Abstract
How to activate adaptive coping strategies has an important and practical meaning for the quality of life of people living with HIV (PLHIV); however, few studies have focused on the effects of sleep disturbances and HIV-related physical symptoms on coping strategies. The specific relationships among coping strategies, sleep disturbances and HIV-related physical symptoms were unknown. We performed a path analysis to examine the proposed model of relationships among sleep disturbances, physical symptoms, and coping strategies. A convenience sample of 69 HIV-positive Asian Americans in San Francisco, Los Angeles, and New York City were recruited and data were collected on demographics, sleep disturbances, HIV-related physical symptoms, and coping strategies. Sleep disturbances directly affect maladaptive coping (β = 0.34), and physical symptoms directly affect adaptive coping (β = 0.30) and maladaptive coping (β = 0.24). Interventions designed to decrease sleep disturbances and physical symptoms should be developed to enhance adaptive coping and reduce maladaptive coping among Asian Americans with HIV.
Keywords: HIV, symptoms, sleep disturbance, coping strategies, Asian Americans
Introduction
Asians American is the rapidly growing population in the United States (U.S.) (Budiman, Cilluffo, & Ruiz, 2019), which California accounts for more than ¼ of the population (26.57%), and Asian Americans accounts for 7.6% of the New York state population in 2018 census (U.S. Census Bureau, 2019). Among different ethnic groups in the U.S., Asian Americans are the only ethnic group present a continuous increase in HIV infection which increase from 4.9 per 100,000 people in 2011 to 5.5 per 100,000 people in 2016 (Kim & Aronowitz T, 2019). From the most recent report on Asian Americans living with HIV in the United States in 2018, Asian Americans living with HIV/AIDS accounted for approximately 2% of the people living with HIV (PLHIV) in the US and dependent areas (Centers for Disease Control and Prevention). HIV-infected Asian Americans are the most understudied ethnic minority group in the United States (Kim & Aronowitz, 2019). With the advent of antiretroviral therapy (ART), HIV has become a chronic condition (Teeraananchai et al., 2017), and posing new challenges for PLHIV. Apart from psychological stress and ethnic differences, most PLHIV experience multiple physical symptoms, including fatigue, weakness and pain that also have a negative impact on medication adherence and quality of life (Zhu et al., 2019; Zhu et al., 2019; Lindayani et al., 2018; Kacanek et al., 2015). However, for Asian Americans, several studies focused on the social and psychological stress aspect of Asian Americans (Chen et al., 2015; Huang et al., 2020), such as acculturation and mental stress, studies focused on physical symptoms, coping strategies and sleep disturbances were limited.
Sleep disturbance, another common complaint among PLHIV, is described as difficulty falling asleep and achieving deep sleep, awakening early, or unrefreshing sleep (Lee et al., 2012; Chen et al., 2013b). The prevalence rates for sleep disturbances range from 47% to 73% in PLHIV (Allavena et al., 2016; Gutierrez et al., 2019; Wu et al., 2015). Sleep disturbances, physical symptoms and psychological status interact with each other; thus, sleep disturbances may be caused by depression, anxiety and physical symptoms such as pain, fatigue, and in turn exacerbate these symptoms in PLHIV (Robbins et al., 2004; Huang et al., 2017; Ren et al., 2018).
Coping strategies can help PLHIV effectively manage their HIV-related discomforts (Finkelstein-Fox et al., 2019). Coping strategies are often classified as either adaptive coping (including active coping, planning, suppression of competing activities, religious adherence, seeking emotional support and social support as well as accepting the illness), and maladaptive coping (including self-distraction, coping with alcohol and substance use, and disengagement and denial of their illness) (Carver et al., 1989; Safren et al., 2002). Research on coping strategies among PLHIV have revealed that adaptive coping strategies are associated with better psychological outcomes that can decrease depression (Fauk et al., 2020), posttraumatic stress symptoms (Yu et al., 2017; Golub et al., 2013), and anxiety (Fekete et al., 2016; Willie et al., 2016). Adaptive coping has also been linked to elevated CD4 counts and viral load suppression (Kremer et al., 2015; Earnshaw et al., 2018). PLHIV who use adaptive coping strategies are more likely to adhere to ART (Guy et al., 2018; Poteat & Lassiter, 2019), use condoms more often (Evans et al., 2013), decrease substance use, and quit smoking (Skalski et al., 2019). In contrast, maladaptive coping strategies have been found to be associated with an increase in disease progression (Earnshaw et al., 2018), present with anxiety and depression (Seffren et al., 2018), as well as a high rate of risk behaviors and alcohol use (Wardell et al., 2018; Weiss et al., 2017).
Obviously, the different health-related outcomes depend on the coping strategies that PLHIV employ. Thus, it is important to explore the factors that can predict coping strategies. Researchers have examined the potential psychosocial causes of coping strategies in PLHIV and have often reported coping strategies as a mediating role of HIV-related stigma and psychological distress (Rachel et al., 2019; Meanley et al.,2019; Zhi et al., 2018) and of ART treatment (Earnshaw et al., 2018), social support, quality of life (Shrestha et al., 2019) and adherence to ART (Guy et al., 2018). In addition, other studies have explored whether socioeconomics, educational level, and gender factors may also affect coping strategies (Dan et al., 2019; Ismail et al., 2017). These studies support that PLHIV use coping strategies to manage their psychosocial and personal stressors. Currently, there is a lack of understanding as on to how the physical symptoms, sleep disturbances and coping strategies interact among PLHIV, even fewer on HIV-infected Asian Americans. As Asian American PLHIV is one of the hardest reach populations in the United States, therefore, in this study, we evaluated the activation effect of sleep disturbances and physical symptoms on coping strategies among Asian American PLHIV.
Theoretical Framework
We formulated a theory of stress and coping to build our hypothesis that described the process of coping activated by stressors (Lazarus & Folkman, 1984). The stressors are the situations or events that PLHIV perceive to be threatening to their physical, psychological, or social health (Lazarus & Folkman, 1984). Based on this, we proposed a study model that links the pathway between physical symptoms, sleep disturbances and coping strategies. In this model, we hypothesized that: (1) sleep disturbances can directly impact both adaptive and maladaptive coping, (2) physical symptoms can directly impact both adaptive and maladaptive coping, and (3) sleep disturbance and physical symptoms interact with each other.
Methods
Sample, settings, and procedures
There were two phases of the study: (1) Phase 1. From January to June 2013, a convenience sample of 50 HIV-positive Asian Americans was recruited in two cities (San Francisco and New York City). Participants were recruited from the Asian & Pacific Islander Wellness Center (A&PI Wellness Center) in San Francisco, the Chinese-American Planning Council, Inc. (CPC), and the Asian/Pacific Islander Coalition on HIV/AIDS Community Health Center (APICHA Community Health Center) in New York City. (2) Phase 2. From September 2017 to January 2020, we recruited an additional 19 Asian American PLHIV from the CPC and Asian Pacific American AIDS Intervention Team (APAIT) in Los Angeles. The 69 participants were recruited by the convenience sampling methods.
The relevant institutional ethical review boards approved this study (#18–000025). The study inclusion criteria were as follows: (a) self-identified as Asian or Pacific Islanders, (b) confirmed HIV serostatus, (c) willing to participate in the survey, and (d) at least 18 years old. After securing written consent from the participants, we conducted cross-sectional audio computer-assisted self-interviews (ACASIs) or Research Electronic Data Captures (REDCap). All participants received a small reimbursement for their participation.
Measures
Participants completed a 60-minute ACASI/REDCap survey that consisted of standardized measures to assess demographics, sleep disturbances, physical symptoms and coping. These measures have been tested in Asian populations and have shown to have strong reliability and validity over time (Lee, 1992; Holzemer et al., 1999; Carver & Scheier, 1997).
Demographics:
We collected the participants’ ages, gender, marital status, ethnicity, educational level, employment status, immigrant status, years of living with HIV, HIV medications, and recent viral load.
Sleep disturbances:
We used the 21-item general sleep disturbance scale (GSDS) (Lee, 1992) to ask participants’ frequency of various sleep-related behaviors during the past week, from 0 (not at all) to 7 (every day). Items refer to the multidimensional aspects of falling asleep and maintaining sleep, as well as aspects of daytime functioning, such as feeling tired or sleepy during the day. The items were summed to obtain a total mean score ranging from 0 (no sleep disturbance) to 7 (frequent sleep disturbance). The overall Cronbach’s alpha reliability estimate for this sample was 0.93.
Physical symptoms:
We used the 64-item revised Sign and Symptom Checklist (SSC) (Holzemer et al., 1999) to assess the intensity of symptoms being experienced by PLHIV in the past 24 hours, including 0 (no/not at all), 1 (mild), 2 (moderate), or 3 (severe). Intensity was summed across symptoms; a higher score indicated higher HIV symptom intensity. In this study, the intensity of the 20 most severe physical symptoms were summed up as the physical symptoms scores. The physical symptoms included rectal bleeding, abdominal pain, chills, prominent leg veins, easy bruising, sore throat, tingling of arms, gas/bloating, rash, fever, day sweats, shortness of breath at rest or with activity, constipation, concern over weight gain, heart racing, chest pain, swollen feet, and itchy skin. The overall Cronbach’s alpha reliability estimate for this sample was 0.72.
Coping strategies:
We used the 28-item brief COPE inventory (Carver & Scheier, 1997) to measure participants’ adaptive and maladaptive coping strategies. Adaptive coping is characterized by active coping, planning, use of instrumental support, positive reframing, acceptance, use of emotional support, humor, and religion. Maladaptive coping is characterized by self-distraction, denial, venting, substance use, behavioral disengagement, and self-blame. Each item scored from one (“I haven’t been doing this at all”) to four (“I’ve been doing this a lot”). Higher scores reflected a higher tendency to implement the corresponding coping strategies. The overall Cronbach’s alpha reliability estimate for this sample was 0.87.
Data analysis
We conducted data analyses using SPSS 24.0 and AMOS 23.0 (IBM, Chicago, IL). In this study, the data meet the assumptions of normality (a one-sample Kolmogorov-Smirnov test did not show statistical significance). The continuous variables were expressed as means and standard deviations (SD). Categorical variables were expressed as proportions or percentages. We tested the hypothesized pathway in three steps. First, we conducted Pearson’s correlation analyses to examine the relationships among sleep disturbances, physical symptoms, and coping strategies. Second, we used pathway analysis to test the hypothesized pathway (Fig. 1) with the Bayesian analysis method. The following fit indices were used (Hu & Bentler, 1999): normed chi-square (χ2/df, 1.0±3.0, p >0.05), root mean square error of approximation (RMSEA <0.08), comparative fit index (CFI >0.9), and Tucker-Lewis Index (TLI, >0.9). Third, after controlling for key demographic variables (age, gender, marital status, ethnicity, educational level, employment status, immigrant status, years of living with HIV, HIV medications, and recent viral load), we removed the parameters that did not significantly differ from zero. We applied the bootstrap method (repeated 1,000 times) to obtain more stable and valid standard errors of the estimates of the direct and indirect effects of these factors to investigate the relationships between sleep disturbances, physical symptoms and coping strategies through different pathways. Standardized regression coefficient (β) and p values for β of direct, indirect, and total effects were identified and reported by path analysis. We replaced missing data using full information maximum likelihood; p <0.05 was considered significant.
Figure 1.
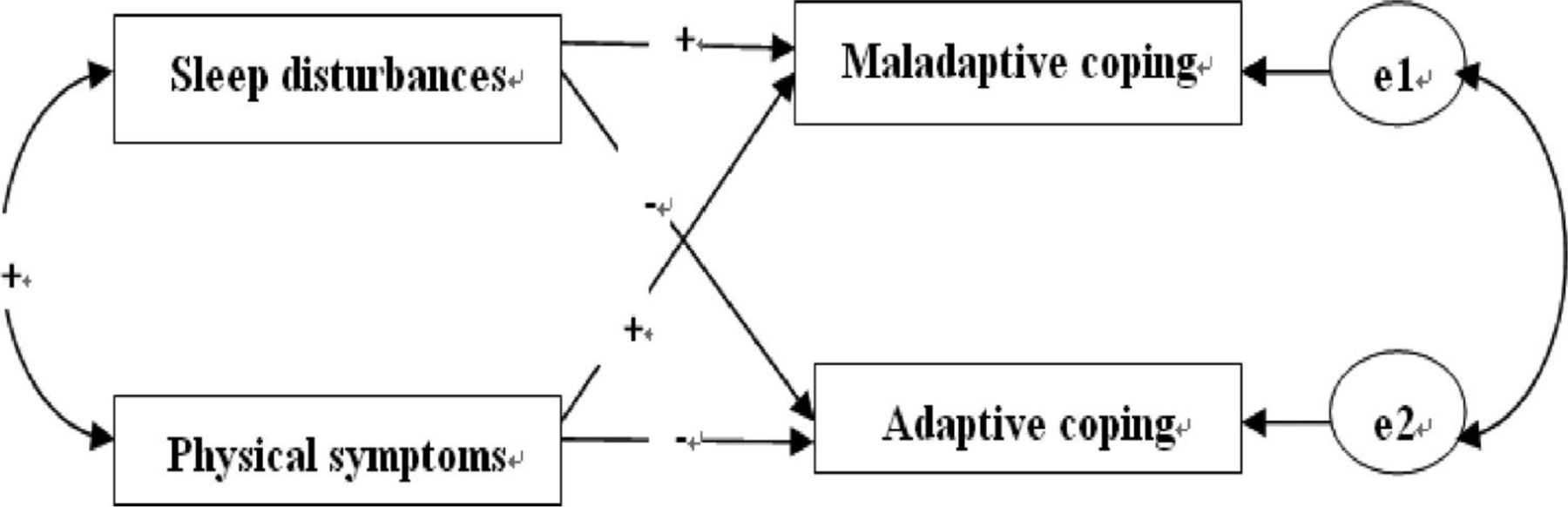
The hypothesized pathway.
Results
Descriptive and bivariate analysis
Demographic characteristics are presented in Table 1. Among the total sample of 69 HIV-infected Asian Americans, 78.30% were male (N=54), with a mean age of 51 years (SD =10.50, range = 31–72) and average years of living with HIV is 14.54 years (SD =6.33, range= 2–33). Results of bivariate analyses are summarized in Table 2. The results suggest that sleep disturbances, physical symptoms, adaptive and maladaptive coping are significantly correlated with each other.
Table 1.
Socio-demographic characteristics of participants (n = 69).
| Variables | n (%) |
|---|---|
| Gender | |
| Male | 54 (78.26%) |
| Female | 15 (21.74%) |
| Ethnicity | |
| Chinese | 35 (50.73%) |
| Philipino | 11 (15.95%) |
| Japanese | 3 (4.35%) |
| Malayscian | 5 (7.25%) |
| Indonesean | 1 (1.44%) |
| Vietnamese | 7 (10.14%) |
| Other | 7 (10.14%) |
| Are you an immigrants to the U.S | |
| Yes | 63 (91.30%) |
| No | 6 (8.70%) |
| Education level | |
| 11th grade or less | 33 (47.81%) |
| High school or GED | 20 (29.00%) |
| 2 years of college/AA degree/technical school training | 10 (14.49%) |
| College (BA or BS) | 5 (7.25%) |
| Doctorate/medical degree/law degree | 1 (1.44%) |
| Currently working status | |
| No | 49 (71.02%) |
| Part time | 10 (14.49%) |
| Full time | 10 (14.49%) |
| Marital statusa | |
| Married | 22 (31.88%) |
| Divorced | 7 (10.14%) |
| Single | 33 (47.83%) |
| Cohabited | 3 (4.35%) |
| Widowed | 2 (2.90%) |
| HIV medication | |
| No | 3 (4.30%) |
| Yes | 66 (95.70%) |
| Recent viral loada | |
| Undetectable | 50 (72.46%) |
| I know my viral load | 7 (10.14%) |
| Don’t know | 11 (15.94%) |
missing data.
Table 2.
Bivariate Correlation among variables.
| Sleep disorder | Physical symptom | Maladaptive coping | Adaptive coping | |
|---|---|---|---|---|
| Sleep disorder | / | 0.287b | 0.404b | −0.156 |
| Physical disorder | 0.287b | / | 0.347b | 0.302a |
| Maladaptive coping | 0.404b | 0.347b | / | 0.524b |
| Adaptive coping | −0.156 | 0.302a | 0.524b | / |
p < 0.05
p < 0.01.
Pathway analysis
After controlling for the participants’ demographic and disease characteristics and deleting the statistically insignificant relationship between sleep disturbances and adaptive coping (p >0.05), we found that most of the hypothesized relationships were significant and supported by the data; the final pathway fit well to the data (χ2(18) = 3.284, p = 0.05, RMSEA = 0.07, CFI = 0.94 & TLI = 0.85). The coefficients for all paths are shown in Figure 2. The standardized direct, indirect, and total estimates of the final model’s paths are shown in Table 3.
Figure 2.
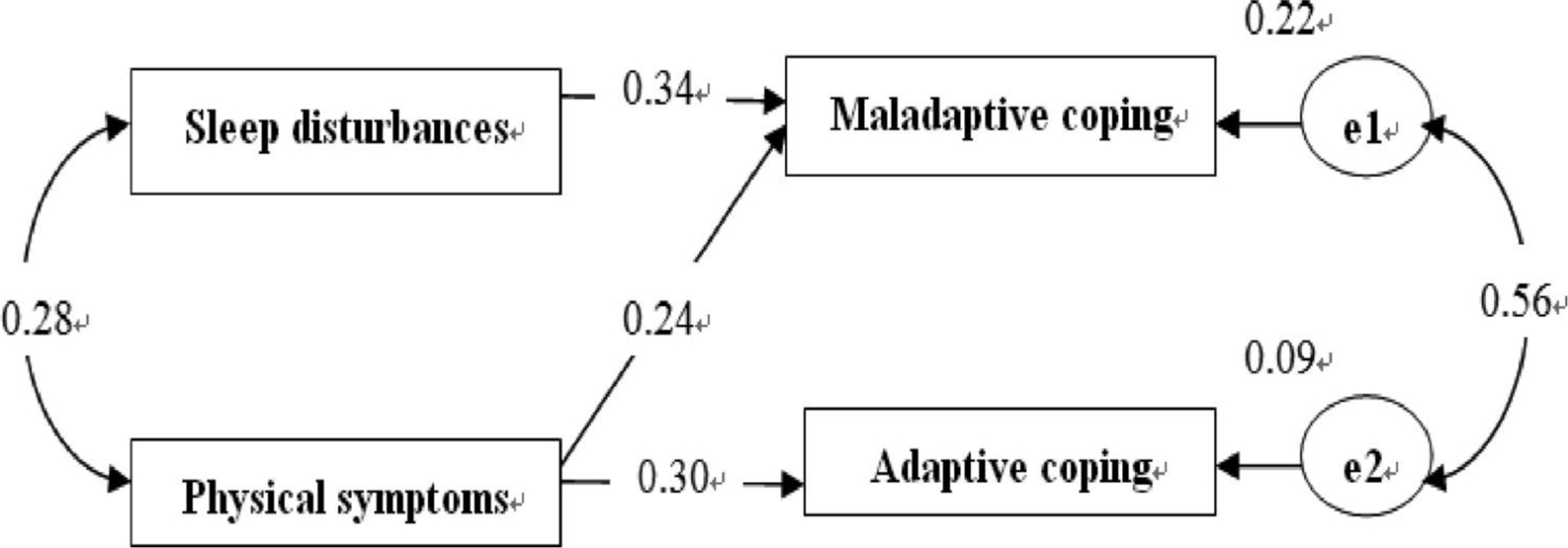
The final pathway.
Note: χ2/df = 3.824, p = 0.05; CFI = 0.94; TLI = 0.85; RMSEA = 0.07.
Table 3.
Effect coefficients of the final model.
| Endogenous variables | Predicting variables | Standardized direct effect β | Standardized indirect effect β | Standardized total effect β |
|---|---|---|---|---|
| Physical symptoms | Sleep disorder | 0.276a | / | 0.276a |
| Adaptive coping | 0.302a | / | −0.302a | |
| Maladaptive coping | 0.240a | 0.094a | −0.334a | |
| Sleep disorder | Physical symptoms | 0.276a | / | 0.276a |
| Adaptive coping | / | 0.083a | 0.083a | |
| Maladaptive coping | 0.340a | 0.066a | 0.406a |
p < 0.01.
Direct and indirect effects of factors affecting adaptive coping
According to the pathway, physical symptoms directly affect adaptive coping (β = 0.302). Although sleep disturbances had no significant direct effect on adaptive coping, they still had a positive total effect (β = 0.083), which can be seen to be mediated by the physical symptoms (indirect β = −0.083).
Direct and indirect effects of factors affecting maladaptive coping
Sleep disturbances directly affected maladaptive coping (β = 0.340) and had a positive total effect on maladaptive coping, which can be seen to be mediated by the physical symptoms (indirect β = 0.066). Physical symptoms had a similar path to maladaptive coping.
Discussion
Coping strategies adopted by PLHIV have very important practical applications because such strategies determine the PLHIV’s quality of life (Dan et al., 2019; Finkelstein-Fox et al., 2019). Studies have tended to emphasize the mediating role of coping strategies on health outcomes (Shrestha et al., 2019; Ye et al., 2018). Conversely, the present study’s perspective focused on the activation of participants’ adaptive and maladaptive coping strategies. To our knowledge, this is one of the initial reports to offer pathway evidence that links sleep disturbances, physical symptoms, and coping strategies among HIV-positive Asian Americans. Our models show that sleep disturbances and physical symptoms are important factors in the participants’ coping strategies. As such, implementing effective strategies in targeting sleep disturbances and physical symptoms can improve adaptive coping and reduce maladaptive coping among Asian American PLHIV.
Physical symptoms and sleep disturbances are common complaints among PLHIV (Wilson et al., 2016; Chen et al., 2013a). In the present study, specifically, self-reported sleep disturbances had a bi-directional association with the intensity of the physical symptoms, which ultimately led to different coping strategies. First, consistent with previous research (Babson et al., 2013), we observed that the PLHIV with more severe sleep disturbances suffered from greater self-reported HIV-related physical symptoms intensity and vice versa. Second, sleep disturbances may indirectly trigger the adaptive coping strategies by the mediation of physical symptoms. Third, for Asian American PLHIV, sleep disturbances can directly trigger maladaptive rather than adaptive coping strategies. That is, Asian American PLHIV suffering from sleep disturbances, difficulty falling or staying asleep, awakening too early, or unrefreshing sleep in combination with some daytime sleepiness or irritability (Chen et al., 2013a) tend to use maladaptive coping strategies to solve the problems, e.g., venting negative emotions, coping through alcohol and substance use and disengagement or denial of their illness (Carver & Scheier, 1997).
In the present study, similar to our previous study on Chinese PLHIV (Chen et al., 2020), we evaluated the physical symptoms of PLHIV as a whole and found that physical symptoms were a critical factor that can contribute to both adaptive and maladaptive coping strategies. The finding indicates that Asian American PLHIV tend to respond with all kinds of coping strategies when physical symptoms are presented (e.g., fatigue, shortness of breath, weakness, rash, tingling of arms). On one hand, participants presented with HIV-related somatic symptoms trigger the adaptive coping strategies, which are characterized by active coping, planning, use of instrumental support, positive reframing, acceptance, use of emotional support, humor, and religion (Carver & Scheier, 1997). These can all contribute to direct active coping (e.g., information-seeking and social support) to relieve somatic disorders. On the other hand, physical symptoms can also trigger the use of maladaptive coping strategies. For example, Asian American PLHIV can escape or ignore the physical discomforts by diverting attention or denial of the potential supports (Dan et al., 2019).
This present study highlights three potentially modifiable factors, including sleep disturbances physical symptoms, and coping strategies. This path analysis can also identify the potential pathways among these three factors. This finding highlights the significant roles of sleep disturbances and HIV-related physical symptoms on coping strategies. Healthcare providers should assess the sleep quality and physical symptoms of PLHIV to understand the potential coping strategies that were used during the HIV management.
Furthermore, this path analysis also shines new research directions for culturally relevant, integrated intervention programs that can enhancing sleep quality and decreasing physical symptoms, and lead to enacting adaptive coping and reducing maladaptive coping among PLHIV, especially for Asian Americans. Currently, very limited evidence is focusing on sleep and symptom management for Asian American PLHIV (CDC, 2013). The present study proved that sleep hygiene education can be effective, including setting up a regular bedtime and exercise, eliminating noise and clocks from the bedroom, regulating bedroom temperature, avoiding the use of sleeping pills, caffeine, alcohol, and naps during the day, engaging in relaxing activities before bed, limiting liquids, taking warm baths, and using the bedroom only for sleep (Chen et al., 2013a), as well as cognitive-behavioral therapy for insomnia (e.g., sleep restriction therapy and stimulus control therapy; Taibi, 2013). Whether these interventions are suitable to improve sleep disturbances among Asian American PLHIV warrants further exploration in future studies.
Limitations
There are several limitations to this study. First, its cross-sectional nature limited casual inference, two data collection phases, and the small sample sizes of Asian Americans PLHIV participants potentially limited the interpretation of causality among sleep disturbances, physical symptoms and coping strategies, and generalizability. Asian Americans PLHIV, however, are one of the hardest-to-recruit populations and this paper will be one of the first few articles focusing on this population. Second, in this analysis, all variables were measured using self-report scales, which may lead to some potential bias (e.g., social desirability response and error in recall) in estimating associations. Thus, future research should include longitudinal design to examine how the relationships among these variables unfold over time. Last, to assess participants’ objective sleep data (e.g., total sleep time, wake after sleep onset) the use of biological and behavioral indicators should be considered with self-reported surveys, such as sleep-awake monitoring devices (Chen et al., 2013b).
Conclusions
In this paper, we examined the associations among sleep disturbances, HIV-related physical symptoms, and coping strategies among Asian American PLHIV. This is a vulnerable group with significant sleep and physical distress, yet reports are limited regarding their experience to activate adaptive or maladaptive coping strategies. This exploratory study proffers that sleep disturbance and physical symptoms are important factors in activating adaptive/ maladaptive coping strategies among Asian American PLHIV. Interventions designed to decrease sleep disturbances and physical symptoms should be developed to enhance adaptive coping and reduce maladaptive coping among Asian American PLHIV. Therefore, self-management strategies can be improved and reduce health disparities among Asian American PLHIV.
References
- Allavena C, Guimard T, Billaud E, De la Tullaye S, Reliquet V, Pineau S, …… COREVIH-Pays de la Loire Troubles du Sommeil Study Group., (2016). Prevalence and Risk Factors of Sleep Disturbance in a Large HIV-Infected Adult Population. AIDS and Behavior,20(2),339–344. doi: 10.1007/s10461-015-1160-5. [DOI] [PubMed] [Google Scholar]
- Babson KA, Heinz AJ, & Bonn-Mille MO,(2013). HIV medication adherence and HIV symptom severity: the roles of sleep quality and memory. AIDS Patient Care STDS, 27(10),544–52. doi: 10.1089/apc.2013.0221. [DOI] [PubMed] [Google Scholar]
- Budiman A, Cilluffo A, & Ruiz NG (2019, May 22). Key facts about Asian origin groups in the U.S. Fact Tank: News in the Numbers Pew Research Center. https://www.pewresearch.org/fact-tank/2019/05/22/key-facts-about-asian-origin-groups-in-the-u-s/ [Google Scholar]
- Carver C, & Scheier M,(1997). Situational coping and coping dispositions in a stressful transaction. Journal of Personality and Social Psychology, 66,184–195. doi: 10.1037//0022-3514.66.1.184. [DOI] [PubMed] [Google Scholar]
- Carve CS, Scheier MF, & Weintraub JK, (1989).Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology,56(2),267–283.doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Diagnoses of HIV infection in the United States and dependent areas,2017. (HIV Surveillance Report) [Google Scholar]
- Centers for Disease Control and Prevention. (2020 March 16). Effective HIV surveillance among Asian Americans and Other Pacific Islanders 2013. [Google Scholar]
- Centers for Disease Control and Prevention. (2020). HIV among Asians Retrieved from https://www.cdc.gov/hiv/group/racialethnic/asians/index.html.
- Chen D, Duan L, Chen X, Zhang Q, Chen Y, Yuan Z, & Li X,(2019). Coping strategies associated factors among older Chinese people living with HIV/AIDS. Psychology, Health & Medicine,1–10. doi: 10.1080/13548506.2019.1659983. [DOI] [PubMed] [Google Scholar]
- Chen WT, Guthrie B, Shiu CS, Wang L, Weng Z, Li CS, … & Luu BV (2015). Revising the American dream: how Asian immigrants adjust after an HIV diagnosis. Journal of advanced nursing, 71(8), 1914–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Lee SY, Shiu CS, Simoni JM, Pan C, Bao M, & Lu H, (2013a). Fatigue and sleep disturbance in HIV-positive women: A qualitative and biomedical approach. Journal of Clinical Nursing, 22(9–10),1262–9. doi: 10.1111/jocn.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Shiu CS, Yang JP, Lee SY, Lee TS, Simoni JM, …… Lu HZ, (2013b). Fatigue and sleep disturbance related to perceived stress in Chinese HIV-positive individuals: A mixed methods study. Journal of AIDS & Clinical Research,4(6). p ii: 15524.doi: 10.4172/2155-6113.1000214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Shiu C, Yang JP, Tun MMM, Zhang L, Wang K, …… Zhao H,(2020). Tobacco use and HIV symptom severity in Chinese people living with HIV. AIDS Care, 32(2),217–222. doi: 10.1080/09540121.2019.1620169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Bogart LM, Laurenceau J, Chan BT, Maughan-Brown BG, Dietrich JJ, …… Katz IT,(2018). Internalized HIV stigma, ART initiation and HIV-1 RNA suppression in South Africa: exploring avoidant coping as a longitudinal mediator. Journal of International AIDS Society,21(10), e25198. doi: 10.1002/jia2.25198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SD, Williams BE, & Leu CS,(2013). Correlates of posttraumatic growth among African Americans living with HIV/AIDS in Mississippi. Online Journal of Rural and Urban Research,3(1). [PMC free article] [PubMed] [Google Scholar]
- Fauk NK, Merry MS, & Mwanri L, (2020). Meaning-making as a coping strategy among transgender women living with HIV in Indonesia. AIDS Care,22,1–5. doi: 10.1080/09540121.2020.1716934. [DOI] [PubMed] [Google Scholar]
- Fekete EM, Chatterton M, Skinta MD, & Williams SL,(2016). Ethnic differences in the links between benefit finding and psychological adjustment in people living with HIV. Journal of Behavioral Medicine,39(3),493–501. doi: 10.1007/s10865-016-9715-0. [DOI] [PubMed] [Google Scholar]
- Finkelstein-Fox L, Park CL, & Kalichman SC,(2019). Health benefits of positive reappraisal coping among people living with HIV/AIDS: a systematic review. Health Psychology Review, 1–33. doi: 10.1080/17437199.2019.1641424. [DOI] [PubMed] [Google Scholar]
- Golub SA, Redina HJ, & Garamel KE,(2013). Identity-related growth and loss in a sample of HIV-positive gay and bisexual men: initial scale development and psychometric evaluation. AIDS and Behavior,17(2),748–759. doi: 10.1007/s10461-012-0338-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez J, Tedaldi EM, Armon C, Patel V, Hart R, &Buchacz K,(2019). Sleep disturbances in HIV-infected patients associated with depression and high risk of obstructive sleep apnea. SAGE Open Medicine,7,205031211984226. doi: 10.1177/2050312119842268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy AA, Niel K, & Du Bois SN,(2018). Emotional Support, Active Coping, and ART Adherence in Young African American Men who have Sex with Men: A Pilot Mediation Model. The Journal of Association of Nurses in AIDS Care,29(4),612–618. doi: 10.1016/j.jana.2018.02.012. [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Henry SB, Nokes KM, Corless IB, Brown MA, Powell-Cope GM, Turner JG, & Inouye J, (1999). Validation of the Sign and Symptom Check-List for Persons with HIV Disease (SSC-HIV). Journal of Advanced Nursing, 30,1041–1049. [DOI] [PubMed] [Google Scholar]
- Hu L.t., & Bentler PM,(1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling,6(1),1–55. doi.org/ 10.1080/10705519909540118 [DOI] [Google Scholar]
- Huang X, Li H, Meyers K, Xia W, Meng Z, Li C,......Wu H,(2017).Burden of sleep disturbances and associated risk factors: A cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Scientific Report,7(1),3657. doi: 10.1038/s41598-017-03968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang F, Chen WT, Shiu CS, Sun W, Toma L, Luu BV, Ah-Yune J (2020). Acculturation, HIV-Related Stigma, Stress, and Patient-Healthcare Provider Relationships Among HIV-Infected Asian Americans: A Path Analysis. Journal of Immigration and Minority Health,1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail SM, Kari F, & Kamarulzaman A (2017). The Socioeconomic Implications among People Living with HIV/AIDS in Sudan: Challenges and Coping Strategies. Journal of the International Association of Providers of AIDS Care,16(5),446–454. doi: 10.1177/2325957415622449 [DOI] [PubMed] [Google Scholar]
- Lazarus RS,& Folkman S,(1984). Stress, appraisal, and coping New York: Springer. [Google Scholar]
- Lee KA, (1992). Self-reported sleep disturbances in employed women. Sleep,15,493–498. doi: 10.1093/sleep/15.6.493 [DOI] [PubMed] [Google Scholar]
- Lee KA, Gay C, Portillo CJ, Coggins T, Davis H, Pullinger CR, Aouizerat BE, (2012). Types of sleep problems in adults living with HIV/AIDS. Journal of Clinical Sleep Medine, 8(1),67–75. doi: 10.5664/jcsm.1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindayani L, Chen YC, Wang JD, & Ko NY(2018). Complex problems, care demands, and quality of life among people living with HIV in the antiretroviral era in Indonesia. The Journal of Association of Nurses in AIDS Care,29(2),300–309. doi: 10.1016/j.jana.2017.10.002. [DOI] [PubMed] [Google Scholar]
- Kacanek D, Angelidou K, Williams PL, Chernoff M, Gadow KD, & Nachman S, International Maternal Pediatric Adolescent AIDS Clinical Trials Group (IMPAACT) P1055 Study Team., (2015). Psychiatric symptoms and antiretroviral non-adherence in US youth with perinatal HIV: a longitudinal study. AIDS,29(10), 1227–1237. doi: 10.1097/QAD.0000000000000697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim B, & Aronowitz T (2019). Invisible Minority: HIV Prevention Health Policy for the Asian American Population. Policy, Politics & Nursing Practice, 20(1),41–49. doi: 10.1177/1527154419828843. [DOI] [PubMed] [Google Scholar]
- Kremer H, Ironson G, Kaplan L, Stuetzele R, Baker N, & Fletcher MA, (2015). Spiritual coping predicts CD4-cell preservation and undetectable viral load over four years. AIDS Care,27(1),71–79. doi: 10.1080/09540121.2014.952220. [DOI] [PubMed] [Google Scholar]
- Meanley S, Yehia BR, Hines J, Thomas R, Calder D, Cater B…. Bauermeister JA (2019). HIV/AIDS-related stigma, immediate families, and proactive coping processes among a clinical sample of people living with HIV/AIDS in Philadelphia, Pennsylvania. Journal of Community Psychology, 47(7), 1787–1798. doi: 10.1002/jcop.22227. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2020, January 16). Key facts about Asian origin groups in the U.S https://www.pewresearch.org/fact-tank/2019/05/22/key-facts-about-asian-origin-groups-in-the-u-s/. [Google Scholar]
- Poteat T, & Lassiter JM, (2019). Positive religious coping predicts self-reported HIV medication adherence at baseline and twelve-month follow-up among Black Americans living with HIV in the Southeastern United States. AIDS Care,31(8), 958–964. doi: 10.1080/09540121.2019.1587363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachel R, Deepa R, Rivet KA, Eduardo R, Peter B, Cecilia C, …… Molina Y, (2019). Experienced HIV-Related Stigma and Psychological Distress in Peruvian Sexual and Gender Minorities: A Longitudinal Study to Explore Mediating Roles of Internalized HIV-Related Stigma and Coping Styles. AIDS and Behavior, 23(3),661–674. doi: 10.1007/s10461-019-02394-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren J, Zhao M, Liu B, Wu Q, Hao Y, Jiao M,......Zheng T (2018). Factors Associated with Sleep Quality in HIV. The Journal of the Association of Nurses in AIDS Care,29(6),:924–931. doi: 10.1016/j.jana.2018.04.006. [DOI] [PubMed] [Google Scholar]
- Robbins JL, Phillips KD, Dudgeon WD, & Hand GA, (2004). Physiological and psychological correlates of sleep in HIV infection. Clinical Nursing Research,13(1),33–52.doi: 10.1177/1054773803259655. [DOI] [PubMed] [Google Scholar]
- Safren SA, Radomsky AS, Otto MW, & Salomon E (2002). Predictors of Psychological Well-Being in a Diverse Sample of HIV-Positive Patients Receiving Highly Active Antiretroviral Therapy. Psychosomatics, 43(6), 478–485. doi: 10.1176/appi.psy.43.6.478. [DOI] [PubMed] [Google Scholar]
- Seffren V, Familiar I, Murray SM, Augustinavicius J, Boivin MJ, Nakasujja N, …… Bass J, (2018).Association between coping strategies, social support, and depression and anxiety symptoms among rural Ugandan women living with HIV/AIDS. AIDS Care,30(7),888–895. doi: 10.1080/09540121.2018.1441969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha S, Shibanuma A, Poudel KC, Nanishi K, Koyama Abe M, Shakya SK, & Jimba M (2019). Perceived social support, coping, and stigma on the quality of life of people living with HIV in Nepal: a moderated mediation analysis. AIDS Care, 31(4),413–420. doi: 10.1080/09540121.2018.1497136. [DOI] [PubMed] [Google Scholar]
- Skalski LM, Martin B & Meade CS (2019). Sexual Orientation, Religious Coping, and Drug Use in a Sample of HIV-Infected African-American Men Living in the Southern USA. Journal of Religion and Health,58(4),1368–1381. doi: 10.1007/s10943-019-00791-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taibi DM(2013). Sleep disturbances in persons living with HIV. The Journal of Association of Nurses in AIDS Care, 24(1 Suppl),S72–85. doi: 10.1016/j.jana.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeraananchai S, Kerr SJ, Amin J, Ruxrungtham K & Law MG (2017). Life expectancy of HIV-positive people after starting combination antiretroviral therapy: a meta-analysis. HIV Medicine, 18(4), 256–266. doi: 10.1111/hiv.12421. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. “ACS Demographic and Housing Estimates”. December 2019. Retrieved March 20, 2020. [Google Scholar]
- Wardell JD, Shuper PA, Rourke SB, & Hendershot CS (2018). Stigma, Coping, and Alcohol Use Severity Among People Living with HIV: A Prospective Analysis of Bidirectional and Mediated Associations. Annals of Behavioral Medicine,52(9),762–772. doi: 10.1093/abm/kax050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Peasant C & Sullivan TP (2017). Intimate Partner Violence and HIV-Risk Behaviors: Evaluating Avoidant Coping as a Moderator. AIDS and Behavior, 21(8), 2233–2242. doi: 10.1007/s10461-016-1588-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willie TC, Overstreet NM, Peasant C, Kershaw T, Sikkema KJ, & Hansen NB (2016). Anxiety and depressive symptoms among people living with HIV and childhood sexual abuse: The role of shame and posttraumatic growth. AIDS and Behavior, 20(8),1609–1620. doi: 10.1007/s10461-016-1298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson NL, Azuero A, Vance DE, Richman JS, Moneyham LD, Raper JL,...... Kempf MC (2016). Identifying Symptom Patterns in People Living with HIV Disease. The Journal of Association of Nurses in AIDS Care, 27(2),121–32. doi: 10.1016/j.jana.2015.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J, Wu H, Lu C, Guo L & Li P (2015).Self-reported sleep disturbances in HIV-infected people: a meta-analysis of prevalence and moderators. Sleep Medicine, 16(8),901–907. doi: 10.1016/j.sleep.2015.03.027. [DOI] [PubMed] [Google Scholar]
- Ye Z, Chen L, & Lin D (2018). The Relationship Between Posttraumatic Stress Disorder Symptoms and Posttraumatic Growth Among HIV-Infected Men Who Have Sex with Men in Beijing, China: The Mediating Roles of Coping Strategies. Frontiers in Psychology, 9, 1787. doi: 10.3389/fpsyg.2018.01787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu NX, Chen L, Ye Z, Li X, & Lin D,(2017). Impacts of making sense of adversity on depression, posttraumatic stress disorder, and posttraumatic growth among a sample of mainly newly diagnosed HIV-positive Chinese young homosexual men: the mediating role of resilience. AIDS Care,29(1),79–85. doi: 10.1080/09540121.2016.1210073 [DOI] [PubMed] [Google Scholar]
- Zhu Z, Zhao R, & Hu Y,(2019). Symptom Clusters in People Living With HIV: A Systematic Review. Journal of Pain and Symptom Management,58(1),115–133. doi: 10.1016/j.jpainsymman.2019.03.018. [DOI] [PubMed] [Google Scholar]
- Zhu Z, Hu Y, Xing W, Guo M, Zhao R, Han S, & Wu B,(2019). Identifying Symptom Clusters Among People Living with HIV on Antiretroviral Therapy in China: A Network Analysis. Journal of Pain and Symptom Management,57(3),617–626. doi: 10.1016/j.jpainsymman.2018.11.011. [DOI] [PubMed] [Google Scholar]


