Abstract
Objectives:
To use latent growth curve and longitudinal structural equation modeling to examine the 2-year trajectory of satisfaction with appearance in adults with burn injury, and that trajectory’s effect on depression 5 years after burn injury.
Design:
Data were collected at discharge after burn injury hospitalization and at 6 months, 1 year, 2 years, and 5 years postdischarge.
Setting:
The Burn Model Systems (BMS) program consisted of a data center and 5 participating burn centers.
Participants:
The sample consisted of adults (N = 720) who were hospitalized for a burn injury, enrolled in the BMS database, and completed measures at least once throughout the 5-year study duration.
Interventions:
Not applicable.
Main Outcome Measures:
Satisfaction With Appearance Scale and Patient Health Questionnaire-9 (depression).
Results:
Women with burn injury reported higher levels of dissatisfaction with their appearance in comparison to their male counterparts over the 2 years after discharge. Individuals with a larger total body surface area (TBSA) affected by a burn also reported greater body dissatisfaction across the postdischarge 2-year period. Results did not support significant gender or TBSA differences in the rate of change of body dissatisfaction trajectories across these 2 years. Individuals with greater body dissatisfaction at 6 months postdischarge tended to have higher depressive symptoms at 5 years. Six month postdischarge, body dissatisfaction scores also mediated the effects of gender and TBSA on depressive symptoms 5 years later.
Conclusions:
It is recommended that individuals with heightened body image dissatisfaction after a burn, particularly women and those with larger TBSA, participate in evidence-based psychosocial interventions to improve long-term adjustment.
Keywords: Body image, Burns, Depression, Rehabilitation
Nonfatal burn injury is one of the primary causes of disability in the United States, affecting more than 480,000 individuals in 2015.1 Significant scarring, damage to the skin’s appearance, and impairment to a person’s physical functioning often accompany severe burn injury.2 In addition to these physical correlates, individuals with a burn injury often experience psychological distress associated with their body image and social interactions.3
Dissatisfaction with body image is a common issue that arises after burn injury and is often associated with the development of later depressive symptoms.4 The distress resulting from scarring and subsequent challenges in social interactions has predicted worsening psychosocial functioning 1 year after hospital release of burn patients.5 Psychosocial adjustment to burn injury is affected by demographic and burn injury characteristics. Women have been shown to be at a higher risk of body image dissatisfaction 6 and 12 months postdischarge and reduced psychosocial adjustment 1 year postdischarge.5
Although the course of satisfaction with appearance after burn injury has been briefly documented, this body of research has been characterized by small sample sizes and patients with minor burn injuries, and restricted to only 1 year after injury.5 It remains unclear whether trajectories of distress with one’s appearance continue to rise after a year or return to preburn levels after individuals with a burn injury learn to accept and manage social interactions.6
The current study aimed to build on past studies by using latent growth curve and longitudinal structural equation modeling to examine the 2-year trajectory of satisfaction with appearance and that trajectory’s effect on depression 5 years after burn injury. A national sample of adults with burn injury from the Burn Model Systems (BMS) database was used.7 We hypothesized that women and individuals with more severe burns, as characterized by a larger total body surface area (TBSA) that is affected by the burn percentage, would have lower satisfaction with their appearance over 2 years and that this dissatisfaction would worsen in those 2 groups over time as compared to men and those with less severe burns.5 This study further examined the effect of the 2-year trajectory of satisfaction with appearance on depressive symptoms 5 years postdischarge. We hypothesized that women and individuals with greater burn severity would have more depressive symptoms 5 years postdischarge and that this association would be mediated by the linear trajectories of satisfaction with appearance.
Methods
Setting
The study used de-identified secondary data from the National Institute on Disability, Independent Living, and Rehabilitation Research BMS.7 The BMS program consisted of a data center and 5 participating burn centers located in Boston, MA; Dallas, TX; Galveston, TX; Baltimore, MD; and Seattle, WA. Each burn center identified participants based on the patient’s burn characteristics as well as where treatment and rehabilitation occurred.
Participants were eligible to participate in the BMS data enrollment if they met 1 of the following subcriteria: (1) ≥10% TBSA if aged ≥65 years and with burn surgery for wound closure; or (2) ≥20% TBSA if aged <65 years and with burn surgery for wound closure. Eligibility criteria also included receiving burn surgery for electrical high-voltage/lightning burns, hand burns, face burns, and/or feet burns. Finally, patients were eligible to participate if they received primary treatment from a BMS center for burn wound closure, had surgery for wound closure within 30 days of the burn injury, and were provided comprehensive rehabilitation services at the respective BMS center.
Participants
To be included in the current analyses, participants had to have data present for at least 1 time point at either discharge, 6 months, 1 year, or 2 years postdischarge for satisfaction with appearance (N = 720; table 1), which resulted in including patients who were injured between 2001 and 2013. Satisfaction With Appearance Scale (SWAP) data began being collected in 2003; therefore, participants who had a burn injury in 2001 and 2002 had a SWAP score at their 1- or 2-year follow-up assessments. For depression, data were collected between 2009 and 2012, resulting in the inclusion of 110 participants who had a burn injury between 2003 and 2008 (table 2).
Table 1.
Participant characteristics
| Characteristics | Values |
|---|---|
| Age (y) | 44.05±15.76 |
| Sex | |
| Male | 510 (70.8) |
| Female | 210 (29.2) |
| Race/ethnicity | |
| White, non-Hispanic | 473 (66.4) |
| Black, non-Hispanic | 110 (15.4) |
| Hispanic | 97 (13.6) |
| Asian | 8 (1.1) |
| Native American | 14 (1.9) |
| Multiracial | 4 (0.6) |
| Other | 5 (0.7) |
| Employment status at time of burn | |
| Employed | 478 (67.0) |
| Unemployed | 141 (19.7) |
| Homemaker | 12 (1.7) |
| Retired | 80 (11.2) |
NOTE. Values are mean ± SD or n (%).
Table 2.
Satisfaction with appearance and depression by gender
| Measure | Overall |
Male |
Female |
Burn Years | |||
|---|---|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | ||
| Satisfaction with appearance | 2003–2013 | ||||||
| Discharge | 565 | 27.1±17.8 | 401 | 25.1±17.2 | 164 | 31.9±18.3 | |
| 6mo | 531 | 29.6±18.6 | 375 | 27.7±17.5 | 156 | 34.2±20.2 | |
| 1y | 552 | 28.9±19.3 | 387 | 27.1±18.7 | 165 | 32.9±20.1 | |
| 2y | 720 | 28.3±19.1 | 510 | 26.1±18.8 | 210 | 33.7±18.9 | |
| Depression | 2003–2008 | ||||||
| 5y | 110 | 5.1±5.5 | 70 | 4.9±5.5 | 40 | 5.4±5.5 | |
Procedure
Patients’ informed consent to participate was obtained during admission or discharge from the burn center based on the protocol approved by each center’s human subjects committee. Participants in the current study were injured between 2001 and 2013. Data for the current study were collected at discharge, and at 6 months, 1 year, 2 years, and 5 years after participants’ injuries.
Measures
Satisfaction With Appearance Scale
The SWAP4 is a 14-item questionnaire that assesses subjective appraisal and social behavior components of body image after a burn injury. Patients rate how accurately each item matches their own thoughts and feelings concerning their appearance after the injury on a scale of 0 (strongly disagree) to 6 (strongly agree). Higher scores on the total SWAP score, ranging from 0 to 84, indicate greater dissatisfaction with one’s appearance and poorer body image. The SWAP measure consists of the following 4 factors: subjective satisfaction of appearance with an emphasis on facial features, satisfaction with nonfacial features, social discomfort due to appearance, and perceived social impact. The SWAP total score has good test-retest reliability (r=.59) and excellent internal consistency (α=.87).4
Patient Health Questionnaire-9
The Patient Health Questionnaire-98 is designed to assess symptoms of depression. The 9 items within the module are scored from 0 to 3. A total score is obtained by summing up a patient’s scores on all items, and a cutoff of 10 has been recommended when screening for major depressive disorder.8 The Patient Health Questionnaire-9 total score has good test-retest reliability (r=.82) and excellent internal consistency (α=.86–.89).8
Data analyses
Latent growth curve analysis was used to predict satisfaction with appearance at discharge and at 6 months, 1 year, and 2 years postdischarge as a function of gender and TBSA. Then a longitudinal structural equation model was created to examine how gender and TBSA percentage predict depression 5 years postdischarge through the mediating effect of satisfaction with appearance. Data were analyzed using Mplus version 7.0.a Maximum likelihood estimation procedures use all observations in the data set, regardless of missing data at 1 or more time points, reducing sampling bias. The comparative fit index (CFI; ≥.95), the Tucker-Lewis Index (TLI; ≥.95), and the root-mean-square error of approximation (RMSEA; ≤.08) were used as criteria for good model fit.
Results
Preliminary analyses indicated that 426 participants had SWAP data at all time points for the 2 years postdischarge. A Little’s missing completely at random test was conducted for all variables used in the models, which indicated that data were missing completely at random (, P=.075). When incorporating the final follow-up depression score, 64 participants had full data for the 5-year model. Full information maximum likelihood was used to estimate missing data. Skewness and kurtosis analyses indicated no problems in normality of continuous TBSA, SWAP, or depression scores, with all values <2.0. The average TBSA percentages ranged from 0% to 90% (mean ± SD: 20.31%±17.85%). Twenty percent of individuals indicated clinically significant levels of depression, using a Patient Health Questionnaire-9 cutoff score of 10.8 As expected, SWAP discharge scores were significantly correlated with 5-year depression scores (r=.34, P<.001). Similarly, TBSA and gender scores were significantly associated with SWAP at discharge ([r=.19, P<.001] and [r=−.14, P<.001], respectively). Gender and TBSA were not significantly associated with patients’ 5-year depression score. Descriptive information for SWAP and depression scores by gender is presented in table 2.
Growth curve for satisfaction with appearance
A growth curve model for satisfaction with appearance (SWAP) was initially created. Participants were included in this analysis if they had at least 1 time point for 1 of the 4 time points for SWAP scores (discharge, and 6-mo, 1-y, and 2-y follow-up), which resulted in an analytic sample of 720 patients. First, all 4 time points for SWAP scores were modeled over time to determine whether a growth curve model could be used to represent the data well. Second, the initial levels and changes in SWAP over the first 2 years after discharge were plotted as a function of gender and TBSA. To achieve this first aim, observed SWAP scores at each time point were modeled as a function of an intercept and a linear slope factor, as well as measurement error. The intercept factor represents the systematic variance in SWAP scores when the time is zero, and the slope factor represents the systematic variance of the change in SWAP scores over time. Factor loadings for the intercept factor were set to 1, while factor loadings for the linear slope factor were set to represent the spacing of time between discharge and 2-year follow-up (0, 1, 2, and 4).
A latent growth curve model examining SWAP across the 4 time points did not fit the data well (χ2=74.72, P<.001 [CFI=.94; TLI=.93; RMSEA =.14; 90% CI, .11–.17]). On examining the mean plot of SWAP scores over time of the entire sample (fig 1), a sharp inflection from discharge to 6-month follow-up warranted examination of a quadratic trend. To achieve adequate model fit, a growth curve model with only the 6-month, 1-year, and 2-year follow-up of SWAP scores was examined, since these time points demonstrated a linear trend. As a result, the slope factor loadings were recoded with the 6-month follow-up as baseline (6-mo follow-up=0; 1-y follow-up=1; 2-y follow-up=3). This resulted in an excellent model fit (, P=.256 [CFI=1.0; TLI=.99; RMSEA=.02; 90% CI, .00–.10). There was also a significant correlation between the intercept and slope factor (b=−.28, P<.001), suggesting that patients reporting higher SWAP scores at 6 months had smaller changes in their SWAP score over time.
Fig 1.
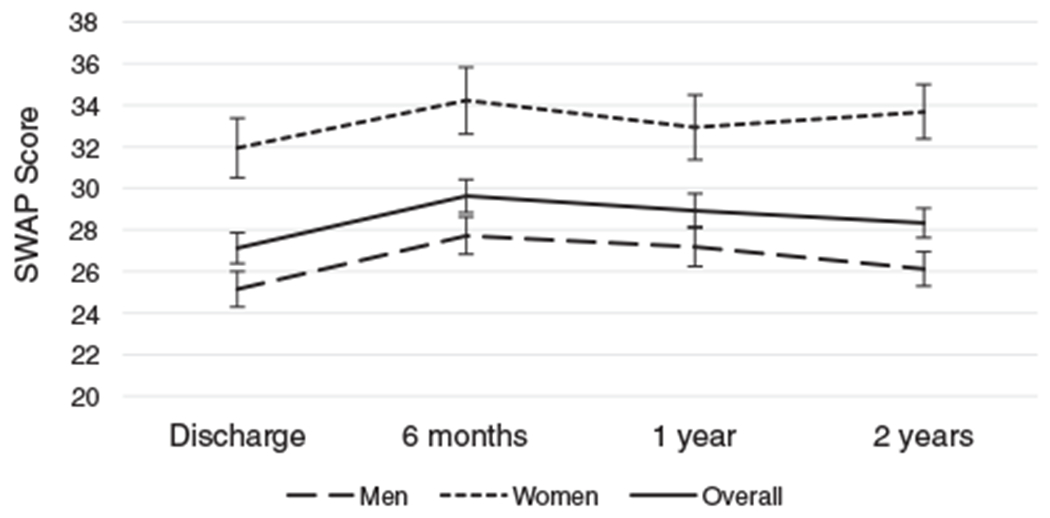
Mean plot of satisfaction with appearance by gender over time.
Next, we added gender and TBSA percent as predictors to the model, controlling for SWAP discharge scores. Participants in this analysis were those who had data for SWAP within at least 1 time point, a TBSA score, and gender reported, resulting in 564 observations. This model resulted in excellent model fit (, P=.314 [CFI=1.0; TLI=1.0; RMSEA=.02; 90% CI, .00–.07). Gender was significantly associated with the intercept factor (b=.26, P=.002). TBSA was also significantly associated with the intercept factor (b=.17, P<.001). SWAP discharge scores were positively associated with the intercept factor (b=.58, P<.001). Neither gender, TBSA, nor SWAP at discharge was associated with the slope factor (P values >.066). This suggests that women had lower satisfaction with appearance at 6-month follow-up compared with men, individuals with greater TBSA had lower satisfaction with appearance at 6-month follow-up than those with less severe TBSA, and individuals with worse overall SWAP scores had worse SWAP scores at discharge. The mean of the slope factor was not significant (P=.983), and the mean trajectory of SWAP scores was relatively flat (see fig 1); therefore, it is unsurprising that the covariates did not predict the rate of change over time.
Longitudinal structural model with satisfaction with appearance and depression
A longitudinal structural equation model was developed to examine the associations between the model covariates and 5-year postdischarge depression scores as mediated by SWAP scores at 6-month follow-up (intercept) and the rate of change in SWAP scores over time (slope), controlling for discharge SWAP scores. Participants in this analysis were again those who had data for SWAP within at least 1 time point, a TBSA score, and gender reported (n=564), 110 of which had available depression scores at the 5-year follow-up. Because full information maximum likelihood estimation was used, the full sample of 564 patient observations was fully included in the model to predict depression scores in the longitudinal structural equation modeling. This model had good fit with an RMSEA of .04 (90% CI, .00–.07), a CFI of 1.0, and a TLI of .98 (, P=.088).
Depression was significantly associated with the intercept factor (b=.53, P<.001). However, depression was not significantly associated with the slope factor (P=.623). This suggests that worse SWAP at 6-month follow-up predicted more depression at 5-year follow-up; however, the rate of change in SWAP scores did not affect 5-year depression.
Gender, TBSA, and SWAP discharge did not significantly directly predict depression scores. However, gender significantly predicted depression through the 6-month follow-up SWAP scores (ie, intercept factor; b=.13, P=.006), but gender did not predict depression through the rate of change in SWAP scores over time (ie, slope). TBSA also predicted depression through the intercept factor (b=.03, P=.00), but not the slope. Likewise, SWAP discharge scores predicted depression through the intercept factor (b=.09, P<.001), but not the slope.
To examine the mediational effects further, bias-corrected bootstrapping with 5000 samples was conducted, indicating a significant mediation of gender on depression through the SWAP intercept (b=.13, 95% CI, .03–.26). This indicates that women had more depression 5 years postdischarge as a function of having worse satisfaction with appearance than men at the 6-month follow-up. There was also a significant mediation of TBSA on depression through the SWAP intercept (b=.01, 95% CI, .00–.01), indicating that patients with greater TBSA had more depression because of having worse satisfaction with appearance at 6-month follow-up. Finally, the association between SWAP discharge scores and depression was also mediated by the SWAP intercept, (b=.02, 95% CI, .01–.03), suggesting that worse satisfaction with appearance at discharge predicted worse satisfaction with appearance at 6 months, and ultimately greater depression 5 years postdischarge. In this final model, 24% of the variance was accounted for in 5-year depression.
Discussion
This is the first study to examine the trajectory of satisfaction with appearance (SWAP) for 2 years after hospital discharge for a burn injury as a function of gender and TBSA, as well as how SWAP levels predict depression 5 years postdischarge. Consistent with our hypothesis, women with burn injury reported significantly higher levels of dissatisfaction with their appearance in comparison to their male counterparts at all time points after discharge. Results build on previous findings demonstrating that women have lower satisfaction with appearance than men, on average, in burn populations.5,9 These gender differences are important because satisfaction with appearance contributes greatly to depressive symptoms in individuals with burn injury and in other chronic illness populations in general.4,10 The findings also support the growing body of literature on the relationship of TBSA to body image.11 Individuals with larger burn areas reported significantly greater body dissatisfaction across the postdischarge 2-year period than those with smaller TBSA. These associations are consistent with those found in other patient populations (eg, skin and breast cancer survivors), suggesting that greater scarring may profoundly affect patients’ satisfaction with appearance.12,13
Although there were gender and TBSA differences in overall SWAP scores, contrary to recent findings5 and our hypotheses, results did not support significant gender or TBSA differences in rate of change in SWAP from 6 months to 2 years after hospital discharge. Established theories explaining the course of adjustment to body disfigurement over time describe an initial stage of body image worsening as individuals respond to the new physical and social demands of the injury,13,14 which did emerge in the current study. However, with time, these theories posit that individuals begin to accept that their condition is, though uncontrollable, tolerable and begin to establish behavioral, cognitive, and social coping skills to help with this period of adjustment.13,14 The overall stable trajectory in SWAP levels after 6 months postdischarge may also be explained by the fact that burns generally heal within the first several months after injury,15 so those first several months may be the most difficult in terms of body dissatisfaction. These changes in body dissatisfaction, in which there is initially an elevation in distress that gradually resolves, are similar to those experienced by patients with vitiligo and breast cancer.14,16 The stability in SWAP score trajectories over the first 2 years after discharge also mirrors the remarkably stable paths of general psychological distress and trauma after a burn injury.17,18
This study further analyzed the indirect effects of SWAP on depressive symptoms 5 years postdischarge. Findings that initial differences in SWAP scores as indicated by the intercept, but not the slope, predicted later depressive symptoms, revealed that overall dissatisfaction with appearance significantly predicts a survivor’s depression. Findings replicate the predictive association between body appearance dissatisfaction and depressive symptoms in patients with scleroderma and cancer.19,20 Moreover, gender and TBSA predicted 5-year depressive symptoms as mediated by 6-month SWAP scores. These findings are consistent with those from recent studies21 and highlight the importance of addressing body image distress in current interventions available for individuals with burn injury, and particularly in women. Because women and those with greater TBSA develop more dissatisfaction with their bodies in comparison to men and those with smaller TBSA, they may be at a heightened risk for poorer psychosocial functioning later on. Results stress the importance of early screening for dissatisfaction with appearance (eg, administering the SWAP) for individuals with burn injury.
It is recommended that individuals with heightened distress/body image dissatisfaction after a burn injury participate in current evidence-based psychosocial interventions (eg, social interaction skills training program and cognitive-behavioral therapy for social anxiety).22,23 These approaches have been shown to be effective in targeting social avoidance behaviors in individuals with burn injury, teaching them skills to manage others’ reactions in social interactions, and to apply these skills in real situations.22,23 To date, research evaluating interventions that specifically target body image satisfaction in individuals with burn injury is necessary but lacking. Future intervention research should focus on specifically addressing individuals’ perceptions of their appearance, targeting maladaptive thought patterns, and measuring changes in SWAP levels for treatment outcome evaluation. In the meantime, patients may greatly benefit from being provided resources for helping with body image dissatisfaction, such as The Body Image Workbook.24,25
Study limitations
This study’s findings should be interpreted in light of several limitations. First, although the relationship of TBSA with body dissatisfaction was examined, information on the visibility of scarring was missing. Because location of injury is a qualitative variable (eg, hands, face, arms, legs), it cannot be integrated into this study’s analyses in a straightforward manner as a predictor. All the analyses required either dichotomous or continuous variables. However, this would be an important direction for future research. Second, this study did not examine personality and specific coping strategies that are known to predict differences in depressive symptoms among individuals with burn injury.26 Further, the importance of appearance seems to play a crucial role in adaptation and coping to a burn injury,27 and future replications of this study would benefit from examination of the effects of this importance on SWAP intercept and trajectories after discharge. Additionally, future studies would benefit from the incorporation of more frequent measurements of satisfaction with appearance within the 6 months after discharge to further understand the nature of changes in body image during this acute recovery period. Research should also incorporate measures of depression before the 5-year postdischarge period, as these data were not available. Similarly, it is important to note attrition across the 5 years of this study. Although analyses suggested that the data are missing at random, and robust estimation methods were used to include all participants’ experiences and minimize biases associated with deletion, it is important for future research to maximize participant retention efforts. Also, depression data were restricted because of the limited period for which depression follow-up scores were collected in the BMS (2009–2013); therefore, a limitation of data availability was not only due to attrition, but also due to the years that the BMS collected data. We included any participant who had data available for at least 1 time point in our analyses. The estimation methods predict patterns using trends to estimate what missing data should be. As a result, simulation studies prove that estimation methods used in this article offer a more justifiable approach to dealing with missing data than deletion.28 Future studies should also control for preinjury depressive symptoms to closely examine longitudinal changes in depressive symptoms as a result of overall SWAP levels and trajectories. It is also unclear whether any gender or TBSA SWAP trajectory differences develop after 2 years, and whether these differences may affect later psychosocial adjustment. Furthermore, since perceived social support, optimism, and indicators of socioeconomic status (eg, employment status) have been associated with depressive symptoms in burn injury patients, it is important to consider the role of these variables in predicting differences in SWAP trajectories in the future.29,30 Finally, it would be important to include other measurements of body dissatisfaction in future studies, as single-reporter biases may underestimate SWAP or depressive symptom levels.
Conclusions
Despite the need for future replication, the findings from the present study extend previous work by longitudinally examining differences in body dissatisfaction for 2 years after a burn injury and for relating these differences to depression 5 years later. Women and those with greater affected body areas had elevated dissatisfaction across the 2 years relative to men and those with a lower TBSA, and these differences were related to greater depressive symptoms 5 years after the burn injury. However, the rate of change in satisfaction with appearance did not significantly differ over the 2-year period. Further research is necessary to comprehend the effects of underlying factors, such as body image importance, personality traits, and scar visibility, on SWAP levels and trajectories over time. Similarly, work is needed to develop and evaluate mental health interventions specifically targeting body dissatisfaction among those who are at a heightened risk (eg, women with greater TBSAs).
Acknowledgments
Support for the Burn Model System National Database is by the U.S. Department of Health and Human Services, National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) in collaboration with the NIDILRR-funded Burn Model System (BMS) centers. However, these contents do not necessarily reflect the opinions or views of the BMS centers, NIDILRR, or the U.S. Department of Health and Human Services.
List of abbreviations:
- BMS
Burn Model Systems
- CFI
comparative fit index
- CI
confidence interval
- RMSEA
root-mean-square error of approximation
- SWAP
Satisfaction With Appearance Scale
- TBSA
total body surface area
- TLI
Tucker-Lewis Index
Footnotes
Disclosures: none.
Supplier
Mplus version 7.0; Muthén & Muthén.
References
- 1.American Burn Association. Burn incidence fact sheet. American Burn Association. 2015. Available at: http://www.ameriburn.org/resources_factsheet.php. Accessed February 6, 2016. [Google Scholar]
- 2.Lawrence JW, Mason ST, Schomer K, Klein MB. Epidemiology and impact of scarring after burn injury. J Burn Care Res 2012;33:136–46. [DOI] [PubMed] [Google Scholar]
- 3.Fauerbach JA, Heinberg LJ, Lawrence JW, Bryant AG, Richter L, Spence RJ. Coping with body image changes following a disfiguring burn injury. Health Psychol 2002;21:115–21. [PubMed] [Google Scholar]
- 4.Lawrence JW, Heinberg LJ, Roca R, Munster A, Spence R, Fauerbach JA. Development and validation of the Satisfaction With Appearance Scale: assessing body image among burn-injured patients. Psychol Assess 1998;10:64–70. [Google Scholar]
- 5.Thombs BD, Notes LD, Lawrence JW, Magyar-Russell G, Bresnick MG, Fauerbach JA. From survival to socialization: a longitudinal study of body image in survivors of severe burn injury. J Psychosom Res 2008;64:205–12. [DOI] [PubMed] [Google Scholar]
- 6.Patterson DR, Everett JJ, Bombardier CH, Questad KA, Lee VK, Marvin JA. Psychological effects of severe burn injuries. Psychol Bull 1993;113:362. [DOI] [PubMed] [Google Scholar]
- 7.Klein MB, Lezotte DL, Fauerbach JA, et al. The National Institute on Disability and Rehabilitation Research Burn Model System Database: a tool for the multicenter study of the outcome of burn injury. J Burn Care Res 2007;28:84–96. [DOI] [PubMed] [Google Scholar]
- 8.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002;32:509–15. [Google Scholar]
- 9.Feingold A, Mazzella R. Gender differences in body image are increasing. Psychol Sci 1998;9:190–5. [Google Scholar]
- 10.Moreira H, Canavarro MC. A longitudinal study about the body image and psychosocial adjustment of breast cancer patients during the course of the disease. Eur J Oncol Nurs 2010;14:263–70. [DOI] [PubMed] [Google Scholar]
- 11.Lawrence JW, Fauerbach JA, Heinberg L, Doctor M. The 2003 clinical research award: visible vs hidden scars and their relation to body esteem. J Burn Care Rehabil 2004;25:25–32. [DOI] [PubMed] [Google Scholar]
- 12.Sobanko JF, Sarwer DB, Zvargulis Z, Miller CJ. Importance of physical appearance in patients with skin cancer. Dermatol Surg 2015;41:183–8. [DOI] [PubMed] [Google Scholar]
- 13.Partridge J. Survival, socialization, and advocacy. J Burn Care Rehabil 2005;26:S32. [Google Scholar]
- 14.Thompson AR, Kent G, Smith JA. Living with vitiligo: dealing with difference. Br J Health Psychol 2002;7:213–25. [DOI] [PubMed] [Google Scholar]
- 15.Nitzschke SL, Aden JK, Serio-Melvin ML, et al. Wound healing trajectories in burn patients and their impact on mortality. J Burn Care Res 2014;35:474–9. [DOI] [PubMed] [Google Scholar]
- 16.Parker PA, Youssef A, Walker S, et al. Short-term and long-term psychosocial adjustment and quality of life in women undergoing different surgical procedures for breast cancer. Ann Surg Oncol 2007; 14:3078–89. [DOI] [PubMed] [Google Scholar]
- 17.Mason ST, Corry N, Gould NF, et al. Growth curve trajectories of distress in burn patients. J Burn Care Res 2010;31:64–72. [DOI] [PubMed] [Google Scholar]
- 18.Mason ST, Lauterbach D, Mckibben JB, Lawrence J, Fauerbach JA. Confirmatory factor analysis and invariance of the Davidson Trauma Scale (DTS) in a longitudinal sample of burn patients. Psychol Trauma 2013;5:10–7. [Google Scholar]
- 19.Benrud-Larson LM, Heinberg LJ, Boling C, et al. Body image dissatisfaction among women with scleroderma: extent and relationship to psychosocial function. Health Psychol 2003;22:130–9. [PubMed] [Google Scholar]
- 20.Goldzweig G, Meirowitz A, Hubert A, et al. Meeting expectations of patients with cancer: relationship between patient satisfaction, depression, and coping. J Clin Oncol 2010;28:1560–5. [DOI] [PubMed] [Google Scholar]
- 21.Thombs BD, Haines JM, Bresnick MG, Magyar-Russell G, Fauerbach JA, Spence RJ. Depression in burn reconstruction patients: symptom prevalence and association with body image dissatisfaction and physical function. Gen Hosp Psychiatry 2007;29:14–20. [DOI] [PubMed] [Google Scholar]
- 22.Blakeney P, Thomas C, Holzer C, Rose M, Berniger F, Meyer WJ. Efficacy of a short-term, intensive social skills training program for burned adolescents. J Burn Care Rehabil 2005;26:546–55. [DOI] [PubMed] [Google Scholar]
- 23.Cukor J, Wyka K, Leahy N, Yurt R, Difede J. The treatment of posttraumatic stress disorder and related psychosocial consequences of burn injury. J Burn Care Res 2015;36:184–92. [DOI] [PubMed] [Google Scholar]
- 24.Cash TF. The body image workbook: an eight-step program for learning to like your looks. Oakland: New Harbinger Publications; 2008. [Google Scholar]
- 25.Cash TF, Smolak L. Body image: a handbook of science, practice, and prevention. New York: Guilford Pr; 2011. [Google Scholar]
- 26.Andrews RM, Browne AL, Drummond PD, Wood FM. The impact of personality and coping on the development of depressive symptoms in adult burns survivors. Burns 2010;36:29–37. [DOI] [PubMed] [Google Scholar]
- 27.Lawrence JW, Fauerbach JA, Thombs BD. A test of the moderating role of importance of appearance in the relationship between perceived scar severity and body-esteem among adult burn survivors. Body Image 2006;3:101–11. [DOI] [PubMed] [Google Scholar]
- 28.Enders C, Bandalos D. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct Equ Modeling 2001;8:430–57. [Google Scholar]
- 29.He F, Zhou Q, Zhao Z, Zhang Y, Guan H. Effect of perceived social support and dispositional optimism on the depression of burn patients. J Health Psychol 2014;21:1119–25. [DOI] [PubMed] [Google Scholar]
- 30.Tedstone JE, Tarrier N, Faragher EB. An investigation of the factors associated with an increased risk of psychological morbidity in burn injured patients. Burns 1998;24:407–15. [DOI] [PubMed] [Google Scholar]


