Abstract
Introduction:
Despite many advances in burn care, the development of extremity contracture remains a common and vexing problem. Extremity contractures have been documented in up to one third of severely burned patients at discharge. However, little is known about the long-term impact of these contractures. The purpose of this study was to examine the association of extremity contractures with employment after burn injury.
Methods:
We obtained data from the Burn Model System database from 1994 to 2003. We included in the study cohort all adult patients who were working prior to injury and identified those discharged with and without a contracture in one of the major extremity joints (shoulder, elbow, wrist, hip, knee and ankle). We classified contracture severity according to mild, moderate and severe categories. We performed descriptive analyses and predictive modeling to identify injury and patient factors associated with return to work (RTW) at 6, 12, and 24 months.
Results:
A total of 1,203 participant records met criteria for study inclusion. Of these, 415 (35%) had developed a contracture at discharge; 9% mild, 12% moderate, and 14% severe. Among 801 (67%) participants who had complete data at 6 months after discharge, 70% of patients without contracture had returned to work compared to 45% of patients with contractures (p < 0.001). RTW increased at each subsequent follow-up time point for the contracture group, however, it remained significantly lower than in no-contracture group (both p < 0.01). In multivariable analyses, female sex, non-Caucasian ethnicity, larger burn size, alcohol abuse, number of in-hospital operations, amputation, and in-hospital complications were associated with a lower likelihood of employment. In adjusted analyses, discharge contracture was associated with a lower probability of RTW at all 3 time points, although its impact significantly diminished at 24 months.
Conclusions:
This study indicates an association between discharge contracture and reduced employment 6, 12 and 24 months after burn injury. Among many other identified patient, injury, and hospitalization related factors that are barriers to RTW, the presence of a contracture at discharge adds a significant reintegration burden for working-age burn patients.
Keywords: Scarring, Burn sequelae, Reintegration, Physical activity, Employment
1. Introduction
In modern burn care, extremity contractures affect up to one in three severely burned patients, a rate essentially unchanged over the past several decades [1,2]. Extremity contractures cause very specific morbidity for survivors as limitations in passive and active range of motion (ROM) interfere with daily living. Contractures in the upper extremities impair the survivor’s ability to eat, write, groom and get dressed. Contractures in the lower extremities impair walking and transfers [3-5]. Altogether, burn scar extremity contractures may significantly challenge the survivor’s ability to effectively reintegrate into a productive role in society.
There is a significant gap in knowledge about the impact of extremity contractures on the livelihood of burn survivors. As prescribed, rehabilitation exercises involve significant time and energy for patients to not only maintain but improve ROM. Some may modify their activities over time and adapt as most daily activities do not use all joints to move through their entire range [6]. More severe joint contractures may be treated with surgical release and additional rehabilitation, although recurrences are common [7-10].
Employment/return to work (RTW) is a significant milestone of functional recovery as a source of revenue, personal identity and life satisfaction [11,12]. A 2012 systematic review by Mason and colleagues indicated that up to 28% of burn survivors never return to any form of employment, highlighting the personal and societal cost of burn injuries [13]. Factors such as injury severity, physical ability, and psychological symptoms pose significant barriers to RTW [14-16]. Even smaller injuries can cause significant loss of productivity [17]. Physical barriers to employment, such as reduced ROM and mobility, have been qualitatively reported in multiple patient surveys [18,19]. However, the specific association of extremity contractures on proportion of those who RTW is not known. We hypothesize that burn scar extremity contracture is associated with a persistently lower return to employment for up to 2 years after injury.
2. Methods
2.1. Study design
This was a retrospective analysis of working-age adults (age 18–64 years) who were prospectively enrolled in the longitudinal Burn Model System (BMS) National Database from 1994 to 2003. This enrollment period was chosen because of detailed ROM data were collected as part of the longitudinal database. The primary outcome of interest was proportion of those who return to work.
2.2. Study setting
The National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) has funded the BMS research program since 1993. Three participating burn centers in the BMS project contributed patients to this study by enrolling adult patients into the database and included: The Johns Hopkins Burn Center, the University of Washington Medicine Regional Burn Center, and the University of Texas Southwestern Medical Center. For patients aged 18–64 years, criteria for inclusion in the BMS database were: burns ≥20% TBSA, or burns to critical areas (the hands, face or feet), or high voltage electrical injury. Full inclusion and exclusion criteria to BMS enrollment can be found at http://burndata.washington.edu/standard-operating-procedures. All patients provided their own consent for enrollment. Complete documentation of the project, data acquisition processes, and verification strategies have been previously described [20]. Institutional Review Boards at each of the BMS participating institutions have approved participant enrollment into the BMS longitudinal database. This study was a secondary data analysis of de-identified data.
2.3. Subjects and study variables
We abstracted de-identified data for participants aged 18–64 years enrolled in the BMS national database who were working prior to injury. ROM measurements in the shoulder, elbow, wrist, hip, knee and ankle joints were recorded in the dataset according to the BMS data dictionary definitions [21]. The presence of hand contractures was categorized as a covariate in this study. Given the number of joints in each hand, including hand contractures and their degrees of severity would add too many variables to this analysis. Participants were defined as having an extremity contracture at discharge if they did not have full, active ROM at any of the specified joints. For each joint, the severity of contracture was assigned by clinicians to the mild, moderate, or severe category. Each category was defined by dividing equally in thirds the normal ROM value for that joint [1]. We obtained data on potential pre-injury factors that may affect RTW outcome, including age, sex, race, payer status, employment-related injury, self-reported history of alcohol or drug abuse, comorbidity and physical disability. Clinical and treatment variables included total body surface area (TBSA) burned and grafted, acute hospital length of stay, inhalation injury, ventilator days, number of in-hospital operations, amputation due to burn, study enrollment site, neuropathy and development of heterotopic ossification. The primary outcome of RTW was collected at 6+/−2 months, 12+/−3 months, and 24+/−6 months after injury.
2.4. Data analyses
We used descriptive statistics to compare those with and without extremity contracture at discharge with respect to pre-injury, injury, and treatment factors. We estimated both unadjusted and adjusted models to determine the association between extremity contracture and employment at each time point. We performed multivariable logistic regression for employment and derived a parsimonious model that included significant factors associated with employment outcome. We included interaction variables between contracture and time points. We used marginal effects, a standard method for estimation in the setting of significant interactions, to report the relative contribution of extremity contracture to RTW at 6, 12, and 24 months [22]. Regression diagnostics tested model assumptions and fit. We also performed additional exploratory analyses including: the impact of upper vs. lower extremity contractures, and severity of contracture (worst site, or cumulative severity) on employment. We tabulated joint contractures by specific anatomic location (shoulder, elbow, wrist, hip, knee, ankle) to better understand their distributions. We grouped them by upper vs. lower extremity, as well as by laterality. To categorize by cumulative severity, we assigned a score (0 = none, 1 = mild, 2 = moderate, 3 = severe) for affected joint per individual and summed the total score. With each of these new exposure variables, we repeated the multivariable logistic regression for employment at 6, 12 and 24 months. Final model performance was evaluated for internal validation by bootstrapping method, for goodness of fit by calibration plot, and for discrimination using the C-statistic.
3. Results
3.1. Participant characteristics
We identified 1,203 participants in the dataset who were working prior to injury and discharged alive. Of these, 415 (35%) developed an extremity contracture by hospital discharge (Fig. 1). Table 1 describes upper and lower extremity contractures according to severity, and in combination. For the upper extremity, 886 individuals (74%) had no contracture, 120 (10%) had a mild contracture, 133 (11%) had a moderate contracture, and 64 (5%) had a severe contracture. For the lower extremity, 1,024 individuals (85%) with no contracture, 25 (2%) with mild contracture, 42 (3%) with moderate contracture, 112 (9%) with severe contracture. The highest proportion of upper extremity-only contractures was moderate (44%, n = 103), whereas most contractures in the lower extremity-only were characterized as severe (62%, n = 61). Of all patients with contractures, 81 (20%) had combined upper and lower extremity deficits.
Fig. 1 –
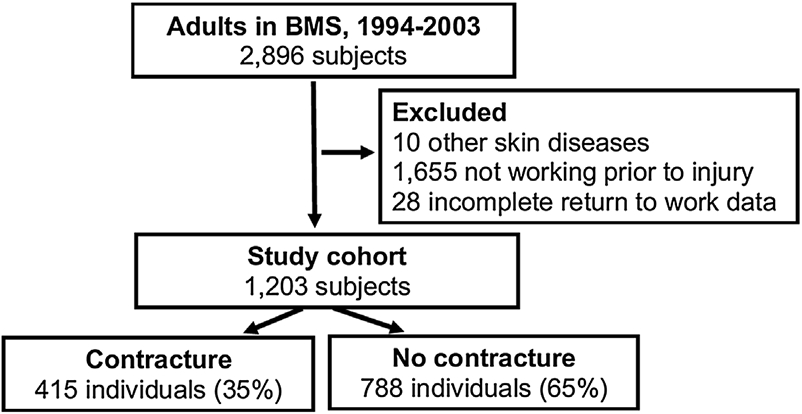
Study flow diagram and distribution of extremity contractures, diagnosed at hospital discharge.
Table 1 –
Distribution of extremity contractures, diagnosed at hospital discharge. The severity of contracture was assigned to mild, moderate, or severe category by dividing equally in thirds the normal ROM value for that joint [1].
| Lower extremity | |||||
|---|---|---|---|---|---|
| Severity | None | Mild | Moderate | Severe | |
| Upper extremity | None | 788 | 15 | 22 | 61 |
| Mild | 86 | 4 | 9 | 21 | |
| Moderate | 103 | 4 | 6 | 20 | |
| Severe | 47 | 2 | 5 | 10 | |
Most participants were male (83%), with a mean age of 37 years. Those discharged with a contracture had a higher mean burn size (TBSA; as well as grafted TBSA) and were more likely to have sustained inhalation injury and pre-injury comorbidity. Days on mechanical ventilation and percentage with complications were significantly higher in the group that developed extremity contracture (Table 2).
Table 2 –
Patient, injury and treatment characteristics, by discharge contracture status.
| Category | No contracture N = 788 |
Contracture N = 415 |
P-value |
|---|---|---|---|
| Age | 37 (12) | 37 (11) | 0.59 |
| Percent male | 83 | 83 | 0.79 |
| TBSA | 15 (15) | 25 (18) | <0.01 |
| TBSA grafted | 5.7 (9) | 12.6 (12.2) | <0.01 |
| Percent with inhalation injury | 7 | 13 | <0.01 |
| Percent with co-morbidity | 24 | 30 | 0.03 |
| Days on mechanical ventilation | 1.8 (9.9) | 5.3 (13.2) | <0.01 |
| Percent with in-hospital complication(s) | 13 | 35 | <0.01 |
3.2. Handling of missing post-discharge RTW data
There were 402 individuals (33%) with missing RTW data at 6 months, 504 (42%) at 12 months, and 602 (50%) at 24 months. A significant proportion of non-response is to be expected in prospective multicenter longitudinal data projects among burn-injured patients. Nevertheless, it prompted us to perform an analysis of specific patient and injury characteristics to verify whether the missingness was non-random [23]. At 6 months after injury, we found that the proportion of male patients, mean injury TBSA, number of operations, ventilator days, number of contractures and severity were not statistically different between responders and non-responders. In contrast, non-responders were slightly older (mean 38.5 vs. 35.3 years, p < 0.01), had larger mean TBSA area grafted (9.3 vs. 7.2%, p < 0.01), and more likely to be non-Caucasian (42% vs. 29%, p < 0.01).
3.3. Factors associated with employment
Among 801 (67%) participants who had complete data at 6 months after discharge, 70% of patients without contracture had returned to work compared to 45% of patients with contractures (p < 0.001). At 12 months, 78% of patients withoutdischarge contracture were working compared to 57% with contracture (p < 0.01, 699 participants with complete data). At 24 months, 81% without discharge contracture were working compared to 65% with contracture (p < 0.01, 601 complete data). By univariate analysis, we identified that the following factors had a p ≤ 0.05 level of association with employment: non-Caucasian race, insurance status, comorbidity, history of drug and alcohol use disorder, recent pre-burn psychiatric treatment. Associated etiology and severity factors included: flame burns, burn size, inhalation injury, extremity burn. Associated treatment factors included enrollment site, TBSA grafted, number of operations, amputation, ventilator days, in-hospital complications, and the development of neuropathy and heterotopic ossification. By multivariable regression analyses, we confirmed several pre-injury factors associated with a lower likelihood of RTW: female sex, non-Caucasian race, and self-reported pre-injury alcohol abuse, which is consistent with prior literature [11,24]. A larger burn size was associated with a lower likelihood of RTW (adjusted OR: 0.96 per additional percent burn, 95% CI 0.94–0.99, p = 0.003). Among treatment factors, a higher number of operations, amputation, and in-hospital complication(s) predicted a lower likelihood of RTW (Table 3). We identified significant interactions between extremity contracture and time points after injury in the multivariable analysis. Thus, we chose marginal effects to report relative associations. At 6 months, extremity contracture was associated with a 27% lower likelihood of employment. At 12 months, it was 21%. At 24 months, it was reduced to 14%. We also noted that at 24 months, confidence intervals in the marginal effect nearly overlapped, demonstrating that the impact of extremity contracture had decreased over time (Table 4). The final regression model performance was verified as acceptable using bootstrapping method, calibration plot, and C-statistic (AUC 0.809). In exploratory analyses, we found no consistent association between contractures in specific joints, laterality, upper extremity vs. lower extremity, worst severity or aggregate severity to employment outcomes (data not shown).
Table 3 –
Significant predictors of return to employment (from final multivariable model).
| Category | Adjusted odds ratio | 95% CI | P-value |
|---|---|---|---|
| Female sex | 0.18 | 0.08–0.41 | <0.001 |
| Non-Caucasian ethnicity | 0.16–0.35 (depending on ethnicity) | 0.04–0.89 | 0.03 |
| TBSA burn (per percent) | 0.96 | 0.94–0.99 | 0.003 |
| Alcohol abuse | 0.2 | 0.07–0.6 | 0.004 |
| # Operations (per operation) | 0.49 | 0.38–0.63 | <0.001 |
| Amputation | 0.04 | 0.01–0.15 | <0.001 |
| In-hospital complication(s) | 0.18 | 0.07–0.49 | 0.001 |
Table 4 –
Adjusted marginal estimates at each time point, by contracture status.
| Time point | Contracture | Adjusted margins | 95% CI |
|---|---|---|---|
| 6 months | No | 0.71 | 0.67–0.74 |
| Yes | 0.48 | 0.43–0.53 | |
| 12 months | No | 0.80 | 0.77–0.83 |
| Yes | 0.57 | 0.52–0.62 | |
| 24 months | No | 0.82 | 0.79–0.85 |
| Yes | 0.64 | 0.58–0.69 |
4. Discussion
A persistently high rate of burn scar contractures is one of the most vexing problems in modern burn care [1,2]. The present study expands on previous work by examining the associations of extremity contractures on RTW. Our principal finding is that extremity contracture is independently associated with lower return to work at 6 months, 12 months and 24 months after injury. This association was strongest at 6 months and decreased progressively to 24 months, although it remained significant. While association does not imply causality, this correlation appears credible from a mechanistic standpoint. To our knowledge, this is the first study that attempts to quantify the impact of burn contractures on return to work.
Employment is a critical source of identity, financial independence and community participation. Our findings support the notion that extremity contracture after burns represents a significant and persistent barrier to work as a reintegration milestone. Although we considered RTW as binary outcome in this study, employment is more accurately a continuum that includes partial vs. full duties, partial vs. full time, and work adaptations. In this regard, additional burn healthcare team advocacy for services such as work hardening and other accommodations can improve employment rates after injury. Carrougher et al. reported that advocacy and education by the burn team can help achieve a high RTW rate (up to 93%) [12]. Interestingly, 31% of patients in that study were provided some workplace accommodation to facilitate RTW. Burn survivors with work-related injuries may report significant physical limitations, fear and difficulty returning to the same job [15,16]. Our cohort study also indicates that women and non-Caucasians are less likely to RTW. In addition, older patients and non-Caucasians have a higher likelihood of non-response, further suggesting disparity. Although these factors are themselves not modifiable, there are likely opportunities to improve on RTW rates in vulnerable groups and individuals through targeted interventions [12,24-27]
In order to maximize the functional goal of employment, clinicians must optimize two important strategies: the prevention of contractures and the mitigation of contractures once they develop. Extremity contractures occur despite aggressive prevention and management strategies supported by practice guidelines [28-30]. Contractures often develop insidiously during recovery as excessive skin fibrosis, immobility and suboptimal positioning all contribute to motion limitation. The severity of joint contractures depends on injury factors such as depth, extent and location of burn, patient factors such as genetic predisposition, age, and adherence to therapy exercises, and treatment factors such as timing of wound closure, mobility and splinting strategies [3,31]. New strategies currently implemented in acute care for burn excision and skin closure (enzymatic debridement, sprayon skin) may affect joint contracture development. As such, their impact on hospitalization and outcomes need to be carefully documented [32,33]. Additionally, the current wave of adoption of early mobility protocols in intensive care units coupled with lighter sedation strategies, and early resumption of range of motion exercises after skin grafting may hold the promise of shorter length of acute hospitalization [34-36]. Altogether, these developments are hopefully reducing the incidence of burn scar contractures in the current era.
Improvements in care after discharge may also mitigate contracture severity and impact. For instance, better transitional care, including close collaboration between surgical and rehabilitation services, frequent patient visits and remote care may improve providers’ ability to monitor progress and support burn survivors in their recovery [37-39]. However, more episodes of care (whether in-person or remote) may not be sufficient given the persistence of skin contraction and scarring over months. Perhaps improving patient adherence to a prescribed program is the key ingredient. In addition to injury, social and economic factors, patient adherence appears related to engagement in the program, perceived efficacy and barriers, positive feedback and support, and patient self-efficacy [40-42].
Can newer technology tools assist in improving ROM and reduce the effects of contractures? Prior work has demonstrated a high level of patient engagement and satisfaction when interactive gaming is used in conjunction with burn therapy [43,44]. In a prospective randomized trial in children, the addition of video game therapy achieved faster gains in ROM at 3 months follow-up compared to standard therapy [45]. We recently completed a study of feasibility, acceptability and safety by enrolling 20 hospitalized burn patients to participate in a single Kinect-based training session. Participants found the modules challenging, yet easy to follow. They also expressed a high level of support for these modules, with acceptable pain and safety levels [46]. A current NIDILRR supported trial is seeking to enroll 50 subjects over 5 years to test whether post-discharge technology-assisted rehabilitation training improves adherence to exercises and activity after discharge (NCT0347654, clinicaltrials.gov).
4.1. Study limitations
There are several important limitations of this retrospective cohort study. These data were collected from 1994 to 2003, when the BMS Database collected detailed ROM measurements, and therefore reflect standard practice from that period. However, we contend that these data are still applicable in terms of the impact on return to work. We performed a number of exploratory analyses but could not clearly determine a consistent association between the aggregate number of contractures, the combination of contractures in specific joints (including laterality), nor the severity of contractures and the primary outcome of interest. We theorize that this cohort had insufficient patient and contracture numbers to study these individual correlations. We were also not able to assess more granular employment outcomes such as part-time work, resumption of prior job duties vs. work accommodations. The latter is an important factor for workers with more intensive manual job duties. It is likely more difficult to return to the same duties given physical limitations, and many individuals and job sites may not have the necessary job training/availability to transition to office work. Altogether, these factors might have mitigated our ability to assess the impact of number of contractures and their severity. Also, this study considered hand contractures as a binary covariate, as the number of joints in each hand would add too much complexity and variables to the analyses. We, of course, acknowledge that suboptimal hand motion is most likely a key factor in RTW. Finally, an extremity contracture diagnosed at discharge does not imply that this represents a fixed deficit for the patient. Our study does not evaluate specific trajectories of recovery based on contracture.
5. Conclusions
An extremity contracture after burn injury is associated with lower employment at 6, 12 and 24 months after injury. As a physical limitation, extremity contracture represents a significant functional barrier to employment. The long-term impact highlights not only the need to support individuals with extremity contractures but also calls for novel strategies to prevent and mitigate extremity contractures as part of comprehensive burn treatment.
Acknowledgement
The contents of this publication were developed in part under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant numbers 90DP0029,90DPBU0001, 90DPBU0004). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Abbreviations:
- AUC
area under the curve
- BMS
Burn Model System
- NIDILRR
National Institute on Disability, Independent Living, and Rehabilitation Research
- ROM
range of motion
- RTW
return to work
- TBSA
total body surface area
REFERENCES
- [1].Goverman J, Mathews K, Goldstein R, et al. Adult contractures in burn injury: a burn model system national database study. J Burn Care Res 2017;38:e328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Schneider JC, Holavanahalli R, Helm P, et al. Contractures in burn injury: defining the problem. J Burn Care Res 2006;27:508–14. [DOI] [PubMed] [Google Scholar]
- [3].Dewey WS, Richard RL, Parry IS. Positioning, splinting, and contracture management. Phys Med Rehabil Clin N Am 201122: 229–47, v. [DOI] [PubMed] [Google Scholar]
- [4].Dudek NT G. Joint contractures. In: Silver JR TD, editor. Essentials of physical medicine and rehabilitation. Saunders/Elsevier; 2008. p. 651–5. [Google Scholar]
- [5].Leblebici B, Adam M, Bagis S, et al. Quality of life after burn injury: the impact of joint contracture. J Burn Care Res 2006;27:864–8. [DOI] [PubMed] [Google Scholar]
- [6].Korp K, Richard R, Hawkins D. Refining the idiom “functional range of motion” related to burn recovery. J Burn Care Res 2015;36:e136–45. [DOI] [PubMed] [Google Scholar]
- [7].Carmichael KD, Maxwell SC, Calhoun JH. Recurrence rates of burn contracture ankle equinus and other foot deformities in children treated with Ilizarov fixation. J Pediatr Orthop 2005;25:523–8. [DOI] [PubMed] [Google Scholar]
- [8].Frame JD, Still J, Lakhel-LeCoadou A, et al. Use of dermal regeneration template in contracture release procedures: a multicenter evaluation. Plast Reconstr Surg 2004;113:1330–8. [DOI] [PubMed] [Google Scholar]
- [9].Iwuagwu FC, Wilson D, Bailie F. The use of skin grafts in postburn contracture release: a 10-year review. Plast Reconstr Surg 1999;103:1198–204. [DOI] [PubMed] [Google Scholar]
- [10].Jones T, McDonald S, Deitch EA. Effect of graft bed on long-term functional results of extremity skin grafts. J Burn Care Rehabil 1988;9:72–4. [DOI] [PubMed] [Google Scholar]
- [11].Brych SB, Engrav LH, Rivara FP, et al. Time off work and return to work rates after burns: systematic review of the literature and a large two-center series. J Burn Care Rehabil 2001;22:401–5. [DOI] [PubMed] [Google Scholar]
- [12].Carrougher GJ, Brych SB, Pham TN, et al. An intervention bundle to facilitate return to work for burn-injured workers: report from a burn model system investigation. J Burn Care Res 2017;38:e70–8. [DOI] [PubMed] [Google Scholar]
- [13].Mason ST, Esselman P, Fraser R, et al. Return to work after burn injury: a systematic review. J Burn Care Res 2012;33:101–9. [DOI] [PubMed] [Google Scholar]
- [14].Esselman PC, Askay SW, Carrougher GJ, et al. Barriers to return to work after burn injuries. Arch Phys Med Rehabil 2007;88:S50–6. [DOI] [PubMed] [Google Scholar]
- [15].Schneider JC, Bassi S, Ryan CM. Employment outcomes after burn injury: a comparison of those burned at work and those burned outside of work. J Burn Care Res 2011;32:294–301. [DOI] [PubMed] [Google Scholar]
- [16].Schneider JC, Shie VL, Espinoza LF, et al. Impact of work-related burn injury on social reintegration outcomes: a life impact burn recovery evaluation (LIBRE) study. Arch Phys Med Rehabil 2020;101(1S):S86–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Goei H, Hop MJ, van der Vlies CH, et al. Return to work after specialised burn care: a two-year prospective follow-up study of the prevalence, predictors and related costs. Injury 2016;47:1975–82. [DOI] [PubMed] [Google Scholar]
- [18].Kornhaber R, Wilson A, Abu-Qamar MZ, McLean L. Adult burn survivors’ personal experiences of rehabilitation: an integrative review. Burns 2014;40:17–29. [DOI] [PubMed] [Google Scholar]
- [19].Mackey SP, Diba R, McKeown D, et al. Return to work after burns: a qualitative research study. Burns 2009;35:338–42. [DOI] [PubMed] [Google Scholar]
- [20].Godleski M, Lee AF, Goverman J, et al. Quantifying contracture severity at hospital discharge in adults: a burn model system national database study. J Burn Care Res 2018;39:604–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Goverman J, Mathews K, Holavanahalli RK, et al. The national institute on disability, independent living, and rehabilitation research burn model system: twenty years of contributions to clinical service and research. J Burn Care Res 2017;38:e240–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Norton EC, Dowd BE, Maciejewski ML. Marginal effects-quantifying the effect of changes in risk factors in logistic regression models. JAMA 2019;321(13):1304–5. [DOI] [PubMed] [Google Scholar]
- [23].Hughes RA, Heron J, Sterne JAC, Tilling K. Accounting for missing data in statistical analyses: multiple imputation is not always the answer. Int J Epidemiol 2019;48(4):1294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Levi B, Kraft CT, Shapiro GD, et al. The associations of gender with social participation of burn survivors: a life impact burn recovery evaluation profile study. J Burn Care Res 2018;39:915–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Arango-Lasprilla JC, Ketchum JM, Stevens LF, et al. Ethnicity/racial differences in employment outcomes following spinal cord injury. NeuroRehabilitation 2009;24:37–46. [DOI] [PubMed] [Google Scholar]
- [26].Razmjou H, Lincoln S, Macritchie I, et al. Sex and gender disparity in pathology, disability, referral pattern, and wait time for surgery in workers with shoulder injury. BMC Musculoskelet Disord 2016;17:401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Smith CK, Anderson NJ. Work-related injuries among commercial janitors in Washington State, comparisons by gender. J Safety Res 2017;62:199–207. [DOI] [PubMed] [Google Scholar]
- [28].Nedelec B, Parry I, Acharya H, et al. Practice guidelines for cardiovascular fitness and strengthening exercise prescription after burn injury. J Burn Care Res 2016;37:e539–58. [DOI] [PubMed] [Google Scholar]
- [29].Parry I, Forbes L, Lorello D, et al. Burn rehabilitation therapists competency tool-version 2: an expansion to include long-term rehabilitation and outpatient care. J Burn Care Res 2017;38:e261–8. [DOI] [PubMed] [Google Scholar]
- [30].Serghiou MA, Niszczak J, Parry I, Richard R. Clinical practice recommendations for positioning of the burn patient. Burns 2016;42:267–75. [DOI] [PubMed] [Google Scholar]
- [31].Klein MB, Logsetty S, Costa B, et al. Extended time to wound closure is associated with increased risk of heterotopic ossification of the elbow. J Burn Care Res 2007;28:447–50. [DOI] [PubMed] [Google Scholar]
- [32].Ryan CM, Parry I, Richard R. Functional outcomes following burn injury. J Burn Care Res 2017;38:e614–7. [DOI] [PubMed] [Google Scholar]
- [33].Schneider JC, Chen L, Simko LC, et al. Challenges to the standardization of burn data collection: a call for common data elements for burn care. J Burn Care Res 2018;39:201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Parry I, Sen S, Palmieri T, Greenhalgh D. Current trends in practice for early mobility with the burn population. J Burn Care Res 2019;40:29–33. [DOI] [PubMed] [Google Scholar]
- [35].Schaller SJ, Anstey M, Blobner M, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 2016;388:1377–88. [DOI] [PubMed] [Google Scholar]
- [36].Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009;373:1874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Espinoza LF, Simko LC, Goldstein R, et al. Post-acute care setting is associated with employment after burn injury. Arch Phys Med Rehabil 2019;100(11):2015–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Hickey S, Gomez J, Meller B, et al. Interactive home telehealth and burns: a pilot study. Burns 2017;43:1318–21. [DOI] [PubMed] [Google Scholar]
- [39].Liu YM, Mathews K, Vardanian A, et al. Urban telemedicine: the applicability of teleburns in the rehabilitative phase. J Burn Care Res 2017;38:e235–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Beinart NA, Goodchild CE, Weinman JA, et al. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J 2013;13:1940–50. [DOI] [PubMed] [Google Scholar]
- [41].Essery R, Geraghty AW, Kirby S, Yardley L. Predictors of adherence to home-based physical therapies: a systematic review. Disabil Rehabil 2017;39:519–34. [DOI] [PubMed] [Google Scholar]
- [42].Miller KK, Porter RE, DeBaun-Sprague E, et al. Exercise after stroke: patient adherence and beliefs after discharge from rehabilitation. Top Stroke Rehabil 2017;24:142–8. [DOI] [PubMed] [Google Scholar]
- [43].Schneider JC, Ozsecen MY, Muraoka NK, et al. Feasibility of an exoskeleton-based interactive video game system for upper extremity burn contractures. PM R 2016;8:445–52. [DOI] [PubMed] [Google Scholar]
- [44].Voon K, Silberstein I, Eranki A, Phillips M, et al. Xbox Kinect based rehabilitation as a feasible adjunct for minor upper limb burns rehabilitation: a pilot RCT. Burns 2016;42:1797–804. [DOI] [PubMed] [Google Scholar]
- [45].Parry I, Painting L, Bagley A, et al. A pilot prospective randomized control trial comparing exercises using videogame therapy to standard physical therapy: 6 months follow-up. J Burn Care Res 2015;36:534–44. [DOI] [PubMed] [Google Scholar]
- [46].Pham TN, Wong JN, Terken T, et al. Feasibility of a Kinect((R))-based rehabilitation strategy after burn injury. Burns 2018;44:2080–6. [DOI] [PubMed] [Google Scholar]


