operative time (min) | 185.2±90.6 | 191.9±77.9 | 0.672b |
| Blood loss (mL) | 382.8±384.3 | 587.4±660.6 | 0.063b |
| Complications | |||
| Gastrointestinal dysfunction | 5 (10.6%) | 3 (4.1%) | 0.259a |
| Coronary artery disease | 0 (0%) | 3 (4.1%) | 0.281a |
| Pneumonia | 0 (0%) | 3 (4.1%) | 0.281a |
| Neurological deterioration | 1 (2.1%) | 2 (2.7%) | >0.999a |
| Hyperkalemia | 2 (2%) | 0 | 0.149a |
| Consciousness disorder | 2 (2%) | 0 | 0.149a |
| Others | 3 (6.4%) | 7 (9.5%) | 0.739a |
| Total | 12 (25.5%) | 15 (20.3%) | 0.510a |
| Inpatient mortality | 1 (2.1%) | 2 (2.7%) | >0.999a |
Data expression: n, %
P-value: a, Fisher’s exact test; b, unpaired t-test, *, statistically significant
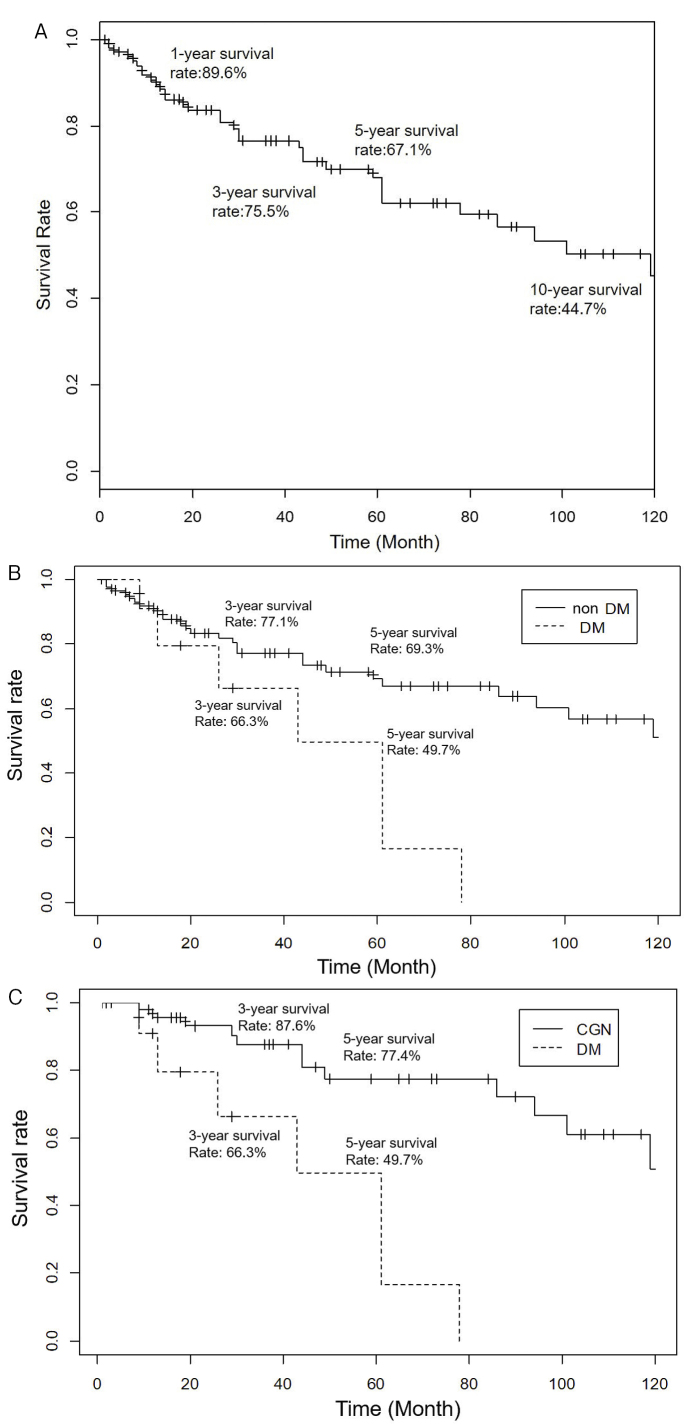
The postoperative survival rates of all patients were 89.6%, 75.5%, 67.1%, and 44.7% at 1, 3, 5, and 10 years (Fig. 1A). The survival rates did not depend on the group (DSA vs. non-DSA), preoperative HD duration (≥21 vs. <21 years), pre- and postoperative mJOA scores, age at surgery (≥65 vs. <65 years), and the time period at which the surgery was performed (early group: July 1997-May 2006 vs. late group: May 2006-August 2012). However, the survival rates significantly depended on the HD causes (DM vs. non-DM, P=0.008; DM vs. CGN, P=0.0001; Fig. 1B, C). Diabetes was associated with worse survival rate compared with other HD causes.
Figure 1.
Kaplan–Meier analysis of postoperative survival rates of all HD patients (A), patients with diabetes (DM) vs. non-DM (B), and chronic glomerulonephritis (CGN) vs. DM (C).
Discussion
In this study, we reported the postoperative complications and survival rate in cervical spine surgery among 121 surgeries in 109 HD patients. In our study, the most common cause of HD was CGN, followed by DM (CGN: 45% in the DSA group, 57.1% in the non-DSA group; DM: 11% in the DSA group, 14.3% in the non-DSA group). According to the annual dialysis report by the Japanese Society for Dialysis Therapy in 2017, the most common cause of HD at the end of 2017 was diabetic nephropathy (39.0%), followed by CGN (27.8%)18). This study demonstrated that HD was caused by DM in 20% and CGN in 50% of cases in 1996, the starting year of our study. The prevalence of DM continuously increased and eventually replaced CGN as the most common cause of HD in 201118). The percentage of DM has continuously increased since 2011, although the rate of increase has slowed down in recent years, whereas the percentage of CGN has steadily declined18). This study indicated that in the future, DM will likely become the main cause of HD in patients undergoing cervical spine surgery.
We performed more complicated surgeries, such as fusion or anterior and posterior surgeries, in the DSA group, which included cases with instability and severe deformity. On the contrary, the non-DSA group was treated with LP alone in most cases. Therefore, the operative time was significantly longer in the DSA group than in the non-DSA group. Chikawa et al. and Yamada et al. also reported that the operation time was longer in the DSA group due to more frequent fusion surgeries7,19). However, intraoperative blood loss was lower in the DSA group, which might be in part due to the shorter duration of HD compared with the non-DSA group. Indeed, longer HD duration might cause fragility of the blood vessels and other tissues and lead to hemorrhage20,21). The recovery rates of the mJOA score in the DSA and non-DSA groups were 4.5 and 4.1, respectively, which is in agreement with the previous reports2,7,19,22).
Recently, using national database, Chikuda et al. has reported the postoperative complication rate of spine surgeries in HD patients (9.55%), which was higher than that in non-HD patients (3.63%)12). Chung et al. investigated the postoperative complication rate in elective lumbar spine surgeries in HD patients and reported major and minor complication rates of 8.1% and 39.6%, respectively14). Ottesen et al. reported that the postoperative complication rate in elective spine surgeries in HD patients and major and minor complication rate were 25.91% and 7.71%, respectively13). The postoperative complication rates in the DSA and non-DSA groups were 23% and 19%, respectively, which were almost equivalent to those in previous reports. The in-hospital mortality rate in this study was 2.5%. Previous reports based on large-scale national database revealed 1.9%-4.05% in-hospital mortality rate in HD patients who underwent any spine surgery12-14), which was almost identical to our results. We also compared the surgical results between patients on HD for more than 21 years and those on HD for less than 20 years. Contrary to our expectation, no significant difference was observed in the postoperative complications between the two groups. Based on our results, the HD duration is not associated with postoperative complications. Other authors reported higher mortality rates in single-center case series (9.1%-11.8%), which was higher than our larger scale data19,22). This might be because the number of cases in those reports was relatively low9,22). Inoue et al. reported 48 cases of decompression surgery of the cervical spine in HD patients23). They reported that the postoperative rates of severe complications and mortality were not significantly different between the HD and non-HD groups. They suggested that decompression surgery alone is a rational, less-invasive, surgical method. However, in our study, one of the cases with lethal outcome due to gastrointestinal perforation was previously subjected to cervical decompression only; therefore, the risk of mortality exists even in decompression surgery.
Hitherto, the postoperative survival rate of HD patients who underwent cervical spine surgery has not been reported on a large-scale. Kumar et al. reported that four out of eight (50%) patients who had undergone cervical spine surgery died within 1 year after the surgeries24). Chikawa et al. investigated the postoperative survival rate in spine surgery in 33 HD patients7) and reported that the postoperative survival rate at 49 months was 72.8%. In this study, the postoperative survival rates of cervical spine surgery in HD patients were 89.6%, 75.5%, 67.1%, and 44.7% at 1, 3, 5, and 10 years. Nagai et al. investigated the survival rate of general HD people at an average age of 62.1 years; this age is almost the same as that in our study. They reported that the survival rate of this population at 5 years was 76.2%, slightly better than that in our study. This might be partly because the mean duration of HD in their study was 8.6 years, compared with more than 20 years in our study25). Hence, HD patients who underwent cervical spine surgery were likely in worse general condition due to longer HD duration.
We also investigated the factors affecting the survival rates. Survival rate did not depend on the group (DSA vs. non-DSA group), preoperative HD duration, pre- and postoperative JOA score, age at surgery, and period at which the surgery was performed. In contrast, the survival rates differed depending on the HD cause (DM vs. non-DM, DM vs. CGN). Specifically, when the cause of HD was DM, the 5-year survival rate was the worst (below 50%). According to the report by Nagai et al., the presence of DM was one of the factors of shorter survival25). Currently, DM has become the main cause of HD; therefore, we can expect that the postoperative survival rate in spine surgery in HD patients will also decrease.
The primary limitation of this study was that it was a retrospective study conducted at a single institute, not a multicenter large-scale study. Therefore, the medical standard of the institute affected the postoperative complications and mortality rate. Another limitation may be a discrepancy in the patient numbers between the DSA and non-DSA groups. Furthermore, since the study period was long (1996-2018), the technique of surgery, postoperative care, and way of HD might have improved in this period, thereby possibly affecting the postoperative complications and mortality and survival rates. However, the survival rate between the early and late groups was not significantly different.
In conclusion, cervical spine surgery in HD patients was associated with a high risk of postoperative complications. However, the complication rate did not differ between the DSA and non-DSA groups, although the operation time was longer in the DSA group and intraoperative bleeding was greater in the non-DSA group. The postoperative survival rate of HD patients undergoing cervical spine surgery was worse if the cause of HD was DM. Therefore, patients undergoing HD due to DM should be monitored more carefully after cervical spine surgery to reduce the risk of negative outcomes and mortality.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: None declared.
Author Contributions: KW, RT, TI, KH, and KO were involved in the study design and data interpretation. KW, RT, TI, and KH were involved in the data analysis. All authors critically revised the report, commented on the drafts of the manuscript, and approved the final report.
Ethical Approval: The study was approved by the review board of Tokyo Women's Medical University (No. 5801).
Informed Consent: This study retrospectively reviews medical records of patients who have undergone a specific procedure for clinical purposes. Therefore, this study is of no more than minimal risk to subjects; thus, the need for informed consent has been waived by the IRB.
References
- 1.Kuntz D, Naveau B, Bardin T, et al. Destructive spondylarthropathy in hemodialyzed patients. A new syndrome. Arthritis Rheum. 1984;27(4):369-75. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Ito M, Kaneda K. Surgical treatment of cervical destructive spondyloarthropathy (DSA). Spine. 2000;25(22):2899-905. [DOI] [PubMed] [Google Scholar]
- 3.Sudo H, Ito M, Abumi K, et al. Long-term follow up of surgical outcomes in patients with cervical disorders undergoing hemodialysis. J Neurosurg Spine. 2006;5(4):313-9. [DOI] [PubMed] [Google Scholar]
- 4.Van Driessche S, Goutallier D, Odent T, et al. Surgical treatment of destructive cervical spondyloarthropathy with neurologic impairment in hemodialysis patients. Spine. 2006;31(6):705-11. [DOI] [PubMed] [Google Scholar]
- 5.Yuzawa Y, Kamimura M, Nakagawa H, et al. Surgical treatment with instrumentation for severely destructive spondyloarthropathy of cervical spine. J Spinal Disord Tech. 2005;18(1):23-8. [DOI] [PubMed] [Google Scholar]
- 6.Shiraishi T, Ikegami T, Okubo Y, et al. Cervical peridural calcification in patients undergoing long-term hemodialysis. Report of two cases. J Neurosurg. 2004;100(3):284-6. [DOI] [PubMed] [Google Scholar]
- 7.Chikawa T, Sakai T, Bhatia NN, et al. Clinical outcomes of spinal surgery in patients treated with hemodialysis. J Spinal Disord Tech. 2013;26(6):321-4. [DOI] [PubMed] [Google Scholar]
- 8.Wada K, Murata Y, Kato Y. Surgical outcome for hemodialysis-related upper cervical lesions. Asian Spine J. 2015;9(5):699-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kato Y, Kanaya K, Itoh T. Destructive spondyloarthropathy of the atlantoaxial joint with severe spinal cord compression in long-term hemodialysis patients. J Orthop Sci. 2006;11(6):644-50. [DOI] [PubMed] [Google Scholar]
- 10.Mikawa Y, Yamaoka T, Watanabe R. Compression of the spinal cord due to destructive spondyloarthropathy of the atlanto-axial joints. J Bone Joint Surg Am. 1996;78(12):1911-4. [DOI] [PubMed] [Google Scholar]
- 11.Vignes JR, Eimer S, Dupuy R, et al. Beta(2)-Microglobulin amyloidosis caused spinal cord compression in a long-term haemodialysis patient. Spinal Cord. 2007;45(4):322-6. [DOI] [PubMed] [Google Scholar]
- 12.Chikuda H, Yasunaga H, Horiguchi H, et al. Mortality and morbidity in dialysis-dependent patients undergoing spinal surgery: analysis of a national administrative database in Japan. J Bone Joint Surg Am. 2012;94(5):433-8. [DOI] [PubMed] [Google Scholar]
- 13.Ottesen TD, McLynn RP, Zogg CK, et al. Dialysis is an independent risk factor for perioperative adverse events, readmission, reoperation, and mortality for patients undergoing elective spine surgery. Spine J. 2018;18(11):2033-42. [DOI] [PubMed] [Google Scholar]
- 14.Chung AS, Campbell DH, Hustedt JW, et al. Inpatient outcomes in dialysis-dependent patients undergoing elective lumbar surgery for degenerative lumbar disease. Spine. 2017;42(19):1494-501. [DOI] [PubMed] [Google Scholar]
- 15.Kushioka J, Takenaka S, Makino T, et al. Risk factors for in-hospital mortality after spine surgery: a matched case-control study using a multicenter database. Spine J. 2020;20(3):321-8. [DOI] [PubMed] [Google Scholar]
- 16.Chin M, Hase H, Miyamoto T, et al. Radiological grading of cervical destructive spondyloarthropathy in long-term hemodialysis patients. J Spinal Disord Tech. 2006;19(6):430-5. [DOI] [PubMed] [Google Scholar]
- 17.Itoh T, Tsuji H. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine. 1985;10(8):729-36. [DOI] [PubMed] [Google Scholar]
- 18.Nitta K, Masakane I, Hanafusa N, et al. Annual dialysis data report 2017, JSDT Renal Data Registry. Ren Replace Ther. 2019;5(53):1-44. [Google Scholar]
- 19.Yamada T, Yoshii T, Hirai T, et al. Clinical outcomes of spinal surgery for patients undergoing hemodialysis. Orthopedics. 2016;39(5):e863-8. [DOI] [PubMed] [Google Scholar]
- 20.Holden RM, Harman GJ, Wang M, et al. Major bleeding in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3(1):105-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kawahara T, Kawahara K, Ito H, et al. Spontaneous renal hemorrhage in hemodialysis patients. Case Rep Nephrol Urol. 2011;1(1):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maruo K, Tachibana T, Arizumi F, et al. Clinical outcomes after posterior cervical decompression and fusion surgery for destructive spondyloarthropathy in patients undergoing long-term hemodialysis: a matched case-control study. J Orthop Sci. 2019;24(3):404-8. [DOI] [PubMed] [Google Scholar]
- 23.Inoue T, Mizutamari M, Fukuda K, et al. Postoperative complications in dialysis-dependent patients undergoing elective decompression surgery without fusion or instrumentation for degenerative cervical or lumbar lesions. Spine. 2018;43(17):1169-75. [DOI] [PubMed] [Google Scholar]
- 24.Kumar A, Leventhal MR, Freedman EL, et al. Destructive spondyloarthropathy of the cervical spine in patients with chronic renal failure. Spine. 1997;22(5):573-7. [DOI] [PubMed] [Google Scholar]
- 25.Nagai K, Matsuura M, Tsuchida K, et al. Prognostic factors for mortality in middle-aged and older hemodialysis patients: a 5-year observational study. J Artif Organs. 2018;21(1):94-101. [DOI] [PubMed] [Google Scholar]