Abstract
Background/purpose
Surgical orthodontic treatment is recommended for patients with severe dentoskeletal discrepancies, while camouflage orthodontic treatment is recommended for patients with mild to moderate discrepancies. However, the decision as to which treatment should be chosen is complicated. The purpose of this study was to determine differences in masticatory function in patients who underwent camouflage and surgical orthodontic treatment for skeletal Class III malocclusion, as well as the usefulness of Wits appraisal in treatment decision based on masticatory functional analysis.
Materials and methods
The study subjects were 45 patients with skeletal Class III malocclusion (15 cases with camouflage orthodontics and 30 cases with orthognatic surgery) and 12 individuals with normal occlusion. We analyzed the pre-treatment records of electromyographic activities of masseter and temporalis muscles and jaw movements.
Results
There were no significant differences in various functional measurements between the camouflage and surgery groups. However, there were significant but not strong correlations between ANB and both masseter muscle activity (r = 0.36, p < 0.01) and expression ratio of abnormal chewing (r = −0.54, p < 0.01). Division of patients into two groups using a cutoff value of −6.0 mm for Wits appraisal showed a significant difference in masseter muscle activity between −6.0 mm or less group and the control (p < 0.01) but none between more than −6.0 mm group and the control.
Conclusion
Camouflage orthodontic treatment is inappropriate for patients with relatively severe dentoskeletal discrepancies. Wits appraisal of −6.0 mm is a potentially useful parameter for treatment decision.
Keywords: Surgical orthodontic treatment, Camouflage orthodontic treatment, Skeletal class III, Masticatory function, Wits appraisal
Introduction
Malocclusion with skeletal Class III is characterized by Angle Class III, anterior crossbite, compensatory inclination of incisors for skeletal discrepancy and uni- or bilateral posterior crossbite due to the transverse maxillary deficiency. Several studies have demonstrated that patients with skeletal Class III malocclusion show disorders of masticatory function associated with the malocclusion and jaw deformity; muscle activity,1, 2, 3 jaw movement,2, 3, 4, 5 masticatory efficacy,1 and bite force.2 However, the effect of the severity of skeletal discrepancy on masticatory functional disorder is not yet clear.
Skeletal Class III malocclusion can be the result of pure mandibular prognathism or maxillary hypoplasia and retrognathism, or a combination of the two.6 Surgical orthodontic treatment is recommended for non-growing patients with severe dentoskeletal discrepancies, while camouflage orthodontic treatment is recommended for patients presenting with mild to moderate discrepancies. However, the decision as to which treatment should be chosen is not always an easy task especially in borderline cases.7 For this reason, the treatment outcome of camouflage and surgical orthodontic treatment has been studied.7, 8, 9, 10, 11 The results of such studies indicated that Wits appraisal is a useful parameter for identifying cases suitable for camouflage or surgical orthodontic treatment.7,9,11 Wits appraisal is a cephalometric parameter representing the perpendicular distance between points A and B on the occlusal plane, and is a marker of the severity of antero-posterior jaw disharmony.12 Eslami et al.7 reported that surgical orthodontic treatment is recommended for cases with Wits appraisal of less than −5.8 mm. However, there is no protocol at present that can help in selecting the most appropriate treatment for patients with skeletal Class III malocclusion. Moreover, as far as we know, there is no study that examined the characteristics of masticatory functions in skeletal Class III cases who received camouflage and surgical orthodontic treatment.
The purpose of this study was first to determine pre-treatment differences in the masticatory function in patients with skeletal Class III malocclusion who underwent camouflage and surgical orthodontic treatment. This part of the study served to assess the relationship between skeletal discrepancy and masticatory functional disorders. The second purpose of the study was to establish the usefulness of Wits appraisal in treatment selection of patients with skeletal Class III malocclusion, based on masticatory function. The tested hypothesis was that surgical orthodontic cases exhibit more severe dentoskeletal problems and masticatory functional disorders than camouflage treatment cases.
Materials and methods
Subjects
Forty-five patients in the permanent dentition with skeletal Class III malocclusion (ANB of less than 1° and unilateral or bilateral Angle Class III molar relationship) and 12 individuals with normal occlusion were the subjects of this study. None had cleft palate, craniofacial syndrome, or severe skeletal asymmetry (≥4 mm mandibular deviation). Patients with skeletal Class III malocclusion were divided into two groups; patients of the surgery group underwent surgical orthodontic treatment (10 males and 20 females, mean age 22.7 ± 7.2 years, −8.8° ≤ ANB≤0.7°) while those of the camouflage group received non-surgical camouflage orthodontic treatment (5 males and 10 females, mean age 22.7 ± 6.4 years, −1.9° ≤ ANB≤0.9°). The decision on the selection of camouflage or surgical orthodontic treatment was conducted at the Department of Orthodontics of Tokushima University Hospital by one board-certified orthodontist, based on the symptoms reported by the patient, facial esthetics, and severity of dentoskeletal malocclusion as assessed by clinical examination and cephalometric analysis especially in ANB and dental compensation of incisors. Wits appraisal has been rarely used in our treatment decision.
Twelve volunteers were the subjects of the control group (4 males and 8 females, mean age 23.9 ± 1.5 years, 2.0° ≤ ANB≤5.0°), who fulfilled the following criteria: no skeletal or dental malocclusion, no symptoms of temporomandibular disorders, and no previous orthodontic treatment.
All clinical data used in this study were from the medical records and measured before treatment. Dentofacial morphology was evaluated on the lateral cephalogram. Table 1 shows parameters measured in the cephalometric analysis. The cephalometric variables were measured twice; 1 week apart, by a single examiner. To test intra-rater reliability, single measure intraclass correlation coefficients (ICC (1, 1)) were calculated and all were more than 0.9, indicating a small method error.
Table 1.
Parameters measured on the cephalogram.
| Parameter | Definition |
|---|---|
| SNA (o) | Angle between S–N and N-A planes |
| SNB (o) | Angle between S–N and N–B planes |
| ANB (o) | Angle between N-A and N–B planes |
| FMA (o) | Angle between mandibular and FH planes |
| Gonial Angle (o) | Angle between the mandibular and ramus planes |
| Go-Me (mm) | Length of mandibular corpus |
| U1 to SN (o) | Angle between the long axis of maxillary central incisor and SN plane |
| L1 to mandibular plane (o) | Angle between the long axis of mandibular central incisor and mandibular plane |
| Overjet (mm) | Horizontal distance between incisal edges (U1 and L1) |
| Overbite (mm) | Vertical distance between incisal edges (U1 and L1) |
| Wits appraisal (mm) | Distance from AO to BO on the occlusal plane |
S: sella, N: nasion, Or: orbitale, Po: porion, Ar: articulare, Go: gonion, Me: menton, A: point A, B: point B, U1: tip of upper incisor, L1: tip of lower incisor, AO: point contacted perpendicularly on the occlusal plane from point A, BO: point contacted perpendicularly on the occlusal plane from point B.
The post hoc power analysis in this study showed average effect size = 0.56 and power of 1-β = 0.77 (sample size = 57, α = 0.05), indicating that the number of participants was to a large extent appropriate. The study protocol was approved by the Ethics Committee of Tokushima University Hospital (#3542) and a signed informed consent was obtained from each participant.
Measurements and evaluation of muscle activity and jaw movement
Muscle activity and jaw movement were recorded as described previously13 with computerized mandibular scanner and electromyograph (K7 Evaluation System; Myotronics-Noromed, Inc., Kent, WA, USA). Electromyographic (EMG) activities of the masseter and anterior temporalis muscles were recorded bilaterally during 3-s maximum voluntary clenching (MVC) at the maximum intercuspal position, using bipolar surface electrodes. The subject was instructed to clench the teeth with maximum effort twice with 7-s interval rest. The mean value of the EMG amplitude was calculated during the median 2 s of the 3-s MVC. The larger mean EMG amplitude achieved on each side was regarded as representative and the average value of bilateral representative measurements was used as the muscle activity value for the individual.
Movement of the mandibular incisal point was recorded during unilateral chewing of the gum (XYLITOL; OralCare Inc., Tokyo, Japan) for 30 s on both the right and left sides and bilateral normal gum chewing for 30 s. Ten chewing strokes from the 5th to the 14th on each side were used to evaluate the jaw movement based on the least variability in path and rhythm.14 The chewing stroke was classified into five specific types by visual inspection according to the cycle shape of the mandibular incisal point movement on the frontal plane, according to the classification of Nie et al.;14 normal type, concave type, reverse type, crossover type and chopping type. The latter four types were regarded as abnormal chewing patterns. The number of each chewing type in 10 strokes was counted and the frequency of each chewing type was investigated. The average numbers of strokes on the right and left sides were used as the number of stroke for the individual.
We used the method described previously in detail for analysis.13 The relative contributions of the masseter and temporalis muscles were assessed by the activity index (AI). A negative AI value corresponded to relatively larger contribution of the temporalis muscle activity than masseter muscle. AI was calculated by the following formula:
| AI= (masseter muscle activity - temporalis muscle activity) × 100 / (masseter muscle activity + temporalis muscle activity) (%) |
The error index (EI) was used to evaluate jaw movement patterns. EI was calculated as the ratio of the number of abnormal chewing types to the total chewing strokes, using the following formula:
| EI = number of strokes showing abnormal chewing type × 100 / number of total strokes (%) |
Statistical analysis
Results were expressed as mean ± standard deviation. Differences between groups were analyzed by analysis of variance (ANOVA). When ANOVA was significant, the Bonferroni/Dunn procedure was performed as a post hoc test. Regression analysis was used to determine the relationship between ANB and masticatory functions. In all tests, a p value less than 0.05 was considered statistically significant. ICC (1, 1) was calculated to test intra-observer reliability. All statistical tests were conducted using IBM SPSS Statistics 25 (IBM Japan, Tokyo, Japan). G∗power 3.1 (Heinrich Heine University Düsseldorf, Düsseldorf, Germany) was used for power analysis to calculate effect size and power (1-β).15
Results
Characteristic of masticatory function in camouflage and surgical orthodontic cases
Table 2 shows the cephalometric parameters for each group. There were significant differences in ANB, L1 to mandibular plane, overbite and Wits appraisal between the control and camouflage group (p < 0.01, each), and significant differences in gonial angle (p < 0.05), SNB, ANB, L1 to mandibular plane, overjet, overbite and Wits appraisal (p < 0.01, each) between the control and surgery group. Moreover, Wits appraisal (p < 0.05), ANB and overjet (p < 0.01, each) were significantly smaller in the surgery group than in the camouflage group. The surgical case showed more severe skeletal Class III with dental compensation of incisors.
Table 2.
Comparison of cephalometric parameters measured before treatment in the three study groups.
| Parameter | Control | Camouflage | Surgery |
|---|---|---|---|
| SNA (o) | 83.2 ± 2.1 | 81.8 ± 2.7 | 80.6 ± 3.7 |
| SNB (o) | 79.1 ± 2.3 | 82.3 ± 2.9 | 83.3 ± 3.7∗∗ |
| ANB (o) | 4.1 ± 1.0 | −0.5 ± 0.9∗∗ | −2.8 ± 2.4∗∗†† |
| FMA (o) | 27.4 ± 5.8 | 29.6 ± 5.7 | 28.3 ± 6.8 |
| Gonial Angle (°) | 121.1 ± 8.2 | 126.6 ± 7.4 | 128.3 ± 8.7∗ |
| Go-Me (mm) | 76.3 ± 3.5 | 77.0 ± 4.6 | 80.2 ± 6.7 |
| U1 to SN (o) | 106.3 ± 4.0 | 110.6 ± 5.8 | 110.2 ± 8.6 |
| L1 to mandibular plane (o) | 99.9 ± 9.5 | 84.0 ± 7.3∗∗ | 81.4 ± 8.7∗∗ |
| Overjet (mm) | 3.3 ± 0.8 | 0.9 ± 2.8 | −1.8 ± 2.8∗∗†† |
| Overbite (mm) | 3.4 ± 1.2 | 1.0 ± 1.5∗∗ | 1.0 ± 2.1∗∗ |
| Wits appraisal (mm) | −0.3 ± 2.3 | −8.4 ± 3.6∗∗ | −11.2 ± 3.5∗∗† |
Values are mean ± SD. ∗p < 0.05, ∗∗p < 0.01, compared with the control group. †p < 0.05, ††p < 0.01, compared with the camouflage and surgery groups.
The masseter muscle activities of both the camouflage and surgery groups were significantly lower than that of the control group (Fig. 1A; p < 0.01). A similar tendency was noted in the temporalis muscle activity but there was no significant difference among the three groups (Fig. 1A). The AI value of the control group was 19.0 ± 11.7%, indicating dominance of masseter muscle activity relative to the temporalis muscle (Fig. 1B). The AI values of both the camouflage (p < 0.05) and surgery groups (p < 0.01) were significantly lower than that of the control group. The EI values of both the camouflage and surgery groups were significantly higher than that of the control group (Fig. 1C; p < 0.01).
Figure 1.
Comparison of (A) muscle activities of the masseter and temporalis muscles, (B) activity index, and (C) error index among the control group, camouflage group, and surgery group. Values are mean ± SD. ∗p < 0.05, ∗∗p < 0.01 (ANOVA).
Statistically significant but not strong correlation were observed between the ANB and masseter muscle activity (Fig. 2A; r = 0.36, p < 0.01), AI (Fig. 2B; r = 0.29, p < 0.05) and EI (Fig. 2C; r = −0.54, p < 0.01), indicating that the more severe skeletal Class III, the lower the masseter muscle activity and the more expression of abnormal chewing strokes.
Figure 2.

Relationship between ANB and masticatory function: (A) masseter muscle activity, (B) activity index, and (C) error index.
Masticatory function in skeletal Class III cases based on wits appraisal
In the next series of studies, we evaluated the masticatory function in all 45 patients with skeletal Class III malocclusion after dividing the patients into two groups based on the value of Wits appraisal, and then assessed the usefulness of Wits appraisal in treatment decision in skeletal Class III malocclusion.
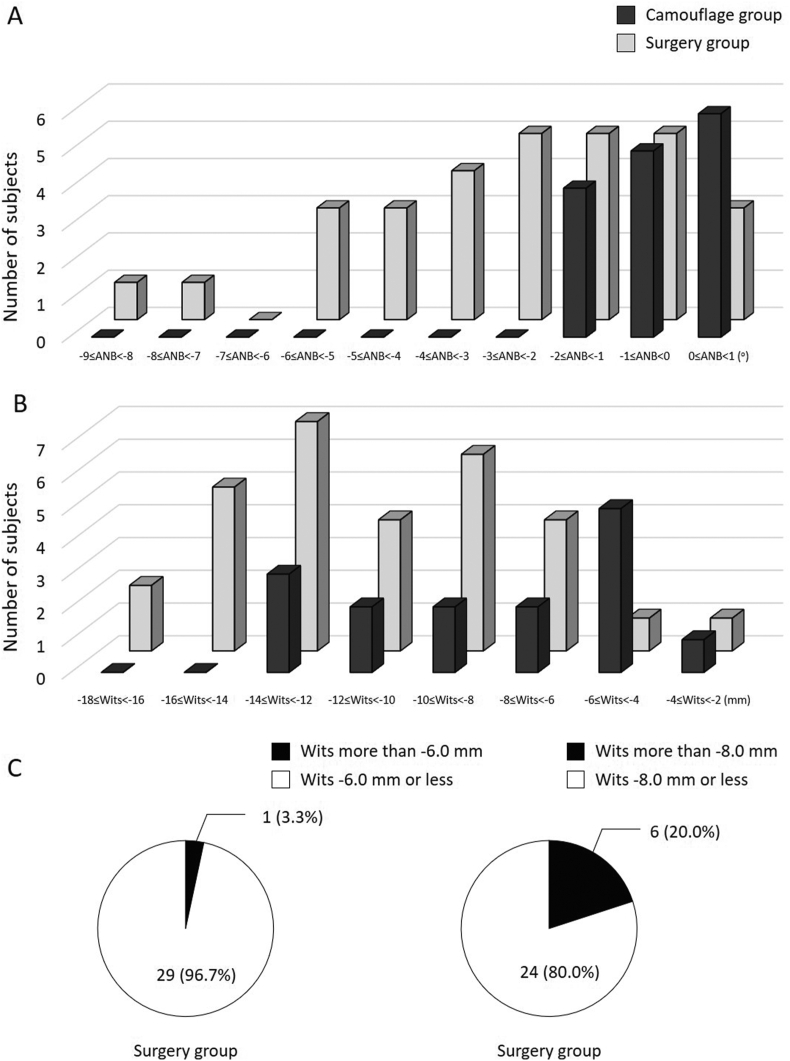
Both ANB and Wits appraisal tended to be smaller in the surgery than camouflage group (Fig. 3A and B) However, the distribution of Wits appraisal was wider in the camouflage group than ANB and overlapped widely between the surgery and camouflage groups (Fig. 3B). Wits appraisal was more than −6.0 mm in only a single case of the surgery group, while it was more than −8.0 mm in 20% of the surgery group (Fig. 3C). Similar to the ANB, Wits appraisal correlated significantly but not strongly with masseter muscle activity (Fig. 4A; r = 0.39, p < 0.01), AI (Fig. 4B; r = 0.29, p < 0.05) and EI (Fig. 4C; r = −0.57, p < 0.01).
Figure 3.
(A) Frequency distribution histogram of ANB in the camouflage and surgery groups. (B) Frequency distribution histogram of Wits appraisal in the camouflage and surgery groups. (C) Number of cases of the surgery group based on Wits appraisal of both −6.0 and −8.0 mm.
Figure 4.

Relationship between Wits appraisal and masticatory function: (A) masseter muscle activity, (B) activity index, and (C) error index.
Dividing the skeletal Class III cases using the Wits appraisal cutoff value of −6.0 mm showed significant differences in masseter muscle activity and the AI value in only the group with Wits appraisal of −6.0 mm or less and the control group (Fig. 5A and B; p < 0.01). On the other hand, the AI values of the subjects with Wits appraisal of more than −6.0 mm were positive, indicating masseter muscle dominance. The EI values of both skeletal Class III groups were significantly higher than the control group (Fig. 5C; p < 0.01). In contrast, using −8.0 mm as the Wits appraisal cutoff value, both skeletal Class III groups showed similar functional performance, i.e., temporalis muscle dominance and high expression of abnormal chewing type (Fig. 6).
Figure 5.
(A) Muscle activities of masseter and temporalis muscles, (B) activity index, and (C) error index based on Wits appraisal −6.0 mm. Values are mean ± SD. ∗∗p < 0.01 (ANOVA).
Figure 6.
(A) Muscle activities of masseter and temporalis muscles, (B) activity index, and (C) error index based on Wits appraisal −8.0 mm. Values are mean ± SD. ∗p < 0.05, ∗∗p < 0.01 (ANOVA).
Discussion
Previous studies identified lower masseter muscle activity with dominance of temporalis muscle and higher expression of abnormal chewing in patients with skeletal Class III malocclusion compared to normal subjects.1, 2, 3, 4, 5 These findings might be due to the anteriorly positioned mandible in skeletal Class III cases. The angel between masseter muscle direction and the FH plane is larger in prognathism patients compared with normal subjects due to the anteriorly positioned mandible.16 That means the masseter muscle of skeletal class III cases directs more vertically. Therefore, it seems that their vertical direction of the masseter muscle interferes with efficient mandibular movement and as a result, skeletal Class III cases express more abnormal chewing strokes, especially with linear opening and closing patterns, compared to normal subjects. Moreover, compared to normal subjects, skeletal Class III cases exhibit a lower bite force and lower masseter muscle activity, based on the smaller cross-sectional area of the masseter muscle.17 Consequently, masticatory muscle activity and jaw movement are influenced by the anatomical structure: horizontal and vertical jaw discrepancy. Our study provided support to the above results, namely, the significant correlations between ANB and both AI and EI, indicating that the more severe skeletal Class III, the lower masseter muscle activity and the more expression of abnormal chewing strokes.
For patients with mandibular prognathism, previous studies demonstrated that improvement of masticatory function to the level seen in healthy subjects with normal occlusion occurs several years after orthognathic surgery18,19 and post-surgical functional training by functional de-compensation is recommended in such patients.13 However, it is noteworthy that patients who undergo surgical orthodontic treatment report better quality of life and more positive esthetic self-perception compared to before treatment.20 Therefore, skeletal discrepancy should be corrected to improve masticatory function and, in that sense, camouflage orthodontic treatment is unlikely to be effective in patients with severe skeletal discrepancy. In treatment planning for skeletal Class III malocclusion, it would be preferable to emphasize the importance of improvement of function.
There is no standard protocol at present for selection of either camouflage or surgical orthodontic treatment and in fact the issue is controversial especially in treatment planning of borderline cases with skeletal Class III malocclusion.7 Camouflage orthodontic treatment is a routine approach for treating adolescents and adults with Class III malocclusion with a mild to moderate skeletal discrepancy21 and it is beneficial for patients who find it difficult to accept orthognathic surgery.22 In this regard, the strategy of camouflage orthodontic treatment in skeletal Class III malocclusion usually involves proclination of the maxillary incisors and retroclination of the mandibular incisors to improve dental occlusion, but the technique might not correct the underlying skeletal problem.23 In addition, some of the patients who undergo camouflage orthodontic treatment and are later not satisfied with treatment results, subsequently opt for surgical orthodontic treatment.24 Camouflage orthodontic treatment has the advantages of attaining acceptable occlusion and esthetics non-surgically but careful consideration is necessary for its application.
Our study was designed to clarify the influence of the degree of skeletal discrepancy on masticatory function by comparing masticatory function between patients who underwent camouflage and surgical orthodontic treatment. Our hypothesis that surgical orthodontic cases exhibit more severe dentoskeletal problems and masticatory functional disorder than camouflage orthodontic cases was rejected. In the present study, surgical orthodontics cases certainly showed more severe dentoskeletal problems than camouflage orthodontic cases. However, there were no significant differences in all functional measurements between patients of the two treatment groups. Therefore, as the next analysis, we conducted regression analysis to determine the relationship between ANB and masticatory function. The results showed significant correlations between ANB and both AI and EI. These results suggest that while many patients with relatively severe dentoskeletal discrepancy should have undergone surgical orthodontic treatment, they received camouflage orthodontic treatment for some reasons, probably patient refusal of surgery and desire for non-invasive approach.
Although ANB is one of the commonly used cephalometric variables for classifying skeletal type, it was reported that Wits appraisal can be used as a critical diagnostic parameter for selection of patients for either camouflage or surgical orthodontic treatment.7,9,11 Wits appraisal was proposed by Jacobson12 who described this parameter to provide reliable indication of the extent or severity of antero-posterior skeletal disharmony of the jaws associated with the jaws/occlusal plane relationship.12 Our study showed different distribution patterns between ANB and Wits appraisal. The distribution of Wits appraisal in the camouflage group was wider than that of ANB and overlapped widely with each group. That means exclusion of Wits appraisal in any treatment plan could lead to underestimation of dentoskeletal discrepancy. In fact, since Wits appraisal was rarely applied in our treatment planning, Wits appraisal of −8.4 mm in our camouflage group was smaller than that reported in previous studies of camouflage cases: −4.4 mm,21 -4.6 mm,9 -4.8 mm,7 -6.9 mm,10 and −7.0 mm.11 Eslami et al.7 reported that skeletal Class III cases with more than −5.8 mm Wits appraisal could be treated successfully by camouflage orthodontic treatment, while surgical orthodontic treatment was recommended for cases with less than −5.8 mm. Therefore, in the next series of experiments, we evaluated the masticatory functions in all patients with skeletal Class III malocclusion after dividing them into two groups based on the value of Wits appraisal. In our study using Wits appraisal of −6.0 mm as the cutoff value, only one patient had Wits appraisal of more than −6.0 mm in the surgery group. Moreover, there was no significant difference in masseter muscle function between the control and patients with skeletal Class III malocclusion and Wits appraisal of more than −6.0 mm. These results suggest that the Wits appraisal cutoff value of −6.0 mm can be potentially useful for treatment decision in patients with skeletal Class III malocclusion, from the point of view of the masticatory functional analysis. In this regard, Stellzig-Eisenhauer et al.9 reported that Wits appraisal was −4.5 ± 0.2 mm in correctly classified patients of the non-surgery group, −13.0 ± 0.5 mm in correctly classified patients of the surgery group, and −7.0 ± 0.5 mm in incorrectly classified patients of the surgery group. As mentioned above, carful approach is needed in treatment planning of patients with Wits appraisal of around 6.0 mm.
In conclusion, we demonstrated in the present study that the more severe skeletal Class III was, the more severe masticatory functional disorder was, however there was no significant difference in masticatory function between camouflage and surgical orthodontic cases. These results suggest that camouflage orthodontic treatment was selected inappropriately in many cases with relatively severe dentoskeletal discrepancy, even though skeletal discrepancy should have been corrected. For appropriate treatment planning, Wits appraisal of −6.0 mm is a potentially useful cutoff value for the selection of either camouflage or surgical orthodontic treatment for patients with skeletal Class III malocclusion, from the point of view of masticatory functional analysis.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
The authors are grateful to the staff of the Department of Orthodontics and Dentofacial Orthopedics, Institute of Biomedical Sciences, Tokushima University Graduate School, for the kind cooperation and advice. This work was supported in part by a grant from Japanese Dental Science Federation, JDSF-DSP1-2019-207-1.
References
- 1.Kobayashi T., Honma K., Shingaki S., Nakajima T. Changes in masticatory function after orthognathic treatment in patients with mandibular prognathism. Br J Oral Maxillofac Surg. 2001;39:260–265. doi: 10.1054/bjom.2000.0576. [DOI] [PubMed] [Google Scholar]
- 2.Nakata Y., Ueda H.M., Kato M., et al. Changes in stomatognathic function induced by orthognathic surgery in patients with mandibular prognathism. J Oral Maxillofac Surg. 2007;65:444–451. doi: 10.1016/j.joms.2005.12.071. [DOI] [PubMed] [Google Scholar]
- 3.Kubota T., Yagi T., Tomonari H., Ikemori T., Miyawaki S. Influence of surgical orthodontic treatment on masticatory function in skeletal Class III patients. J Oral Rehabil. 2015;42:733–741. doi: 10.1111/joor.12307. [DOI] [PubMed] [Google Scholar]
- 4.Ueki K., Marukawa K., Shimada M., Nakagawa K., Yamamoto E., Niizawa S. Changes in the chewing path of patients in skeletal class III with and without asymmetry before and after orthognathic surgery. J Oral Maxillofac Surg. 2005;63:442–448. doi: 10.1016/j.joms.2004.06.059. [DOI] [PubMed] [Google Scholar]
- 5.Takeda H., Nakamura Y., Handa H., Ishii H., Hamada Y., Seto K. Examination of masticatory movement and rhythm before and after surgical orthodontics in skeletal Class III patients with unilateral posterior cross-bite. J Oral Maxillofac Surg. 2009;67:1844–1849. doi: 10.1016/j.joms.2009.04.027. [DOI] [PubMed] [Google Scholar]
- 6.Ngan P., Moon W. Evolution of Class III treatment in orthodontics. Am J Orthod Dentofacial Orthop. 2015;148:22–36. doi: 10.1016/j.ajodo.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Eslami S., Faber J., Fateh A., Sheikholaemmeh F., Grassia V., Jamilian A. Treatment decision in adult patients with class III malocclusion: surgery versus orthodontics. Prog Orthod. 2018;19:28. doi: 10.1186/s40510-018-0218-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kerr W.J., Miller S., Dawber J.E. Class III malocclusion: surgery or orthodontics? Br J Orthod. 1992;19:21–24. doi: 10.1179/bjo.19.1.21. [DOI] [PubMed] [Google Scholar]
- 9.Stellzig-Eisenhauer A., Lux C.J., Schuster G. Treatment decision in adult patients with Class III malocclusion: orthodontic therapy or orthognathic surgery? Am J Orthod Dentofacial Orthop. 2002;122:27–37. doi: 10.1067/mod.2002.123632. [DOI] [PubMed] [Google Scholar]
- 10.Troy B.A., Shanker S., Fields H.W., Vig K., Johnston W. Comparison of incisor inclination in patients with Class III malocclusion treated with orthognathic surgery or orthodontic camouflage. Am J Orthod Dentofacial Orthop. 2009;135:146. doi: 10.1016/j.ajodo.2008.07.012. e1-9. [DOI] [PubMed] [Google Scholar]
- 11.Martinez P., Bellot-Arcís C., Llamas J.M., Cibrian R., Gandia J.L., Paredes-Gallardo V. Orthodontic camouflage versus orthognathic surgery for class III deformity: comparative cephalometric analysis. Int J Oral Maxillofac Surg. 2017;46:490–495. doi: 10.1016/j.ijom.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Jacobson A. The "Wits" appraisal of jaw disharmony. Am J Orthod. 1975;67:125–138. doi: 10.1016/0002-9416(75)90065-2. [DOI] [PubMed] [Google Scholar]
- 13.Kawai N., Shibata M., Watanabe M., Horiuchi S., Fushima K., Tanaka E. Effects of functional training after orthognathic surgery on masticatory function in patients with mandibular prognathism. J Dent Sci. 2020;15:419–425. doi: 10.1016/j.jds.2020.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nie Q., Kanno Z., Xu T., Lin J., Soma K. Clinical study of frontal chewing patterns in various crossbite malocclusions. Am J Orthod Dentofacial Orthop. 2010;138:323–329. doi: 10.1016/j.ajodo.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 15.Faul F., Erdfelder E., Lang A.G., Buchner A.G. ∗Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 16.Ariji Y., Kawamata A., Yoshida K., et al. Three-dimensional morphology of the masseter muscle in patients with mandibular prognathism. Dentomaxillofacial Radiol. 2000;29:113–118. doi: 10.1038/sj/dmfr/4600515. [DOI] [PubMed] [Google Scholar]
- 17.Lee D.H., Yu H.S. Masseter muscle changes following orthognathic surgery: a long-term three-dimensional computed tomography follow-up. Angle Orthod. 2012;82:792–798. doi: 10.2319/111911-717.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwase M., Ohashi M., Tachibana H., Toyoshima T., Nagumo M. Bite force, occlusal contact area and masticatory efficiency before and after orthognathic surgical correction of mandibular prognathism. Int J Oral Maxillofac Surg. 2006;35:1102–1107. doi: 10.1016/j.ijom.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 19.Yamashita Y., Otsuka T., Shigematsu M., Goto M. A long-term comparative study of two rigid internal fixation techniques in terms of masticatory function and neurosensory disturbance after mandibular correction by bilateral sagittal split ramus osteotomy. Int J Oral Maxillofac Surg. 2011;40:360–365. doi: 10.1016/j.ijom.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 20.Palomares N.B., Celeste R.K., Miguel J.A. Impact of orthosurgical treatment phases on oral health-related quality of life. Am J Orthod Dentofacial Orthop. 2016;149:171–181. doi: 10.1016/j.ajodo.2015.07.032. [DOI] [PubMed] [Google Scholar]
- 21.Blagitz M.N., Almeida G.A., Normando D. Factors associated with the stability of compensatory orthodontic treatment of Class III malocclusion in the permanent dentition. Am J Orthod Dentofacial Orthop. 2020;158:e63–e72. doi: 10.1016/j.ajodo.2020.06.030. [DOI] [PubMed] [Google Scholar]
- 22.Lin J., Gu Y. Preliminary investigation of nonsurgical treatment of severe skeletal Class III malocclusion in the permanent dentition. Angle Orthod. 2003;73:401–410. doi: 10.1043/0003-3219(2003)073<0401:PIONTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Burns N.R., Musich D.R., Martin C., Razmus T., Gunel E., Ngan P. Class III camouflage treatment: what are the limits? Am J Orthod Dentofacial Orthop. 2010;137:9. doi: 10.1016/j.ajodo.2009.05.017. e1-13. [DOI] [PubMed] [Google Scholar]
- 24.Lisboa C.O., Borges M.S., Medeiros P.J.D., Motta A.T., Mucha J.N. Orthodontic-surgical retreatment of facial asymmetry with occlusal cant and severe root resorption: a 3-year follow-up. Am J Orthod Dentofacial Orthop. 2017;152:268–280. doi: 10.1016/j.ajodo.2016.06.052. [DOI] [PubMed] [Google Scholar]