Abstract
Coracoid process is a hook-like structure connected with multiple ligaments. The complexity and its close relations often create confusion. The aim of this study is to identify the ligaments attached to the coracoid process as discrete structures on 3T magnetic resonance imaging (MRI) scans. This is a retrospective observational study. One-hundred twenty MRI shoulder studies performed during November and December 2019 at Dept of Radiology, Deenanath Mangeshkar Hospital, Pune, were evaluated. These were obtained on 3T MRI (Siemens, Pennsylvania, United States) machine. All scans were evaluated by two experienced musculoskeletal radiologists. The ligaments studied were coracohumeral (CHL), coracoclavicular (CCL), coracoacromial (CAL), and coracoglenoid (CGL) ligaments. Mean age of cohort was 56.3 years with 59.2% males and 56.2% right shoulder studies. Pain was the main presenting symptom (49%) followed by instability (35%). Reader 1 identified CHL in 106 out of 120 and reader 2 identified 108 out of 120 on all 3 planes. Substantial interobserver agreement (κ =0.65) was noted for sagittal T1 and proton density fat saturated (PDFS) sequences. Both readers could identify CCL and CAL ligaments in all three sequences with better confidence on nonfat saturated sagittal images. Reader 1 identified CGL in 9 on axial and 12 on sagittal images among 120 cases. Reader 2 identified CGL in 13 on axial and 16 on sagittal images among 120 cases. With a κ = 0.702 for the axial PDFS and κ = 0.72 for sagittal T1 and PDFS sequence, substantial interobserver agreement was noted. Sagittal images were better in the evaluation of CGL. Identifying ligaments attached to coracoid on MRI helps in managing associated pathological states.
Keywords: capsuloligamentous complex, coracoglenoid ligament, coracohumeral ligament, coracoclavicular ligament, coracoacromial ligament
Introduction
Shoulder joint is the most mobile joint in the body. The ligaments attached to the glenoid, humerus, and the coracoid form the most important stabilizers of the shoulder joint. The coracoid also is a vital anchor for several tendinous and ligamentous attachments. The important ligamentous structures ( Fig. 1 ) attached to the coracoid process are coracohumeral (CHL), coracoclavicular (CCL), coracoacromial (CAL), and coracoglenoid (CGL) ligaments. The coracoid and its associated structures are linked to numerous pathologic conditions involving the shoulder 1
Fig. 1.
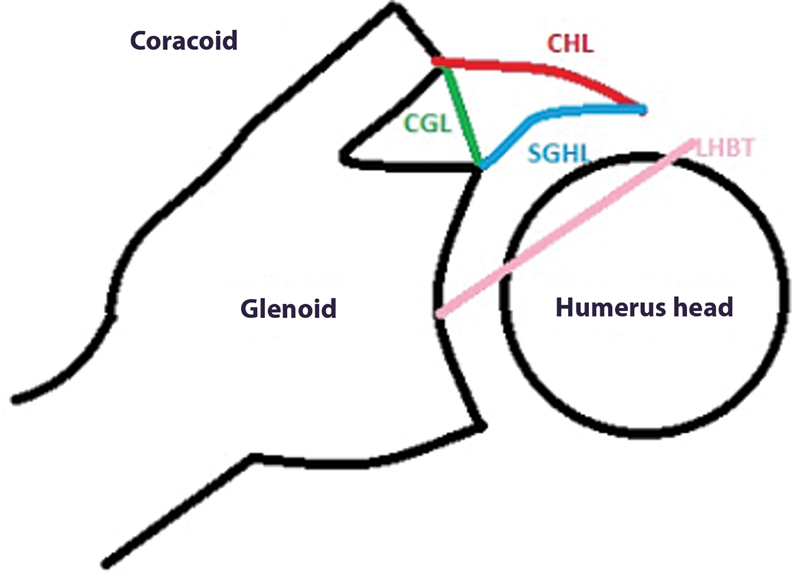
Normal ligaments from coracoid process (axial). CGL, coracoglenoid ligament; CHL, coracohumeral ligament; LHBT, long head of the biceps tendon; SGHL, superior glenohumeral ligament.
The CHL ( Fig. 2 ) arises outside the glenohumeral joint from the lateral aspect of the bottom of the coracoid process of the scapula. It broadens to merge with the rotator interval capsule and inserts on both the lesser and greater tuberosities. The CHL arises from the dorsolateral aspect of the base of the coracoid process and courses through the rotator interval to blend with fibers from the superior glenohumeral ligament (SGHL).
Fig. 2.
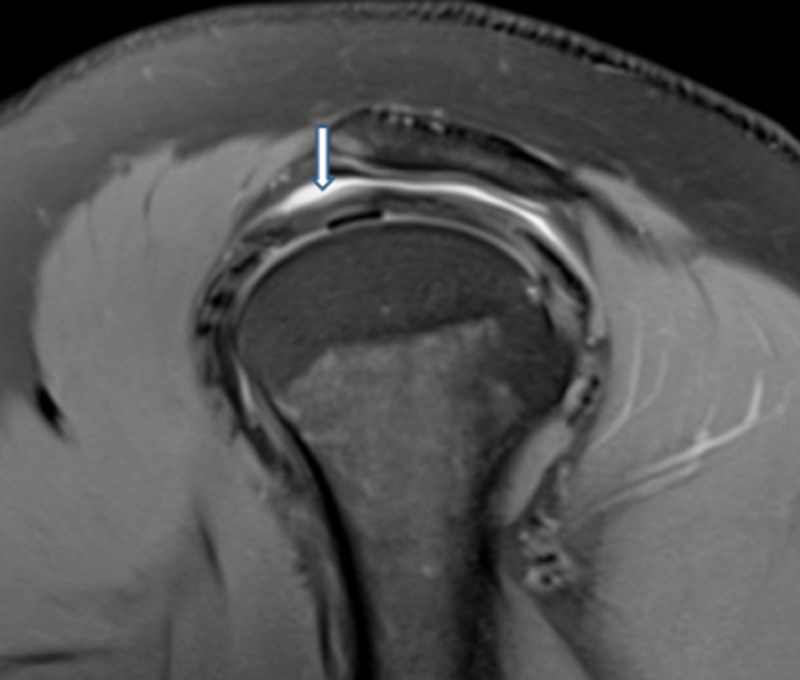
Magnetic resonance imaging PDFS sagittal image showing coracohumeral ligament.
The CCL is a complex of two components: the conoid and trapezoid segments. These two segments are continuous inferiorly at the coracoid process attachment but separate before attaching to the inferior aspect of the clavicle superiorly ( Fig. 3A–D ).
Fig. 3.
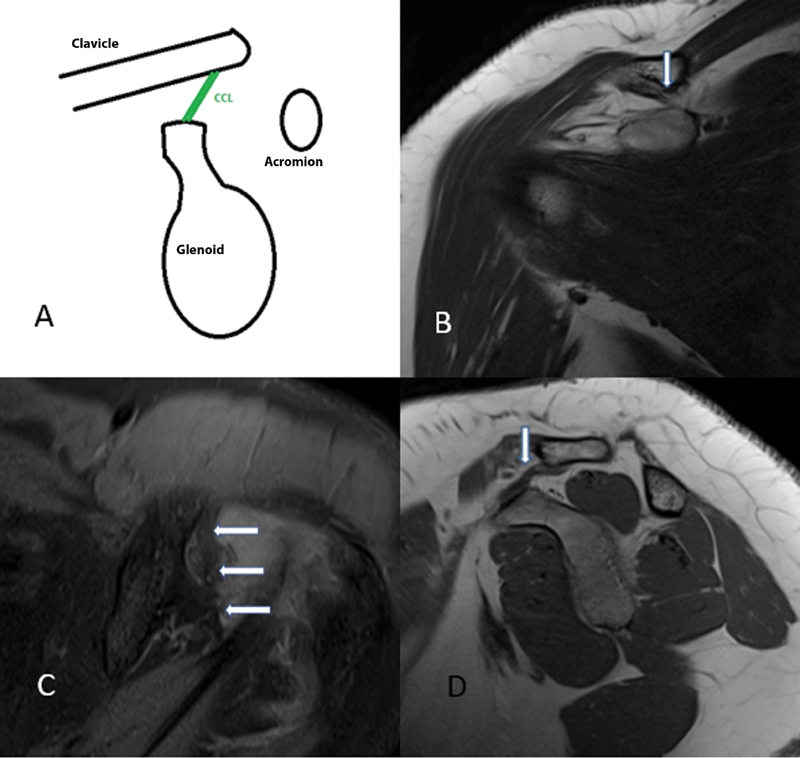
Coracoclavicular ligament in sagittal graphical ( A ), coronal T2 ( B ), axial PDFS ( C ), and sagittal T1 images ( D ).
In 1970s, Dr. Charles Neer 2 first described CAL as a pain generator. The CAL extends from the inferior anterolateral surface of the acromion to the lateral border of the coracoid process ( Fig. 4A–D ).
Fig. 4.
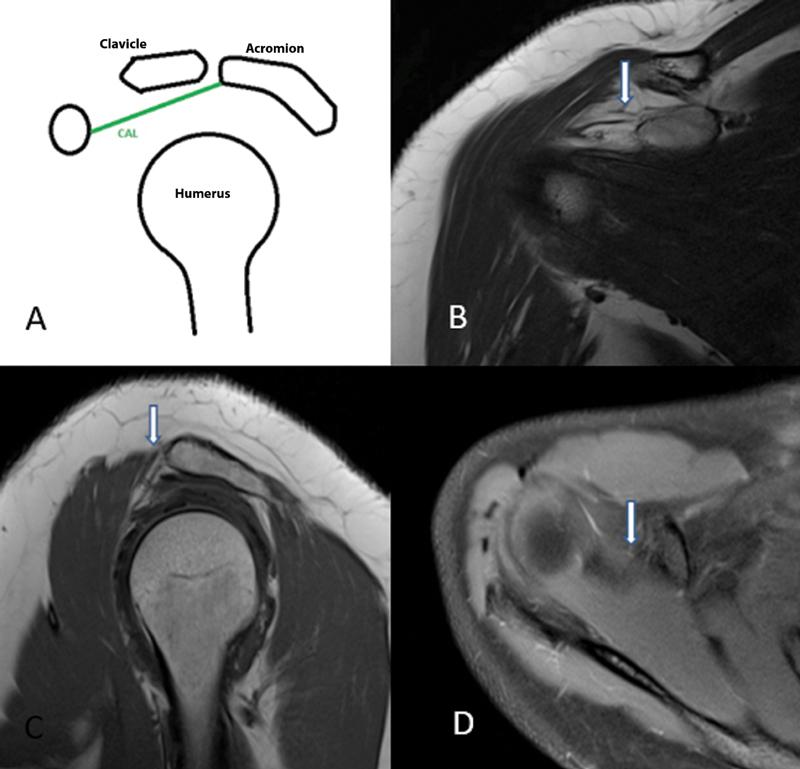
Coracoacromial ligament in sagittal graphical ( A ), coronal T2 ( B ), sagittal T1 ( C ), and axial PDFS ( D ) images.
The CGL, first described by Sappey in 1867, 3 is a structure that originates at the base of the coracoid process and projects toward the glenoid labrum zone. However, there is no mention within the recent literature except within the study done by Zappia et al in 2017 ( Fig. 5A and B ).
Fig. 5.
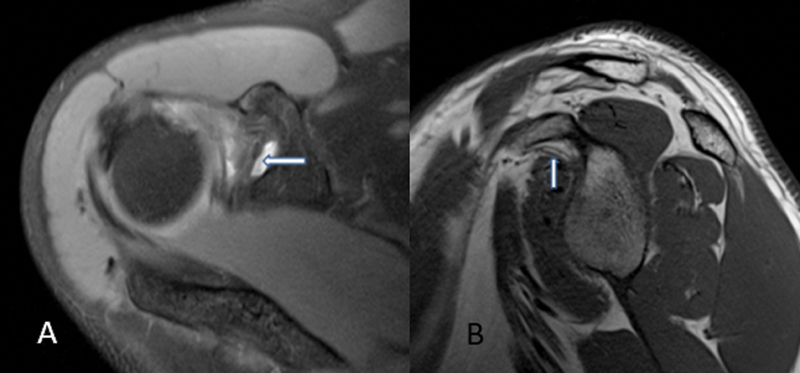
Coracoglenoid ligament in axial PDFS ( A ) and sagittal T1 ( B ) images.
The CGL is the thick band of the connective tissue forming part of anterosuperior capsuloligamentous complex. Detailed evaluation has been performed in the past by Li et al, 4 Kolts et al, 5 and Pouliart et al 6 in cadaveric studies.
The CGL originates in the middle of the upper or posterior surface of the coracoid process, usually between the CAL and CHL, and inserts on the supraglenoid tubercle, covering the origin of the long tendon of the biceps, while remaining extraarticular. The appearance of CGL has multiple variations and is often found in association with CHL or SGHL. 1
The aim of this study was to identify the ligaments attached to the coracoid process as discrete structures on 3T magnetic resonance imaging (MRI) without any arthrography/contrast separately from the adjacent structures. The routine identification of this structure helps in avoiding confusion with pathologies of neighboring structures.
Materials and Methods
We retrospectively evaluated 120 MRI scans of the shoulder, performed at Dept of Radiology, Deenanath Mangeshkar Hospital and Research Institute, Pune. Patients who underwent MRI examination of the shoulder in the months of November and December 2019 were selected from our database. No exclusion criteria were used.
The MRI scans were performed on 3T magnet (Siemens; Magnetom Skyra), with a dedicated shoulder coil. Our MRI shoulder protocol includes sequences acquired with a neutral position of the arm: PDFS (TR-3000, TE-30, Matrix-312 × 256) in three orthogonal planes, that is, axial, oblique sagittal, and oblique coronal planes. Smallest field of view (12–15 cm) that do not produce aliasing was used. These were supplemented by oblique coronal non-fat saturated T2 (TR-3500, TE-80, Matrix- 312 × 256) and oblique sagittal T1 (TR-600, TE-12, Matrix- 312 × 256) sequences. Slice thickness was 2.5 mm in all planes.
On MRI, the CHL was seen as a linear, laterally downslope hypointense structure traversing the fat above the shoulder joint on the first few coronal oblique sections after the coracoid process. On sagittal images lateral to the coracoid process, it can be seen traversing the fat above the joint capsule. Further laterally, it merges with the rotator interval joint capsule, where it cannot be identified as a separate structure. The fused CHL anterosuperior joint capsule also can be seen on axial sections just below the level of the coracoid process. CCL will be visualized as a hypointense band running posterosuperior from base of coracoid process to undersurface of clavicle. CCL is visualized in the sagittal, coronal, or axial planes as a hypointense band extending inferomedial from the inferior anterolateral surface of the acromion to the lateral border of the coracoid process.
On the basis of the known anatomy and the imaging description, 6 7 we assumed that the CGL should appear as a hypointense band running in the subcoracoid fat from the base of the coracoid process to the supraglenoid tubercle.
Based on this understanding, the images were individually evaluated by two experienced musculoskeletal radiologists (5 years for reader 1 and 4 years for reader 2).
On MRI examinations, the ligaments were evaluated. Only those scans in which the ligaments could be visualized separately from the adjacent structures like SGHL and long head of the biceps tendon (LHBT) were considered “positive identification.” Patients in whom the presence/visualization of the ligament was suspicious were interpreted as “non visualization.”
Results
Mean age of the cohort was 56.3 years. Out of this subject population, 59.2% patients were male and 56.2% shoulder studies were from the right side. Pain was the main presenting symptom (49%) followed by shoulder instability (35%) ( Tables 1 , 2 , 3 , 4 ).
Table 1. MRI evaluation of CHL by two radiologists.
| Reader 1 | Reader 2 | |
|---|---|---|
| Axial PDFS | 106 (88.3%) | 108 (90%) |
| Sagittal T1/PDFS | 106 (88.3%) | 108 (90%) |
| Coronal T2/PDFS | 106 (88.3%) | 108 (90%) |
Abbreviations: CHL, coracohumeral ligament; MRI, magnetic resonance imaging; PDFS, proton density fat saturated.
Table 2. MRI evaluation of CCL by two radiologists.
| Reader 1 | Reader 2 | |
|---|---|---|
| Axial PDFS | 120 (100%) | 120 (100%) |
| Sagittal T1/PDFS | 120 (100%) | 120 (100%) |
| Coronal T2/PDFS | 120 (100%) | 120 (100%) |
Abbreviations: CCL, coracoclavicular ligament; MRI, magnetic resonance imaging; PDFS, proton density fat saturated.
Table 3. MRI evaluation of CAL by two radiologists.
| Reader 1 | Reader 2 | |
|---|---|---|
| Axial PDFS | 120 (100%) | 120 (100%) |
| Sagittal T1/PDFS | 120 (100%) | 120 (100%) |
| Coronal T2/PDFS | 120 (100%) | 120 (100%) |
Abbreviations: CAL, coracoacromial ligament; MRI, magnetic resonance imaging; PDFS, proton density fat saturated.
Table 4. MRI evaluation of CGL by two radiologists.
| Reader 1 | Reader 2 | |
|---|---|---|
| Axial PDFS | 9 (7.5%) | 12 (10%) |
| Sagittal T1/PDFS | 13 (10.8%) | 16 (13.3%) |
| Coronal T2/PDFS | 0(0) | 0(0) |
Abbreviations: CGL, coracoglenoid ligament; MRI, magnetic resonance imaging; PDFS, proton density fat saturated.
Reader 1 could identify CHL in 106 cases out of 120 and reader 2 could identify 108 cases out of 120 on axial, sagittal, and coronal images. Total number of cases agreed by both readers were 105. With a κ = 0.65 for the sagittal T1 and PDFS sequence substantial interobserver agreement was noted.
Both the Readers could identify CCL and CAL in all three sequences. However, the confidence with which the ligament could be identified was better on non-fat saturated sagittal images.
Reader 1 could identify the CGL in 9 cases on axial (7.5%) and on 12 cases on sagittal images (10%) among total 120 cases. Reader 2 could identify the CGL in 13 cases on axial (10.8%) and on 16 cases on sagittal images (13.3%) among total 120 cases. Total number of cases agreed by both readers—axial only (8) and sagittal only (11). Seven cases were identified on both axial and sagittal planes by both readers.
With a κ = 0.702 for the axial PDFS and κ = 0.72 for sagittal T1 and PDFS sequence substantial interobserver agreement was noted. Sagittal images were better than axial images in the evaluation of CGL.
Discussion
This study shows that majority of the ligaments arising from the coracoid process can be identified discretely on noncontrast (plain) MRI scans of the shoulder on 3T.
To the best of our knowledge, there is no study that has been done to evaluate ligaments arising from the coracoid process on 3T MRI for their positive identification, although there are few studies in addressing individual ligaments as below.
Li et al in his study showed that MRI is a satisfactory method for CHL depiction, and a thickened CHL is highly suggestive of frozen shoulder. 8 The identification of CHL was studied in normal healthy volunteers by these authors in their control group consisting of 120 and found to be 91.7%. This correlates with our study that detected the ligament in average 89.65%.
Totterman et al 9 reported that the CAL is best viewed in an oblique sagittal plane.
Zappia et al 10 studied the identification and classification of the CGL on MR and MR arthrography imaging. The anterosuperior ligament complex formed by the CGL, the SGHL, and the CHL was classified into six subtypes. They found distinct CGL in over 35% of the cases.
Crótida de la Cuadra-Blanco 11 in their study showed the presence of the CGL as a constant anatomical structure. They also revealed that it is developed as a stronger structure in cases where the LHBT exclusively originates from the glenoid labrum and lacks any bony attachment on the scapula.
Antonio et al 12 in their study reported that CCL plays a central role in maintaining acromioclavicular joint stability, and its appearance should be carefully scrutinized in all patients undergoing shoulder MRI.
Based on the criteria mentioned, the various ligaments were identified. Most of the ligaments were better identified on nonfat saturated images except for CHL that was better seen on PDFS sequence. There was no difficulty in identifying the CCL and CAL. However, the CHL could not be seen as a discrete structure from its origin at the base of the coracoid to the humeral insertion in contiguous sequential images.
Using the criterion of a hypointense band running from the base of the coracoid process to the supraglenoid tubercle, CGL as discrete structure was identified in ∼10% of the totally evaluated cases. CGL was better identified in nonfat saturated sagittal images. The axial PDFS was less sensitive in identifying the ligament probably due to the lack of good interface in between the structures owing to dark ligament and fat. Identification of CGL was 10% in comparison to 35% by Zappia et al probably due to use of MR arthrography by the latter. However, the methodology adopted by them to identify an extraarticular structure like CGL on MR arthrography is not completely understood.
There could be other reasons for the reduced number of positive cases of CGL identification in our study. First, there are limited cadaveric studies in identification of this ligament consistently in all human beings. Second, there could be a learning curve in identifying this structure on MRI. Third, the existing anatomical planes may not be customized to the evaluation of this structure, the importance of which is currently not well understood.
A limitation of this study is nonevaluation of normal subjects without any shoulder-related symptomatology. However, the involvement of CGL in patients with shoulder pain and instability that formed most of the examinations evaluated in this study is as yet indeterminate. Second, most of the symptomatic patients were treated conservatively and only few needed surgical explorations in the form of arthroscopy for various other reasons. CGL cannot be visualized during the arthroscopic procedure as it is an extraarticular structure.
Inability to identify CHL consistently could be due to its laxity in neutral position for MR of shoulder, close proximity of its inferior portion with LHBT and SGHL, and complex anatomy of the ligament as it extends superoinferiorly.
CAL and CCL are fairly established ligaments according to literature, orthopaedic surgeons, and radiologists with respect to their presence, functions, and pathologies. There were no obvious limitations regarding their evaluation.
Conclusion
The coracoid process acts as an important landmark that serves as a guide in shoulder surgeries. The various pathological conditions involving the coracoid and the ligaments attached to it are broad. These conditions may limit the normal mobility of the shoulder joint and incapacitate the patient. Hence, detailed anatomy of the coracoid and its related structures is crucial.
CGL being a less studied ligament needs a special mention and needs to be studied in more detail as a comparative study between the cadavers and normal asymptomatic population with MRI as well as those with shoulder pathologies to identify its clinical and etiopathological significance. Imaging planes will also need to be modified to evaluate the CHL due to declining use of invasive techniques like for MR arthrography for its evaluation owing to the increasing use of 3T MRI.
Funding Statement
Source of Funding Nil.
Conflicts of Interest There are no conflicts of interest.
Disclosure
No disclosures.
Financial Support and Sponsorship
Nil.
References
- 1.Mohammed H, Skalski M R, Patel D B. Coracoid process: the lighthouse of the shoulder. Radiographics. 2016;36(07):2084–2101. doi: 10.1148/rg.2016160039. [DOI] [PubMed] [Google Scholar]
- 2.Neer C. Anterior Acromioplasty for the Chronic Impingement Syndrome in the Shoulder. J Bone Joint Surg. 1972;54(01):41–50. [PubMed] [Google Scholar]
- 3.Sappey P.(1867). Traite d'anatomie descriptive, vol. II, part I. Paris. Cited in: Weinstabl R, Herz H, Firbas W. Zusammenhang des Ligamentum coracoglenoidale mit dem Musculus pectoralis minor1986125126–131. [PubMed] [Google Scholar]
- 4.Li J Q, Tang K L, Wang J. MRI findings for frozen shoulder evaluation: is the thickness of the coracohumeral ligament a valuable diagnostic tool? PLoS One. 2011;6(12):e28704. doi: 10.1371/journal.pone.0028704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kolts I, Busch L C, Tomusk H. Anatomy of the coracohumeral and coracoglenoidal ligaments. Ann Anat. 2000;182(06):563–566. doi: 10.1016/S0940-9602(00)80105-3. [DOI] [PubMed] [Google Scholar]
- 6.Pouliart N, Somers K, Eid S, Gagey O. Variations in the superior capsuloligamentous complex and description of a new ligament. J Shoulder Elbow Surg. 2007;16(06):821–836. doi: 10.1016/j.jse.2007.02.138. [DOI] [PubMed] [Google Scholar]
- 7.Pouliart N, Boulet C, Maeseneer M D, Shahabpour M. Advanced imaging of the glenohumeral ligaments. Semin Musculoskelet Radiol. 2014;18(04):374–397. doi: 10.1055/s-0034-1384827. [DOI] [PubMed] [Google Scholar]
- 8.Petchprapa C N, Beltran L S, Jazrawi L M, Kwon Y W, Babb J S, Recht M P. The rotator interval: a review of anatomy, function, and normal and abnormal MRI appearance. AJR Am J Roentgenol. 2010;195(03):567–576. doi: 10.2214/AJR.10.4406. [DOI] [PubMed] [Google Scholar]
- 9.Totterman S M, Miller R J, Meyers S P. Basic anatomy of the shoulder by magnetic resonance imaging. Top Magn Reson Imaging. 1994;6:86–93. [PubMed] [Google Scholar]
- 10.Zappia M, Castagna A, Barile A, Chianca V, Brunese L, Pouliart N. Imaging of the coracoglenoid ligament: a third ligament in the rotator interval of the shoulder. Skeletal Radiol. 2017;46(08):1101–1111. doi: 10.1007/s00256-017-2667-9. [DOI] [PubMed] [Google Scholar]
- 11.de la Cuadra-Blanco C, Arráez-Aybar L A, Murillo-González J A, Herrera-Lara M E, Mérida-Velasco J A, Mérida-Velasco J R. Development of the human biceps brachii tendon and coracoglenoid ligament (7th-12th week of development) Cells Tissues Organs. 2017;203(06):365–373. doi: 10.1159/000455191. [DOI] [PubMed] [Google Scholar]
- 12.Antonio G E, Cho J H, Chung C B, Trudell D J, Resnick D. Pictorial essay. MR imaging appearance and classification of acromioclavicular joint injury. AJR Am J Roentgenol. 2003;180(04):1103–1110. doi: 10.2214/ajr.180.4.1801103. [DOI] [PubMed] [Google Scholar]


