Abstract
Depression and posttraumatic stress (DPTS) are common psychiatric comorbidities following burn injury. The purpose of this study was to develop an admission scoring system that assesses the risk of development of depression or posttraumatic symptoms in the burn population. This study is a retrospective review of the prospectively collected Burn Model System National Database. Adult burn survivors enrolled from 2014 to 2018 (n = 486) were included. The primary outcome was the presence of DPTS symptoms at 6, 12, or 24 months postinjury. Logistic regression analysis was used to identify demographic and clinical predictors of DPTS symptoms. A risk scoring system was then created based on assigning point values to relevant predictor factors. The study population had a mean age of 46.5 ± 15.8 years, mean burn size of 18.3 ± 19.7%, and was 68.3% male. Prior to injury, 71.3% of the population was working, 47.9% were married, and 50.8% had completed more than a high school education. An 8-point risk scoring system was developed using the following predictors of DPTS symptom development: gender, psychiatric treatment in the past year, graft size, head/neck graft, etiology of injury, and education level. This study is the first to develop a DPTS symptom risk scoring system for burn injury. This scoring system will aid in identifying burn survivors at high risk of long-term psychiatric symptoms that may be used to improve screening, monitoring, timely diagnosis, and interventions.
Posttraumatic stress (PTS) and depression are prevalent globally, with 5.6% of the population reporting PTS symptoms following a traumatic event and a depression prevalence of 4.4%.1,2 Psychiatric morbidity is common following burn injury with 9% to 45% of survivors reporting PTS symptoms and 34% reporting depression symptoms in the year following injury.3–6 Compared to the general population, burn survivors experience 7-fold higher rates of mental health-related emergency department visits after injury.7 Among traumatic injury populations, nearly 20% reported depression and/or PTS symptoms at 1-year postinjury, indicating that burn survivors experience higher rates of psychiatric morbidity than the overall traumatic injury population.8 The previously described overrepresentation of psychiatric morbidity among burn survivors compared to the general population may be attributed to higher prevalence of premorbid psychiatric issues among burn survivors.3,9 Additional common comorbidities following burn injury including long-term pain, physical impairment, and life-threat perception which have also been shown to be contributors to long-term PTS symptoms and depression.3,6,9–12
Previous studies have highlighted the increased impact of emotional trauma following burn injuries on quality of life, PTS, and depression outcomes compared to the physical injury.13 In the burn population, changes in self-image have a stronger correlation than changes in appearance on development of PTS.14 Similarly, survivor-specific qualities like personality traits and attribution of blame are associated with the development of PTS symptoms and depression following burn injury.15,16 Pain, a common postburn symptom, is another significant predictor of PTS and depression symptom development.5,6 There is no association between age and PTS or depression symptoms in the burn population. Similar to the general population, women are at higher risk of symptom development as compared to men.5,15,17,18 A relationship between burn size and postburn psychological symptoms has limited evidence, signifying the importance of determining other important predictors of psychological sequelae in the burn population.5,15
Psychological symptoms including PTS and depression have an economic and functional cost associated with them. Both depression and PTS introduce an economic burden to the survivor, family, and healthcare system due to changes in employment and treatment costs.19,20 Additionally, psychological symptoms are associated with reduced earnings and lower rates of employment.21,22 Functionally, both PTS and depression are associated with decreased physical functioning and increased fatigue and pain following burn injury.23,24 In the general population, PTS is associated with physical morbidities such as hypertension and cardiovascular disease, among others, as well as decreased health-related quality of life.25 Similarly, depression is associated with increased mortality and decreased quality of life.26,27 The significant contributions of PTS and depression to economic and functional outcomes signify the importance of early detection and timely treatment.
Scoring systems have been created that assess risk of substance misuse, appearance concerns, hospital readmission, and heterotopic ossification following burn injury.28–31 Screening tools and risk scoring systems have been used successfully in burn care to better understand recovery trajectories and risk-stratify potential injury-related complications.28–31 Early intervention reduces rates of PTS and depression as well as symptom recurrence.32–34 Given the prevalence of psychological symptoms in the burn population and associated and negative outcomes, there is a need to develop a standardized mental health risk assessment in this population. The purpose of this study is to develop such a risk scoring system to identify burn survivors at time of hospital admission at risk of developing PTS or depression symptoms. At time of hospital admission, many burn survivors are unable to directly communicate or participate in their care plan. The development of this tool will use demographic and clinical characteristics known at admission to identify a subgroup of the burn population that may benefit from early interventions.
METHODS
Database
This study utilizes data from the Burn Model Systems (BMS) National Database. The BMS Database is a multicenter, longitudinal database created in 1993 as a means of exploring the long-term psychosocial outcomes of burn survivors, and is funded by the National Institute on Disability, Independent Living, and Rehabilitation Research. The BMS National Database is a centralized database that utilizes REDCap electronic data capture tools and is housed at the BMS National Data and Statistical Center at the University of Washington.35 Modifications have been made to inclusion criteria over time. Details regarding inclusion criteria, data collection, and data sites can be found at http://burndata.washington.edu.36 Six burn centers have contributed to the database since its creation.35 Demographic and clinical data are collected at time of discharge from the acute care hospital. For the purposes of this study, outcomes are examined at 6 ± 2, 12 ± 3, and 24 ± 6 months postinjury. Informed consent is obtained from all participants and each site’s Institutional Review Board oversees data collection. According to current BMS database enrollment criteria, participants who were burned between 2014 and 2018, alive at discharge, required autografting surgery for wound closure, consented, and met one of the following criteria were included in the study:
18 to 64 years of age with a burn injury ≥20% total body surface area OR
≥65 years of age with a burn injury ≥10% total body surface area OR
≥18 years of age with a burn injury to their face/neck, hands, or feet OR
≥18 years of age with a high-voltage electrical burn injury.
Prior to 2014, the current instruments used for DPTS were not collected. Our sample was further refined to only include subjects with outcome data on depression and PTSD during the data collection time period.
Demographic and Clinical Variables
Demographic and clinical variables of the study population available at time of admission to the hospital were examined. Demographic data included age, gender, race, ethnicity, marital status, education level, and preinjury employment status. The BMS National Database uses medical record abstraction to collect the variable “Gender” with response options of male and female (although the term “sex” is consistent with established data standards, this manuscript uses the term “gender” to be consistent with the language used in the database).37 Clinical characteristics included burn size, TBSA grafted, history of psychiatric treatment in the past year, head or neck burn, head or neck graft, inhalation injury, etiology of injury, and circumstances of injury. While grafting is not always performed upon admission, TBSA grafted was used as a surrogate for the presence of full or deep-partial thickness injury. The authors determined that a trained burn surgeon would be able to estimate the need for autografting at admission. The outcome is the presence of depression and/or PTS symptoms (referred to as DPTS for the purposes of this manuscript) at 6, 12, or 24 months after injury. Evidence-based cutoff values for the Patient-Reported Outcomes Measurement Information System (PROMIS) depression scale (≥60) and Patient Civilian Checklist (≥50) were used to identify clinically significant depression and PTS symptoms, respectively.38,39 The PROMIS depression scale is one of three PROMIS negative affect item banks using a 7-day time frame and a 5-point Likert rating scale that ranges from 1 (“Never”) to 5 (“Always”).40 The Patient Civilian Checklist is a 17-item self-report measure with responses ranging from 1 (“Not at all”) to 5 (“Extremely”).41 Higher scores on both measures are associated with worse symptoms of depression or posttraumatic stress (DPTS). Both instruments are reliable and valid.40,41
Data Analysis
Descriptive statistics were calculated for demographic and clinical characteristics, using t-tests for quantitative variables and chi-square tests for categorical variables (Table 1). Logistic regression models were used to identify statistically significant demographic and clinical predictors of Depression or PTS symptoms at 6, 12, or 24 months postinjury (Table 2). Multiple imputation was utilized to account for missing data.42 The imputation models included all variables to be considered in the analysis and estimates from 50 datasets were combined using Rubin’s rules.43 The results of those models were checked using standard diagnostics.44 A P value less than .05 was considered statistically significant. Three overall criteria were used to assess the model: discrimination (c-statistic), calibration (calibration plot), and internal validity (bootstrapped 200 samples for each of the 50 imputed datasets for a total of 10,000 bootstrap samples).45–47
Table 1.
Demographic and clinical characteristics of the study population at hospital discharge
| Variable | Total | No DPTS Symptoms Group | DPTS Symptoms Group | P |
|---|---|---|---|---|
| Number of subjects | 388 | 285 | 103 | — |
| Age, mean (SD) | 46.5 (15.8) | 47.4 (16.3) | 44.1 (14.0) | .07 |
| Male, % (n) | 68.3 (265) | 73.0 (208) | 55.3 (57) | <.001 |
| Caucasian, % (n) | 80.0 (300) | 81.0 (221) | 77.5 (79) | .57 |
| Hispanic, % (n) | 17.9 (68) | 17.3 (48) | 19.6 (20) | .60 |
| Burn size, mean TBSA (SD) | 18.3 (19.7) | 16.5 (18.4) | 23.2 (22.4) | <.001 |
| Graft size, mean TBSA (SD) | 12.7 (18.5) | 10.8 (16.6) | 18.2 (22.2) | <.001 |
| Psychiatric treatment in past year, % (n) | 18.0 (66) | 14.6 (39) | 27.3 (27) | .01 |
| Head/neck burn, % (n) | 47.8 (185) | 43.5 (124) | 59.8 (61) | <.001 |
| Head/neck graft, % (n) | 12.9(50) | 8.8 (25) | 24.5 (25) | <.001 |
| Married preinjury, % (n) | 47.9 (151) | 49.6 (111) | 44.0 (40) | .37 |
| Working preinjury, % (n) | 71.3 (258) | 773.0 (195) | 66.3 (63) | .21 |
| Inhalation injury, % (n) | 13.8 (53) | 10.9 (31) | 21.8 (22) | .01 |
| Etiology of injury | .07 | |||
| Fire/flame injury, % (n) | 55.2 (213) | 54.1 (153) | 58.3 (60) | |
| Electrical, % (n) | 6.7 (26) | 5.3 (15) | 10.7 (11) | |
| Other, % (n) | 38.1 (147) | 40.6 (115) | 31.1 (32) | |
| Suspected self-inflicted injury, % (n) | 4.9 (19) | 2.8 (8) | 10.8 (11) | .01 |
| More than high school education, % (n) | 50.8 (157) | 47.5 (105) | 59.1 (52) | .07 |
DPTS, depression and/or posttraumatic stress; PROMIS, Patient-Reported Outcomes Measurement Information System; TBSA, total body surface area.
No DPTS group = did not exhibit evidence of depression and/or posttraumatic stress symptoms at 6, 12, or 24 months after injury.
DPTS group = exhibited evidence of depression (PROMIS depression score >60) and/or posttraumatic stress symptoms (Patient Civilian Checklist score >50) at 6, 12, or 24 months after injury.
Table 2.
Logistic regression examining predictors of development of depression and/or posttraumatic stress symptoms
| Variable | Odds Ratio | P | Confidence Interval | |
|---|---|---|---|---|
| Female | 2.03 | .006 | 1.23 | 3.37 |
| Graft size | 1.02 | .007 | 1.01 | 1.03 |
| Head/neck graft | 2.54 | .007 | 1.29 | 5.00 |
| Psychiatric treatment | 2.19 | .016 | 1.16 | 4.13 |
| Electrical injury | 3.99 | .003 | 1.60 | 9.93 |
| More than high school education | 0.53 | .026 | 0.30 | 0.93 |
Risk Scoring System Development
A point system for determining risk of DPTS symptoms at 6, 12, or 24 months after injury was calculated using the demographic and clinical variables described above. This system was modeled after the Framingham Heart Study methodology.48 This methodology has also been used to develop risk calculators for other burn outcomes.28,49 The risk scoring system was constructed as follows: 1) the model was estimated; 2) risk factors were organized into categories and reference values were chosen; 3) reference risk factor profile is determined based on risk factor organization and reference values; 4) determine the distance from each category to the base; 5) constants are set; 6) determine the number of points associated with each category; 7) determine risks associated with point totals. This results in an admission risk scoring system for development of DPTS symptoms at 6, 12, or 24 months postinjury in the burn population.
RESULTS
Demographic and Clinical Characteristics
A total of 8012 subjects were eligible for the study based on BMS database criteria. Of these, 3684 subjects were excluded based on underage, not alive at discharge, and no consent. An additional 3842 subjects were excluded for not having outcome data within the collection window, leaving a sample of 486 subjects. Final sample included 486 subjects, of which 388 did not have any missing outcome data and the characteristics of this sample are detailed in Table 1. For regression analyses, due to multiple imputation methods, all 486 subjects were included (Figure 1). The population had a mean age of 46.5 ± 15.8 years, mean burn size of 18.3 ± 19.7%, and was 68.3% male. Prior to injury, 71.3% of the population was working, 47.9% were married, and 50.8% had completed more than a high school education. Further details on the demographic and clinical makeup of the population can be found in Table 1. The following variables were missing more than 5% of data: highest level of education completed (24.1%); preinjury marital status (20.2%); psychiatric treatment in the past year (9.7%); preinjury employment status (8.2%).
Figure 1.
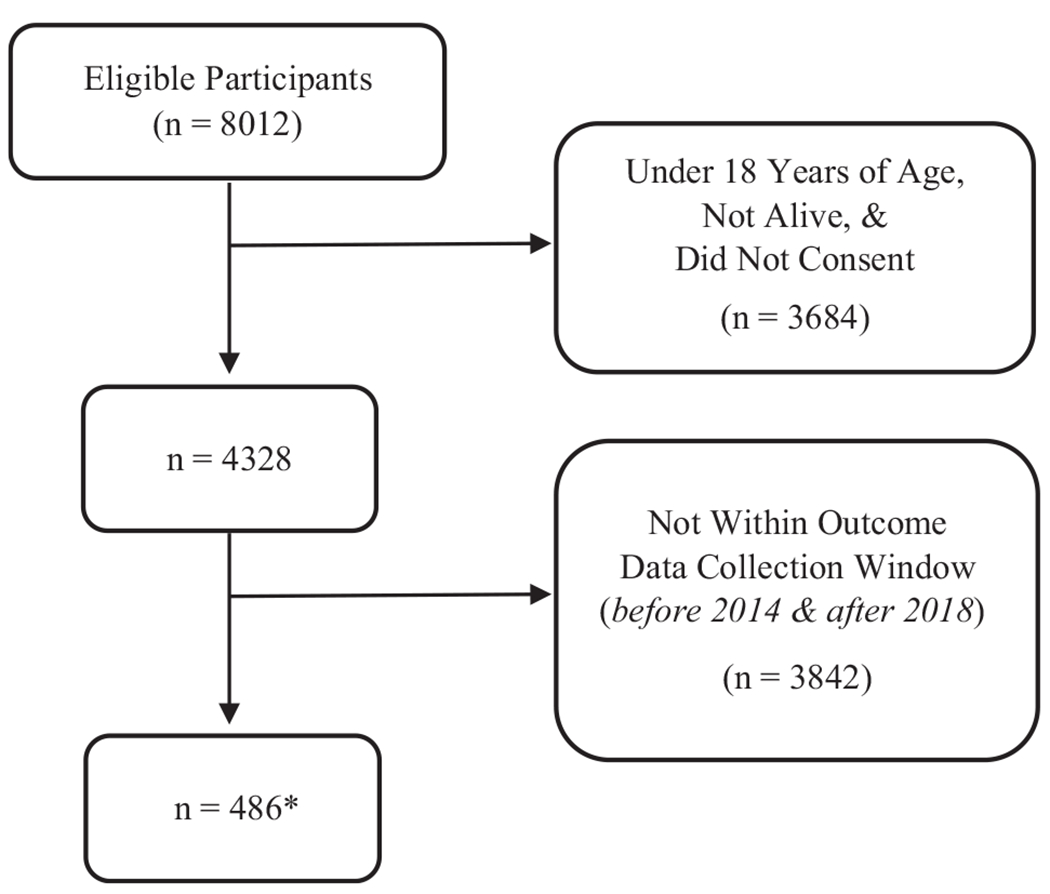
Sample size determination. Flow diagram depicting the selection of study participants. Participants were selected from those eligible for the Burn Model System Longitudinal Database (n = 8012) and further reduced based on the indicated inclusion and exclusion criteria. *Final sample included 486 subjects, of which 388 did not have any missing outcome data and the characteristics of this sample are detailed in Table 1. For regression analyses, due to multiple imputation methods, all 486 subjects were included.
Data Analysis
Regression analyses showed an increased odds of development of DPTS symptoms is significantly associated with female gender, graft size, head/neck graft, psychiatric treatment in the past year, electrical injury, and having less than a high school education. Women were approximately two times as likely as men to develop DPTS symptoms (odd ratio [OR] 2.03; P = .006). For every 1% increase in graft size there is a 2% increase in the odds of developing DPTS symptoms (OR 1.02; P = .007). Graft size was not dichotomized and is the percentage of TBSA that was grafted. Therefore, the OR represents each one percentage point change in graft size. Grafts to the head/neck and psychiatric treatment in the past year were associated with 2.5 and 2.2 times the odds of developing DPTS symptoms, respectively. Regarding etiology of injury, those with an electrical injury exhibited four times the odds of developing DPTS symptoms. Further, those with more than a high school education were 0.53 times the odds of developing DPTS symptoms (Table 2).
Risk Score System Development
Based on the predictors, the DPTS symptom risk scoring system was developed (Table 3). The scoring system includes six variables: gender, psychiatric treatment in the past year, graft size, head/neck graft, etiology of injury, and education level. The model’s c-statistic is 0.73. A box and whiskers plot of the predicted probability of DPTS symptoms for each risk score is shown (Figure 2). The risk scoring system demonstrates graphical evidence of validity in predicting DPTS symptoms at 1 year with higher points associated with higher risk.
Table 3.
Admission scoring system for assessing depression and/or posttraumatic stress symptom risk
| Indicator | Points |
|---|---|
| Gender | |
| Male | 0 |
| Female | 1 |
| Graft size | |
| 0%–30% | 0 |
| 31%–60% | 1 |
| >60% | 2 |
| Head/neck graft | |
| No | 0 |
| Yes | 1 |
| Psychiatric treatment in the past year | |
| No | 0 |
| Yes | 1 |
| Etiology of injury | |
| Fire/flame | 0 |
| Other | 0 |
| Electrical | 2 |
| Education level | |
| Greater than high school | 0 |
| High school or less | 1 |
Points are added to produce a final risk score.
Figure 2.
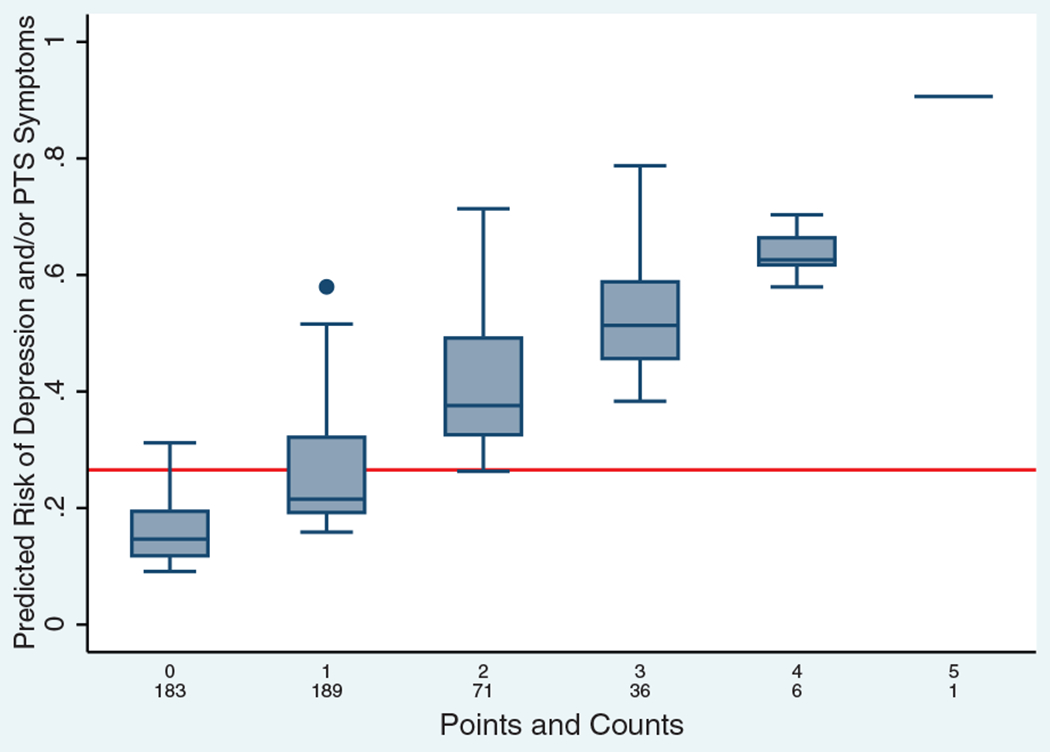
Risk of developing depression and/or posttraumatic stress symptoms by risk score. The x-axis is each possible point sum with the count for each point sum below it. The bar in the middle of each box represents the median predicted risk, and the top and bottom of the box are the 75th and 25th percentiles of the distribution, respectively. The whiskers cover 1.5 times the difference between the 25th and 75th percentiles, and the dots represent values that are outside of this range. The horizontal line indicates the prevalence of depression and/or posttraumatic stress symptoms among the study population (26.6%).
DISCUSSION
This paper is the first to create a burn-specific DPTS symptom risk scoring system at time of hospital presentation. Gender, education level, previous psychiatric treatment, graft size, wound closure requiring skin grafts, and mechanism of burn injury are significant predictors of DPTS symptom development. This scoring system will aid in identifying those at high risk of developing DPTS symptoms following burn injury, which may lead to implementing early interventions, prophylactic treatments, and can guide future studies.
There is a compelling need for a tool that assesses the risk for development of DPTS symptoms following a burn injury given the limits of classic screening instruments in this population. Inpatient risk assessment in those exposed to trauma provides an opportunity to identify those at risk of DPTS symptom development, rather than waiting for symptomology to present following discharge. Screening patients early in hospital admission is feasible.50–53 Screening instruments include the Patient Health Questionnaire 9-item (Ref), Beck Depression Inventory, Hospital Anxiety and Depression Scale, or Symptom Checklist-90 for depression and the Screen for Posttraumatic Stress Symptoms, Self-Rating Scale for Posttraumatic Stress Disorder, Post Traumatic Stress Scale 5-item, or the Patient Civilian Checklist for PTS, among others.54,55 However, because burn survivors are often admitted to the intensive care unit and are chemically sedated, or experience delirium, the use of these patient-administered instruments during much of their hospitalization is not possible. A risk calculator that can be administered with admission characteristics, severity of burn, and collateral information from family and friends is particularly relevant in the burn survivor population.
Early intervention is a key component in treating DPTS symptoms. Many burn survivors experience some form of DPTS following injury, therefore the burn population is especially in need of a tool to more accurately identify and target those with clinically significant symptoms in order to target intervention.56 A systematic review of early intervention following traumatic injury found cognitive-behavioral therapy-based treatment to be the most effective treatment for DPTS symptoms, though any intervention in conjunction with collaborative care had a significant impact on the population.57 A treatment protocol utilizing cognitive-behavioral therapy for DPTS symptoms has shown promise in the burn population.58 Zatzick et al described the feasibility of early mental health interventions in trauma populations, though noted that treatment plans require further delineation.59 Therefore, use of a risk identifying tool will aid clinicians in targeting treatment for burn survivors most in need.5
Risk scoring systems provide an opportunity to identify portions of a population that may require additional screening, treatment, and potential prophylaxis. Scoring systems are often used in critical care and clinical trial settings to assess for risk and severity of disease, respectively.60 Other risk scoring systems developed within the burn population include the Heterotopic Ossification Calculator and the Re-Admission Risk Calculator.28,29 The Heterotopic Ossification Calculator identifies subpopulations of burn survivors at risk of a rare and debilitating complication, providing the opportunity to intervene early. The Re-Admission Calculator can be used to identify those at high risk of readmission to acute care from a rehabilitation setting.13,14 Risk scoring systems have demonstrated clinical efficacy, with the Framingham Heart Study generating a risk assessment for heart disease over a predetermined period and serving as a guiding instrument in clinician treatment guidelines.61,62 The benefits of scoring systems include additional screening, monitoring, and timely diagnosis and intervention for at risk populations.
This risk scoring tool also fits into the goals and guidelines of providing trauma-informed care and could be used in identifying which patients may need additional psychoeducational and psychosocial support.63,64 The core philosophy of trauma-informed care includes an understanding that many people enter the medical setting with a history of past traumas that potentially make them more vulnerable to the stress of medical treatment, and that the medical setting itself can be perceived as threatening. This situation can put patients at risk for the development of new traumatic stress symptoms or trigger preexisting symptoms. The nature of burn care is particularly threatening with ongoing painful procedures, long hospitalizations, and large and rotating medical teams. Within trauma-informed care, there is an acknowledgment that care is patient centered and that each patient is an active participant in their care in order to make the environment less threatening. Goals of care in a trauma-informed approach also include early identification of those most at risk for acute stress and having mental health services available for more intensive intervention.
The National Center for Traumatic Stress has outlined a psychosocial preventative health model (2011 Center for Pediatric Traumatic Stress) that identifies three phases of care and a stepped approach to treatment. The first step acknowledges that the majority of patients may experience some challenges during hospitalization, but they are overall resilient and have good coping strategies, resources, and support coming into the hospital. The intervention goal is to prevent secondary trauma of the healthcare setting by engaging in trauma-informed care practices that include providing universal education about normative responses to trauma as well as comfort and basic assistance to support their individual coping strategies. The second step consists of identifying those patients who have an acute stress reaction or exacerbated distress during medical procedures and established risk factors indicating potential for long-term difficulties. This group will need more immediate and targeted interventions to address emotional distress and promote adaptive coping strategies for the medical environment. Hospital mental health services should be involved at this stage. The third step includes those who have preexisting risk factors, who have an acute stress reaction and are experiencing persistent and/or escalating distress impacting their ability to function. These patients may have other struggles that are impacting natural coping resources, such as depression, grief, anxiety, anger, and substance abuse; they will need more intensive and ongoing care by the hospital mental health providers and continued mental health services once discharged. While trauma-informed care practices should continue for all patients in the outpatient burn clinic setting, the risk stratification score can identify which patients might benefit from early intervention (steps 2 and 3).65 This study has purposefully not identified specific cutoff values for the risk scoring system, as the nature and risk of different interventions should determine the corresponding cut point(s). Further research on interventions is necessary to determine these cut points.
This study has several limitations to consider. The authors combined depression and PTS into one model given the size of the dataset, similarity of treatment approaches, and because risk assessment serves as the first step in identifying populations with a potential need. Some variables, such as amputation, were not included in the analysis due to limitations of the BMS database in terms of how variables were coded and variable inclusion. The authors are unable to perform an external validation given the lack of an additional dataset that is publicly accessible and uses the same outcomes measures in a burn population, therefore internal validation was used for this model. Cutoff values in outcome measures were used in this study to assess clinically significant symptoms, but do not necessarily represent a diagnosis of major depressive disorder or posttraumatic stress disorder. This risk scoring system provides a risk assessment and should be used in conjunction with rigorous clinical assessment to determine appropriate interventions. Lastly, risk factors included in the calculator were limited to demographic and clinical characteristics available in the BMS Database; however, characteristics were chosen based on previous research identifying predictors of DPTS symptoms. When assessing patients clinically, risk factors for DPTS symptoms not found in this dataset, such as family history, prior diagnosed mental disorder, and others, should also be considered.66,67 As integrated healthcare systems, the Burn Model System Centers may have additional resources that are not representative of national burn centers, and therefore the results of the study may underrepresent DPTS symptoms of the national sample. Additionally, due to the database inclusion criteria, the study sample is biased toward a more severely injured population. However, the Burn Model System Database has been shown to be representative of the national burn population.68
This study created an 8-point risk scoring system that stratifies burn patients by risk of DPTS symptom development at time of hospital admission. This risk scoring system may assist in providing burn survivors with early targeted interventions. Additionally, future research may aid in determining clinical cut points for this risk calculator and further validate the tool utilizing postinjury psychiatric diagnostic evaluations.
ACKNOWLEDGEMENTS
This manuscript was accepted as a poster presentation at the 2020 American Burn Association National Meeting.
Funding:
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR): NIDILRR grant number 90DPBU0001. NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, or HHS, and one should not assume endorsement by the Federal Government.
Conflict of interest statement.
K.R. reports grants from NIDILRR. R.Z. receives royalties from 1) Oakstone for an educational CD: Physical Medicine and Rehabilitation a Comprehensive Review; 2) Springer/Demos publishing for serving as coeditor of the text: Brain Injury Medicine. R.Z. serves on the Scientific Advisory Board of Myomo, Oxeia Biopharma, ElMINDA, and Biodirection. C.M.R. reports grants from NIDILRR and Shriners Hospitals for Children. J.C.S. reports grants from NIDILRR and Department of Defense during the conduct of this study. No other authors have any conflicts of interest to disclose.
REFERENCES
- 1.World Health Organization. Depression and other common mental disorders: global health estimates. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO [Google Scholar]
- 2.Koenen KC, Ratanatharathorn A, Ng L et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med 2017;47:2260–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Logsetty S, Shamlou A, Gawaziuk JP et al. Mental health outcomes of burn: a longitudinal population-based study of adults hospitalized for burns. Burns 2016;42:738–44. [DOI] [PubMed] [Google Scholar]
- 4.Davydow DS, Katon WJ, Zatzick DF. Psychiatric morbidity and functional impairments in survivors of burns, traumatic injuries, and ICU stays for other critical illnesses: a review of the literature. Int Rev Psychiatry 2009;21:531–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wiechman SA, Ptacek JT, Patterson DR, Gibran NS, Engrav LE, Heimbach DM. Rates, trends, and severity of depression after burn injuries. J Burn Care Rehabil 2001;22:417–24. [DOI] [PubMed] [Google Scholar]
- 6.Giannoni-Pastor A, Eiroa-Orosa FJ, Fidel Kinori SG, Arguello JM, Casas M. Prevalence and predictors of posttraumatic stress symptomatology among burn survivors: a systematic review and meta-analysis. J Burn Care Res 2016;37:e79–89. [DOI] [PubMed] [Google Scholar]
- 7.Mason SA, Nathens AB, Byrne JP et al. Association between burn injury and mental illness among burn survivors: a population-based, self-matched, longitudinal cohort study. J Am Coll Surg 2017;225:516–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zatzick D, Jurkovich GJ, Rivara FP et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg 2008;248:429–37. [DOI] [PubMed] [Google Scholar]
- 9.Dyster-Aas J, Willebrand M, Wikehult B, Gerdin B, Ekselius L. Major depression and posttraumatic stress disorder symptoms following severe burn injury in relation to lifetime psychiatric morbidity. J Trauma 2008;64:1349–56. [DOI] [PubMed] [Google Scholar]
- 10.Dalal PK, Saha R, Agarwal M. Psychiatric aspects of burn. Indian J Plast Surg 2010;43:S136–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goverman J, Mathews K, Nadler D et al. Satisfaction with life after burn: A Burn Model System National Database Study. Burns 2016;42:1067–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stoddard FJ Jr, Ryan CM, Schneider JC. Physical and psychiatric recovery from burns. Psychiatr Clin North Am 2015;38:105–20. [DOI] [PubMed] [Google Scholar]
- 13.Schneider JC, Trinh NH, Selleck E et al. The long-term impact of physical and emotional trauma: the station nightclub fire. PLoS One 2012;7:e47339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bryant RA. Predictors of post-traumatic stress disorder following burns injury. Burns 1996;22:89–92. [DOI] [PubMed] [Google Scholar]
- 15.Hobbs K Which factors influence the development of post-traumatic stress disorder in patients with burn injuries? A systematic review of the literature. Burns 2015;41:421–30. [DOI] [PubMed] [Google Scholar]
- 16.Giannoni-Pastor A, Gomà-i-Freixanet M, Valero S et al. Personality as a predictor of depression symptoms in burn patients: a follow-up study. Burns 2015;41:25–32. [DOI] [PubMed] [Google Scholar]
- 17.Theman K, Singerman J, Gomez M, Fish JS. Return to work after low voltage electrical injury. J Burn Care Res 2008;29:959–64. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington (DC): American Psychiatric Association; 1994. [Google Scholar]
- 19.Gene-Cos N Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care: National Collaborating Centre for Mental Health. Psychiatr Bull 2006;30:357; available from https://login.treadwell.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=edo&AN=ejs14855385&site=eds-live&scope=site; accessed 19 May, 2019. [Google Scholar]
- 20.Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry 2015;76:155–62. [DOI] [PubMed] [Google Scholar]
- 21.Kessler RC, Heeringa S, Lakoma MD et al. Individual and societal effects of mental disorders on earnings in the United States: results from the national comorbidity survey replication. Am J Psychiatry 2008;165:703–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luciano A, Meara E. Employment status of people with mental illness: national survey data from 2009 and 2010. Psychiatr Serv 2014;65:1201–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edwards RR, Smith MT, Klick B et al. Symptoms of depression and anxiety as unique predictors of pain-related outcomes following burn injury. Ann Behav Med 2007;34:313–22. [DOI] [PubMed] [Google Scholar]
- 24.Ullrich PM, Askay SW, Patterson DR. Pain, depression, and physical functioning following burn injury. Rehabil Psychol 2009;54:211–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McFarlane AC. The long-term costs of traumatic stress: intertwined physical and psychological consequences. World Psychiatry 2010;9:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brenes GA. Anxiety, depression, and quality of life in primary care patients. Prim Care Companion J Clin Psychiatry 2007;9:437–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ganguli M, Dodge HH, Mulsant BH. Rates and predictors of mortality in an aging, rural, community-based cohort: the role of depression. Arch Gen Psychiatry 2002;59:1046–52. [DOI] [PubMed] [Google Scholar]
- 28.Schneider JC, Simko LC, Goldstein R et al. Predicting heterotopic ossification early after burn injuries: a risk scoring system. Ann Surg 2017;266:179–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider JC, Gerrard P, Goldstein R et al. Predictors of transfer from rehabilitation to acute care in burn injuries. J Trauma Acute Care Surg 2012;73:1596–601. [DOI] [PubMed] [Google Scholar]
- 30.Oaie E, Piepenstock E, Williams L. Risk factors for peri-traumatic distress and appearance concerns in burn-injured inpatients identified by a screening tool. Scars Burn Heal 2018;4:2059513118765294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rockne WY, Quinn KC, James G, Cochran A. Identification of substance use disorders in burn patients using simple diagnostic screening tools (AUDIT/DAST-10). Burns 2019;45:1182–8. [DOI] [PubMed] [Google Scholar]
- 32.Reynolds CF III, Cuijpers P, Patel V et al. Early intervention to reduce the global health and economic burden of major depression in older adults. Annu Rev Public Health 2012;33:123–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kearns MC, Ressler KJ, Zatzick D, Rothbaum BO. Early interventions for PTSD: a review. Depress Anxiety 2012;29:833–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu BH, Dimsdale JE. Posttraumatic stress disorder in patients with burn injuries. J Burn Care Rehabil 1999;20:426–33; discussion 422. [DOI] [PubMed] [Google Scholar]
- 35.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goverman J, Mathews K, Holavanahalli RK et al. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: twenty years of contributions to clinical service and research. J Burn Care Res 2017;38:e240–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.U.S. Department of Health and Humans Services. HHS implementation guidance on data collection standards for race, ethnicity, sex, primary language, and disability status. 2011; available from https://aspe.hhs.gov/reports/hhs-implementation-guidance-data-collection-standards-race-ethnicity-sex-primary-language-disability-0; accessed 19 May, 2019.
- 38.Clover K, Lambert SD, Oldmeadow C et al. PROMIS depression measures perform similarly to legacy measures relative to a structured diagnostic interview for depression in cancer patients. Qual Life Res 2018;27:1357–67. [DOI] [PubMed] [Google Scholar]
- 39.Gardner PJ, Knittel-Keren D, Gomez M. The Posttraumatic Stress Disorder Checklist as a screening measure for posttraumatic stress disorder in rehabilitation after burn injuries. Arch Phys Med Rehabil 2012;93:623–8. [DOI] [PubMed] [Google Scholar]
- 40.Schalet BD, Pilkonis PA, Yu L et al. Clinical validity of PROMIS Depression, Anxiety, and Anger across diverse clinical samples. J Clin Epidemiol 2016;73:119–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 1996;34;669–73. doi: 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- 42.Sterne JAC, White IR, Carlin JB et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338:b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Buuren S Flexible imputation of missing data. 2nd ed. Boca Raton (FL): CRC/Chapman & Hall; 2018. [Google Scholar]
- 44.Abayomi K, Gelman A, Levy M. Diagnostics for multivariate imputations. J R Stat Soc Ser C (Appl Stat) 2008;57:273–91. [Google Scholar]
- 45.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med 2015;162:55–63. [DOI] [PubMed] [Google Scholar]
- 46.Moons KG, Altman DG, Reitsma JB et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 2015;162:W1–73. [DOI] [PubMed] [Google Scholar]
- 47.Grunkemeier GL, Wu Y. Bootstrap resampling methods: something for nothing? Ann Thorac Surg 2004;77:1142–4. [DOI] [PubMed] [Google Scholar]
- 48.Fox CS, Sullivan L, D’Agostino RB Sr, Wilson PW; Framingham Heart Study. The significant effect of diabetes duration on coronary heart disease mortality: the Framingham Heart Study. Diabetes Care 2004;27:704–8. [DOI] [PubMed] [Google Scholar]
- 49.Gerrard P, Goldstein R, Divita MA et al. Validity and reliability of the FIM instrument in the inpatient burn rehabilitation population. Arch Phys Med Rehabil 2013;94:1521–6.e4. [DOI] [PubMed] [Google Scholar]
- 50.Jaramillo S, Suffoletto B, Callaway C, Pacella-LaBarbara M. Early screening for posttraumatic stress disorder and depression among injured emergency department patients: a feasibility study. Acad Emerg Med 2019;26:1232–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Karamchandani RR, Vahidy F, Bajgur S et al. Early depression screening is feasible in hospitalized stroke patients. PLoS One 2015;10:e0128246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roaten K, Johnson C, Genzel R, Khan F, North CS. Development and implementation of a universal suicide risk screening program in a safety-net hospital system. Jt Comm J Qual Patient Saf 2018;44:4–11. [DOI] [PubMed] [Google Scholar]
- 53.Imran JB, Richmond RE, Madni TD et al. Determining suicide risk in trauma patients using a universal screening program. J Trauma Acute Care Surg 2018;85:182–6. [DOI] [PubMed] [Google Scholar]
- 54.Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. J Trauma Stress 2005;18:53–62. [DOI] [PubMed] [Google Scholar]
- 55.Aben I, Verhey F, Lousberg R, Lodder J, Honig A. Validity of the Beck Depression Inventory, Hospital Anxiety and Depression Scale, SCL-90, and Hamilton Depression Rating Scale as screening instruments for depression in stroke patients. Psychosomatics 2002;43:386–93. [DOI] [PubMed] [Google Scholar]
- 56.Ehde DM, Patterson DR, Wiechman SA, Wilson LG. Post-traumatic stress symptoms and distress following acute burn injury. Burns 1999;25:587–92. [DOI] [PubMed] [Google Scholar]
- 57.Giummarra MJ, Lennox A, Dali G, Costa B, Gabbe BJ. Early psychological interventions for posttraumatic stress, depression and anxiety after traumatic injury: a systematic review and meta-analysis. Clin Psychol Rev 2018;62:11–36. [DOI] [PubMed] [Google Scholar]
- 58.Cukor J, Wyka K, Leahy N, Yurt R, Difede J. The treatment of posttraumatic stress disorder and related psychosocial consequences of burn injury: a pilot study. J Burn Care Res 2015;36:184–92. [DOI] [PubMed] [Google Scholar]
- 59.Zatzick D, Roy-Byrne P, Russo J et al. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Arch Gen Psychiatry 2004;61:498–506. [DOI] [PubMed] [Google Scholar]
- 60.Brabrand M, Folkestad L, Clausen NG, Knudsen T, Hallas J. Risk scoring systems for adults admitted to the emergency department: a systematic review. Scand J Trauma Resusc Emerg Med 2010;18:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sullivan LM, Massaro JM, D’Agostino RB Sr. Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med 2004;23:1631–60. [DOI] [PubMed] [Google Scholar]
- 62.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421. [PubMed] [Google Scholar]
- 63.Harris M, Fallot RD. Trauma-informed inpatient services. New Dir Ment Health Serv 2001:33–46. doi: 10.1002/yd.23320018905 [DOI] [PubMed] [Google Scholar]
- 64.Reeves E A synthesis of the literature on trauma-informed care. Issues Ment Health Nurs 2015;36:698–709. [DOI] [PubMed] [Google Scholar]
- 65.Trauma Informed Care. The national child traumatic stress network. https://www.nctsn.org/trauma-informed-care; 17 accessed Nov. 2021. [Google Scholar]
- 66.Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. N Engl J Med 2017;376:2459–69. [DOI] [PubMed] [Google Scholar]
- 67.Malhi GS, Mann JJ. Depression. Lancet 2018;392:2299–312. [DOI] [PubMed] [Google Scholar]
- 68.Lezotte DC, Hills RA, Heltshe SL et al. Assets and liabilities of the Burn Model System data model: a comparison with the National Burn Registry. Arch Phys Med Rehabil 2007;88:S7–17. [DOI] [PubMed] [Google Scholar]


