Abstract
Introduction:
The aim of this study was to assess the effect of a community-based intervention on social capital, quality of life, self-care, and health literacy among elderly.
Materials and Methods:
This quasi-experimental trial was conducted at two health-care centers in Isfahan, Iran, which assigned to the intervention and control groups. A total of 86 elderly (60 years or above) enrolled in the study. The intervention program consisted of 12 weekly group sessions with various health topics. Nine sessions held in the health-care center and three local tours in different locations of the neighborhood. The control group received routine care of health centers. Social capital, quality of life, self-care, and health literacy were assessed at baseline and 1 month after the intervention in two groups.
Results:
Mental component of quality of life (P = 0.026), self-care, and health literacy (P < 0.001) showed a significant increase in the intervention group compared to the control group at 1 month after the intervention. The total score of social capital and the dimensions of local community participation, social agency, feelings of security and trust, interactions with neighbors, and interactions with family and friends improved in the intervention group (P < 0.001). However, there was no significant difference in the dimensions of tolerance of diversity (P = 0.241) and value of life (P = 0.928).
Conclusions:
This community-based interventions with a variety of diverse and participatory components can be used as a strategy to promote the health of the elderly in primary health care.
Keywords: Aging, health literacy, primary health care, quality of life, self-care, social capital
Introduction
Over the past 50 years, the proportion of older people in general populations has increased substantially within a relatively short time.[1] According to national statistics, 21.7% of Iran's population will be over 60 by 2050.[2]
The concept of “successful aging” has been proposed in the field of geriatric research literature in the last 20 years. In fact, research paradigms have changed from the negative aspects of aging to positive elements of preventive medicine, such as lifestyle improvement, physical activity, nutrition modification, improving cognitive abilities, mental abilities, and active social participation.[3,4]
Previous studies have strongly emphasized the importance of social interventions as one of the strongest predictors of a successful aging.[5] Likewise, some research has shown the relationship between health literacy and self-care behaviors with social factors, as well as their synergistic effect on each other.[6] Social determinants of health have been considered as mediating variables affecting health inequalities, because these determinants affect health-related behaviors. Social capital is one of the social determinants of health that is closely related to both structural and intermediate determinants.[7,8] Social capital follows Putnam's approach, according to a conceptual model designed for the elderly. It consists of private social resources (family and friends), collective social resources (community), structural aspects (social, contacts and partnerships), and thematic aspects (social support and sense of belonging).[9]
Self-care is a conscious action that individuals, family members, and the community take to maintain their health. The ability to perform self-care depends on many social determinants and health situations.[10] Self-care is as a major strategy for health promotion and disease prevention. Improving self-care habits lead to increased healthy eating and physical activity, thereby reducing the risk of death and disabilities related to health inequalities among the elderly.[11]
Health literacy is defined as cognitive and social skills that give people sufficient motivation and ability to have access, perception, and proper use of information to maintain and promote optimal health status.[12] Low health literacy leads to less participation in prevention and health promotion activities, weakens self-care in chronic diseases, increases hospitalization, and ultimately leads to increased morbidity and mortality.[13,14] Previous research has shown that two basic elements of participatory learning and social support in the context of interaction between individuals are effective in increasing the health literacy of the elderly. Innovative community-based interventions can help improve understanding, judgment, and use of health information due to these two important factors.[15] In fact, such interventions can simultaneously improve the health literacy and the ability of the elderly self-care.[16]
A complex intervention is an intervention that combines a number of synergistic and related components to achieve outcomes that cannot be obtained by focusing on one element.[17,18] When designing and implementing interventions that seek to assess the simultaneous impact of several components, the invention of complex interventions helps improve the quality of work.[19] Reviews have shown that complex interventions in health-care centers improve positive outcomes such as the self-rated health and quality of life.[20]
Despite the strong emphasis on education of self-care, the repetition of traditional, scattered, and noncodified practices has reduced the power of this important aspect of health strategies. On the other hand, in many settings, health promotion services are incompatible with complex and psychological needs of older adults, which requires innovative interventions in the field of mutual trust and close interaction to increase accessibility and acceptance.[21] Interventions implemented in primary health-care centers play a key role in improving health-related behaviors.[22] Thus, design and implementation of group interventions that have synergistic effects on important health factors can provide evidence for more widespread use in health policy-making.
The purpose of this study was to design and implement a multicomponent and complex intervention[23] to promote social capital, quality of life, self-care, and health literacy in elderly in Isfahan (IRAN), with regard to dimensions of access and cocreation, so that it can be integrated in the services of the universal health network.
Materials and Methods
Trial design
A pragmatic community-based, quasi-experimental trial with a controlled group was designed and carried out in two academic primary healthcare centers from November 2019 to January 2020, in Isfahan, Iran. Potential participants were assessed for eligibility in October 2019.
The trial was approved by the Ethics Committee of the Isfahan University of Medical Sciences, Isfahan, Iran (code: IR.MUI.MED.REC.1397.311). Furthermore, this study was registered in IRCT (approval code: IRCT20191011045056N1).
Study population
We used the comparison of mean differences, according to previous similar studies on quality of life, to measure the sample size (means differences of psychological dimension). With an effect size of 0.7, the sample size in each group was calculated to be at least 35 people.[24] The sample size was considered about 42 people in each group, based on statistical power of 80%, significance level of 5%, and 20% drop rate.
A convenience sampling strategy was adopted. Two academic urban health-care centers, under the auspices of the district Health Center of Isfahan, which are geographically distant, but have the similar socioeconomic status and demographic structure, were allocated to intervention and control groups. They were selected from two different centers to prevent “contamination” between intervention and control participants. Potential participants were recruited in routine visits, or actively calling seniors who were registered in the electronic social impact bond (SIB) database (an abbreviation for the Persian equivalent of electronic “integrated health system”) and possibly met the eligibility criteria.
Participants were eligible if they were community dwelling from two urban areas that aged 60 years or above and had literacy skills for reading and writing. Participants were excluded if they needed help to go to the primary health-care centers, had cognitive impairment or dementia, had medical conditions that contraindicated physical activity, and had any severe mental health problem that prevents individuals from participating in group activities.
Blinding was not possible with regard to the educational and group-based nature of the intervention. Before the implementation of the trial, written informed consent was obtained from all the participants.
Intervention
This study was a community-based study, with multiple and varied components implemented in a complex intervention program. Intervention and content of the sessions were in line with a similar study protocol, published by Laura Coll-Planas et al. in 2018.[11] The intervention was designed to enhance social support and participation (social capital) in the elderly as mediating factors between social determinants and health outcomes and with the potential to improve the quality of life and well-being of the elderly. Intervention materials and methods slightly adjusted to fit our country's cultural and indigenous conditions.
The intervention program consisted of 12 weekly, 2-h sessions with the following topics:
Health and self-care: The facilitator introduces the program, participants introduce themselves, facilitator conduct a group discussion using photos of self-care daily activities, asking the group to bring a personal item from home the next meeting, creating a wall newspaper of member paintings, handicrafts, writing, etc.
Physical activity: Participants talk about the personal object they brought from home, discussing, and setting a specific achievable goal of daily living during the week. They identify appropriate locations for physical activity using local mapping, short instruction and discussing about the benefits and limitations of physical activity, agreeing on the destination for a group walk in the next session
Local first walk: Group does a walk with origins start and end at the health-care center and does physical activity in a place like a park or gym
Emotional health: Participants talk about achieving personal goals. There will be short tutorials on problem-solving techniques, group discussion on coping strategies, a relaxation exercise
Healthy eating habits: Short tutorials on healthy and inexpensive eating tips, group discussion on eating habits, cheaper nutrition tips, and about the places where they shop. Agree on the market or store for local circulation next week
Second local circulation: Groups visit the local supermarket. During the meeting, they discuss their eating habits and preferences for shopping
Loneliness and social relationships: A brief tutorial on concepts of loneliness and social relationships, group discussion focusing on thoughts, and perceptions of loneliness and social relationships. Divide the group into subgroups to create keywords stories about social communication
Community participation: Reading a story about a woman participating in local community activities by a member, identifying important local community activities using the local map and discussing them, group discussion on the limitations and benefits of social participation, agree on an important social place in the area for the next visit
Third local circle: The group visits an important local place, one of the site's operators explains to the group about the place and its activities. Groups are encouraged to participate in social activities
Personal autonomy: A brief tutorial on the concept of personal autonomy, group discussion of personal autonomy, discussion of the practical case put forward by the trainer
Get in touch with health professionals: A video showing how to prepare for a medical encounter. Describe the thoughts and feelings of the group members when meeting a health-care provider and their personal knowledge of health resources in the community
Group discussion final session: Expressing people's thoughts and feelings about the program, creating, and donating an imaginary gift to another participant, the group shares a farewell meal.
The intervention team consisted of four health-care providers, and one physician (with experience in health care), previously trained as group facilitators by the researchers during a 2-day workshop based on the instructional guide. Intervention was carried out at two academic health-care centers, including 12 sessions that were held weekly for 2 h, and was conducted in two groups of 20 participants. Nine of the 12 sessions executed in the center, and three sessions were held as local trips: In a public space for physical activity (park or pedestrian paths), in a large supermarket, and in a community asset that presents voluntary charitable activities that can be of interest to the participants.
One health-care professional, as an observer, recorded quantitative and qualitative measures of implementation, such as fidelity and adherence. Each participant received a code and completed the questionnaires at the beginning of the study by interviewing them. Outcome interviewers were health-care professionals who received the necessary training on interviewing and completing questionnaires, before starting the intervention. The control group received routine care of primary health centers.
Outcomes
Study outcomes included social capital, quality of life, self-care, and health literacy, which were measured before starting the intervention and 1 month after the intervention. Participants could take a short break when answering questions wherever they got tired.
The Iranian version of short-form health survey-12 (SF-12) was used to assess the quality of life, in two general physical and mental dimensions.[25] The minimum and maximum range of this questionnaire is 12–48, and scores are assessed as follows: 12–24 = weak, 25–36 = moderate, and 37–48 = good. Satisfactory internal consistency for both summary measures, which are the physical component summary (PCS) and the mental component summary (MCS), has been shown; Cronbach's alpha for PCS-12 and MCS-12 was 0.73 and 0.72, respectively. In addition, correlations between the SF-12 scales and single items showed its good convergent validity for two main dimensions.[25]
To measure social capital, the Onyx and Bullen social capital questionnaire was used, in which eight dimensions are measured, which are participation in the local community; proactivity in a social context; feelings of trust and safety; neighborhood connections; family and friends connections; tolerance of diversity; value of life; and relationships and work connections.[26] The validity and reliability of this questionnaire in the Iranian elderly have already been reviewed.[27] This questionnaire consists of 36 questions of Likert scale (5-point items from very low to very high). In this study, the last 5 questions, related to the work environment, have been omitted, due to the retirement of the most participants. Onyx and Bullen had previously used the social capital score not including questions for those employed (the 5 questions which were only applicable to people who were employed are not included), and validity and reliability of this form have already been reviewed.[26] Therefore, the minimum and maximum score of this questionnaire is from 31 to 155 in our research.
The health literacy for Iranian adults questionnaire was designed by Montazeri et al. This questionnaire has 33 items and examines health literacy in 5 dimensions of access, reading, understanding, appraisal, and decision.[28] Its minimum and maximum score is 33–165.
The questionnaire for assessing the self-care ability of the elderly has 40 items. This questionnaire was extracted for the elderly population of Iran, based on a review of studies consistent with Orem theory. The result of exploratory factor analysis in this questionnaire indicates the existence of 5 factors: physical self-care, daily self-care, emotional self-care, social self-care, and self-care when sick. These 5 factors explained nearly 79.93% of the variance of the questionnaire. Furthermore, the internal consistency (Cronbach's alpha) was 0.864.[29] Its score is between minimum and maximum of 40–160.
Statistical analysis
SPSS 26(SPSS Inc., Chicago, IL, USA). software was used to describe and analyze the data. The baseline demographic characteristics were represented by frequency (percentage) and mean ± standard deviation. At the level of inferential statistics, an independent samples t-test and the Chi-square test were used to compare the means of age and to compare the frequency distribution of qualitative data between the two groups, respectively. According to the results of the Kolmogorov–Smirnov test indicating the normality of the data distribution, independent samples t-test was used for comparing the changes of outcomes from baseline to 1 month after intervention between two groups. A significance level of < 0.05 was considered in all analyses.
Results
A total of 101 people were evaluated for eligibility, of which 86 people were included in the study (41 people in the intervention group and 45 people in the control group). Ten persons discontinued intervention (n = 4) or lost follow-up (n = 6). Among the participants, 41 and 35 patients completed the follow-up in intervention and control groups, respectively, and others were lost [Figure 1].
Figure 1.
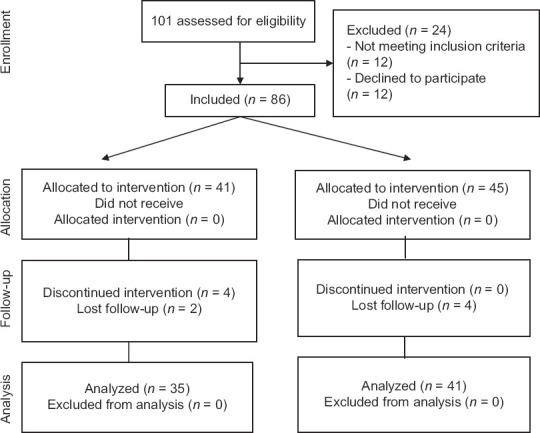
Flow diagram of the study
The intervention was implemented for 12 weeks, between October and December 2019. Outcomes measured before the start of the study (baseline) and 1 month after the end of the intervention. A follow-up and evaluation of outcomes was scheduled for 6 months after the end of the study, which was not possible due to the outbreak of COVID-19 pandemic, and the limitations and restrictions placed on the presence of elderly in the community in this period of time.
Baseline characteristics
The basic demographic and clinical characteristics of the participants in two intervention and control groups are presented in Table 1. The mean age of study participants was 66.4 ± 4/2 years. More than half of the participants were women. They had mostly received primary education and less than diploma. The majority of participants lived with their spouses, and 15.8% lived alone (widowed or divorced or never married). Most of the participants had comorbidities such as diabetes and hypertension. Due to the uncertainty about the accuracy of the recorded data on income, the amount of income is not given in Table 1. The age mean and relative frequency of individuals in terms of gender, education, marital status, and comorbidities were the same in both intervention and control groups at baseline.
Table 1.
Comparison of baseline demographic and clinical characteristics between two groups
| Characteristics | Intervention (n=35) | Control (n=41) | P |
|---|---|---|---|
| Gender, n (%) | |||
| Male | 15 (42.1) | 19 (46.3) | 0.819† |
| Female | 20 (57.9) | 22 (53.7) | |
| Age (years), mean±SD | 65.5±4.4 | 66.7±3.9 | 0.23†† |
| Education, n (%) | |||
| Less than high school graduate | 18 (51.4) | 25 (61) | 0.49† |
| High school graduate and more | 17 (48.6) | 16 (39) | |
| Marital status, n (%) | |||
| Single | 3 (8.6) | 9 (22) | 0.129† |
| Married | 32 (91.4) | 32 (78) | |
| Income, n (%) | |||
| Has income | 19 (54.3) | 23 (56.1) | 1.0† |
| Has no income | 16 (45.7) | 18 (43.9) | |
| Comorbidity, n (%) | |||
| Yes | 31 (88.6) | 31 (75.6) | 0.235† |
| No | 4 (11.4) | 10 (24.4) |
Data shown mean±SD or n (%). †Used of Chi-square test, ††Used of independent samples t-test. Single=widows and those who have never been married. Has income=retirees and freelancers; no income=unemployed and housewives. Comorbidities include diabetes, and chronic conditions such as hypothyroidism, cancer, and chronic respiratory disease. SD: Standard deviation
Outcomes
In the baseline, the mean score of most outcomes did not differ significantly between the two groups (P > 0.05). The results of comparison of changes between baseline and after the intervention are shown in Table 2, which indicates a significant improvement in the total scores of social capital in the intervention group (11.6 [8.21,14.98]) compared to control group (−2.36 [−4.93, 0.20]). Social capital in terms of tolerance for diversity was higher in the control group at baseline. However, we were able to adjust the baseline difference with the comparison of changes between baseline and after the intervention. When comparing the groups, a significant improvement was observed in the intervention group in terms of participation in local community, proactivity in a social context, feelings of trust and safety, neighborhood connections, and family and friends connections; however, no significant change was observed in the tolerance of diversity and value of life (P = 0.241, P = 0.928).
Table 2.
Comparison of outcomes at the baseline and one month after the intervention
| Variable | Baseline | P † | Intra group changes | P †† | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Intervention | Control | Intervention | Control | |||
| Total social capital | 78.09±10.00 | 79.63±13.22 | 0.563 | 11.6 (8.21-14.98) | −2.36 (−4.93-0.20) | <0.001 |
| Participation in local community | 12.40±3.29 | 12.15±3.69 | 0.752 | 3.42 (2.07-4.77) | −0.0.17 (−1.06-0.72) | <0.001 |
| Proactivity in a social context | 13.46±2.05 | 13.71±2.45 | 0.629 | 1.97 (1.16-2.77) | −1.19 (−1.99-−0.39) | <0.001 |
| Feelings of trust and safety | 13.77±2.53 | 14.29±3.59 | 0.462 | 1.37 (0.72-2.01) | 0.39 (−0.33-1.11) | 0.044 |
| Neighborhood connections | 12.94±2.73 | 12.63±3.64 | 0.675 | 2.51 (1.51-3.51) | −1.73 (−2.44-−1.01) | <0.001 |
| Family and friends connections | 7.91±2.29 | 7.68±2.44 | 0.672 | 1.65 (0.79-2.51) | −0.56 (−1.33-0.20) | <0.001 |
| Tolerance of diversity | 5.43±1.77 | 6.44±1.58 | 0.011 | 0.08 (−0.52-0.69) | 0.60 (−0.03-1.25) | 0.241 |
| Value of life | 5.86±1.11 | 6.39±1.32 | 0.064 | 0.34 (−0.05-0.74) | 0.36 (0.04-0.68) | 0.928 |
| other | 6.31±1.16 | 6.34±1.48 | 0.929 | 0.22 (−0.30-0.76) | 0.14 (−0.33-0.62) | 0.826 |
| Total quality of life | 31.09±4.66 | 31.34±5.26 | 0.828 | 1.91 (1.05-2.77) | 0.46 (−1.01-1.93) | 0.090 |
| Physical | 12.77±1.99 | 12.73±2.09 | 0.933 | 0.42 (0.01-0.83) | 0.43 (−0.13-1.00) | 0.976 |
| Mental | 18.31±3.40 | 18.61±4.15 | 0.734 | 1.48 (0.74-2.22) | 0.02 (−1.04-1.09) | 0.026 |
| Self-care | 136.46±7.04 | 136.34±7.13 | 0.944 | 11.02 (8.86-13.19) | 0.90 (−0.26-2.06) | <0.001 |
| Health literacy | 82.97±14.39 | 80.48±12.64 | 0.431 | 25.71 (20.59-30.83) | 2.56 (1.32-3.80) | <0.001 |
†Comparison of two groups at baseline, ††Comparison of group differences at one month after the intervention using independent samples t-test, Data shown mean±SD. SD: Standard deviation
The results of statistical analysis with independent samples t-test also showed that changes in the mental component of quality of life in the intervention group (1.48 [0.74, 2.22]) compared to the control group (0.02 [−1.04, 1.09]) demonstrate a significant improvement after the intervention (P = 0.026). Furthermore, the mean scores of Self care and health literacy in the intervention group showed a significant improvement 1 month after the completion of the intervention (P < 0.001) [Table 2]. Self-care showed significant improvement in the dimensions of physical self-care, emotional self-care, social self-care, and self-care during illness. In addition, health literacy improved in terms of access, understanding, appraisal, and decision-making (P < 0.05).
Discussion
This complex intervention seemed to improve social capital, the mental component of quality of life, self-care, and health literacy in older adults under coverage of urban primary health-care centers.
The intervention improved social capital in terms of participation in the local community, proactivity in a social context, feelings of trust and safety, neighborhood connections, and family and friends’ connections; however, no significant change was observed in the tolerance of diversity and value of life. Among these dimensions, social agency (proactivity in a social context) and sense of trust are the most important causal factors. Improving these two factors can lead to improving other dimensions such as the value of life and tolerance of diversity.[30] The community participation dimension is strongly related to the dimensions of friend and family relationships and neighborhood relationships.[31] In our results, the dimensions of tolerance of diversity and value of life did not show significant change. Changing these two factors may require longer and more fundamental interventions.
Previous studies using this questionnaire in the elderly population of Iran have often been descriptive cross-sectional and have shown low participation in the local community. However, a significant relationship has been observed between the level of mental health, quality of life, and social capital of the elderly in all dimensions.[27] Our results demonstrated a significant improvement in the mental dimension of quality of life in the intervention group compared to the control group. These promising results in improving social capital and quality of life are supported by previous studies which have shown that the most effective interventions to improve mental health of the elderly are multidimensional and social interventions.[5,32] These studies emphasize the effect of active group interventions on increasing social support and improving the health of the elderly. Indeed, loneliness and isolation of the elderly is one of the important factors in reducing the health of the elderly.[33,34] The WHO In “the Global Strategy and Action Plan on Aging and Health (2017) emphasizes the expansion of physical and social interventions based on social support for the elderly in communities. With this approach, primary health-care providers can be effective in reducing inequality and increasing the well-being of the vulnerable older adults.[35] However, the results of our study on improving social capital were different from the results of a similar study in deprived urban areas.[36] Our study was conducted in centers located in areas with a middle socioeconomic level, and the participants in our study probably had a high self-management and desire to participate in a community-based intervention. Previous researches have shown that socioeconomic low level and income can be a considerable barrier in social participation and self-management.[37] Repeating similar studies for the elderly in disadvantaged areas is recommended to evaluate results in other socioeconomic settings.
Furthermore, the intervention promoted self-care and health literacy generally. Self-care showed significant improvement in the dimensions of physical self-care, emotional self-care, social self-care, and self-care during illness. In addition, health literacy improved in terms of access, understanding, appraisal, and decision-making. The impact of complex interventions on improving self-care, health literacy, and the mental health of the community-dwelling older adults has been demonstrated in previous studies earlier.[16,20,38,39]
The important point in designing community-based interventions is to pay attention to dimensions of access and cocreation, so that they can be integrated into the services of the universal health network, while their clinical effectiveness is also measured.[23] Comprehensive health centers in the Iranian health system have expanded well in cities in recent years. With the development of the SIB electronic health network, the quality and quantity of service to citizens has been improved. Now, with the increase of the country's elderly population, new and more diverse programs must be designed and implemented using the cheap and available capacity of primary health-care centers.
This intervention can be used as a model for designing similar simple interventions that have high feasibility and can be implemented in short periods of several weeks in primary health centers by health workers.
Study strengths and limitations
One of the limitations of this study was the small number of health care centers involved in the study, due to budgetary and time constraints. On the other hand, the quasi-experimental nature of the study limits the generalizability of the study. However, the matching of intervention and control groups in demographic characteristics and outcomes at the baseline time point increases the power of study. In addition, selection of intervention and control groups from two different centers with geographical distance prevented contamination of samples.
The strength of the study is the implementation of a well-designed 12-week intervention program based on a precise protocol. Furthermore, the capacity to implement this intervention with the available facilities of primary health-care centers in urban neighborhoods provides the generalizability and extending it to other local contexts.
Conclusions
Our results show that community and group-based interventions with a variety of components in primary care centers can lead to an overall improvement in social capital, quality of life, and self-care and health literacy in community-dwelling older adults. However, it seems that increasing social capital in some dimensions requires continuous and longer interventions.
Financial support and sponsorship
This study has been supported by the Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study is a part of the clinical specialist thesis (Community Medicine), approved by the Isfahan University of Medical Sciences. We are grateful to older adult participants for their cooperation in this study.
References
- 1.World Health Organization. Integrated care for older people: Guidelines on community-level interventions to manage declines in intrinsic capacity. Geneva: World Health Organization; 2017. [PubMed] [Google Scholar]
- 2.Mehri N, Messkoub M, Kunkel S. Trends, determinants and the implications of population aging in Iran. Ageing Int. 2020;45:327–43. [Google Scholar]
- 3.Huppert FA. Psychological well-being: Evidence regarding its causes and consequences. Applied psychology: health and well being. 2009;1:137–64. [Google Scholar]
- 4.James Rippe., editor. Lifestyle Medicine. Boca Raton: Taylor & Francis; 2019. [Google Scholar]
- 5.Ten Bruggencate T, Luijkx KG, Sturm JJ. Social needs of older people: A systematic literature review. Ageing and Society. 2018;38:1745–70. [Google Scholar]
- 6.Geboers B, Reijneveld SA, Jansen CJ, de Winter AF. Health literacy is associated with health behaviors and social factors among older adults: Results from the LifeLines Cohort Study. J Health Commun. 2016;21:45–53. doi: 10.1080/10810730.2016.1201174. [DOI] [PubMed] [Google Scholar]
- 7.Solar O, Irwin A. Geneva, Switzerland: WHO Document Production Services; 2010. A conceptual framework for action on the social determinants of health. [Google Scholar]
- 8.Nyqvist F, Forsman AK. Netherlands: Springer; 2015. Social capital as a health resource in later life: The relevance of context. [Google Scholar]
- 9.Coll-Planas L, Nyqvist F, Puig T, Urrútia G, Solà I, Monteserín R. Social capital interventions targeting older people and their impact on health: A systematic review. J Epidemiol Community Health. 2017;71:663–72. doi: 10.1136/jech-2016-208131. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Self-care in the context of primary health care. Bangkok, Thailand: WHO Regional Office for South-East Asia; 2009. [Google Scholar]
- 11.Coll-Planas L, Blancafort S, Rojano X, Roqué M, Monteserín R. Promoting self-management, health literacy and social capital to reduce health inequalities in older adults living in urban disadvantaged areas: Protocol of the randomised controlled trial AEQUALIS. BMC Public Health. 2018;18:345. doi: 10.1186/s12889-018-5219-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manafo E, Wong S. Health literacy programs for older adults: A systematic literature review. Health Educ Res. 2012;27:947–60. doi: 10.1093/her/cys067. [DOI] [PubMed] [Google Scholar]
- 13.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 14.Findley A. Low health literacy and older adults: Meanings, problems, and recommendations for social work. Soc Work Health Care. 2015;54:65–81. doi: 10.1080/00981389.2014.966882. [DOI] [PubMed] [Google Scholar]
- 15.de Wit L, Fenenga C, Giammarchi C, di Furia L, Hutter I, de Winter A, et al. Community-based initiatives improving critical health literacy: A systematic review and meta-synthesis of qualitative evidence. BMC Public Health. 2017;18:40. doi: 10.1186/s12889-017-4570-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin SC, Chen IJ, Yu WR, Lee SD, Tsai TI. Effect of a community-based participatory health literacy program on health behaviors and health empowerment among community-dwelling older adults: A quasi-experimental study. Geriatr Nurs. 2019;40:494–501. doi: 10.1016/j.gerinurse.2019.03.013. [DOI] [PubMed] [Google Scholar]
- 17.O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9:e029954. doi: 10.1136/bmjopen-2019-029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Detels R GM, Abdool Karim Q, Chuan Tan C. 6th ed. UK: Oxford University Press; 2015. Introduction to development and evaluation of complex multicomponent interventions. Oxford Textbook of Global Public Health; pp. 751–60. [Google Scholar]
- 19.Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ. 2007;334:455–9. doi: 10.1136/bmj.39108.379965.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong KC, Wong FKY, Yeung WF, Chang K. The effect of complex interventions on supporting self-care among community-dwelling older adults: A systematic review and meta-analysis. Age Ageing. 2018;47:185–93. doi: 10.1093/ageing/afx151. [DOI] [PubMed] [Google Scholar]
- 21.Srivarathan A, Jensen AN, Kristiansen M. Community-based interventions to enhance healthy aging in disadvantaged areas: Perceptions of older adults and health care professionals. BMC Health Serv Res. 2019;19:7. doi: 10.1186/s12913-018-3855-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berenguera A, Pons-Vigués M, Moreno-Peral P, March S, Ripoll J, Rubio-Valera M, et al. Beyond the consultation room: Proposals to approach health promotion in primary care according to health-care users, key community informants and primary care centre workers. Health Expect. 2017;20:896–910. doi: 10.1111/hex.12530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnstone G, Dickins M, Lowthian J, Renehan E, Enticott J, Mortimer D, et al. Interventions to improve the health and wellbeing of older people living alone: A mixed-methods systematic review of effectiveness and accessibility. Ageing & Society. 2019;417:1–50. [Google Scholar]
- 24.Salimi F, Garmaroudi G, Hosseini SM, Batebi AJ. Effect of self–care educational program to improving quality of life among elderly referred to health centers in Zanjan J Educ Community Health. 2015;2:28–37. [Google Scholar]
- 25.Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S. The Iranian version of 12-item Short Form Health Survey (SF-12): Factor structure, internal consistency and construct validity. BMC Public Health. 2009;9:341. doi: 10.1186/1471-2458-9-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Onyx J, Bullen PJ. Measuring social capital in five communities. The journal of applied behavioral science. 2000;36:23–42. [Google Scholar]
- 27.Eftekharin R, Kaldi A, Sam S, Sahaf R, Vatan RF. Validity and reliability of Persian version of Onyx Social Capital Scale in elderly people. Iran J ageing. 2016;11:174–89. [Google Scholar]
- 28.Montazeri A, Tavousi M, Rakhshani F, Azin SA, Jahangiri K, Ebadi M, et al. Health Literacy for Iranian Adults (HELIA): Development and psychometric properties. Payesh. 2014;13:589–99. [Google Scholar]
- 29.Pak MH, Hashemlo LJ. Design and psychometric properties of a selfcare questionnaire for the elderly. Salmand: Iranian Journal of Ageing. 2015;10:120–31. [Google Scholar]
- 30.Ievdokymov V, Lehenchuk S, Zakharov D, Andrusiv U, Usatenko O, Kovalenko L. Social capital measurement based on “The value explorer” method. Manag Sci Lett. 2020;10:1161–8. [Google Scholar]
- 31.Bullen P, Onyx J. Social capital: The measurement tool. PO Box 181, Coogee, NSW, 2034: Citeseer. 2007 [Google Scholar]
- 32.Seah B, Kowitlawakul Y, Jiang Y, Ang E, Chokkanathan S, Wang W. A review on healthy ageing interventions addressing physical, mental and social health of independent community-dwelling older adults. Geriatr Nurs. 2019;40:37–50. doi: 10.1016/j.gerinurse.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 33.Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: A systematic review. BMC Public Health. 2011;11:647. doi: 10.1186/1471-2458-11-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Markle-Reid M, Ploeg J, Fraser KD, Fisher KA, Bartholomew A, Griffith LE, et al. Community program improves quality of life and self-management in older adults with diabetes mellitus and comorbidity. J Am Geriatr Soc. 2018;66:263–73. doi: 10.1111/jgs.15173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Geneva: World Health Organization; 2017. World Health Organization. Global strategy and action plan on ageing and health. [Google Scholar]
- 36.Blancafort Alias S, Monteserín Nadal R, Moral I, Roqué Fígols M, Rojano I Luque X, Coll-Planas L. Promoting social capital, self-management and health literacy in older adults through a group-based intervention delivered in low-income urban areas: Results of the randomized trial AEQUALIS. BMC Public Health. 2021;21:84. doi: 10.1186/s12889-020-10094-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meek KP, Bergeron CD, Towne SD, Ahn S, Ory MG, Smith ML. Restricted social engagement among adults living with chronic conditions. Int J Environ Res Public Health. 2018;15:158. doi: 10.3390/ijerph15010158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uemura K, Yamada M, Okamoto H. The effectiveness of an active learning program in promoting a healthy lifestyle among older adults with low health literacy: A randomized controlled trial. Gerontology. 2021;67:25–35. doi: 10.1159/000511357. [DOI] [PubMed] [Google Scholar]
- 39.Wong AK, Wong FK, Chang K. Effectiveness of a community-based self-care promoting program for community-dwelling older adults: A randomized controlled trial. Age Ageing. 2019;48:852–8. doi: 10.1093/ageing/afz095. [DOI] [PubMed] [Google Scholar]


