Abstract
Objective:
To examine differences in long-term employment outcomes in the postacute care setting.
Design:
Retrospective review of the prospectively collected Burn Model System National Database.
Setting and Participants:
A total of 695 adult survivors of burn injury enrolled between May 1994 and June 2016 who required postacute care at a Burn Model System center following acute care discharge were included. Participants were divided into 2 groups based on acute care discharge disposition. Those who received postacute care at an inpatient rehabilitation facility (IRF) following acute care were included in the IRF group (N=447), and those who were treated at a skilled nursing facility, long-term care hospital, or other extended-care facility following acute care were included in the Other Rehab group (N=248).
Interventions:
Not applicable.
Main Outcome Measures:
Employment status at 12 months postinjury. Propensity score matching and logistic regression were utilized to determine the effect of postacute care setting on employment status.
Results:
Individuals in the IRF group had larger burns and were more likely to have an inhalation injury and to undergo amputation. At 12 months postinjury, the IRF group had over 9 times increased odds of being employed compared to the Other Rehab group, using propensity score matching (P=.046).
Conclusions:
While admitting patients with more severe injuries, IRFs provided a long-term benefit for survivors of burn injury in terms of regaining employment. Given the current lack of evidence-based guidelines on postacute care decisions, the results of this study shed light on the potential benefits of the intensive services provided at IRFs in this population.
Keywords: Employment, Postacute care, Rehabilitation, Skilled nursing facilities
As medical advances in acute burn care have greatly reduced mortality in the burn population over the past 40 years,1 long-term functionality and quality of life have emerged as important areas of focus for both patients and clinicians. Return to work is an increasingly important goal of burn care and rehabilitation, as employment indicates significant community participation.2 Survivors of burn injury who are working at long-term follow-up report better physical and psychosocial outcomes than those who are not working.2 However, many survivors of burn injury experience significant challenges that delay or prevent full recovery and return to previous lifestyles. Those with particularly complex medical and rehabilitation needs often are unable to return home and resume working following acute care admission. Instead, these individuals transition to postacute care (PAC) settings, which the Medicare Payment Advisory Committee define as facilities that provide rehabilitation (or palliative) services after a stay in an acute care hospital.3
Over the past 10 years, an increasing number of patients are transitioning to PAC settings following acute burn care. During this time, 5906 survivors of burn injury received PAC services in inpatient rehabilitation facilities (IRFs), 4713 in skilled nursing facilities (SNFs), and 1599 in other extended-care facilities, such as long-term care hospitals (LTCHs), according to the American Burn Association’s National Burn Repository, which includes data from 101 United States burn centers.4 These various PAC settings offer services that differ in intensity, duration, and physician supervision. IRFs provide active and ongoing medical management and require patients to participate in a rehabilitation program consisting of at least 3 hours of therapy per day, at least 5 days per week.5 SNFs also provide ongoing medical management and multidisciplinary therapy services, however, these facilities provide less frequent physician and therapy services and do not require patients to participate in an intensive therapy program.6 LTCHs provide hospital-level care for more extended periods of time; patient lengths of stay at LTCHs average 25 days or greater.7 Other PAC settings include hospice facilities and traditional nursing homes.
PAC settings are also becoming a more common discharge disposition following acute care admission among the United States general population. Between 1996 and 2010, the number of patients in the United States discharged to PAC settings increased by nearly 50%, or 1.2 million people.8 PAC spending is the fastest growing area of Medicare costs,9-11 and, according to a recent Institute of Medicine report, spending on PAC services is the largest driver of overall variation in Medicare spending.12
Despite the growing number of patients among the general United States population and among those with a history of burn injury treated in PAC settings, few studies have investigated differences in outcomes by PAC setting. Largely due to insufficient data and lack of common data elements across PAC settings, little is known about the types of patients who would benefit most from each setting.9,13,14 Furthermore, PAC settings often care for distinct patient populations requiring various levels of care. For example, patients with a history of stroke and hip fracture who are discharged to an SNF tend to be older15,16 and are more likely to have experienced a complication in acute care15 and to have comorbidities such as dementia and congestive heart failure, compared to those who were sent to IRFs or home.15 Survivors of burn injury discharged to SNFs also tend to be older.17 Thus, it is difficult to compare the outcomes of patients treated in different PAC settings, as any observed differences in outcomes may be attributed to differences in individual patient characteristics. Research focusing on PAC is also complicated by the fact that nonclinical factors, including insurance coverage, socioeconomic status, provider reimbursement structures, clinician and patient preferences, and geographic availability, may influence PAC disposition decisions.18,19 Propensity scores offer 1 method to overcome these inherent challenges. By identifying and comparing only those patients who are most alike and have the same chance of receiving a particular treatment, propensity scores allow one to mimic random assignment, a task that is difficult in PAC settings. In this way, propensity scores enable one to attribute differences in outcomes to treatment effects.20 The Burn Model System (BMS) National Database, the largest national database in the field of burns that tracks functional and psychosocial recovery,21 offers an opportunity to circumvent historical challenges to research. The BMS National Database collects data from individuals treated at IRFs, SNFs, LTCHs, and several other PAC settings and administers the same set of outcome measurements to all participants. Thus, this database represents a unique tool to evaluate outcomes across various PAC settings. This study aims to use the BMS National Database and propensity score methods to compare long-term employment and quality of life outcomes following burn injury by PAC setting.
Methods
Data source and study population
Data from the prospectively collected BMS National Database between May 1994 and June 2016 were analyzed. Six burn centers in the United States have contributed to this database over the lifespan of the project (1994-present).21 Individuals over 18 years of age who were alive at the time of acute care discharge and received treatment at a PAC setting following acute care were included. For this time period, the BMS National Database included data on survivors who met the following inclusion criteria: (1) deep second- and third-degree burns greater than 10% of the total body surface area (TBSA) in patients over 50 years of age; (2) deep second- and third-degree burns greater than 20% TBSA; (3) deep second- and third-degree burns with serious threat of function or cosmetic threat that involves the face, hands, feet, genitalia, perineum, or major joints; (4) third-degree burns greater than 5% TBSA; (5) deep electrical burns including lightning injury; (6) burn injury with inhalation injury; and (7) circumferential burns of the extremity or chest.
Modifications have been made to the inclusion criteria over time. Details of the BMS National Database inclusion criteria, data collection process, and data collection sites can be found at http://burndata.washington.edu/.
Written consent was obtained from all participants, and the outlined research protocol was approved by the Partners Institutional Review Board.
Participants were divided into 2 groups based on acute care discharge disposition. Those who received PAC services at an IRF following acute care were included in the IRF group, and those who were treated at an SNF, LTCH, or other extended-care facility following acute care were included in the Other Rehab group.
All IRFs included in the BMS National Database are affiliated with BMS centers and thus are linked to specialized burn care. The SNFs, LTCHs, and other extended-care facilities captured by the BMS National Database are not affiliated with BMS centers.
Variables
The following demographic and clinical variables were collected through self-report or medical record abstraction within 30 days of discharge: age, sex, race, ethnicity, burn size, burn etiology, location of burn injury, primary insurance, number of days in the intensive care unit, presence of inhalation injury, amputation, preinjury marital status, preinjury employment status, history of psychological treatment or counseling, preinjury alcohol abuse, and preinjury drug abuse.
Outcomes
Employment status, the primary outcome, was assessed at 12 months postinjury through self-report or medical record abstraction. Participants were considered “employed” if they were working full- or part-time and were paid at least minimum wage.
Health-related quality of life, the secondary outcome, was also assessed at 12 months postinjury through the 12-Item Short Form Health Survey, Physical Component Summary (PCS) and Mental Component Summary (MCS).
Propensity score matching
The propensity score is the chance of receiving a particular treatment “for a patient with given observed prognostic variables.”20(p683) Propensity scores can be used to identify a set of individuals with very similar characteristics, and thus very similar chances of receiving a particular treatment. In propensity score matching, patients with very similar scores but who received different treatments are matched into pairs and then compared. In this study, propensity score matching was used to obtain comparable groups of individuals from the IRF group and the Other Rehab group. The 16 previously outlined demographic and clinical variables, which were readily available in the BMS National Database and have been found in prior research to influence acute care discharge disposition,22 were used to create the propensity scores. A range of caliper widths (0.01, 0.025, 0.05, 0.075, and 0.1), which indicate the difference in propensity scores of matched individuals from each of the 2 groups, were examined. The smallest caliper width, 0.01, was utilized for all analyses, as this caliper was more narrowly defined and included only the most similar matches while maintaining a good c-statistic (c=0.78).
Data analysis
Following a previously described methodology,23 multiple imputation was used to account for variables that were missing with a frequency >10% (race, marital status, location of burn injury, and intensive care unit length of stay). The imputations were checked using the diagnostics suggested by Abayomi et al.24
Descriptive statistics were generated for demographic and medical data. Logistic regression was used to evaluate the effect of PAC setting on employment status at 12 months postinjury. Analyses of secondary outcomes utilized linear regression to evaluate the effect of PAC setting on physical function and mental health at 12 months postinjury. In addition to the propensity scores, BMS site and acute care length of stay were included in these analyses as covariates. Odds ratios were examined for each of the propensity score caliper widths to assess for consistency of findings. C-statistics and calibration curves were examined for each model.
All statistical analyses were performed using STATAa version 15. A P value of ≤.05 was used for statistical significance.
Results
This study included a total of 695 survivors of burn injury. Of these, 447 were included in the IRF group and 248 were included in the Other Rehab group. Those in the IRF group were younger, had larger burns, and were less likely to be single than those in the Other Rehab group (P<.01; table 1). Individuals in the IRF group were also more likely to be Hispanic, be employed at the time of injury, have an inhalation injury, and undergo an amputation compared to those in the Other Rehab group (P<.05; see table 1). Additionally, the IRF group was significantly less likely to be insured by Medicare (P<.001). At 12 months postinjury, 21.4% of the IRF group and 19.4% of the Other Rehab group were working (table 2).
Table 1.
Demographic and clinical characteristics of the study population
| Variable | Other Rehab | IRF | P Value | Missing, n (%) |
|---|---|---|---|---|
| No. of participants | 248 | 447 | ||
| Age (y), mean ± SD* | 51.2±18.5 | 44.8±16.1 | <.01 | 0 (0) |
| Male, n (%)† | 170±68.5 | 312±69.8 | .73 | 0 (0) |
| White, n (%)† | 213±93.8 | 360±93.8 | .97 | 84 (12.1) |
| Hispanic and/or Latina, n (%)† | 10±4.5 | 60±14.3 | <.01 | 52 (7.5) |
| Single, n (%)† | 104±61.2 | 79±45.4 | <.01 | 351 (50.5) |
| Employed at time of injury, n (%)† | 75±32.3 | 264±59.5 | <.01 | 19 (2.7) |
| TBSA burned (%), mean ± SD* | 16.3±14.9 | 34.3±21.2 | <.01 | 11 (1.6) |
| Burn etiology, n (%)† | <.01 | 33 (4.8) | ||
| Fire/flame | 151 (67.4) | 343 (78.3) | ||
| Scald | 33 (14.7) | 26 (5.9) | ||
| Grease | 6 (2.7) | 13 (3) | ||
| Electricity | 3 (1.3) | 28 (6.4) | ||
| Other | 31 (13.8) | 28 (6.4) | ||
| Location of burn injury, n (%)† | ||||
| Head/neck/face | 108 (46.4) | 308 (68.9) | <.01 | 15 (2.2) |
| Trunk | 141 (60.5) | 338 (75.8) | <.01 | 15 (2.2) |
| Perineum | 27 (12.5) | 93 (21.4) | .01 | 44 (6.3) |
| Arm | 144 (62.1) | 368 (82.5) | <.01 | 17 (2.5) |
| Hand | 126 (54.8) | 345 (77.1) | <.01 | 18 (2.6) |
| Leg | 136 (58.9) | 293 (65.5) | <.01 | 17 (2.5) |
| Foot | 69 (30.1) | 156 (35.0) | .01 | 20 (2.9) |
| Inhalation injury, n (%)† | 36 (15.7) | 104 (23.5) | .02 | 23 (3.3) |
| Primary payer, n (%)† | <.01 | 54 (7.8) | ||
| Medicare | 76 (37.6) | 78 (17.8) | ||
| Medicaid | 33 (16.3) | 81 (18.5) | ||
| Private/HMO/PPO | 22 (10.9) | 118 (26.9) | ||
| Worker’s comp | 23 (11.4) | 67 (15.3) | ||
| Other | 48 (23.8) | 95 (21.6) | ||
| ICU length of stay (d), mean ± SD* | 12.6±1.51 | 34.9±2.13 | <.001 | 355 (51.1) |
| Psychological therapy or counseling preinjury, n (%)† | 55 (24.8) | 72 (16.6) | .01 | 39 (5.6) |
| Amputation, n (%)† | 18 (9.4) | 83 (19.0) | <.01 | 67 (9.6) |
| Alcohol abuse in last 12 mo, n (%)† | 48 (22.0) | 91 (21.1) | .79 | 46 (6.6) |
| Drug abuse in last 12 mo, n (%)† | 39 (18.4) | 66 (15.3) | .31 | 51 (7.3) |
Abbreviations: HMO, health maintenance organization; ICU, intensive care unit;PPO, preferred provider organization.
Two-sample t tests used to identify any differences in demographic and clinical variables between groups.
Chi-square tests used to identify any differences in demographic and clinical variables between groups.
Table 2.
Employment status at 12 months postinjury
| Employed | Other Rehab | IRF | P Value |
|---|---|---|---|
| All participants, n (%) | 24 (19.4) | 65 (21.4) | .639 |
| 0.01 Caliper participants, n (%) | 3 (7.7) | 18 (14.0) | .300 |
Fifty data sets were imputed. Using the 0.01 caliper, 294 individuals matched (204 from the IRF group and 90 from the Other Rehab group), with some participants in each group matching more than once (fig 1). Of the individuals who matched using the 0.01 caliper, 14% of the IRF group and 7.7% of the Other Rehab group were working at 12 months postinjury (see table 2).
Fig 1.
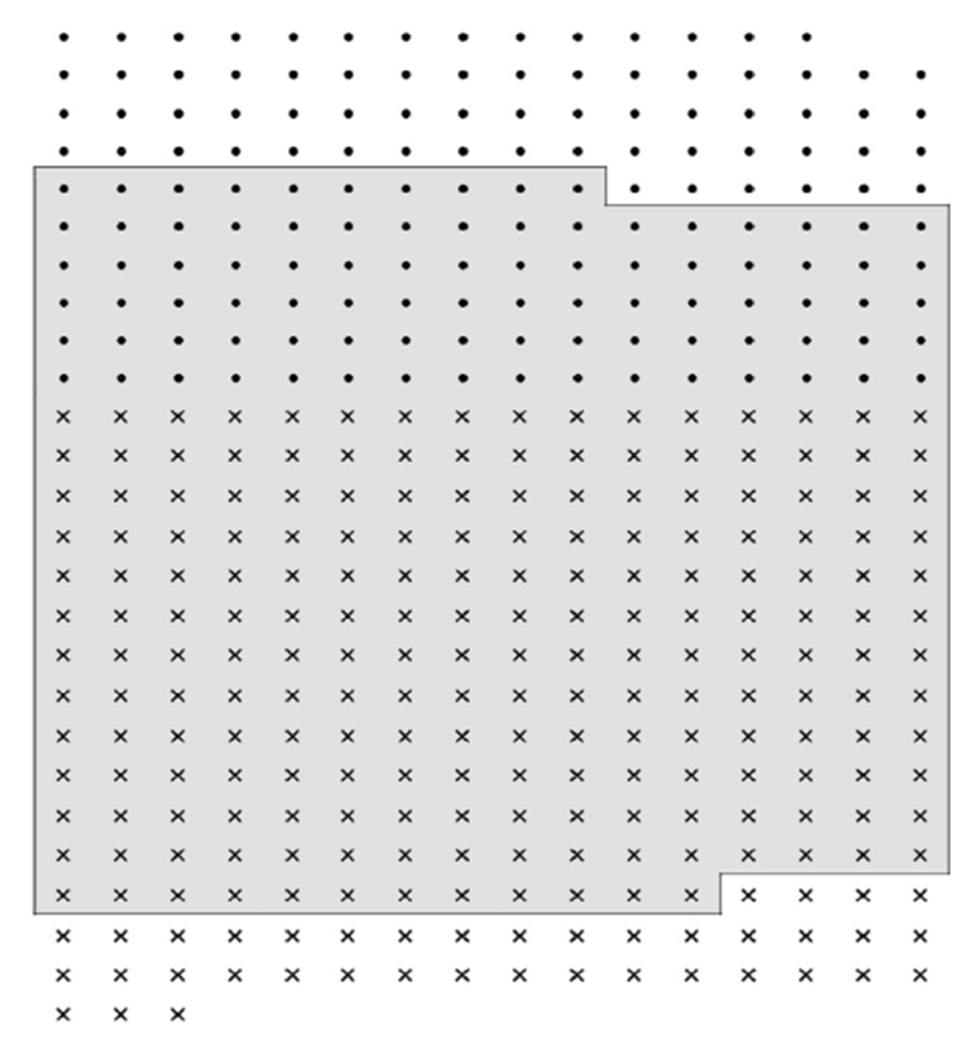
The 0.01 caliper propensity score matched group. Each dot represents an individual included in the Other Rehab group, and each ˟ indicates an individual included in the IRF group. The outlined and shaded box represents the 0.01 propensity score matched group, which includes 204 individuals from the IRF group and 90 individuals from the Other Rehab group.
In the logistic regression analysis, the IRF group had over 9 times increased odds of being employed at 12 months postinjury compared to the Other Rehab group (OR=9.707, P=.046; table 3). Qualitatively similar, statistically significant results were achieved across multiple caliper widths (OR=17.17, P=.026 for 0.025 caliper; OR=12.14, P=.042 for 0.05 caliper;OR=12.43, P=.038 for 0.075 caliper; OR=13.66, P=.033 for 0.1 caliper). The c-statistic of both the 0.01 and 0.1 caliper logistic regression models was 0.78, thus indicating a good fit. The calibration curves demonstrated good calibration up to a predicted probability of employment of 40%.
Table 3.
Long-term employment outcomes for survivors of burn injury: comparing patients at IRFs vs Other Rehab settings using the propensity score matched group
| Propensity Score Caliper* | No. | Odds Ratio† | 95%Confidence Interval | P Value | C-Statistic | 95%Confidence Interval |
|---|---|---|---|---|---|---|
| 0.01 | 266 | 9.707 | 1.04-90.40 | .046 | 0.78 | 0.64-0.91 |
| 0.1 | 382 | 13.66 | 1.5-149.83 | .033 | 0.78 | 0.70-0.86 |
Calipers indicate the difference in propensity scores of matched individuals from each of the 2 groups (IRF and Other Rehab). The smallest caliper,0.01, is the most narrowly defined and included only the most similar matches. The largest caliper, 0.1, is the least narrowly defined and included the least similar matches.
Adjusted for the propensity scores, BMS site, and acute care length of stay. The following variables were used to create propensity scores: age, sex, race, ethnicity, burn size, burn etiology, location of burn injury, primary insurance, number of days in the intensive care unit, presence of inhalation injury, amputation, preinjury marital status, preinjury employment status, history of psychological treatment or counseling, preinjury alcohol abuse, and preinjury drug abuse.
In analyses of secondary outcomes, the IRF group was found to have significantly higher PCS scores than the Other Rehab group. MCS scores did not differ between groups. However, these models demonstrated poor discrimination and calibration and were thus excluded from final analyses (c-statistics ranging from 0.57 to 0.60 and from 0.54 to 0.57 for PCS and MCS, respectively).
Discussion
Decisions about PAC can have a profound effect on a patient’s recovery, however, little is known about which patients benefit most from the various PAC settings. Previous efforts to compare outcomes across PAC settings have been hindered by the lack of common data elements across settings,25 as well as by fundamental differences in patient populations. By utilizing the BMS National Database and propensity score matching, the present study attempted to address these 2 historical challenges. As mentioned previously, the BMS National Database offers a unique opportunity to evaluate employment and other outcomes across various PAC settings, as it includes data from individuals treated at a variety of PAC settings and administers the same set of outcome measurements to all participants. Furthermore, while the IRF and Other Rehab groups differed significantly in terms of several demographic and clinical variables and thus may represent fundamentally different patient populations, the use of propensity scores allowed for the identification of only the most similar study participants. Propensity score matching enabled the comparison of individuals across groups who had a similar chance of receiving treatment at either an IRF or Other Rehab facility. To the best of our knowledge, this is the first study to evaluate differences in employment outcomes for survivors of burn injury by PAC setting.
In the present study, survivors of burn injury in the IRF group had larger burns and were significantly more likely to have an inhalation injury and to undergo an amputation compared to the Other Rehab group. In propensity score–matched regression analyses, the IRF group had almost 10 times increased odds of being employed at 12 months postinjury compared to those in the Other Rehab group. Thus, while IRFs admitted survivors of burn injury with more severe injuries, treatment at an IRF was associated with long-term employment.
Employment is a particularly important outcome after an injury and after PAC. For many within and beyond the burn community, return to work represents significant community participation and constitutes a major milestone in recovery.26 A number of meta-analyses, literature reviews, and studies of the general population have established that employed individuals are healthier than those who are unemployed.27-29 Among individuals with disabilities, those who are employed report significantly lower rates of smoking and better quality of life,30 have lower Medicare and Medicaid costs,30 and experience mental distress less frequently than those who are not employed.31 Within the burn population, employment status has been shown to be a valid indicator of postinjury physical and psychosocial health.2 Survivors of burn injury working at long-term follow-up report better psychosocial health and less pain compared to those not working.2 However, burn injuries can have a tremendous effect on return to work. One 2-center study found that 66% and 90% of survivors of burn injury had returned to work at 6 and 24 months postinjury, respectively.32 However, 1 center found that only 37% of survivors returned to the same job, with the same employer, and without accommodations. Patients with burn injuries face a number of barriers that may delay or prevent return to work, including pain, scarring, contractures, amputations, weakness, neurologic problems, impaired mobility, issues with appearance, and workplace conditions.33-35 Several variables included in the propensity score calculations, such as burn size, burn location (hand burn), and psychiatric history have been previously associated with time to return to work.35 Survivors of burn injury who were injured at work face additional difficulties upon work reintegration.36 Given the prevalence of these barriers, as well as the demonstrated importance of postinjury employment, the results of this study may be particularly important for the PAC patient population and their clinicians. PAC services offered at IRFs may maximize not only employment but also long-term well-being.
Most of what is known about postacute burn care comes from research conducted in the IRF setting. Many survivors of burn injury admitted to IRFs present with cognitive-communication impairments,37 and, at the time of discharge from acute care, are likely to have significant range of motion deficits.22 Nevertheless, survivors of burn injury treated at IRFs make significant functional improvements from admission to discharge,38 and treatment at a specialized burn unit within an IRF has been shown to decrease burn center length of stay and allow for a more rapid restoration of physical and psychological function, compared to treatment at nonspecialized rehabilitation facilities.39 Fewer studies have examined outcomes for survivors of burn injury who transition to SNFs. As in the present study, survivors of burn injury who are SNF-bound tend to be older.17,40 Researchers have found that older survivors of burn injury discharged to SNFs demonstrate increased mortality compared to those discharged home after accounting for age, burn size, and presence of inhalation injury.41 These previous studies were limited by single center data, small sample sizes, and lack of random assortment or propensity score matching.
Researchers in other fields have begun to use propensity score and other methods to investigate outcomes associated with IRF and SNF-level care. Among trauma patients, those treated at IRFs have significantly increased functional independence and likelihood of discharge to home compared to propensity score— matched controls.42 IRF care is also associated with decreased 1-year mortality for patients of trauma injury,42 while SNF care following a trauma admission is associated with a higher risk of subsequent mortality.43 Similarly, in multivariate and propensity score analyses, patients with a history of stroke who are discharged to IRFs were found to be more likely to recover activities of daily living and to return to their communities than those discharged to SNFs.44 After controlling for clinically significant variables such as age, functional status at discharge from acute care, and total hours of rehabilitation, patients with a history of stroke who were discharged to IRFs also had improved physical and cognitive function compared to those discharged to SNFs.16,44 Furthermore, a Canadian study using multiple logistic regressions and propensity score matching found that patients with traumatic spinal cord injuries who receive IRF care are more likely to return home than those who do not receive IRF care.45
Much of the existing literature on PAC in the general United States population focuses on Medicare enrollees and, within this population, on common conditions such as stroke, hip fracture, and lower-extremity joint replacement.13,14 This focus is likely the result of the relative availability of data on the Medicare patient population. Among Medicare beneficiaries enrolled in fee-for-service in 2013, over 40% were discharged from an acute care hospital to a PAC setting.46 Of these, 20% were discharged to an SNF, 17% to a home health agency, 4% to an IRF, and 1% to an LTCH.46 Furthermore, about 85% of hip fracture and lower-extremity joint replacement and 70% of patients with history of stroke go on to a PAC setting after discharge from acute care.47 Other studies of the Medicare population have shown that, as in the present study, those treated at SNFs tend to be older than individuals treated at IRFs.14 However, there is a paucity of research examining differences in outcomes by PAC setting, and the literature is occasionally conflicting.13,15,44,48,49 The only study to compare outcomes across the various PAC settings for patients with a wide range of diagnoses failed to find consistent differences in hospital readmission rates and in changes in mobility or self-care.50 Furthermore, researchers have noted significant variation in the availability and use of PAC, often by geographic region.13,51,52 This variation further highlights the need for evidence-based criteria to guide decisions about discharge to PAC settings.
Study limitations
Several limitations to this study must be noted. This study evaluated employment status, but other important outcomes, such as physical functioning, mental health, and community integration, may also be affected by PAC setting. Additionally, this study was not able to investigate employment outcomes beyond 12 months postinjury, and it did not evaluate changes in employment status over time. This study was also unable to evaluate specific details of employment, such as primary occupation and number of hours worked; these factors may be important in determining the value of treatment at an IRF after burn injury. The BMS National Database does not collect information regarding specific treatments and rehabilitation protocols, which may affect long-term employment and other outcomes. Two variables, marital status and intensive care unit length of stay, were not collected for the entire duration of the data collection period and thus contributed more missing data than others. Several other variables known to influence return to work after burn injury were not collected for the duration of the BMS National Database years examined and contributed too much missing data to be included in this study. In the BMS National Database, burn size is calculated by including full- and partial-thickness burns, however, the extent of full and partial thickness is not recorded. Thus, it was not possible in this study to distinguish these details of burn severity between the IRF and Other Rehab groups. In addition, propensity scores remove overt biases but cannot account for hidden biases, or biases resulting from unknown or unmeasured differences between study participants before treatment.53 Variables that were unobservable or not collected in the BMS National Database could not be included in the matching procedure, and thus it is possible that bias remains even after propensity score matching. For example, while the FIM instrument and comorbidities may affect acute care discharge disposition, these variables are not readily available in the BMS National Database and thus could not be included in the propensity score. A myriad of other factors, such as socioeconomic status, insurance payment structures, individual preferences and attitudes, and geographic availability, may also affect discharge to PAC but are not available in the BMS National Database and thus were beyond the scope of this study. Future studies would benefit from the inclusion of such variables. Furthermore, all IRFs included in this study are affiliated with BMS centers, and thus the observed benefits associated with IRFs may be partially due to receiving burn-specific PAC at a BMS-affiliated center. The confidence intervals accompanying the odds ratios are very wide; thus, the estimate of the effect of PAC setting on employment status at 12 months postinjury is measured somewhat imprecisely. This is likely due to the relatively small sample size used for analyses. Finally, the BMS National Database only includes information from 6 burn centers, and thus the results of this study may not reflect the outcomes of all United States survivors of burn injury and PAC settings. However, the BMS National Database has been shown to be representative of the United States burn population.54
Conclusions
Survivors of burn injury discharged to IRFs have significantly increased odds of being employed at 12 months postinjury compared to a propensity score–matched population discharged to other rehabilitation settings. With its use of the BMS National Database, this study is unique in its ability to compare outcomes across various PAC settings. Similar data sets do not exist in other PAC populations and have thus resulted in the current lack of evidence-based guidelines on PAC decisions. Future research focused on identifying predictors of the various PAC settings may provide additional insight into long-term employment outcomes. Nevertheless, the results of this study shed light on the potential benefits of receiving intensive PAC services at IRFs and may help inform future guidelines regarding discharge to PAC settings.
Acknowledgments
Supported by the National Institute on Disability, Independent Living, and Rehabilitation Research (grant no. 90DP0035 and 90DPBU0001).
List of abbreviations:
- BMS
Burn Model System
- IRF
inpatient rehabilitation facility
- LTCH
long-term care hospital
- MCS
Mental Component Summary
- PAC
postacute care
- PCS
Physical Component Summary
- SNF
skilled nursing facility
- TBSA
total body surface area
Footnotes
The contents of this manuscript do not necessarily represent the policy of the National Institute on Disability, Independent Living, and Rehabilitation; the Administration for Community Living; or the Department of Health and Human Services.
Disclosures: none.
Suppliers
a. STATA, version 15; StataCorp.
References
- 1.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med 1998;338:362–6. [DOI] [PubMed] [Google Scholar]
- 2.Dyster-Aas J, Kildal M, Willebrand M, Gerdin B, Ekselius L. Work status and burn specific health after work-related burn injury. Burns 2004;30:839–42. [DOI] [PubMed] [Google Scholar]
- 3.MedPac. Post-acute care. Available at: http://www.medpac.gov/-research-areas-/post-acute-care. Accessed September 20, 2017.
- 4.American Burn Association. 2016 national burn repository. Chicago: American Burn Association; 2016. [Google Scholar]
- 5.Medicare Learning Network. Inpatient rehabilitation therapy services: complying with documentation requirements. Available at: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/Inpatient_Rehab_Fact_Sheet_ICN905643.pdf. Accessed September 5, 2017.
- 6.Centers for Medicare and Medicaid Services. Medicare coverage of skilled nursing facility care. Available at: https://www.medicare.gov/Pubs/pdf/10153.pdf. Accessed September 5, 2017.
- 7.Centers for Medicare and Medicaid Services. Long-term care hospital services. Available at: https://www.medicare.gov/coverage/long-term-care-hospitals.html#1351. Accessed September 20, 2017.
- 8.Burke R, Juarez-Colunga E, Levy C, Prochazka A, Coleman E, Ginde A. Rise of post – acute care facilities as a discharge destination of US hospitalizations. JAMA Intern Med 2015;175:295–7. [DOI] [PubMed] [Google Scholar]
- 9.Ackerly DC, Grabowski DC. Post-acute care reform — beyond the ACA. N Engl J Med 2014;370:689–91. [DOI] [PubMed] [Google Scholar]
- 10.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in medicare point to the potential for cost savings in these settings. Health Aff 2013;32:864–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mechanic R Post-acute care — the next frontier for controlling medicare spending. N Engl J Med 2014;370:692–4. [DOI] [PubMed] [Google Scholar]
- 12.Newhouse J, Garber A, Graham R, McCoy M, Mancher M, Kibria A. Variation in health care spending: target decision making, not geography. Washington (DC): National Academies Press; 2013. [PubMed] [Google Scholar]
- 13.Buntin MB. Access to postacute rehabilitation. Arch Phys Med Rehabil 2007;88:1488–93. [DOI] [PubMed] [Google Scholar]
- 14.Buntin MB, Garten AD, Paddock S, Saliba D, Totten M, Escarce JJ. How much is postacute care use affected by its availability? Health Serv Res 2005;40:413–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beeuwkes Buntin M, Hoverman Colla C, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after post-acute care for stroke and hip fracture. Med Care 2010;48:776–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan L, Sandel ME, Jette AM, et al. Does postacute care site matter? A longitudinal study assessing functional recovery after a stroke. Arch Phys Med Rehabil 2013;94:622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pham TN, Kramer CB, Wang J, et al. Epidemiology and outcomes of older adults with burn injury: an analysis of the national burn repository. J Burn Care Res 2009;30:30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ottenbacher KJ, Graham JE. The state-of-the-science: access to postacute care rehabilitation services. A review. Arch Phys Med Rehabil 2007;88:1513–21. [DOI] [PubMed] [Google Scholar]
- 19.Foster M, Tilse C. Referral to rehabilitation following traumatic brain injury: a model for understanding inequities in access. Soc Sci Med 2003;56:2201–10. [DOI] [PubMed] [Google Scholar]
- 20.Braitman LE, Rosenbaum PR. Rare outcomes, common treatments: analytic strategies using propenisty scores. Ann Intern Med 2014;137:693–6. [DOI] [PubMed] [Google Scholar]
- 21.Goverman J, Mathews K, Holavanahalli RK, et al. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: twenty years of contributions to clinical service and research. J Burn Care Res 2017;38:e240–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pham TN, Carrougher GJ, Martinez E, et al. Predictors of discharge disposition in older adults with burns: a study of the burn model systems. J Burn Care Res 2015;36:607–12. [DOI] [PubMed] [Google Scholar]
- 23.Leyrat C, Seaman SR, White IR, et al. Propensity score analysis with partially observed covariates: How should multiple imputation be used? Stat Methods Med Res 2019;28:3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abayomi K, Gelman A, Levi M. Diagnostics for multivariate imputations. J R Stat Soc 2008:273–91. Series C57. [Google Scholar]
- 25.Heinemann AW. State of the science on postacute rehabilitation: setting a research agenda and developing an evidence base for practice and public policy. An introduction. Assist Technol 2008;20:55–60. [DOI] [PubMed] [Google Scholar]
- 26.Esselman PC. Community integration outcome after burn injury. Phys Med Rehabil Clin N Am 2011;22:351–6. [DOI] [PubMed] [Google Scholar]
- 27.Ross CE, Mirowsky J. Does employment affect health? J Health Soc Behav 1995;36:230. [PubMed] [Google Scholar]
- 28.McKee-Ryan FM, Song Z, Wanberg CR, Kinicki AJ. Psychological and physical well-being during unemployment: a meta-analytic study. J Appl Psychol 2005;90:53–76. [DOI] [PubMed] [Google Scholar]
- 29.Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav 2009;74:264–82. [Google Scholar]
- 30.Hall JP, Kurth NK, Hunt SL. Employment as a health determinant for working-age, dually-eligible people with disabilities. Disabil Health J 2013;6:100–6. [DOI] [PubMed] [Google Scholar]
- 31.Okoro C, Strine T, McGuire L, Balluz L, Mokdad A. Employment status and frequent mental distress among adults with disabilities. Occup Med (Chic Ill) 2007;57:217–20. [DOI] [PubMed] [Google Scholar]
- 32.Brych SB, Engrav LH, Rivara FP, et al. Time off work and return to work rates after burns: systematic review of the literature and a large two-center series. J Burn Care Rehabil 2001;22:401–5. [DOI] [PubMed] [Google Scholar]
- 33.Schneider JC, Bassi S, Ryan CM. Barriers impacting employment after burn injury. J Burn Care Res 2007;30:294–300. [DOI] [PubMed] [Google Scholar]
- 34.Esselman PC, Askay SW, Carrougher GJ, et al. Barriers to return to work after burn injuries. Arch Phys Med Rehabil 2007;88:S50–6. [DOI] [PubMed] [Google Scholar]
- 35.Mason ST, Esselman P, Fraser R, Schomer K, Truitt A, Johnson K. Return to work after burn injury: a systematic review. J Burn Care Res 2012;33:101–9. [DOI] [PubMed] [Google Scholar]
- 36.Schneider JC, Shie VL, Espinoza LF, et al. Impact of work-related burn injury on social reintegration outcomes: a life impact burn recovery evaluation (LIBRE) study. Arch Phys Med Rehabil 2017. Nov 26 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hendricks CT, Camara K, Violick Boole K, et al. Burn injuries and their impact on cognitive-communication skills in the inpatient rehabilitation setting. J Burn Care Res 2017;38:e359–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sliwa JA, Heinemann A, Semik P. Inpatient rehabilitation following burn injury: patient demographics and functional outcomes. Arch Phys Med Rehabil 2005;86:1920–3. [DOI] [PubMed] [Google Scholar]
- 39.DeSanti L, Lincoln L, Egan F, Demling R. Development of a burn rehabilitation unit: impact on burn center length of stay and functional outcome. J Burn Care Rehabil 1998;19:414–9. [DOI] [PubMed] [Google Scholar]
- 40.Douglas SL, Daly BJ, O’Toole EE, Kelley CG, Montenegro H. Age differences in survival outcomes and resource use for chronically critically ill patients. J Crit Care 2009;24:302–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Palmieri TL, Molitor F, Chan G, et al. Long-term functional outcomes in the elderly after burn injury. J Burn Care Res 2012;33:497–503. [DOI] [PubMed] [Google Scholar]
- 42.Nehra D, Nixon ZA, Lengenfelder C, et al. Acute rehabilitation after trauma: does it really matter? J Am Coll Surg 2016;223:755–63. [DOI] [PubMed] [Google Scholar]
- 43.Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA 2011;305:1001–7. [DOI] [PubMed] [Google Scholar]
- 44.Kramer AM, Steiner JF, Schlenker RE, et al. Outcomes and costs after hip fracture and stroke: a comparison of rehabilitation settings. J Am Med Assoc 1997;277:396–404. [PubMed] [Google Scholar]
- 45.Cheng CL, Plashkes T, Shen T, et al. Does specialized inpatient rehabilitation affect whether or not people with traumatic spinal cord injury return home? J Neurotrauma 2017;34:2867–76. [DOI] [PubMed] [Google Scholar]
- 46.Medicare Payment Advisory Commission. Report to the congress: Medicare payment policy. Washington (DC): Medpac; 2015. [Google Scholar]
- 47.Buntin MB, Colla CH, Escarce JJ. Effects of payment changes on trends in post-acute care. Health Serv Res 2009;44:1188–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kane RL. Assessing the effectiveness of postacute care rehabilitation. Arch Phys Med Rehabil 2007;88:1500–4. [DOI] [PubMed] [Google Scholar]
- 49.Prvu Bettger JA, Stineman MG. Effectiveness of multidisciplinary rehabilitation services in postacute care: state-of-the-science. a review. Arch Phys Med Rehabil 2007;88:1526–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gage B, Morley M, Smith L, et al. Post-acute care payment reform demonstration: final report. Baltimore: Centers for Medicare & Medicaid Services; 2012. [Google Scholar]
- 51.Medicare Payment Advisory Comission. Report to the congress: Medicare and the health care delivery system. Washington (DC): Medpac; 2018. [Google Scholar]
- 52.Kane RL, Lin W-C, Blewett LA. Geographic variation in the use of post-acute care. Health Serv Res 2002;37:667–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Okoli GN, Sanders RD, Myles P. Demystifying propensity scores. Br J Anaesth 2014;112:13–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lezotte DC, Hills RA, Heltshe SL, et al. Assets and liabilities of the Burn Model System data model: a comparison with the National Burn Registry. Arch Phys Med Rehabil 2007;88(12 Suppl 2):S7–17. [DOI] [PubMed] [Google Scholar]


