Abstract
Spontaneous portosystemic shunt (SPSS) refers to collateral vessels that communicate between the portal vein system and systemic circulation. SPSS mainly includes esophageal varices, gastric varices, left gastric vein, recanalized paraumbilical vein, abdominal wall varices, and spontaneous splenorenal shunt. SPSS contributes to the development of hepatic encephalopathy caused by portal vein inflow bypassing and carries a higher risk of death in liver cirrhosis. Abdominal contrast-enhanced computed tomography is a major imaging approach to establish a diagnosis of SPSS and evaluate its location and feature. This review primarily describes the main contrast-enhanced CT features of SPSS in liver cirrhosis.
1. Introduction
Spontaneous portosystemic shunt (SPSS) refers to collateral vessels that communicate between the portal vein system and systemic circulation [1] (Figure 1). SPSS is traditionally considered as a compensatory mechanism of portal hypertension in liver cirrhosis because it can decompress the portal venous system [2]. However, SPSS has been recently regarded as a feature of severe portal hypertension and associated with poor prognosis [3].
Figure 1.
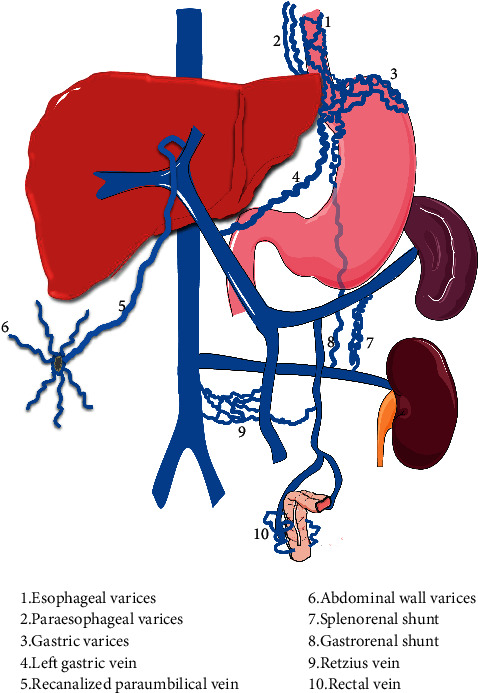
A schematic diagram of spontaneous portosystemic shunt in liver cirrhosis. Note: (1) esophageal varices; (2) paraesophageal varices; (3) gastric varices; (4) left gastric vein; (5) recanalized paraumbilical vein; (6) abdominal wall varices; (7) splenorenal shunt; (8) gastrorenal shunt; (9) Retzius vein; (10) rectal vein.
Until now, the pathophysiological mechanism of SPSS has not been completely elucidated. Traditionally, the formation of SPSS may be attributed to the dilatation of preexisting vessels, but recent studies suggest that it may also be related to neovascularization driven by vascular endothelial growth factor [4, 5]. Additionally, it seems that nonviral liver cirrhosis, especially alcoholic cirrhosis, is significantly associated with the development of SPSS [6, 7].
SPSS mainly includes esophageal varices, gastric varices, left gastric vein, recanalized paraumbilical vein, abdominal wall varices, and spontaneous splenorenal shunt (SSRS) [8]. SPSS contributes to a variety of serious complications, including gastrointestinal bleeding secondary to gastroesophageal variceal rupture and hepatic encephalopathy caused by portal vein inflow bypassing [1], and increases the risk of death [9].
A detailed description of the vascular anatomy of SPSS by imaging examinations is helpful to further understand the formation of collateral vessels secondary to portal hypertension. In recent years, abdominal contrast-enhanced computed tomography (CT) scan is a commonly used imaging technique to evaluate the development of collateral vessels [10]. Herein, we briefly review the prevalence, classification, clinical significance, and therapeutic implications of SPSS with an emphasis on the main contrast-enhanced CT features of SPSS in liver cirrhosis.
2. Prevalence
The prevalence of various types of SPSS on the contrast-enhanced CT scan is different (Figure 2). Esophageal varices are one of the most common types of SPSS in cirrhotic patients undergoing CT scan, with a prevalence of 23.9–58.6% [11–13]. The prevalence of SSRS is 16.1–42.8% [10, 12, 14, 15], that of recanalized paraumbilical vein is 2.9–38% [12, 14], that of paraesophageal shunt is 10.4–22% [13, 14, 16], and that of gastric varices is 11.7–21.6% [12, 17].
Figure 2.
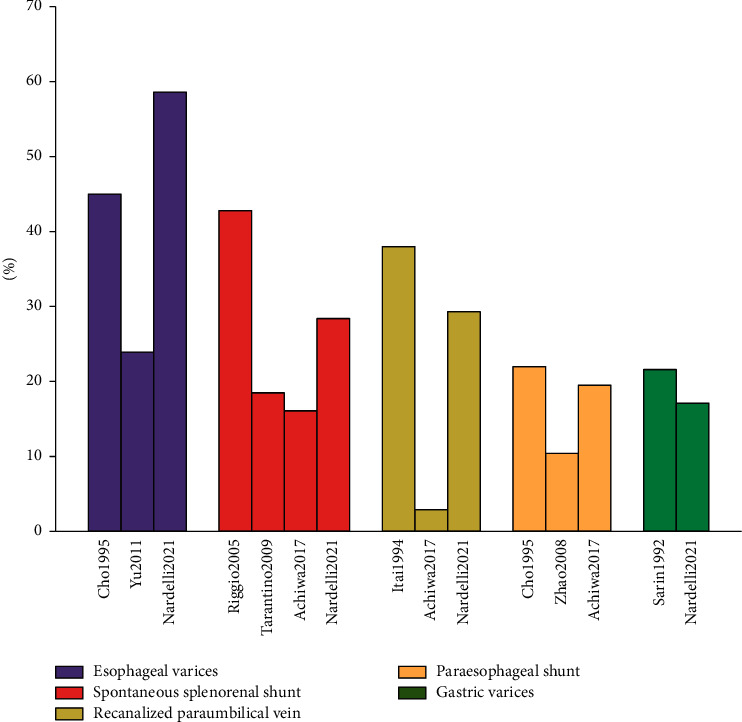
Prevalence of various types of SPSS on the contrast-enhanced CT scan.
3. Classifications
Traditionally, SPSS is termed as varices and shunts [18]. For example, gastroesophageal varices (GEVs) are attributed to the former type and SSRS to the latter one. Nowadays, SPSS is often classified as a drainage into the superior or inferior vena cava according to the outflow tract of collateral vessels [19]. Esophageal varices, paraesophageal varices, and gastric varices drain into the superior vena cava; by comparison, gastrorenal shunt, splenorenal shunt, recanalized paraumbilical vein, and abdominal wall varices drain into the inferior vena cava. It is also divided into small (i.e., the maximum diameter was <8 mm) and large (i.e., the maximum diameter was ≥8 mm) SPSS according to the maximum diameter of SPSS.
4. Clinical Significance
SPSS may be closely associated with the development of hepatic decompensation events, including hepatic encephalopathy, gastrointestinal bleeding, ascites, and portal vein thrombosis, and death (Table 1). First, large SPSS is a well-known precipitating factor for hepatic encephalopathy. Studies demonstrated that a maximum diameter of SPSS ≥ 8 mm or a total cross-sectional area of SPSS > 83 mm2 is more prone to develop hepatic encephalopathy [1, 7]. Second, the effect of SPSS on the development of gastrointestinal bleeding in liver cirrhosis remains controversial. Qi et al. found that cirrhotic patients with SSRS had a low prevalence of acute upper gastrointestinal bleeding, probably because it reduces portal pressure, thereby preventing the development of variceal bleeding [20]. By contrast, Nardelli et al. found that cirrhotic patients with SPSS had a higher risk of gastrointestinal bleeding and considered SPSS as a feature of severe portal hypertension and a marker of poor outcome [12]. Third, the association of SPSS with ascites in cirrhotic patients is also unclear. Renzulli et al. found that ascites was the most common decompensation event during follow-up in cirrhotic patients with SPSS and was an independent predictor of decompensation-free survival [25]. By contrast, Saks et al. reported that SSRS was associated with a lower risk of developing ascites in liver transplantation candidates, and the presence of ascites could not predict the risk of death in such patients [22]. Fourth, SPSS is associated with a higher risk of developing portal vein thrombosis in general patients with liver cirrhosis and liver transplantation recipients, probably due to its secondary reduction in portal blood flow [6, 9, 24]. Fifth, nearly all recent studies have found that SPSS had a lower transplantation-free survival and was an independent predictor for death in liver cirrhosis [1, 6, 7, 12].
Table 1.
Comparison of decompensated events and death between with and without SPSS.
| First author (year) | Study design | Enrollment period | Target population | No. of pts. in total | No. of pts. with shunt | Radiological evaluation | HE | Gastrointestinal bleeding | Ascites | Portal vein thrombosis | Death | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| With shunt | Without shunt | With shunt | Without shunt | With shunt | Without shunt | With shunt | Without shunt | With shunt | Without shunt | |||||||
| Qi et al. (2017) [20] | Cross-sectional | Jun. 2012–Dec. 2013 | LC | 105 | 11 | CT or MRI | 2 (18.2%) | 4 (4.7%) | 0 (0%) | 17 (18.1%) | 7 (63.6%) | 52 (55.3%) | NA | NA | 0 (0%) | 4 (4.3%) |
| He et al. (2018) [21] | Cohort | Jan. 2004–Dec. 2014 | LC | 903 | 188 | Angiography | 89 (47.3%) | 278 (39.0%) | 175 (93.1%) | 623 (87.1%) | 126 (67.0%) | 606 (84.7%) | NA | NA | 68 (36.2%) | 311 (43.5%) |
| Saks et al. (2018) [22] | Cohort | Jan. 2001–Feb. 2016 | LT | 741 | 173 | CT or MRI | NA | NA | 25% | 28% | 43% | 59% | 13% | 4% | 35% | 42% |
| Simón-Talero et al. (2018) [7] | Cohort | 2010–2015 | LC | 1729 | 1036 | CT or MRI | L: 32% | 8% | L: 25% | 11% | L: 57% | 32% | L: 18% | 5% | L: 38% | 32% |
| S: 19% | S: 26% | S: 55% | S: 10% | S: 28% | ||||||||||||
| Allard et al. (2021) [23] | Cohort | Jan. 2003–Dec. 2016 | LT | 335 | 197 | CT | NA | NA | NA | NA | NA | NA | 36 (18.3%) | 13 (9.5%) | 7 (4.0%) | 6 (4.9%) |
| Nardelli et al. (2021) [12] | Cohort | Mar. 2015–Jul. 2019 | LC | 222 | 141 | CT | 28 (20%) | 11 (13%) | 31 (22%) | 13 (16%) | 84 (60%) | 47 (58%) | 22 (16%) | 3 (4%) | SPSS has a higher mortality | |
| Rathi et al. (2021) [24] | Cohort | 2009–2017 | LC | 127 | 89 | CT or MRI | Large SPSS had a higher risk of HE | NA | NA | 12 (14%) | 3 (8%) | 27 (30%) | 3 (8%) | NA | NA | |
| Yi et al. (2021) [9] | Cohort | Dec. 2014–Aug. 2019 | LC | 122 | 37 | CT or MRI | 4 (10.8%) | 6 (7.1%) | 25 (67.6%) | 67 (78.8%) | 23 (62.2%) | 50 (58.8%) | 13 (35.1%) | 27 (31.8%) | 7 (18.9%) | 4 (4.7%) |
| Dajti et al. (2022) [6] | Cohort | Jan. 2014–Dec. 2017 | ACLD | 235 | 141 | CT or MRI | 9 (6.4%) | 3 (3.2%) | 22 (15.6%) | 5 (5.3%) | 33 (23.4%) | 13 (13.9%) | 20 (14.2%) | 3 (3.2%) | 22 (15.6%) | 9 (9.6%) |
Pts., patients; LC, liver cirrhosis; LT, liver transplantation; SPSS, spontaneous portosystemic shunt; SSRS, spontaneous splenorenal shunt; HE, hepatic encephalopathy; CT, computed tomography; MRI, magnetic resonance imaging; L, large SPSS; S, small SPSS; ACLD, advanced chronic liver disease.
5. Therapeutical Implications
Effective treatment of SPSS should be critical for improving the outcomes of cirrhotic patients and liver transplantation recipients. First, the rupture of GEVs can cause massive upper gastrointestinal bleeding and even lethal hemorrhagic shock [26]. Undoubtedly, the prophylaxis of high-risk GEVs from bleeding and urgent hemostasis of GEVs by vasoactive drugs, endoscopy, and/or transjugular intrahepatic portosystemic shunts (TIPS) should be necessary for saving the patients' lives [27, 28]. Second, large SPSS can induce refractory and recurrent hepatic encephalopathy, negatively influencing the quality of life and survival [7]. Thus, their closure by balloon-occluded retrograde transvenous obliteration (BRTO) and other vascular interventional treatments should be warranted for improving the patients' outcomes [29]. Third, TIPS can effectively decompress the portosystemic pressure and is mainly indicated for the treatment and prevention of GEVs' bleeding [27]. If adjunctive variceal embolization was performed during TIPS procedures, the risk of variceal rebleeding can be further decreased [30]. On the other hand, the presence of large SPSS increases the risk of post-TIPS overt hepatic encephalopathy [21]. Recently, a randomized controlled trial demonstrates that prophylactic embolization of large SPSS during TIPS procedures can reduce the risk of overt hepatic encephalopathy without any increased risk of other liver-related complications [31, 32]. These findings supported embolization of varices and SPSS during TIPS procedures. Fourth, SPSS has a portal blood flow “stealing” effect, reducing the portal blood flow into the graft and impairing the functional recovery of the graft, which may significantly affect the outcomes of liver transplant recipients [2]. Thus, it has been recommended that SPSS should be ligated during liver transplantation procedures [33].
6. Evaluation of SPSS on CT
Angiography is the gold standard diagnostic method used to examine the presence of SPSS, but invasive and expensive, even risky for patients with severe liver dysfunction [34]. By comparison, both contrast-enhanced CT and magnetic resonance imaging (MRI) scans are more convenient imaging methods. Notably, Renzulli et al. demonstrated excellent intraobserver and interobserver agreement in almost all types of SPSS detection and measurement by using CT [25]. Besides, identification of anatomical structures and characteristics (e.g., diameter) of SPSS by using CT can further strengthen the performance of currently available approaches for risk stratification in cirrhotic patients with complications of portal hypertension [35]. Except for measurement of the diameter of SPSS by CT, Praktiknjo et al. developed a software that could automatically calculate the cross-sectional area of SPSS based on the CT image processing [36] and found that the total cross-sectional area of SPSS was more advantageous than the diameter of SPSS for predicting the progression of cirrhosis [1].
As for the diagnosis of GEVs, endoscopy is the gold standard diagnostic method, and it can provide variceal eradication [37]. Contrast-enhanced CT and MRI scans are alternatives with excellent diagnostic accuracy for varices in liver cirrhosis [38–40]. Lipp et al. evaluated the effectiveness of CT and/or MRI examinations for the detection of esophageal varices compared with endoscopy and found that CT was a superior imaging method to MRI for the detection of esophageal varices and could accurately exclude the possibility of large esophageal varices to avoid the need or frequency of endoscopy screening in liver cirrhosis [41]. It should be noted that endoscopy fails to evaluate the entire spectrum of extraparietal GEVs and nongastroesophageal portosystemic collaterals [25]. By comparison, a CT scan can more comprehensively evaluate the anatomy and classification of SPSS, including paraesophageal varices or other perigastric collaterals.
6.1. Esophageal Varices
Esophageal varices, which refer to tortuously dilated esophageal veins [42], are one of the main complications of portal hypertension [43], and esophageal variceal bleeding is one of the most common causes of death in liver cirrhosis [44, 45]. About 30% of patients with liver cirrhosis develop esophageal variceal bleeding [42]. The mortality of each variceal bleeding episode is 10–20% [42]. On the portal vein phase of contrast-enhanced CT scan, esophageal varices manifest as enhanced channels adjacent to the surface of the esophageal lumen or protruding into the esophageal lumen, with round, tubular, or scalloped borders [13, 40] (Figure 3).
Figure 3.
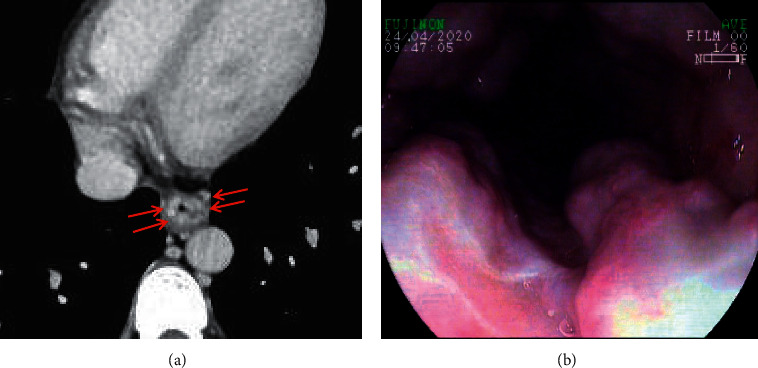
Esophageal varices. In a 38-year-old male with liver cirrhosis, the axial contrast-enhanced CT scan (a) on the portal vein phase demonstrated that esophageal varices (red arrow) were enhanced channels adjacent to the surface of the esophageal lumen, with round, tubular, or scalloped borders. Upper gastrointestinal endoscopy (b) showed several tortuous varices in the esophagus.
6.2. Paraesophageal Varices
Paraesophageal varices, which are dilated veins outside the esophageal wall [46], usually flow into the superior vena cava through the dilated azygos vein or hemiazygos vein and rarely into the inferior vena cava through the inferior phrenic vein [16, 47]. Paraesophageal varices can extend to the thoracic cavity, manifesting as a mass on the plain CT scan, which may be misdiagnosed as a mediastinal tumor [48, 49]. On the portal vein phase of contrast-enhanced CT scan, paraesophageal varices manifest as tortuous vessels outside the esophageal wall, reaching the level of aortic arch upwards and the cardia downwards [50] (Figure 4).
Figure 4.
Paraesophageal varices. In a 37-year-old male with liver cirrhosis, the axial contrast-enhanced CT scan on the portal vein phase demonstrated that paraesophageal varices (red arrow) were tortuous vessels outside the esophageal wall.
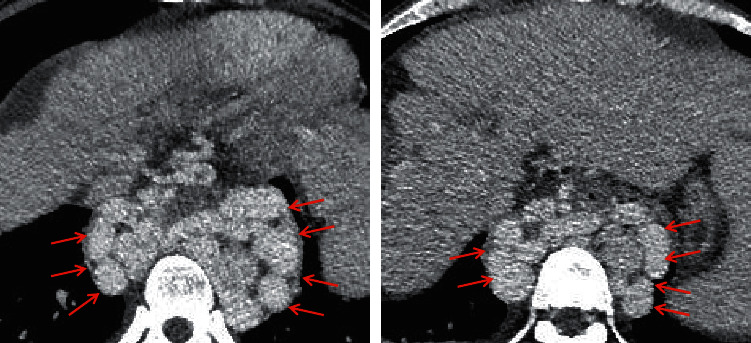
6.3. Gastric Varices
Gastric varices, which refer to tortuous and dilated veins located at the posterosuperior aspect of gastric fundus [46], are a major cause of upper gastrointestinal bleeding in patients with portal hypertension [51]. Gastric varices receive the blood from the left gastric vein, posterior gastric vein, and short gastric vein, and the blood flows into the lower esophageal vein, paraesophageal vein, and/or left inferior phrenic vein [52]. Esophageal and gastric varices are often concomitant [53, 54], which should be classified as GEVs, the most common type of gastric varices. Besides, isolated gastric varices (IGVs) are another type of gastric varices [17]. GEVs are further classified into two subtypes, including GEVs 1, which refer to esophageal varices extending along the lesser curvature of the stomach, and GEVs 2, which refer to esophageal varices extending along the gastric fundus [17]. IGVs are also further classified into two subtypes, including IGVs 1, which refer to varices located at the gastric fundus, and IGVs 2, which refer to isolated varices located at the gastric body and antrum or pylorus [17]. On the portal vein phase of the contrast-enhanced CT scan, gastric varices manifest as long, nodular, and/or tortuous enhanced structures [55] (Figure 5).
Figure 5.
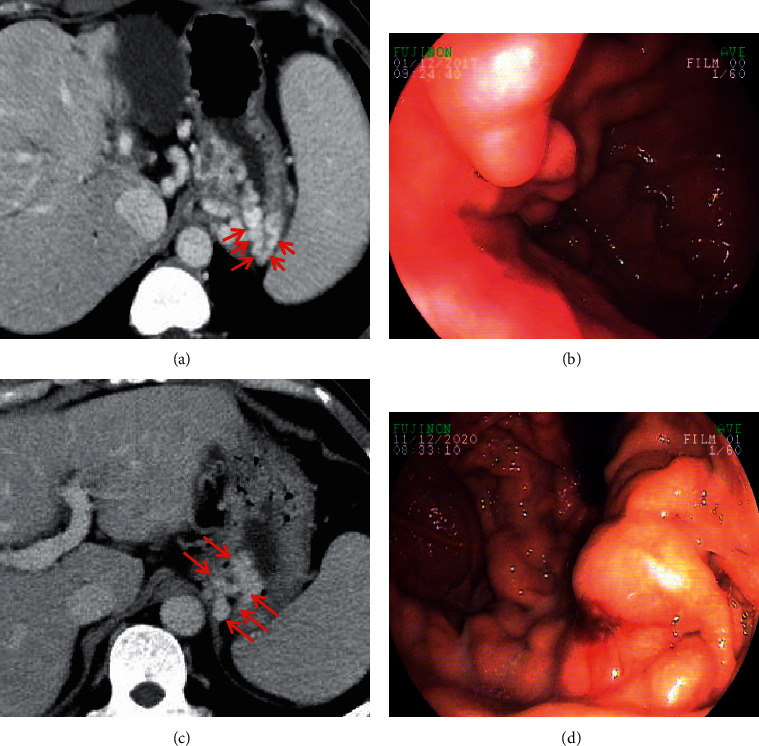
Gastric varices. In a 47-year-old female and a 56-year-old male with liver cirrhosis, the axial contrast-enhanced CT scan on the portal vein phase demonstrated that gastric varices (red arrow) were long, nodular, and tortuous enhanced channels at the gastric fundus. Upper gastrointestinal endoscopy showed dilated and tortuous varices at the gastric fundus. Note: (a, b) the contrast-enhanced CT scan and endoscopy of a 47-year-old female, respectively; (c, d) the contrast-enhanced CT scan and endoscopy of a 56-year-old male, respectively.
6.4. Left Gastric Vein
The left gastric vein, also known as the gastric coronary vein [56], is divided into anterior and posterior branches [57]. The anterior branch forms a reticular vessel at the junction of the stomach and esophagus and anastomoses with the gastric varices, and the posterior branch anastomoses with the paraesophageal vein [57]. The anastomosis of the left gastric vein can be located at the main portal vein, splenic vein, splenoportal vein angle, or left portal vein branch [58]. Patients with the left gastric vein draining into the main portal vein are more prone to cause gastroesophageal variceal bleeding than those with the left gastric vein draining into the splenic vein or splenoportal vein junction [53]. On the portal vein phase of the contrast-enhanced CT scan, the enlarged and tortuous left gastric vein can be observed at the lesser curvature of the stomach and the posterior wall of the left hepatic lobe [59] (Figure 6).
Figure 6.

Left gastric vein. A 76-year-old female with a three-year history of autoimmune-related liver cirrhosis presented with recurrent hematemesis and melena. The coronal contrast-enhanced CT scan on the portal vein phase demonstrated the enlarged and tortuous left gastric vein (red arrow) at the lesser curvature of the stomach and the posterior wall of the left hepatic lobe.
6.5. Recanalized Paraumbilical Vein
The paraumbilical vein, which originates from the left portal vein branch, can be reopened in the setting of portal hypertension and anastomoses with the abdominal wall vein [60]. The large paraumbilical vein can decrease the risk of esophageal variceal bleeding but precipitate the development of hepatic encephalopathy [61, 62]. On the portal vein phase of the contrast-enhanced CT scan, the recanalized paraumbilical vein is a round, dilated, or tubular enhanced structure, descending to the umbilicus from the left portal vein branch [63] (Figure 7).
Figure 7.
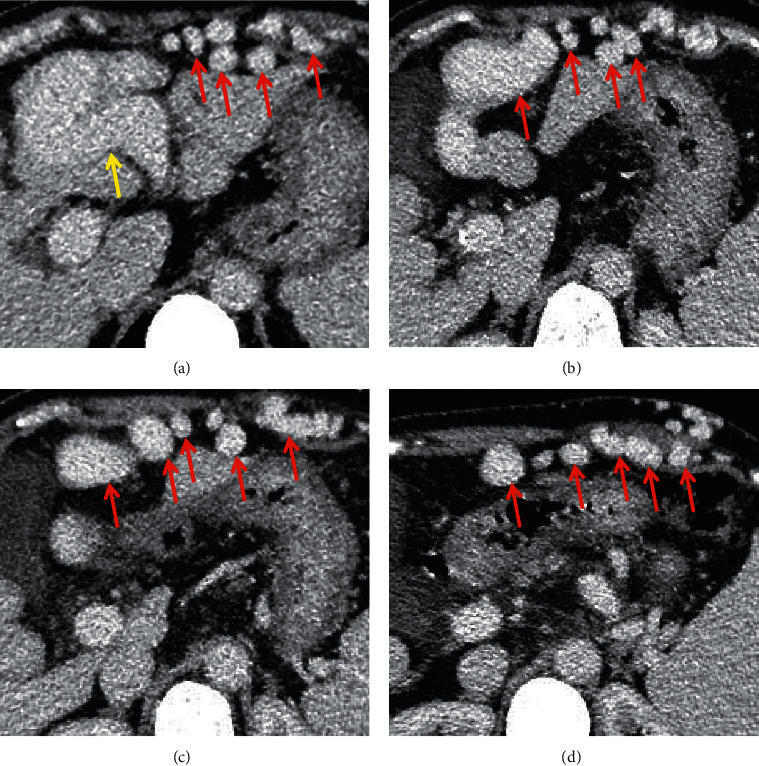
Recanalized paraumbilical vein. In a 65-year-old female with liver cirrhosis, the axial contrast-enhanced CT scan on the portal vein phase demonstrated that the recanalized paraumbilical vein (red arrow) was a round, dilated, or tubular enhanced structure, originating from the left portal vein branch (yellow arrow).
6.6. Abdominal Wall Varices
Abdominal wall varices, which refer to dilated or tortuous veins in the anterior abdominal wall, are commonly seen in the settings of portal hypertension or superior and inferior vena cava obstruction [64]. In patients with severe portal hypertension, varicose veins can be radiated from the umbilicus, which is called “caput medusa” sign [65]. When the superior vena cava is obstructed, the blood flow direction of superficial varicose veins above the umbilicus is downwards [66]. When the inferior vena cava is obstructed, the blood flow direction of superficial abdominal wall veins below the umbilicus is upwards [67]. The presence of abdominal wall varices predicts a worse survival of patients with liver cirrhosis [68]. On the portal vein phase of contrast-enhanced CT scan, abdominal wall varices manifest as dilated, enhanced, and tortuous structures [65] (Figure 8).
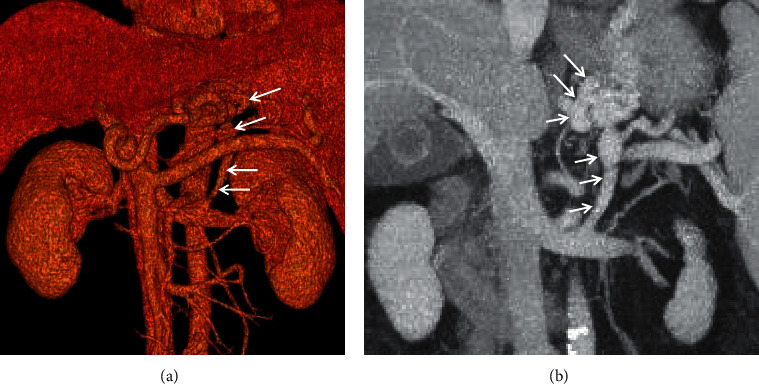
Figure 8.
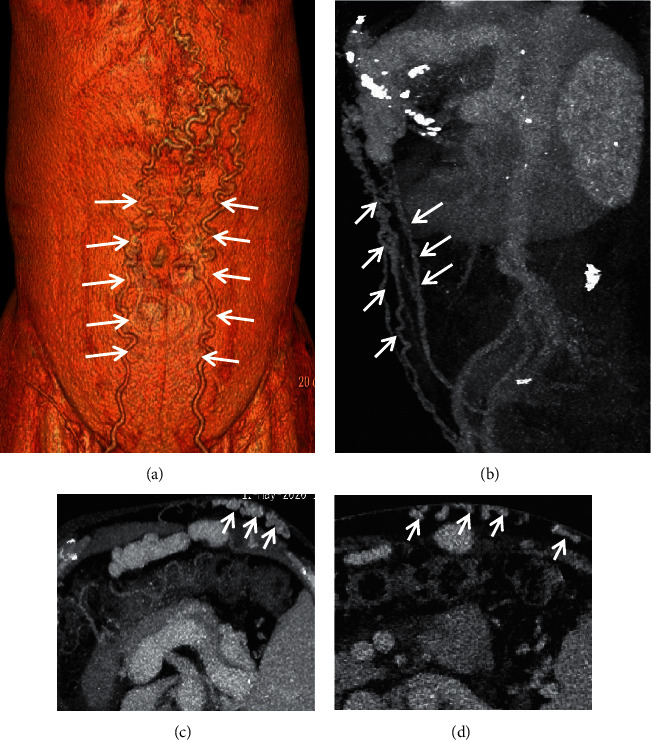
Abdominal wall varices. In a 65-year-old female with liver cirrhosis, the contrast-enhanced CT scan on the portal vein phase demonstrated that abdominal wall varices (white arrow) manifested as dilated, enhanced, and tortuous structures. (a) Three-dimensional reconstruction; (b) sagittal contrast-enhanced CT; (c, d) axial contrast-enhanced CT.
6.7. Spontaneous Splenorenal Shunt
SSRS often refers to abnormally dilated vessels connecting between the splenic vein and renal vein [14]. Besides, gastrorenal shunt, which refers to spontaneously abnormal communication between the gastric vein and renal vein [4], should be attributed to SSRS. SSRS may worsen liver function and increase the risk of hepatic encephalopathy and death in liver cirrhosis [9]. On the portal vein phase of contrast-enhanced CT scan, SSRS manifests as enhancement of abnormally dilated vessels originating from the splenic or gastric veins to the left renal vein [22] (Figures 9 and 10).
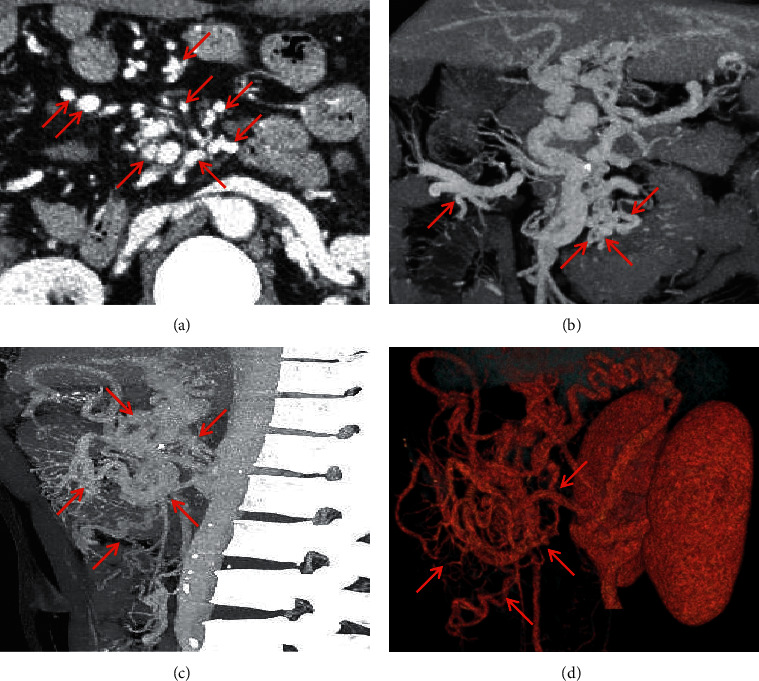
Figure 9.
Splenorenal shunt. In a 62-year-old female with liver cirrhosis, the axial contrast-enhanced CT scan on the portal vein phase demonstrated that splenorenal shunt (red arrow) manifested as enhancement of abnormally dilated vessels originating from the splenic vein to the left renal vein.
Figure 10.
Gastrorenal shunt. A 62-year-old male with a four-year history of unexplained liver cirrhosis presented with recurrent hematemesis. The contrast-enhanced CT scan on the portal vein phase demonstrated that gastrorenal shunt (white arrow) manifested as enhancement of abnormally dilated vessels originating from the gastric vein to the left renal vein. (a) Three-dimensional reconstruction; (b) coronal contrast-enhanced CT.
6.8. Retzius Vein
The Retzius vein refers to collateral vessels between the superior or inferior mesenteric vein and inferior vena cava in the retroperitoneum [47]. The Retzius vein is a number of small and easily neglected vessels in normal conditions and may gradually dilate when portal hypertension occurs. The blood of the Retzius vein mainly comes from the pancreaticoduodenal vein, ileocolic vein, lumbar vein, and gonadal vein [69]. On the portal vein phase of contrast-enhanced CT scan, the Retzius vein manifests as tortuously dilated vessels in the retroperitoneum (Figure 11).
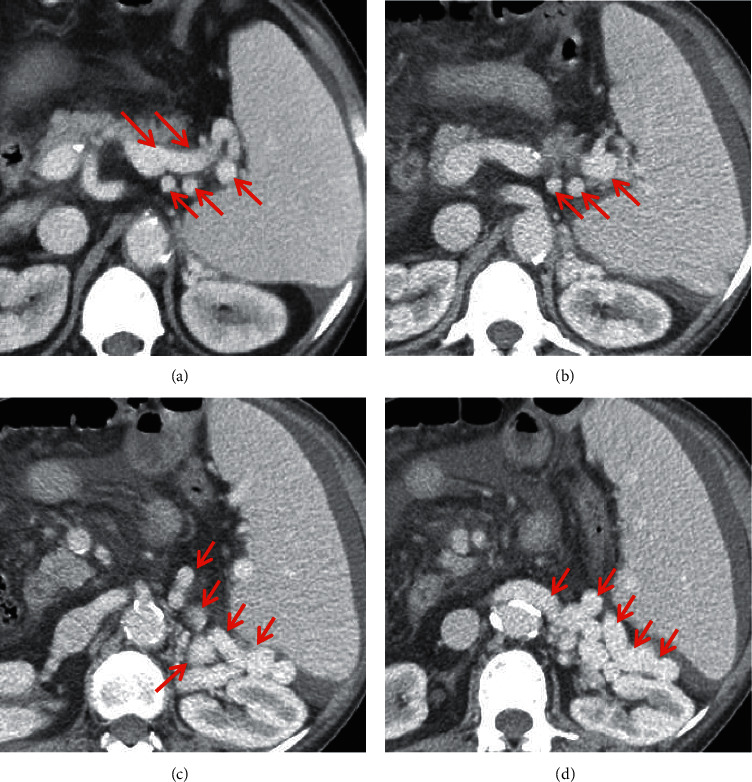
Figure 11.
Retzius vein. A 48-year-old male patient with an eleven-year history of alcoholic-related liver cirrhosis presented with hematochezia. The contrast-enhanced CT scan on the portal vein phase demonstrated that the Retzius vein (red arrow) manifested as tortuously dilated vessels in the retroperitoneum in the portal vein phase. (a) Axial contrast-enhanced CT; (b) coronal contrast-enhanced CT; (c) sagittal contrast-enhanced CT; (d) three-dimensional reconstruction.
6.9. Rectal Varices
Rectal varices, which refer to dilated rectal veins, originate from the anastomosis vessels of the superior rectal vein and the middle or inferior rectal veins in the lower rectum [70]. The inferior mesenteric vein is a feeding vessel for rectal varices, and rectal varices mainly flow into the internal iliac vein via the middle and/or inferior rectal vein [71]. Rectal variceal bleeding is rare, with an incidence of 0.45% to 3.6%, but it is often lethal [72]. On the portal vein phase of contrast-enhanced CT scan, rectal varices manifest as dilated and enhanced veins in the lower rectum.
7. Conclusions
SPSS mainly includes the esophagogastric venous plexus, paraumbilical venous plexus, retroperitoneal venous plexus, and rectal venous plexus, which manifests as tortuous, dilated, and enhanced vessels on the portal vein phase of contrast-enhanced CT scan. CT images are helpful for clinicians to diagnose different types of SPSS.
Conflicts of Interest
The authors declare no conflicts of interest.
Authors' Contributions
Xingshun Qi was involved in conceptualization. Fangfang Yi, Xiaozhong Guo, Qing-Lei Zeng, Benqiang Yang, Yanglan He, and Xingshun Qi were involved in methodology. Xiaozhong Guo, Qing-Lei Zeng, Benqiang Yang, Ankur Arora, and Xingshun Qi were involved in validation. Fangfang Yi, Xiaozhong Guo, Shanshan Yuan, and Xingshun Qi conducted formal analysis. Fangfang Yi and Xingshun Qi were involved in writing—original draft. Fangfang Yi, Xiaozhong Guo, Qing-Lei Zeng, Yanglan He, and Xingshun Qi were involved in writing—review and editing. Xingshun Qi was involved in supervision. Fangfang Yi, Xiaozhong Guo, and Qing-Lei Zeng have contributed equally.
References
- 1.Praktiknjo M., Simón-Talero M., Römer J., et al. Total area of spontaneous portosystemic shunts independently predicts hepatic encephalopathy and mortality in liver cirrhosis. Journal of Hepatology . 2020;72(6):1140–1150. doi: 10.1016/j.jhep.2019.12.021. [DOI] [PubMed] [Google Scholar]
- 2.Vidal-Gonzalez J., Quiroga S., Simon-Talero M., Genesca J. Spontaneous portosystemic shunts in liver cirrhosis: new approaches to an old problem. Therapeutic Advances in Gastroenterology . 2020;13 doi: 10.1177/1756284820961287.175628482096128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guillaume M., Bureau C. Should the presence of spontaneous portosystemic shunts be implemented to the model for end-stage liver disease score for a better prediction of outcome? Gastroenterology . 2018;154(6):1569–1571. doi: 10.1053/j.gastro.2018.03.035. [DOI] [PubMed] [Google Scholar]
- 4.Wind P., Alves A., Chevallier J. M., et al. Anatomy of spontaneous splenorenal and gastrorenal venous anastomoses. Review of the literature. Surgical and Radiologic Anatomy . 1998;20(2):129–134. doi: 10.1007/s00276-998-0129-8. [DOI] [PubMed] [Google Scholar]
- 5.Moreau R. VEGF-induced angiogenesis drives collateral circulation in portal hypertension. Journal of Hepatology . 2005;43(1):6–8. doi: 10.1016/j.jhep.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Dajti E., Renzulli M., Colecchia A., et al. Size and location of spontaneous portosystemic shunts predict the risk of decompensation in cirrhotic patients. Digestive and Liver Disease . 2022;54(1):103–110. doi: 10.1016/j.dld.2020.12.114. [DOI] [PubMed] [Google Scholar]
- 7.Simón-Talero M., Roccarina D., Martínez J., et al. Association between portosystemic shunts and increased complications and mortality in patients with cirrhosis. Gastroenterology . 2018;154(6):1694–1705. doi: 10.1053/j.gastro.2018.01.028. [DOI] [PubMed] [Google Scholar]
- 8.Henseler K. P., Pozniak M. A., Lee F. T., Winter T. C. Three-dimensional CT angiography of spontaneous portosystemic shunts. RadioGraphics . 2001;21(3):691–704. doi: 10.1148/radiographics.21.3.g01ma14691. [DOI] [PubMed] [Google Scholar]
- 9.Yi F., Guo X., Wang L., et al. Impact of spontaneous splenorenal shunt on liver volume and long-term survival of liver cirrhosis. Journal of Gastroenterology and Hepatology . 2021;36(6):1694–1702. doi: 10.1111/jgh.15386. [DOI] [PubMed] [Google Scholar]
- 10.Riggio O., Efrati C., Catalano C., et al. High prevalence of spontaneous portal-systemic shunts in persistent hepatic encephalopathy: a case-control study. Hepatology . 2005;42(5):1158–1165. doi: 10.1002/hep.20905. [DOI] [PubMed] [Google Scholar]
- 11.Yu N. C., Margolis D., Hsu M., Raman S. S., Lu D. S. K. Detection and grading of esophageal varices on liver CT: comparison of standard and thin-section multiplanar reconstructions in diagnostic accuracy. American Journal of Roentgenology . 2011;197(3):643–649. doi: 10.2214/ajr.10.5458. [DOI] [PubMed] [Google Scholar]
- 12.Nardelli S., Riggio O., Turco L., et al. Relevance of spontaneous portosystemic shunts detected with CT in patients with cirrhosis. Radiology . 2021;299(1):133–140. doi: 10.1148/radiol.2021203051. [DOI] [PubMed] [Google Scholar]
- 13.Cho K. C., Patel Y. D., Wachsberg R. H., Seeff J. Varices in portal hypertension: evaluation with CT. RadioGraphics . 1995;15(3):609–622. doi: 10.1148/radiographics.15.3.7624566. [DOI] [PubMed] [Google Scholar]
- 14.Achiwa S., Hirota S., Kako Y., Takaki H., Kobayashi K., Yamakado K. Radiological anatomy of spontaneous splenorenal shunts in patients with chronic liver disease. Japanese Journal of Radiology . 2017;35(4):206–214. doi: 10.1007/s11604-017-0623-1. [DOI] [PubMed] [Google Scholar]
- 15.Tarantino G., Citro V., Conca P., et al. What are the implications of the spontaneous spleno-renal shunts in liver cirrhosis? BMC Gastroenterology . 2009;9(1):p. 89. doi: 10.1186/1471-230x-9-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao L. Q., He W., Chen G. Characteristics of paraesophageal varices: a study with 64-row multidetector computed tomograghy portal venography. World Journal of Gastroenterology . 2008;14(34):5331–5335. doi: 10.3748/wjg.14.5331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarin S. K., Lahoti D., Saxena S. P., Murthy N. S., Makwana U. K. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology . 1992;16(6):1343–1349. doi: 10.1002/hep.1840160607. [DOI] [PubMed] [Google Scholar]
- 18.Arora A., Rajesh S., Meenakshi Y. S., Sureka B., Bansal K., Sarin S. K. Spectrum of hepatofugal collateral pathways in portal hypertension: an illustrated radiological review. Insights into Imaging . 2015;6(5):559–572. doi: 10.1007/s13244-015-0419-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moubarak E., Bouvier A., Boursier J., et al. Portosystemic collateral vessels in liver cirrhosis: a three-dimensional MDCT pictorial review. Abdominal Radiology . 2012;37(5):746–766. doi: 10.1007/s00261-011-9811-0. [DOI] [PubMed] [Google Scholar]
- 20.Qi X., Qi X., Zhang Y., et al. Prevalence and clinical characteristics of spontaneous splenorenal shunt in liver cirrhosis: a retrospective observational study based on contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) scans. Medical Science Monitor . 2017;23:2527–2534. doi: 10.12659/msm.901656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He C., Lv Y., Wang Z., et al. Association between non-variceal spontaneous portosystemic shunt and outcomes after TIPS in cirrhosis. Digestive and Liver Disease . 2018;50(12):1315–1323. doi: 10.1016/j.dld.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 22.Saks K., Jensen K. K., McLouth J., et al. Influence of spontaneous splenorenal shunts on clinical outcomes in decompensated cirrhosis and after liver transplantation. Hepatology Communications . 2018;2(4):437–444. doi: 10.1002/hep4.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allard M. A., Akamatsu N., Kokudo T., et al. Clinical significance of spontaneous portosystemic shunts in living donor liver transplantation. Liver Transplantation . 2021;27(1):77–87. doi: 10.1016/j.dld.2020.11.020. [DOI] [PubMed] [Google Scholar]
- 24.Rathi S., Brocco S., Formentin C., et al. Spontaneous portosystemic shunts in cirrhosis: detection, implications, and clinical associations. Digestive and Liver Disease . 2021;53(11):1468–1475. doi: 10.1016/j.dld.2020.11.020. [DOI] [PubMed] [Google Scholar]
- 25.Renzulli M., Dajti E., Ierardi A. M., et al. Validation of a standardized CT protocol for the evaluation of varices and porto-systemic shunts in cirrhotic patients. European Journal of Radiology . 2022;147 doi: 10.1016/j.ejrad.2021.110010.110010 [DOI] [PubMed] [Google Scholar]
- 26.Jakab S. S., Garcia-Tsao G. Screening and surveillance of varices in patients with cirrhosis. Clinical Gastroenterology and Hepatology . 2019;17(1):26–29. doi: 10.1016/j.cgh.2018.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lv Y., Yang Z., Liu L., et al. Early TIPS with covered stents versus standard treatment for acute variceal bleeding in patients with advanced cirrhosis: a randomised controlled trial. The Lancet Gastroenterology and Hepatology . 2019;4(8):587–598. doi: 10.1016/s2468-1253(19)30090-1. [DOI] [PubMed] [Google Scholar]
- 28.An Y., Xu X., Ren T., et al. Adherence to non-selective beta blockers for prevention of variceal bleeding in cirrhotic patients. International Journal of General Medicine . 2021;14:6713–6724. doi: 10.2147/ijgm.s326192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mukund A., Chalamarla L. K., Singla N., Shasthry S. M., Sarin S. K. Intractable hepatic encephalopathy in cirrhotic patients: mid-term efficacy of balloon-occluded retrograde portosystemic shunt obliteration. European Radiology . 2020;30(6):3462–3472. doi: 10.1007/s00330-019-06644-4. [DOI] [PubMed] [Google Scholar]
- 30.Qi X., Liu L., Bai M., et al. Transjugular intrahepatic portosystemic shunt in combination with or without variceal embolization for the prevention of variceal rebleeding: a meta-analysis. Journal of Gastroenterology and Hepatology . 2014;29(4):688–696. doi: 10.1111/jgh.12391. [DOI] [PubMed] [Google Scholar]
- 31.Tripathi D., Bureau C. Prophylactic embolization of large spontaneous portosystemic shunts with tips: a panacea for post tips hepatic encephalopathy? Hepatology . 2022 doi: 10.1002/hep.32525. [DOI] [PubMed] [Google Scholar]
- 32.Lv Y., Chen H., Luo B., et al. Concurrent large spontaneous portosystemic shunt embolization for the prevention of overt hepatic encephalopathy after tips: a randomized controlled trial. Hepatology . 2022 doi: 10.1002/hep.32453. [DOI] [PubMed] [Google Scholar]
- 33.Golse N., Bucur P. O., Faitot F., et al. Spontaneous splenorenal shunt in liver transplantation: results of left renal vein ligation versus renoportal anastomosis. Transplantation . 2015;99(12):2576–2585. doi: 10.1097/tp.0000000000000766. [DOI] [PubMed] [Google Scholar]
- 34.Takayasu K., Moriyama N., Shima Y., et al. Sonographic detection of large spontaneous spleno-renal shunts and its clinical significance. British Journal of Radiology . 1984;57(679):565–570. doi: 10.1259/0007-1285-57-679-565. [DOI] [PubMed] [Google Scholar]
- 35.Reeder S. B. Portosystemic shunts: should we pay closer attention with cross-sectional imaging? Radiology . 2021;299(1):141–142. doi: 10.1148/radiol.2021204282. [DOI] [PubMed] [Google Scholar]
- 36.Praktiknjo M., Torner J., Simón-Talero M., et al. Reply to: “Definition of SPSS: we need to speak the same language”: computer-assisted image processing for better quantification. Journal of Hepatology . 2020;73(2):464–465. doi: 10.1016/j.jhep.2020.04.012. [DOI] [PubMed] [Google Scholar]
- 37.Zhang C. X., Xu J. M., Li J. B., et al. Predict esophageal varices via routine trans-abdominal ultrasound: a design of classification analysis model. Journal of Gastroenterology and Hepatology . 2016;31(1):194–199. doi: 10.1111/jgh.13045. [DOI] [PubMed] [Google Scholar]
- 38.Deng H., Qi X., Zhang Y., Peng Y., Li J., Guo X. Diagnostic accuracy of contrast-enhanced computed tomography for esophageal varices in liver cirrhosis: a retrospective observational study. Journal of Evidence-Based Medicine . 2017;10(1):46–52. doi: 10.1111/jebm.12226. [DOI] [PubMed] [Google Scholar]
- 39.Deng H., Qi X., Guo X. Computed tomography for the diagnosis of varices in liver cirrhosis: a systematic review and meta-analysis of observational studies. Postgraduate Medical Journal . 2017;129(3):318–328. doi: 10.1080/00325481.2017.1241664. [DOI] [PubMed] [Google Scholar]
- 40.Li Q., Wang R., Guo X., et al. Contrast-enhanced CT may be a diagnostic alternative for gastroesophageal varices in cirrhosis with and without previous endoscopic variceal therapy. Gastroenterology Research and Practice . 2019;2019:15. doi: 10.1155/2019/6704673.6704673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lipp M. J., Broder A., Hudesman D., et al. Detection of esophageal varices using CT and MRI. Digestive Diseases and Sciences . 2011;56(9):2696–2700. doi: 10.1007/s10620-011-1660-8. [DOI] [PubMed] [Google Scholar]
- 42.Giordano C., Klingler A. Quick recertification series. Journal of the American Academy of Physician Assistants . 2011;24(7):53–54. doi: 10.1097/01720610-201107000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Li Q., Guo X., Feng J., et al. Risk factors for esophageal collateral veins in cirrhosis with and without previous endoscopic esophageal variceal therapy. Canadian Journal of Gastroenterology and Hepatology . 2022;2022:13. doi: 10.1155/2022/6666791.6666791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kraja B., Mone I., Akshija I., Kocollari A., Prifti S., Burazeri G. Predictors of esophageal varices and first variceal bleeding in liver cirrhosis patients. World Journal of Gastroenterology . 2017;23(26):4806–4814. doi: 10.3748/wjg.v23.i26.4806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li Q. Q., Li H. Y., Bai Z. H., Philips C. A., Guo X. Z., Qi X. S. Esophageal collateral veins in predicting esophageal variceal recurrence and rebleeding after endoscopic treatment: a systematic review and meta-analysis. Gastroenterol Repeprt . 2020;8(5):355–361. doi: 10.1093/gastro/goaa004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lupescu I., Masala N., Capsa R., Campeanu N., Georgescu S. A. CT and MRI of acquired portal venous system anomalies. Journal of Gastrointestinal and Liver Diseases: JGLD . 2006;15(4):393–398. [PubMed] [Google Scholar]
- 47.Ibukuro K., Tsukiyama T., Mori K., Inoue Y. Veins of retzius at CT during arterial portography: anatomy and clinical importance. Radiology . 1998;209(3):793–800. doi: 10.1148/radiology.209.3.9844676. [DOI] [PubMed] [Google Scholar]
- 48.Lee S. Y., Kuo H. T., Peng M. J., et al. Azygos vein varix mimicking mediastinal mass in a patient with liver cirrhosis. Chest . 2005;127(2):661–664. doi: 10.1378/chest.127.2.661. [DOI] [PubMed] [Google Scholar]
- 49.Ohtomo K., Itai Y., Makita K., et al. Portosystemic collaterals on MR imaging. Journal of Computer Assisted Tomography . 1986;10(5):751–755. doi: 10.1097/00004728-198609000-00007. [DOI] [PubMed] [Google Scholar]
- 50.He C., Qi X., Han G. Large paraesophageal varices causing recurrent hepatic encephalopathy. The American Journal of the Medical Sciences . 2014;348(6):p. 512. doi: 10.1097/maj.0b013e318290c134. [DOI] [PubMed] [Google Scholar]
- 51.Ishikawa T., Ushiki T., Mizuno K. I., et al. CT-maximum intensity projection is a clinically useful modality for the detection of gastric varices. World Journal of Gastroenterology . 2005;11(47):7515–7519. doi: 10.3748/wjg.v11.i47.7515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vianna A., Hayes P. C., Moscoso G., et al. Normal venous circulation of the gastroesophageal junction. Gastroenterology . 1987;93(4):876–889. doi: 10.1016/0016-5085(87)90453-7. [DOI] [PubMed] [Google Scholar]
- 53.Adithan S., Venkatesan B., Sundarajan E., Kate V., Kalayarasan R. Color doppler evaluation of left gastric vein hemodynamics in cirrhosis with portal hypertension and its correlation with esophageal varices and variceal bleed. Indian Journal of Radiology and Imaging . 2010;20(4):289–293. doi: 10.4103/0971-3026.73541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Willmann J. K., Weishaupt D., Böhm T., et al. Detection of submucosal gastric fundal varices with multi-detector row CT angiography. Gut . 2003;52(6):886–892. doi: 10.1136/gut.52.6.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhu K., Meng X., Pang P., et al. Gastric varices in patients with portal hypertension: evaluation with multidetector row CT. Journal of Clinical Gastroenterology . 2010;44(5):e108–e115. doi: 10.1097/MCG.0b013e3181c115c6. [DOI] [PubMed] [Google Scholar]
- 56.Zhou H. Y., Chen T. W., Zhang X. M., et al. Diameters of left gastric vein and its originating vein on magnetic resonance imaging in liver cirrhosis patients with hepatitis B: association with endoscopic grades of esophageal varices. Hepatology Research . 2014;44(10):E110–E117. doi: 10.1111/hepr.12246. [DOI] [PubMed] [Google Scholar]
- 57.Hino S., Kakutani H., Ikeda K., et al. Hemodynamic assessment of the left gastric vein in patients with esophageal varices with color doppler EUS: factors affecting development of esophageal varices. Gastrointestinal Endoscopy . 2002;55(4):512–517. doi: 10.1067/mge.2002.122333. [DOI] [PubMed] [Google Scholar]
- 58.Song B., Li C., Liu Z., Zhao L., Bai W. Evaluation on the anatomy and variation of left gastric vein in normal adults with MSCTA. Chinese Journal of Medical Imaging Technology . 2011;27(4) [Google Scholar]
- 59.Kang H. K., Jeong Y. Y., Choi J. H., et al. Three-dimensional multi-detector row CT portal venography in the evaluation of portosystemic collateral vessels in liver cirrhosis. RadioGraphics . 2002;22(5):1053–1061. doi: 10.1148/radiographics.22.5.g02se011053. [DOI] [PubMed] [Google Scholar]
- 60.Horton K. M., Fishman E. K. Paraumbilical vein in the cirrhotic patient: imaging with 3D CT angiography. Abdominal Imaging . 1998;23(4):404–408. doi: 10.1007/s002619900369. [DOI] [PubMed] [Google Scholar]
- 61.Marenco S., Giannini E. G., Savarino V. Patent paraumbilical vein-induced hepatic encephalopathy. Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association . 2010;8(10):p. A28. doi: 10.1016/j.cgh.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 62.Singla V., Galwa R., Saxena A., Khandelwal N. Cruveilhier baumgarten syndrome with giant paraumbilical vein. Journal of Postgraduate Medicine . 2008;54(4):328–329. doi: 10.4103/0022-3859.43520. [DOI] [PubMed] [Google Scholar]
- 63.Aagaard J., Jensen L., Sørensen T., Christensen U., Burcharth F. Recanalized umbilical vein in portal hypertension. American Journal of Roentgenology . 1982;139(6):1107–1110. doi: 10.2214/ajr.139.6.1107. [DOI] [PubMed] [Google Scholar]
- 64.Qi X., Han G. Abdominal-wall varices in the budd–chiari syndrome. New England Journal of Medicine . 2014;370(19):p. 1829. doi: 10.1056/nejmicm1308567. [DOI] [PubMed] [Google Scholar]
- 65.Giambelluca D., Caruana G., Cannella R., Picone D., Midiri M. The “caput medusae” sign in portal hypertension. Abdominal Radiology . 2018;43(9):2535–2536. doi: 10.1007/s00261-018-1493-4. [DOI] [PubMed] [Google Scholar]
- 66.Sheth S., Ebert M. D., Fishman E. K. Superior vena cava obstruction evaluation with MDCT. American Journal of Roentgenology . 2010;194(4):W336–W346. doi: 10.2214/ajr.09.2894. [DOI] [PubMed] [Google Scholar]
- 67.Sonin A. H., Mazer M. J., Powers T. A. Obstruction of the inferior vena cava: a multiple-modality demonstration of causes, manifestations, and collateral pathways. RadioGraphics . 1992;12(2):309–322. doi: 10.1148/radiographics.12.2.1561419. [DOI] [PubMed] [Google Scholar]
- 68.Li H., Wang R., Méndez-Sánchez N., Peng Y., Guo X., Qi X. Impact of spider nevus and subcutaneous collateral vessel of chest/abdominal wall on outcomes of liver cirrhosis. Archives of Medical Science . 2019;15(2):434–448. doi: 10.5114/aoms.2018.74788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sharma M., Rameshbabu C. S. Collateral pathways in portal hypertension. Journal of Clinical and Experimental Hepatology . 2012;2(4):338–352. doi: 10.1016/j.jceh.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kovacs T. O. G., Jensen D. M. Varices: esophageal, gastric, and rectal. Clinics in Liver Disease . 2019;23(4):625–642. doi: 10.1016/j.cld.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 71.Yoshino K., Imai Y., Nakazawa M., et al. Therapeutic strategy for patients with bleeding rectal varices complicating liver cirrhosis. Hepatology Research . 2014;44(11):1088–1094. doi: 10.1111/hepr.12232. [DOI] [PubMed] [Google Scholar]
- 72.Shudo R., Yazaki Y., Sakurai S., Uenishi H., Yamada H., Sugawara K. Clinical study comparing bleeding and nonbleeding rectal varices. Endoscopy . 2002;34(3):189–194. doi: 10.1055/s-2002-20289. [DOI] [PubMed] [Google Scholar]


