Abstract
Adenoid cystic carcinoma (ACC) is a rare malignancy characterized by high incidence of relapse. When relapsing, ACC has an indolent but relentless behaviour, thus leading to a poor long-term prognosis. The treatment of choice of relapsing ACC remains surgery followed by radiotherapy, whenever feasible. Therapeutic weapons are limited to systemic drugs. The most widely used chemotherapy regimen is the combination of cisplatin and doxorubicin, however with low response rate and not long lasting; there is also a lack of alternatives for second line therapies in case of disease progression. Therefore, a more comprehensive strategy aimed at identifying at preclinical level the most promising drugs or combination is clearly needed. In this study, the cytotoxic effects of two standard chemotherapy drugs, cisplatin and doxorubicin, and of five targeted therapy-drugs was tested in vitro, on an h-TERT immortalized ACC cell line, and in vivo, on zebrafish embryos with ACC tumoral cell xenograft. Then, combinations of one standard chemotherapy drug plus one targeted therapy drug were also evaluated, in order to find the best treatment strategy for ACC. Data obtained demonstrated that both vorinostat and olaparib significantly increased the standard chemotherapy cytotoxic effects, suggesting new interesting therapeutic options for ACC.
Subject terms: Cancer, Cancer therapy, Head and neck cancer, Oral cancer
Introduction
Adenoid cystic carcinoma (ACC) is a rare malignancy arising mostly from salivary glands and from other sites, as trachea, bronchi, breast and skin, with an incidence of 4.5 cases per 100,000 individuals1. It represents 20% of malignant tumors of the major salivary glands and 58% of the minor salivary glands2. ACC is reported to relapse in till 50–60% of the cases, both locally and at distant sites3–5.
Generally, when relapsing, ACC has an indolent but relentless behaviour, thus leading to a poor long-term prognosis; 10-year OS ranges from 52 to 65% in several retrospective series6, 7.
Locoregional or distant recurrences represent a crucial part of the patient journey, as negatively impacting on prognosis and with higher risk of patient’s quality of life deterioration. The treatment of choice of relapsing ACC remains surgery followed by radiotherapy, whenever feasible. In case of absence of indications for locoregional treatments, with a patient experiencing symptomatic disease or at high risk of complications, therapeutic weapons are limited to systemic drugs.
The most widely used chemotherapy regimen is the combination of cisplatin and doxorubicin, however with response rate (RR) of 25% and not long lasting; there is also a lack of alternatives for second line therapies in case of disease progression8. Several target agents have been studied in ACC, mostly as single agents and in the absence of molecular selection. Recently, the most promising results have been obtained with multikinase inhibitor lenvatinib and with antiangiogenetic drugs as sorafenib and axitinib; however, these drugs reported a response rate of about 15% with a non-negligible burden of adverse events9–12. The most frequently reported molecular alteration, aside the MYB/MYB1 pathognomonic fusions, is the NOTCH-1 mutation13; in this regard, tailored targeted approaches have been studied and are currently ongoing in NOTCH-mutated ACC14. Overall, targeted agents seem to benefit a small quote of recurrent and/or metastatic (RM) ACC, at the price of drug-induced toxicities. Therefore, a more comprehensive strategy aimed at identifying at preclinical level the most promising drugs or combination is clearly needed.
The primary aim of our study is the evaluation in vitro and in vivo of new therapeutic strategies that can expand therapeutic possibilities available for patients with RM ACC.
Methods
Cell culture
The human ACC (hTERT) cell line, derived from a primary untreated and predominantly cribriform ACC of the tongue base immortalized using h-TERT transfection, was kindly given by Prof. Adel El-Naggar (Department of Pathology, The University of Texas, MD Anderson Cancer Center, Houston, TX, USA). Cells were maintained in standard medium, as previously reported15. ACC (hTERT) cells doubling time both at 37 °C and at 32 °C, 5% CO2 was calculated according to ATCC (American Type Culture Collection, Virginia, USA). Cells were authenticated by the GenePrint 10 System (Promega Italia, Milan, Italy), according to the protocols suggested by the manufacturer. Cells were used between passage 144 and 155 and periodically tested for mycoplasma.
Cells treatment
ACC (hTERT) cells (15,000 cells/well) were plated in 24-well plates with complete medium. For the concentration–response curves, cells were exposed to the following drugs concentration: cisplatin (Selleckchem Chemicals, Houston, Texas, USA) (0.03–24 µM); doxorubicin (Selleckchem Chemicals) (0.001–1 µM); lenvatinib (MedChem Express, Monmouth Junction, New Jersey, USA) (0.05–2 µM); vorinostat (MedChem Express) (0.1–9 µM); everolimus (Selleckchem Chemicals) (0.5–250 nM); palbociclib (Selleckchem Chemicals) (0.03–9 uM); olaparib (Selleckchem Chemicals) (0.15–18 µM). According to cells doubling time, ACC (hTERT) cells were treated with the drugs for 4 days.
Cell viability and cell proliferation assay
Cell viability was assessed by 3-(4,5-Dimethyl-2-thiazol)-2,5-diphenyl-2H-tetrazolium bromide (MTT) dye reduction assay according to the manufacturer protocol (Sigma Aldrich, Italia, Milan, Italy) and performed as previously described16. Cell proliferation rate was evaluated with TC20 automated cell counter (Bio-Rad, Segrate, Milan, Italy).
Drug combination experiments
Drug combination experiments were performed to evaluate drug interactions on ACC cell viability, according to the Chou and Talaly method17. Cells were treated for 4 days with the following drugs, used alone or in combination: cisplatin (0.018–13.2 µM) and palbociclib (0.020–14.742 µM), doxorubicin (0.002–0.255 µM) and palbociclib (0.026–3 µM), cisplatin (0.187–21.3 µM) and vorinostat (0.064–7.26 µM), doxorubicin (0.002–0.255 µM) and vorinostat (0.14–16 µM), cisplatin (0.1–30.37 µM) and everolimus (0.41–157.46 nM), doxorubicin (0.002–0.255 µM) and everolimus (0.62–70.3 nM), cisplatin (0.75–25.66 µM) and olaparib (0.874–29.74 µM), doxorubicin (0.002–0.255 µM) and olaparib (0.23–26.6 µM), vorinostat (0.018–13.5 µM) and palbociclib (0.02–14.58 µM). Drug concentrations used in the combinations followed a fixed dilution ratio, as recommended for the most efficient data analysis18. Data were analysed using the CompuSyn software (ComboSyn inc. Paramus, NJ, USA) as previously described16.
Collection of zebrafish eggs and fish maintenance
All zebrafish were handled according to national and international guidelines (EU Directive 2010/63/EU), following protocols approved by the local committee (Organismo Preposto al Benessere Animale (OPBA), Università degli Studi di Brescia, protocol no. 211B5.24) and authorized by the Ministry of Health (authorization no. 393/2017-PR). The experiments were complied with the ARRIVE guidelines (https://arriveguidelines.org). Healthy adult wild-type zebrafish (AB strain) were used for egg production. Fishes were maintained under standard laboratory conditions19, at 28 °C on a constant 14-h light/10-h dark cycle. Fish were fed thrice daily with a combination of granular dry food and fresh artemia (Special Diet Services, SDS Diets; LBS Biotech, Horley, UK). Collection of zebrafish eggs and maintenance of developing embryos has been performed as previously described20.
Zebrafish single-drug treatment concentration
Embryos maintained in fish water plus PTU (1-phenyl-2-thiourea) were manually dechorionated at 48 h post-fertilization (hpf) and treated for 3 days with each single drug at these concentration range: cisplatin (25–50 µM), doxorubicin (5–20 µM), vorinostat (25–50 µM), palbociclib (5–10 µM), olaparib (25–100 µM), everolimus (1–5 µM). For each drug the toxicity was tested, and the final effective concentration was set for subsequent experiments.
Tumor xenograft
ACC cells (1.25 × 106 cells) were labelled with the vital red fluorescent dye CellTrackerTM CM-DiI (final concentration 0.66 ng/mL; Thermo Fisher Scientific, Milan, Italy), and resuspended in 25 µL of PBS for microinjections. Tumor xenograft was performed as previously described20. Drugs or solvents were directly added to the PTU-fish water and after 3 days of treatment (T3), pictures were taken. The tumour areas of vehicle- and drug-treated groups at T0 and T3 were analysed with Axio Zoom Fluorescent Microscope (Carl Zeiss AG, Oberkochen, Germany) and measured with Noldus DanioScopeTM software (Noldus information Technology). Data obtained were analysed by GraphPad Prism software version 6.01.
Statistical analysis
Data analysis was performed using GraphPad Prism software version 5.02 (GraphPad Software, La Jolla, CA). Statistical analysis was carried out using one-way ANOVA analysis with a post hoc test (Bonferroni’s test) for multiple comparisons, considering p < 0.05 as threshold for statistical significance. Data are expressed as mean ± SEM of three independent experiments, unless otherwise specified. Cytotoxicity experiments were carried out at least three times, each point run in triplicate.
Results
Standard chemotherapy and target therapy drugs induced cytotoxicity in ACC cell line
ACC (hTERT) cell line doubling time was firstly evaluated (Fig. S1). Being the cells doubling time around 50 h, ACC cells were treated with the drugs for 4 days.
The cytotoxicity of the two standard chemotherapeutic agents (cisplatin and doxorubicin) and five target therapy drugs (everolimus, palbociclib, olaparib, vorinostat and lenvatinib) were tested on ACC (hTERT) cell line.
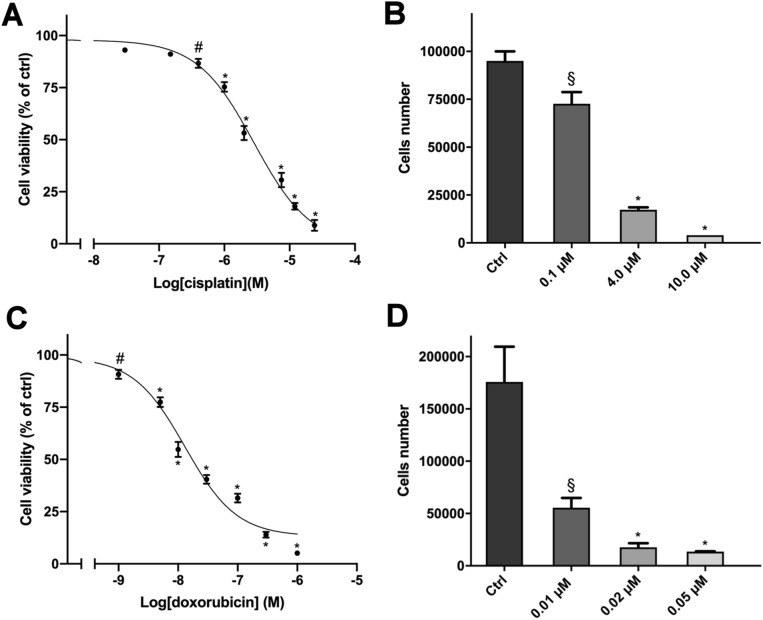
Exposure of cells to increasing concentrations of cisplatin and doxorubicin for 4 days led to a concentration-dependent reduction of cell viability, analysed by MTT assay. Sigmoidal concentration–response function was applied to calculate the IC50 value, that was, respectively, 3 μM (95% confidence interval (CI): 2.3–3.5 μM) and 0.013 μM (95% CI 0.01–0.017 μM) for cisplatin and doxorubicin (Fig. 1A,C). The standard chemotherapy drugs were highly active in inducing cytotoxicity, as their efficacy reached over the 90% at the highest concentration tested.
Figure 1.
Cytotoxic effect of cisplatin and doxorubicin in hTERT cells. (A) Concentration–response curve of cisplatin-induced inhibition of cell viability. Cells were treated with increasing concentrations of cisplatin (0.03–24 µM) for 4 days. (B) Effect of cisplatin on cell proliferation. Cells were treated for 4 days with three concentrations of cisplatin. (C) Concentration–response curve of doxorubicin-induced inhibition of cell viability. Cells were treated with increasing concentrations of doxorubicin (0.001–1 µM) for 4 days. (D) Effect of doxorubicin on cell proliferation. Cells were treated for 4 days with three concentrations of doxorubicin. Cell viability was evaluated by MTT assay while cells proliferation was assessed after cells count with trypan blue exclusion. Data are shown as mean ± SEM [*p < 0.0001; #p < 0.01; §p < 0.05].
Also, a cell count was performed in order to evaluate the effect on the cell proliferation rate. As reported in Fig. 1B,D, cell count confirmed data obtained in the MTT viability test.
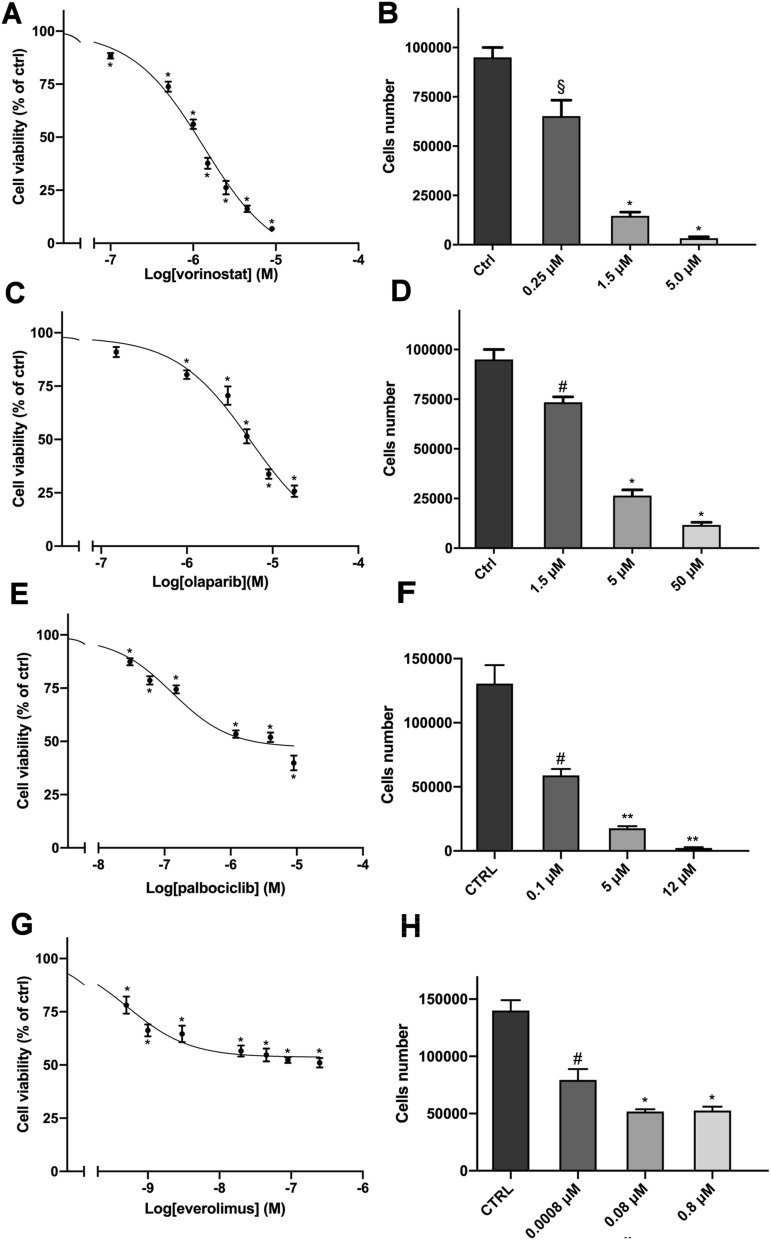
We then evaluated the effect of ACC potentially effective target therapy drugs. Among the drugs tested, the four drugs listed below resulted to be effective in reducing cell viability, considering drug concentrations compatible with clinical practice: vorinostat, olaparib, palbociclib and everolimus (Fig. 2A,C,E,G). The IC50 values were: vorinostat 1.3 µM (95% CI 1.1–1.6 μM), olaparib 5.5 µM (95% CI 3.8–8.1 μM), palbociclib 0.13 µM (95% CI 0.09–0.2 μM), everolimus 0.5 nM (95% CI 0.3–0.8 nM). Drug effects on cell proliferation were also evaluated, as reported in Fig. 2B,D,F,H. Detailed data on drugs potency and efficacy are reported in Table 1. Lenvatinib was as well tested for cytotoxic effects on ACC (hTERT) cells, but its efficacy was very poor, remaining far above the 50% value of cell viability even at high drug concentrations (Fig. S2).
Figure 2.
Cytotoxic effect of target therapy drugs in hTERT cells. (A,C,E,G) Concentration–response curves of vorinostat-, olaparib-, palbociclib- and everolimus-induced inhibition of cell viability. Cells were treated with increasing concentrations of vorinostat (0.1–9 µM) or olaparib (0.15–18 µM) or palbociclib (0.03–9 µM) or everolimus (0.5–250 nM) for 4 days. (B,D,F,H) Effect of vorinostat, olaparib, palbociclib and everolimus respectively, on cell proliferation. Cells were treated for 4 days with three concentrations of each drug. Cell viability was evaluated by MTT assay while cells proliferation was assessed after cells count with trypan blue exclusion. Data are shown as mean ± SEM [*p < 0.0001; ** p<0.001; #p < 0.01; §p < 0.05].
Table 1.
Drugs potency and efficacy.
| Drugs | IC50 (95% C.I.) | % cell mortality (± SEM) at max concentration (M) |
|---|---|---|
| Cisplatin | 3 μM (2.3 to 3.5 μM) | 91.15% (± 2.6) at 24 μM |
| Doxorubicin | 0.013 μM (0.01 to 0.017 μM) | 94.91% (± 0.77) at 1 μM |
| Vorinostat | 1.3 μM (1.1 to 1.6 μM) | 96.28% (± 0.47) at 13.5 μM |
| Olaparib | 5.5 μM (3.8 to 8.1 μM) | 74.26% (± 2.69) at 18 μM |
| Palbociclib | 0.13 μM (0.09 to 0.2 μM) | 60.13% (± 3.4) at 9 μM |
| Everolimus | 0.5 nM (0.3 to 0.8 nM) | 48.96% (± 2.23) at 250 nM |
In vivo effects of both standard chemotherapy and target therapy drugs
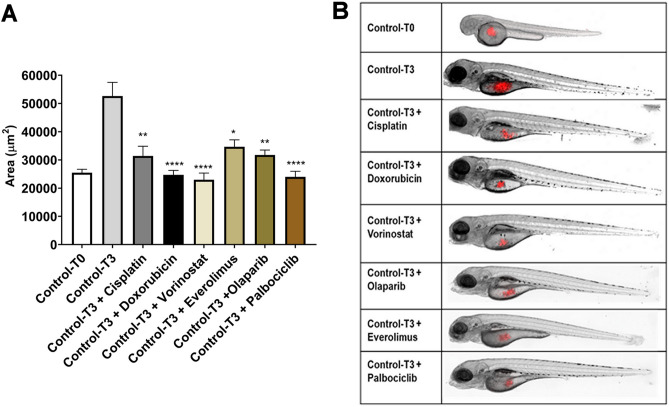
The cytotoxic effects observed in vitro was then tested in vivo in the experimental model of cell xenograft on zebrafish embryos. As zebrafish embryos were maintained at the temperature of 32 °C, ACC cell behavior was studied in terms of viability and doubling time at 32 °C and results indicated that this cell line was able to growth and duplicate at this temperature (Fig. S3). The ACC cells were injected in zebrafish embryos and the tumor area was evaluated at different times. In particular, each single drug or solvent were directly added to the fish water and after 3 days of treatment the tumor areas of vehicle- and drug-treated groups at T0 (2 h after treatment) and T3 (3 days of treatment) were measured (Fig. 3B).
Figure 3.
Chemotherapy drugs and target therapy drugs reduced the tumor xenograft area of hTERT cells. (A) The tumor area of T0 and T3 drug-treated and solvent-treated groups was measured with Noldus DanioScopeTM software. (B) A representative image is shown. Control-T0, time point at injection (control embryos at 48 hpf); Control-T3, time point 3 days later in fish water with solvent alone (untreated embryos at 120 hpf); Control-T3+ drugs, time point 3 days later in fish water with drugs (treated embryos at 120 hpf). The experiments were performed twice and each group was representative of 25 embryos. Data are shown as mean ± SEM [****p < 0.0001; **p < 0.01; *p < 0.05].
As reported in Fig. 3A, ACC tumor grew very fast in the injected area of the yolk sac, approximately doubling its area in 72 h (mean area (μm2) ± SEM: 29.11 ± 0.9 × 103 μm2 and 52.6 ± 4.9 × 103 μm2 at T0 and T3, respectively). All the drugs tested significantly reduced the tumor area compared to T3-vehicle. In particular, doxorubicin, vorinostat and palbociclib exposure reduced the tumor area at levels comparable to the T0 group (mean area (μm2) ± SEM: 24.7 ± 1.6 × 103 μm2; 23.0 ± 2.3 × 103 μm2 and 24.0 ± 2.0 × 103 μm2, respectively). Cisplatin, everolimus and olaparib treatment, although less effective in reducing tumor area compared to the other drugs tested, led to a significant difference as compared to the T3-vehicle group (mean area (μm2) ± SEM: 31.4 ± 3.4 × 103 μm2; 34.7 ± 2.4 × 103 μm2 and 31.8 ± 1.7 × 103 μm2, respectively).
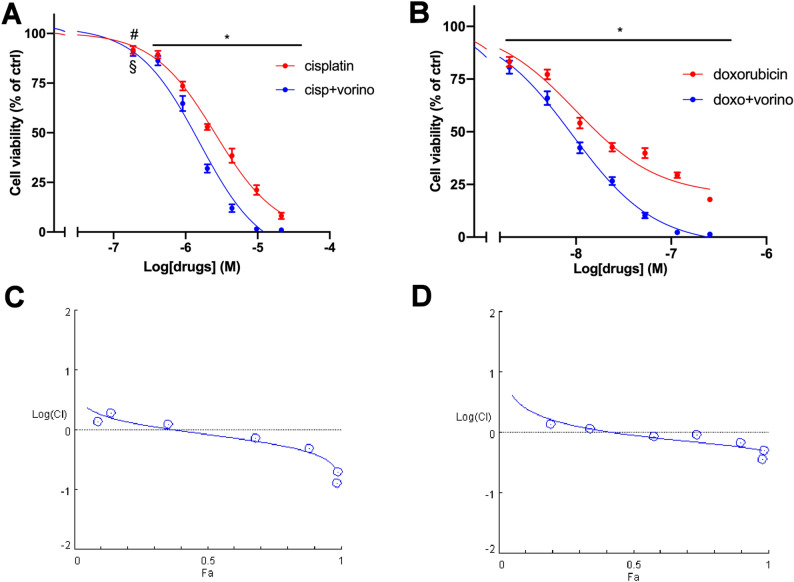
Vorinostat and olaparib enhanced cytotoxicity induced by standard chemotherapy drugs
In order to evaluate the effect on ACC cells of target therapy drugs combined with either doxorubicin or cisplatin, the Chou–Talalay method was applied, as described in “Methods” section. The most promising results were obtained with the combination vorinostat plus cisplatin and vorinostat plus doxorubicin. In these cases, the combined treatments in ACC cells induced synergistic cytotoxic effects compared to each single compound. The concentration–response curves of single standard chemotherapy drug and of the combined treatments are reported in Fig. 4A,B. An increase in the potency was also observed in both combinations. Results obtained were analyzed with CompuSyn software; the combination index plots and the synergic effects are shown in Fig. 4C,D. The combination index (CI) values were < 1 starting from 0.68 to 2 μM for vorinostat and cisplatin, respectively. In the case of vorinostat/doxorubicin, CI < 1 was observed with 0.68 μM vorinostat and 0.011 μM doxorubicin.
Figure 4.
Vorinostat enhanced the effect of the chemotherapy drugs on hTERT cell viability. (A) Concentration–response curves of cisplatin− and cisplatin plus vorinostat-induced inhibition of cell viability. Cells were treated with increasing concentrations of cisplatin alone or in combination with vorinostat at fixed concentration molar ratio (cisplatin:vorinostat = 2.9:1) for 4 days. (B) Concentration–response curves of doxorubicin− and doxorubicin plus vorinostat-induced inhibition of cell viability. Cells were treated with increasing concentrations of doxorubicin alone or in combination with vorinostat at fixed concentration molar ratio (doxorubicin: vorinostat = 1:62.7) for 4 days. Cell viability was evaluated by MTT assay. Data are shown as mean ± SEM. (C,D) Semilogarithmic-Combination Index Plot of combined treatments with cisplatin plus vorinostat and doxorubicin plus vorinostat respectively. Dose and effect data obtained were converted to Fa values and analyzed with CompuSyn software [*p < 0.0001; #p < 0.01; §p < 0.05].
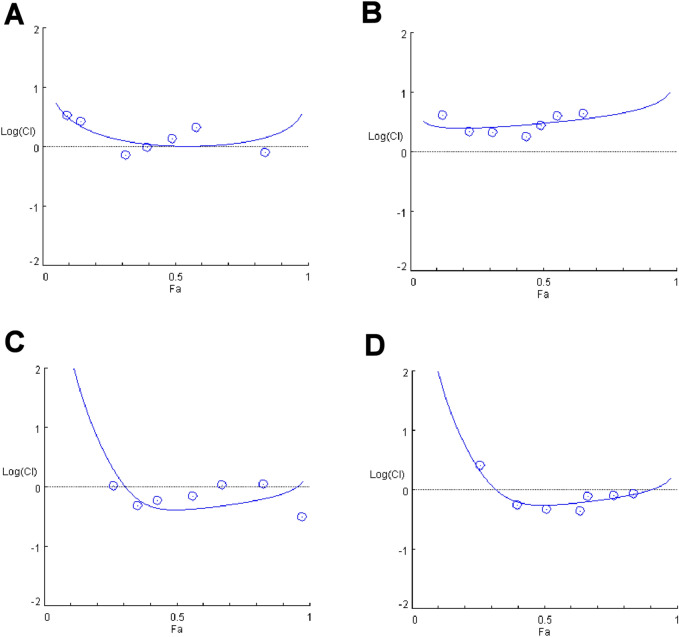
Interestingly, olaparib treatment in ACC cells enhanced cytotoxicity induced by standard chemotherapy drugs. Indeed, both olaparib/cisplatin and olaparib/doxorubicin combined treatment increased cytotoxic effect as compared to each single-drug treatment which resulted in an increase in the potency (Fig. 5A,B). The Chou-Thalalay analysis confirmed the additive effect of the combined treatments (CI = 1, see Fig. 5C,D).
Figure 5.
Olaparib enhanced the effect of the chemotherapy drugs on hTERT cell viability. (A) Concentration–response curves of cisplatin− and cisplatin plus olaparib-induced inhibition of cell viability. Cells were treated with increasing concentrations of cisplatin alone or in combination with olaparib at fixed concentration molar ratio (cisplatin:olaparib = 1:1.2) for 4 days. (B) Concentration–response curves of doxorubicin− and doxorubicin plus olaparib-induced inhibition of cell viability. Cells were treated with increasing concentrations of doxorubicin alone or in combination with olaparib at fixed concentration molar ratio (doxorubicin:olaparib = 1:104.3) for 4 days. Cell viability was evaluated by MTT assay. Data are shown as mean ± SEM. (C,D) Semilogarithmic-Combination Index Plot of combined treatments with cisplatin plus olaparib and doxorubicin plus olaparib respectively. Dose and effect data obtained were converted to Fa values and analyzed with CompuSyn software [*p < 0.0001].
All target therapy drugs were tested in combination with standard chemotherapy drugs, but as emerged in the analysis (Fig. 6), palbociclib and everolimus did not produce any significant increase in the single standard chemotherapy treatments. Specific concentration–response curves are reported in Fig. S4.
Figure 6.
Effect of palbociclib and everolimus combined with chemotherapy drug. Semilogarithmic-Combination Index Plot of combined treatments with (A) cisplatin plus palbociclib, (B) doxorubicin plus palbociclib, (C) cisplatin plus everolimus and (D) doxorubicin plus everolimus. Dose and effect data obtained were converted to Fa values and analyzed with CompuSyn software.
Discussion
Chemotherapy has been for years the mainstay of treatment of relapsed ACC not eligible to locoregional treatment, but with no proofs of benefit in increasing survival21–23. No treatment options are present up to now for second line therapy24. Target therapy has emerged as a treatment option, but data till now available are quite disappointing. Single agents cetuximab, imatinib, dovitinib, bortezomib, cabozantinib, and bortezomib showed limited response rate (0–6%)24. Even combination therapy of chemotherapy plus imatinib or bortezomib did not show synergistic effects in unselected population25, 26. These unsatisfactory results underline the importance of comprehensively dissecting the therapeutic pathways involved in ACC and widely testing in preclinical models the activity of drug(s). The burden of mutations in ACC is low, with a few alterations recognized as therapeutically actionable13. This is mirrored by the paucity of trials aimed at delivering targeted treatments associated with known mutations or with altered molecular pathways. Moreover, the additive or synergistic effect of chemotherapy and targeted agents have not been widely studied at preclinical level.
ACC is a rare tumor and one of the main limitations for the research activity is the lack of models for the study of the disease. As an in vitro model we used the only cell line available, a human ACC cell line immortalized using h-TERT transfection. It has already been authenticated and well characterized15 and based on its genomic/proteomic profile (e.g., negative staining for p63) it resembles the more aggressive forms of ACC (ACC-I)27.
In the present study, human ACC (hTERT) cell line was used to test in vitro the pharmacological effects of standard chemotherapy and target therapy agents used in monotherapy or in combination, to give the preclinical bases for a pharmacological strategy for ACC treatment. We selected the most employed chemotherapy agents in ACC, cisplatin and doxorubicin26, studied to verify their cytotoxic and antiproliferative effect in the ACC experimental model used, and five target therapy agents, vorinostat, olaparib, palbociclib, everolimus and lenvatinib. The drug concentrations used in the study are consistent with the doses actually used in the clinic and with the resulted plasmatic concentrations28–35.
The rationale underlying the target therapy drugs chosen to evaluate their cytotoxic activity lies on data in literature, showing that the targets of these drugs were involved in the ACC carcinogenesis and progression. Indeed, it has been shown that recurring mutations in chromatin remodelling regulations genes are involved in ACC36. Vorinostat, a histone deacetylase inhibitor, showed response just in 7% of the case as monotherapy, but exerted its synergistic effect with cisplatin in preclinical models37, 38. Moreover, vorinostat in association with cisplatin demonstrated efficacy in depleting cancer stem cells and reducing tumor viability in ACC primary cell38. The PARP inhibitor olaparib was chosen because of the demonstrated presence in ACC of molecular alterations involved in DNA repair pathways, and thus possibly having a role both as single agent and in combination with chemotherapy13. Role of cycline dependent kinase (CDK) inhibitors has been recently evaluated in an in vitro study in ACC, with evidence of synergistic antitumoral activity in combination with cisplatin39. Everolimus may play a role in ACC, as, in an ACC cell line, Younes et al.40 showed the role of phosphatidylinositol 3-kinase (PI3K)-Akt-mammalian target of rapamycin (mTOR) as potentially target of therapy. Everolimus in a phase 2 study41 showed a median progression-free survival (PFS) of 11.2 months and about 80% of stable disease, however no partial or complete response were achieved. Finally, lenvatinib is a second-generation multiple kinase inhibitor with a strong anti-angiogenic effect; it reported responses in the range of 12–16% and high rate of disease stabilization (about 70% of patients), but with half of the patients reporting toxicity of grade 3 or greater11, 12.
Our results demonstrated the in vitro cytotoxic activity of the standard chemotherapy drugs. Among targeted agents, vorinostat reported the highest efficacy, with a cell mortality of over 90%, while modest efficacy emerged for olaparib and palbociclib and poor efficacy for everolimus. Finally, lenvatinib did not induce significant cytotoxic effects in ACC (hTERT) cell line, and this poor performance could be explained by the lack of vascular components of in vitro models, that are indeed one of the main mechanisms of action of this drug. The in vitro cytotoxic effect of all the drugs tested was confirmed and strengthen by results obtained in the in vivo model of ACC (hTERT) cell line xenograft in zebrafish embryos. This animal model offers a valid and useful tool for in vivo first drug screening20, 42.
In the context of ACC tumor, several studies confirmed that a two-drug polychemotherapy gives better response rate compared with monotherapy43, even if with limited duration and uncertain benefit in overall survival. Therefore, the association of chemotherapy and targeted agents is a logical step to be carried out44 and we tried to demonstrate the activity of these combinations in the in vitro model of ACC cell line. Our results demonstrated that the two standard chemotherapy agents (cisplatin or doxorubicin) plus vorinostat or olaparib were effective. Indeed, vorinostat significantly increased both the efficacy and the potency of the standard chemotherapy agents and the combination exerted a synergic effect. Also olaparib improved the performance of the two chemotherapy agents, resulting in an addictive effect. These effects found their rationale in the specific molecular mechanism of the drugs: both cisplatin and doxorubicin hamper DNA replication and RNA transcription, the first inducing the formation of intra- and inter-strand cross-link of nuclear DNA45, the second interacting with DNA by intercalation and inhibiting macromolecular biosynthesis. This effect finally leads to cell cycle arrest and apoptosis. Vorinostat increases the formation of hyperacetylated histones, which therefore blocks the interaction of histone with DNA and leaves it more accessible by cisplatin or doxorubicin. Therefore, the synergistic effect induced by vorinostat may be due to the action upstream of the chemotherapy agents, which facilitates and greatly enhances their effects and this result in ACC cells is in line with the finding that vorinostat sensitizes ACC tumor cells to chemotherapy38. Olaparib, on the other hand, preventing the repair of the DNA damages induced by platinum compounds or doxorubicin46, acts downstream of cisplatin and doxorubicin, adding a further barrier to cell proliferation.
Taken together, our results indicate that combined treatment with vorinostat or olaparib with standard chemotherapy agents cisplatin and doxorubicin is significantly more effective than monotherapy. These data set the basis for further studies in a dedicated prospective clinical trial. The drug combination proposed have already been examined in clinical trials. Back in 2014, a phase I trial showed tolerability and promising activity of the combination PARPi + cisplatin in solid tumors47. Given the strong preclinical rationale of synergistic effects between CDK inhibitors and platinum-based therapy48 combination is under evaluation in an ongoing phase I clinical trial (NCT02897375). Finally, phase I-II study on HDAC inhibitors vorinostat with platinum chemotherapy agents showed promising clinical activity and good tolerability, even in a triplet combination with taxol or capecitabine49, 50.
Supplementary Information
Author contributions
Conceptualization: P.B., S.S. Formal Analysis: T.S., A.A. Funding acquisition: P.B., S.S. Investigation: T.S., A.A., R.M.B. Methodology: A.A., S.S., R.M.B., D.Z. Project administration: S.S., S.A.B., P.B. Writing—original draft: T.S., A.A., S.A.B. Writing—review & editing: L.L., C.G., M.T., D.L., D.T., D.Z., M.M., A.B.
Funding
The funding was provided by local grant of the University of Brescia.
Data availability
All data generated or analysed during this study are included in this published article [and its Supplementary Information files]. Further details are available on request from the corresponding author.
Competing interests
Paolo Bossi: Advisory board or conference honoraria: Merck, Sanofi, Merck Sharp & Dohme, Sun Pharma, Angelini, Molteni, Bristol-Myers Squibb, Helsinn, GSK. All other authors declare no competing interests in the area of adenoid cystic carcinoma.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Teresa Savarese, Andrea Abate, Sandra Sigala and Paolo Bossi.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-14197-8.
References
- 1.Ellington CL, et al. Adenoid cystic carcinoma of the head and neck: Incidence and survival trends based on 1973–2007 Surveillance, Epidemiology, and End Results data. Cancer. 2012;118:4444–4451. doi: 10.1002/cncr.27408. [DOI] [PubMed] [Google Scholar]
- 2.Coca-Pelaz A, et al. Adenoid cystic carcinoma of the head and neck—An update. Oral Oncol. 2015;51:652–661. doi: 10.1016/j.oraloncology.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Xu B, et al. Predictors of outcome in adenoid cystic carcinoma of salivary glands: A clinicopathologic study with correlation between MYB fusion and protein expression. Am. J. Surg. Pathol. 2017;41:1422–1432. doi: 10.1097/PAS.0000000000000918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terhaard CH, et al. Salivary gland carcinoma: Independent prognostic factors for locoregional control, distant metastases, and overall survival: Results of the Dutch head and neck oncology cooperative group. Head Neck. 2004;26:681–692. doi: 10.1002/hed.10400. [DOI] [PubMed] [Google Scholar]
- 5.Xu MJ, et al. Mortality risk after clinical management of recurrent and metastatic adenoid cystic carcinoma. J. Otolaryngol. Head Neck Surg. 2018;47:28. doi: 10.1186/s40463-018-0273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ciccolallo L, Licitra L, Cantú G, Gatta G, EUROCARE Working Group Survival from salivary glands adenoid cystic carcinoma in European populations. Oral Oncol. 2009;45:669–674. doi: 10.1016/j.oraloncology.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 7.van Weert S, et al. Adenoid cystic carcinoma of the head and neck: A single-center analysis of 105 consecutive cases over a 30-year period. Oral Oncol. 2013;49:824–829. doi: 10.1016/j.oraloncology.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Laurie SA, Ho AL, Fury MG, Sherman E, Pfister DG. Systemic therapy in the management of metastatic or locally recurrent adenoid cystic carcinoma of the salivary glands: A systematic review. Lancet Oncol. 2011;12:815–824. doi: 10.1016/S1470-2045(10)70245-X. [DOI] [PubMed] [Google Scholar]
- 9.Thomson DJ, et al. Phase II trial of sorafenib in advanced salivary adenoid cystic carcinoma of the head and neck. Head Neck. 2015;37:182–187. doi: 10.1002/hed.23577. [DOI] [PubMed] [Google Scholar]
- 10.Keam B, et al. Randomized phase II study of axitinib versus observation in patients with recurred or metastatic adenoid cystic carcinoma. J. Clin. Oncol. 2020;38:6503–6503. doi: 10.1200/JCO.2020.38.15_suppl.6503. [DOI] [PubMed] [Google Scholar]
- 11.Tchekmedyian V, et al. Phase II study of lenvatinib in patients with progressive, recurrent or metastatic adenoid cystic carcinoma. J. Clin. Oncol. 2019;37:1529–1537. doi: 10.1200/JCO.18.01859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Locati LD, et al. Patients with adenoid cystic carcinomas of the salivary glands treated with lenvatinib: Activity and quality of life. Cancer. 2020;126:1888–1894. doi: 10.1002/cncr.32754. [DOI] [PubMed] [Google Scholar]
- 13.Ho AS, et al. Genetic hallmarks of recurrent/metastatic adenoid cystic carcinoma. J. Clin. Investig. 2019;129:4276–4289. doi: 10.1172/JCI128227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferrarotto R, et al. ACCURACY a phase II trial of AL101, a selective gamma secretase inhibitor, in subjects with recurrent/metastatic (R/M) adenoid cystic carcinoma (ACC) harboring Notch activating mutations (Notchmut) Ann. Oncol. 2020;31(suppl_4):S599–S628. [Google Scholar]
- 15.Li J, Perlaky L, Rao P, Weber RS, El-Naggar AK. Development and characterization of salivary adenoid cystic carcinoma cell line. Oral Oncol. 2014;50:991–999. doi: 10.1016/j.oraloncology.2014.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abate A, et al. Cytotoxic effect of trabectedin in human adrenocortical carcinoma cell lines and primary cells. Cancers (Basel) 2020;12:928. doi: 10.3390/cancers12040928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chou TC, Talalay P. Quantitative analysis of dose-effect relationships: The combined effects of multiple drugs or enzyme inhibitors. Adv. Enzym. Regul. 1984;22:27–55. doi: 10.1016/0065-2571(84)90007-4. [DOI] [PubMed] [Google Scholar]
- 18.Chou TC. Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol. Rev. 2006;58:621–681. doi: 10.1124/pr.58.3.10. [DOI] [PubMed] [Google Scholar]
- 19.Westerfield MA. Guide for the Laboratory Use of Zebrafish (Danio rerio): The Zebrafish Book. 4. University of Oregon Press; 2000. [Google Scholar]
- 20.Gianoncelli A, et al. Adrenocortical carcinoma xenograft in zebrafish embryos as a model to study the in vivo cytotoxicity of abiraterone acetate. Endocrinology. 2019;160:2620–2629. doi: 10.1210/en.2019-00152. [DOI] [PubMed] [Google Scholar]
- 21.Licitra L, et al. Cisplatin in advanced salivary gland carcinoma. A phase II study of 25 patients. Cancer. 1991;68:1874–1877. doi: 10.1002/1097-0142(19911101)68:9<1874::AID-CNCR2820680904>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 22.Airoldi M, et al. Phase II randomized trial comparing vinorelbine versus vinorelbine plus cisplatin in patients with recurrent salivary gland malignancies. Cancer. 2001;91:541–547. doi: 10.1002/1097-0142(20010201)91:3<541::AID-CNCR1032>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 23.Licitra L, et al. Cisplatin, doxorubicin and cyclophosphamide in advanced salivary gland carcinoma. A phase II trial of 22 patients. Ann. Oncol. 1996;7:640–642. doi: 10.1093/oxfordjournals.annonc.a010684. [DOI] [PubMed] [Google Scholar]
- 24.Alfieri S, et al. Systemic therapy in metastatic salivary gland carcinomas: A pathology-driven paradigm? Oral Oncol. 2017;66:58–63. doi: 10.1016/j.oraloncology.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 25.Argiris A, Ghebremichael M, Burtness B, Axelrod RS, Deconti RC, Forastiere AA. A phase 2 trial of bortezomib followed by the addition of doxorubicin at progression in patients with recurrent or metastatic adenoid cystic carcinoma of the head and neck: A trial of the Eastern Cooperative Oncology Group (E1303) Cancer. 2011;117:3374–3382. doi: 10.1002/cncr.25852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghosal N, et al. Phase II study of cisplatin and imatinib in advanced salivary adenoid cystic carcinoma. Br. J. Oral Maxillofac. Surg. 2011;49:510–515. doi: 10.1016/j.bjoms.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 27.Ferrarotto R, et al. Proteogenomic analysis of salivary adenoid cystic carcinomas defines molecular subtypes and identifies therapeutic targets. Clin. Cancer Res. 2021;27(3):852–864. doi: 10.1158/1078-0432.CCR-20-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vorinostat. IBM Micromedex® DRUGDEX® (Electronic Version). IBM Watson Health, https://www.micromedexsolutions.com/ (Accessed 16 January 2021).
- 29.Olaparib. IBM Micromedex® DRUGDEX® (Electronic Version). IBM Watson Health. https://www.micromedexsolutions.com. Accessed 16 January 2021.
- 30.Palbociclib. IBM Micromedex® DRUGDEX® (Electronic Version). IBM Watson Health. https://www.micromedexsolutions.com. Accessed 16 January 2021.
- 31.Everolimus. IBM Micromedex® DRUGDEX® (Electronic Version). IBM Watson Health. https://www.micromedexsolutions.com. Accessed 16 January 2021.
- 32.van Tilburg CM, et al. Phase I/II intra-patient dose escalation study of vorinostat in children with relapsed solid tumor, lymphoma, or leukemia. Clin. Epigenet. 2019;11:188. doi: 10.1186/s13148-019-0775-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tamura K, et al. Phase I study of palbociclib, a cyclin-dependent kinase 4/6 inhibitor, in Japanese patients. Cancer Sci. 2016;107:755–763. doi: 10.1111/cas.12932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ikeda M, et al. Safety and pharmacokinetics of lenvatinib in patients with advanced hepatocellular carcinoma. Clin. Cancer Res. 2016;22:1385–1394. doi: 10.1158/1078-0432.CCR-15-1354. [DOI] [PubMed] [Google Scholar]
- 35.Gupta A, Jarzab B, Capdevila J, Shumaker R, Hussein Z. Population pharmacokinetic analysis of lenvatinib in healthy subjects and patients with cancer. Br. J. Clin. Pharmacol. 2016;81:1124–1133. doi: 10.1111/bcp.12907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frierson HF, Jr, Moskaluk CA. Mutation signature of adenoid cystic carcinoma: Evidence for transcriptional and epigenetic reprogramming. J. Clin. Investig. 2013;123:2783–2785. doi: 10.1172/JCI69070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goncalves PH, et al. A phase 2 study of vorinostat in locally advanced, recurrent, or metastatic adenoid cystic carcinoma. Oncotarget. 2017;8:32918–32929. doi: 10.18632/oncotarget.16464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Almeida LO, et al. Unlocking the chromatin of adenoid cystic carcinomas using HDAC inhibitors sensitize cancer stem cells to cisplatin and induces tumor senescence. Stem Cell Res. 2017;21:94–105. doi: 10.1016/j.scr.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu L, Li L, Zhang J, Cai W, Zhao S, Liu S. Accumulated cytotoxicity of CDK inhibitor dinaciclib with first-line chemotherapy drugs in salivary adenoid cystic carcinoma cells. Odontology. 2020;108:300–311. doi: 10.1007/s10266-019-00451-5. [DOI] [PubMed] [Google Scholar]
- 40.Younes MN, et al. Concomitant inhibition of epidermal growth factor and vascular endothelial growth factor receptor tyrosine kinases reduces growth and metastasis of human salivary adenoid cystic carcinoma in an orthotopic nude mouse model. Mol. Cancer Ther. 2006;5:2696–2705. doi: 10.1158/1535-7163.MCT-05-0228. [DOI] [PubMed] [Google Scholar]
- 41.Kim DW, et al. A multicenter phase II study of everolimus in patients with progressive unresectable adenoid cystic carcinoma. BMC Cancer. 2014;14:795. doi: 10.1186/1471-2407-14-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang B, Xuan C, Ji Y, Zhang W, Wang D. Zebrafish xenotransplantation as a tool for in vivo cancer study. Fam. Cancer. 2015;14:487–493. doi: 10.1007/s10689-015-9802-3. [DOI] [PubMed] [Google Scholar]
- 43.Lorini L, et al. Prognosis and management of recurrent and/or metastatic head and neck adenoid cystic carcinoma. Oral Oncol. 2021;115:105213. doi: 10.1016/j.oraloncology.2021.105213. [DOI] [PubMed] [Google Scholar]
- 44.Chabner BA, Roberts TG. Timeline: Chemotherapy and the war on cancer. Nat. Rev. Cancer. 2005;5:65–72. doi: 10.1038/nrc1529. [DOI] [PubMed] [Google Scholar]
- 45.Wang D, Lippard SJ. Cellular processing of platinum anticancer drugs. Nat. Rev. Drug Discov. 2005;4:307–320. doi: 10.1038/nrd1691. [DOI] [PubMed] [Google Scholar]
- 46.Zhu G, Chang P, Lippard SJ. Recognition of platinum-DNA damage by poly(ADP-ribose) polymerase-1. Biochemistry. 2010;49:6177–6183. doi: 10.1021/bi100775t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Balmaña J, et al. Phase I trial of olaparib in combination with cisplatin for the treatment of patients with advanced breast, ovarian and other solid tumors. Ann. Oncol. 2014;25(8):1656–1663. doi: 10.1093/annonc/mdu187. [DOI] [PubMed] [Google Scholar]
- 48.Roberts PJ, Kumarasamy V, Witkiewicz AK, Knudsen ES. Chemotherapy and CDK4/6 inhibitors: Unexpected bedfellows. Mol. Cancer Ther. 2020;19(8):1575–1588. doi: 10.1158/1535-7163.MCT-18-1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yoo C, et al. Phase I and pharmacodynamic study of vorinostat combined with capecitabine and cisplatin as first-line chemotherapy in advanced gastric cancer. Investig. New Drugs. 2014;32(2):271–278. doi: 10.1007/s10637-013-9983-2. [DOI] [PubMed] [Google Scholar]
- 50.Ramalingam SS, et al. Phase I and pharmacokinetic study of vorinostat, a histone deacetylase inhibitor, in combination with carboplatin and paclitaxel for advanced solid malignancies. Clin. Cancer Res. 2007;13(12):3605–3610. doi: 10.1158/1078-0432.CCR-07-0162. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its Supplementary Information files]. Further details are available on request from the corresponding author.