Abstract
Background/purpose
Bone quality may affect the implantation protocol. This study aimed to assess whether training protocols could improve novice dental practitioners’ abilities in judging bone densities with tactile sensation.
Materials and methods
Twenty-five operators were recruited to evaluate the density of artificial polyurethane bone blocks by a 2-mm twist-drill drilling and reported the bone quality perceived in a 100-mm VAS line. Five blocks (densities: 0.08–0.48 g/cm3) were used to simulate cancellous bone with extremely low to medium–high densities. Five tests were performed on three days, separated by one week and one month. A training session was arranged on the first day and the third day. In each test, the operator drilled a 0.8 g/cm3 block as the reference (VAS = 100) and then the five test blocks in a randomized sequence. Each training session included a 0.8 g/cm3 followed by five 0.16 and 0.32 g/cm3 alternative block-drillings. VAS values and number of density-sequencing errors were analyzed with GLM repeated measures and Friedman test.
Results
While mean VAS values were significantly different among the five test blocks, it was not noticed in blocks of the same density between test sessions. Significant linear correlations were observed between VAS values and block densities. Training did not influence the VAS evaluation and hardness sequencing in general but training significantly reduced the sequencing errors in operators with inferior initial performance.
Conclusion
The proposed training protocol can improve the bone-quality perception among less experience dentists with poorer initial performance in bone density evaluation.
Keywords: Artificial bone blocks, Bone quality, Dental education, Dental implant, Tactile sensation
Introduction
Bone quality and bone quantity have been reported to be two important factors determining the success of dental implant treatment.1 Higher implant failure rates were noted when dental implants were placed in bone with poor quality.2,3 Various surgical techniques and implant designs have been proposed to achieve better primary stability in poor-quality bones and to improve the long-term prognosis.4, 5, 6, 7, 8, 9, 10, 11 On the other hand, bone quality usually defines the surgical technique to be adopted and the implant design to be selected. Manufacturers also recommend specific implant site preparation protocols according to different bone qualities for most implant systems.
Many clinicians utilize the perception of drilling with a 2-mm twist drill for assessing variations in bone density at the implant site. A survey suggested that the most popular method for assessing bone quality among Swedish specialists was the hand-felt perception of drilling resistance.12 The tactile feedback provided by the 2-mm twist drill is considered crucial for identifying bone quality. Drilling provides information of cortical bone thickness and trabecular bone density. Most dentists classified bone quality into four types according to the classification proposed by Lekholm and Zarb in 1986.13 Mish compared the perception of drilling into four types of mineralized bone to drilling into oak or maple, pine or spruce, balsa wood, and Styrofoam®, respectively. Thus, evaluating bone density is critically essential for deciding the depth and width of an osteotomy, undersizing the drilling sequence, selecting a tapered vs. non-tapered implant, countersinking, immediate loading and healing time. The clinician usually decides on the surgical drilling protocol to be selected according to tactile feedback from a 2-mm twist drill. Although assessing bone quality has been deemed crucial for implant therapy, to our knowledge, few studies have evaluated the reliability of surgeons' perception in the assessment of bone quality. Trisi and Rao demonstrated that hand feeling could help differentiate D1 from D4 bone but failed to distinguish between the intermediate classes of bone quality.14 Our previous investigation found only a slight discrepancy in bone classification among specialists but wide variations in performance between specialists and general practitioners as well as among general practitioners,15 indicating a need to develop a calibration system for reducing such differences between dental professionals. Artificial bone blocks of different densities may be employed to train the tactile perception of dentists who have less experience in implant therapy. Thus, the purpose of this study was to assess whether novice dental practitioners’ abilities in judging bone densities with tactile sensation can be improved after an artificial bone blocks (Sawbones®) training protocol.
Materials and methods
Study enrollment
Twenty-five operators (postgraduate year - 1/2, PGY) at the National Taiwan University Hospital (NTUH) were voluntarily recruited to participate in this study from September 2017 to February 2018. They were board-certified dentists (average age: 26.3) without implant surgery experiences. The study protocol was approved by the NTUH institutional research ethic committee (Approval number: 201612189RIND). Participants were tested at their convenience and were assured that the performance would be recorded anonymously.
Artificial test blocks
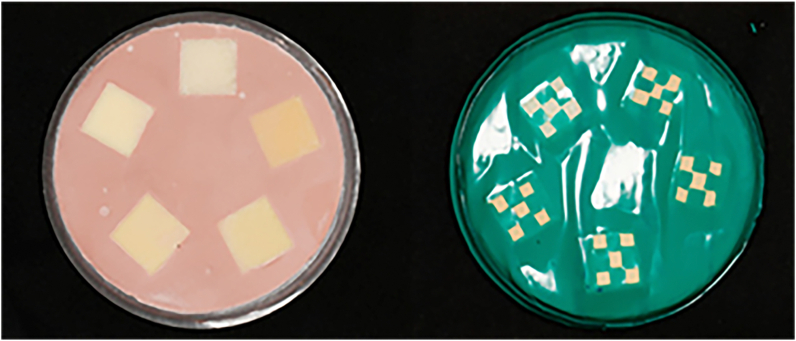
Participants were asked to evaluate the bone quality of artificial bone blocks fabricated using polyurethane rigid-typed foam blocks (Sawbones, Pacific Research Laboratory Inc., Vashon, WA, USA). Five types of standardized artificial bone blocks, 5-pcf, 10-pcf, 15-pcf, 20-pcf and 30-pcf, were fabricated to simulate bones with extremely low to medium–high cancellous densities of 0.08, 0.16, 0.24, 0.32, and 0.48 g/cm3, respectively. In addition, a 50-pcf bone block (0.8 g/cm3) was taken to represent the highest bone density for comparison during testing and training. The mean bone mineral density is 0.31 g/cm3 for the posterior maxilla and 0.55 g/cm3 for the anterior maxilla.16 The polyurethane blocks were cut into a dimension of 16 mm (length) × 16 mm (width) × 25 mm (height) and embedded in type IV die stone in a plastic container, as shown in Fig. 1. The surface was covered with PVC tape (thickness: 0.18 mm) to avoid the possibility of differentiating the bone block by surface profile.
Figure 1.
A plastic container containing five test blocks of different densities (left) covered with PVC tape (right).
Training protocol
A newly developed training protocol was designed after a pilot study which investigated the bone quality perception of clinicians with different surgical experiences.15 The training used 10-pcf and 20-pcf blocks to simulate human cancellous bone with low density and low-to-medium density, respectively.9,15 Operators performed drilling at 1500 rpm (25N-cm torque) with Surgic XT Plus machine (NSK Nakanishi Inc., Tochigi, Japan) with a new 2-mm twist drill (Nobel Biocare, Gothenburg, Sweden, 2x7-15mm) to evaluate bone quality. Each training session included a 50-pcf drilling followed by five 10-pcf and 20-pcf alternative drillings. The operators were informed of the density values of the 50-pcf block as the hardest bone available in the study. The haptic feedback of this reference test block would be VAS = 100 on the 100-mm visual analog scale. At the same time, VAS = 0 was defined as having no drilling resistance at all. During training, the operators were informed that 10-pcf and 20-pcf blocks represented the low-density bone and low-to-medium-density bone, respectively, without their exact densities being mentioned.
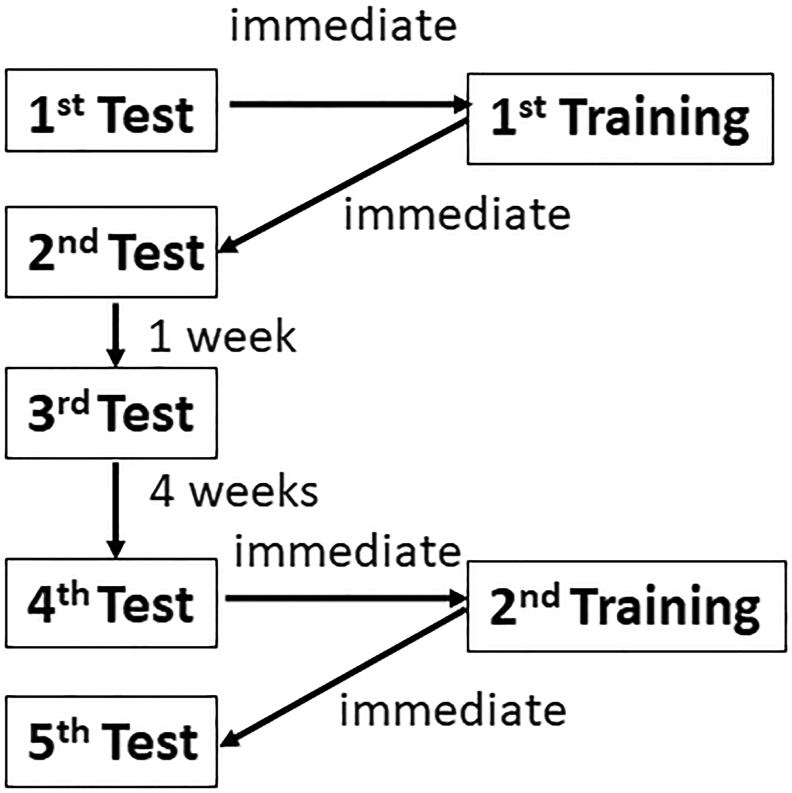
Test and training sessions
The experiments for each operator included five tests and two training sessions (Fig. 2). The first session, including the 1st and 2nd tests separated by the 1st training, was performed on the first day, and the second session, including the 3rd test, was conducted one week later. Four weeks later, the third session, including the 4th and 5th tests separated by the 2nd training, was performed. At the beginning of each test, all the operators drilled the 50-pcf reference block and had the haptic feedback as VAS = 100 on the 100-mm visual analog scale. In each of the five tests, the operator drilled the five artificial bone blocks of different densities (5-pcf, 10-pcf, 15-pcf, 20-pcf, and 30-pcf) in a randomized sequence and reported the bone quality perceived in a 100-mm VAS line after each drilling.
Figure 2.
Flow chart of experiment comprising five tests and two training sessions.
Statistical analysis
The VAS values of five test blocks in the five tests were analyzed using GLM repeated measures (IBM SPSS Statistics, Version 27, Armonk, NY, USA) to shed light on the training effect on bone density evaluation. The critical value was set at P ≤ 0.05. Linear regression was performed to correlate the VAS values reported with the exact bone density of blocks. Each operator's accuracy in sequencing the five bone densities in different test series was also analyzed using SPSS Friedman test and post-hoc Wilcoxon sign test to clarify the effect of training on individual performance.
Results
This study included 25 operators (16 females and nine males) with a mean age of 26.3 years (24.5–30.0 years). They were board-certified dentists with no implant surgery experience. Fig. 3 shows their reported drilling-perception VAS values for the 5-pcf, 10-pcf, 15-pcf, 20-pcf, and 30-pcf blocks in the five tests, indicating significant differences in mean VAS values among the test blocks of different densities. Moreover, Fig. 4 shows significant linear correlations (p < 0.0001) between VAS values and block densities in the five tests (Fig. 4). However, between different test sessions, the mean drilling-perception VAS values of same-density test blocks did not vary significantly (Fig. 3). In other words, the training sessions between Test 1 and Test 2 and between Test 4 and Test 5 had no significant influence on the reported bone quality VAS evaluation.
Figure 3.
Drilling-perception VAS values reported for 5-pcf, 10-pcf, 15-pcf, 20-pcf, 30-pcf blocks in five tests.
Figure 4.
Linear correlations (p < 0.0001) between VAS values and block densities in five tests.
Effects of training on ability in sequencing sawbones quality of different densities
The operators’ abilities in sequencing the Sawbones hardness (5-pcf < 10-pcf < 15-pcf < 20-pcf < 30-pcf) were evaluated through comparing their reported VAS values. For each operator, ten pairs of comparisons could be made from the five Sawbones in each test (Table 1). Results show no significant difference in percentages of sequencing errors among 25 operators in 10 comparisons from the five tests, implying that the training between Test 1 and Test 2 and between Test 4 and Test 5 did not have apparent effects on accurate hardness sequencing (Table 2). However, the training effect emerged when the operators were divided into superior initial performance (SIP group, N = 20) and inferior initial performance groups (IIP group, N = 5) according to their initial sequencing accuracy in 10 comparisons (SIP group: ≥ 9; IIP group: ≤8) in Test 1 (Table 2). The training significantly reduced the sequencing errors in the IIP group but not in the SIP group (p < 0.05, Table 2). The highest error rate occurred in the sequencing of 15-pcf and 20-pcf blocks, with significant difference in performance between the two groups (p < 0.05).
Table 1.
Number of errors in sequencing block hardness between two blocks.
| 5-pcf | 10-pcf | 15-pcf | 20-pcf | |
|---|---|---|---|---|
| 10-pcf | 16 (10/100, 6/25) |
|||
| 15-pcf | 0 (0/100, 0/25) |
6(4/100, 2/25) | ||
| 20-pcf | 1 (1/100, 0/25) |
5(2/100, 3/25) | 52(36/100, 16/25)∗ | |
| 30-pcf | 0 (0/100, 0/25) |
1(1/100, 0/25) | 6 (5/100, 1/25) |
9 (8/100, 1/25) |
The data in each cell contain the number of errors in sequencing block hardness between two blocks in the 5 tests of all 25 operators, and the data in brackets represent the number of errors in 100 comparisons of the SIP group and in 25 comparisons of the IIP group. (SIP group: superior initial performance group; IIP group: inferior initial performance group).
∗Significant difference in performance between SIP and IIP groups, p = 0.0134.
Table 2.
Percentage of errors in sequencing in the five tests.
| Test 1 | Test 2 | Test 3 | Test 4 | Test 5 | |
|---|---|---|---|---|---|
| All operators | 8.4% | 6.0% | 6.8% | 9.2% | 8.0% |
| SIP group | 5.5% | 4.5% | 6.5% | 8.5% | 7.5% |
| IIP group | 22.0% | 12.0% | 8.0% | 12.0% | 8.0% |
SIP group: superior initial performance group; IIP group: inferior initial performance group.
Discussion
Although bone quality has been reported to be one of the critical factors for the success of implant treatment, bone quality is a complex term and is open to interpretation.1 The evidence for the efficacy of clinical methods in assessing bone quality or density before and during endosseous dental implant placement is scarce, as these methods have not been evaluated as diagnostic or prognostic tests.17 Evaluation of bone density is of both need and importance during implant placement with regard to deciding on the depth and width of an osteotomy, undersizing the drilling sequence, submerging vs. not submerging an implant, selecting a tapered vs. non-tapered implant, countersinking, immediate loading, and healing time. Many clinicians assess bone density variations according to the tactile perception when drilling with a 2-mm twist drill. Although assessing bone quality has been deemed critical for implant therapy, to our knowledge, few studies have evaluated the reliability of surgeons’ perception in the assessment of bone quality. Our previous investigation found a considerable discrepancy between specialists and general practitioners as well as among general practitioners.15 This study tried to develop a calibration system to decrease the disparity between dental professionals. The test blocks fabricated using Sawbones of different densities were used to train the tactile perception of dentists with less experience in implant therapy.
In this study, the 25 operators were all board-certified dentists with no implant surgery experience. The present findings revealed a significant correlation between their reported perceptual VAS values and block densities. On the other hand, the results showed no significant difference in mean drilling-perception VAS values of same-density test blocks in different test sessions, implying that the training sessions had no significant influence on the bone quality VAS values assessment. Possible sequencing errors in the 10 paired block comparisons of the five tests indicated most mistakes occurring in comparison of blocks with 5-pcf (0.08 g/cm3) or 10-pcf (0.16 g/cm3) difference and very few occurring in comparison of blocks with greater density differences. The present results were consistent with previous findings, which demonstrated that hand feeling helped distinguish between D1 and D4 bones but failed to differentiate between the intermediate classes of bone quality.14
When all the operators were taken as one group, there was no significant difference in the percentage of sequencing errors between different test sessions, suggesting that the proposed training protocol did not significantly reduce sequencing errors. However, the present results did demonstrate improvement in perceptual cognition of block density among operators with poor initial performance in Test 1. In view of this finding, dentists with inferior initial performance in tactile perception should be identified to undergo the training protocol to improve their ability to classify bone quality. Further investigations with a larger sample size are needed.
The data showed significant linear correlations between the VAS values reported and the block densities in the five tests (Fig. 4). There was no significant difference between the VAS values between different tests. The data showed that the operators' VAS score given to a block was close to the true density percentage of the blocks with 50-pcf block as a reference before each test. With the 50-pcf block as the reference (VAS = 100), the reported VAS scores in the five tests for the 5-pcf blocks (density = 10% of 50-pcf) were ranged from 11.0 ± 2.3 to 17.4 ± 2.0, and for the 30-pcf blocks (density = 60% of 50-pcf block) from 69.1 ± 3.9 to 77.6 ± 2.2. The results suggested that a reference block drilling, before implant surgery, may help inexperienced operators identify bone quality of implant sites. Further investigations are needed to clarify this suggestion.
This pilot study presented an inexpensive training protocol that is easy to administer. Drilling performance results of a small number of residents suggest possible effect of the proposed training protocol in improving bone quality classification ability among inexperienced dentists with poor initial performance.
Declaration of competing interest
The authors have no conflict of interest relevant to this article.
Acknowledgements
This study was financially supported by National Taiwan University Hospital, NTUH-107-32.
References
- 1.van Steenberghe D., Jacobs R., Desnyder M., Maffei G., Quirynen M. The relative impact of local and endogenous patient-related factors on implant failure up to the abutment stage. Clin Oral Implants Res. 2002;13:617–622. doi: 10.1034/j.1600-0501.2002.130607.x. [DOI] [PubMed] [Google Scholar]
- 2.Engquist B., Bergendal T., Kallus T., Linden U. A retrospective multicenter evaluation of osseointegrated implants supporting overdentures. Int J Oral Maxillofac Implants. 1988;3:129–134. [PubMed] [Google Scholar]
- 3.Jaffin R.A., Berman C.L. The excessive loss of Brånemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2–4. doi: 10.1902/jop.1991.62.1.2. [DOI] [PubMed] [Google Scholar]
- 4.Marković A., Calvo-Guirado J.L., Lazić Z., et al. Evaluation of primary stability of self-tapping and non-self-tapping dental implants. A 12-week clinical study. Clin Implant Dent Relat Res. 2013;15:341–349. doi: 10.1111/j.1708-8208.2011.00415.x. [DOI] [PubMed] [Google Scholar]
- 5.O'Sullivan D., Sennerby L., Jagger D., Meredith N. A comparison of two methods of enhancing implant primary stability. Clin Implant Dent Relat Res. 2004;6:48–57. doi: 10.1111/j.1708-8208.2004.tb00027.x. [DOI] [PubMed] [Google Scholar]
- 6.Romanos G.E., Basha-Hijazi A., Gupta B., Ren Y.F., Malmstrom H. Role of clinician's experience and implant design on implant stability. An ex vivo study in artificial soft bones. Clin Implant Dent Relat Res. 2014;16:166–171. doi: 10.1111/j.1708-8208.2012.00470.x. [DOI] [PubMed] [Google Scholar]
- 7.Toyoshima T., Wagner W., Klein M.O., Stender E., Wieland M., Al-Nawas B. Primary stability of hybrid self-tapping implant compared to a cylindrical non-self-tapping implant with respect to drilling protocols in an ex vivo model. Clin Implant Dent Relat Res. 2011;13:71–78. doi: 10.1111/j.1708-8208.2009.00185.x. [DOI] [PubMed] [Google Scholar]
- 8.Turkyilmaz I., Aksoy U., McGlumphy E.A. Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: a clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Relat Res. 2008;10:231–237. doi: 10.1111/j.1708-8208.2008.00084.x. [DOI] [PubMed] [Google Scholar]
- 9.Wang T.M., Lee M.S., Wang J.S., Lin L.D. The effect of implant design and bone quality on insertion torque, resonance frequency analysis, and insertion energy during implant placement in low or low- to medium-density bone. Int J Prosthodont (IJP) 2015;28:40–47. doi: 10.11607/ijp.4063. [DOI] [PubMed] [Google Scholar]
- 10.Herrero-Climent M., Lemos B.F., Herrero-Climent F., et al. Influence of implant design and under-preparation of the implant site on implant primary stability. An in vitro study. Int J Environ Res Publ Health. 2020;17:4436. doi: 10.3390/ijerph17124436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pérez-Pevida E., Cherro R., Camps-Font O., Piqué N. Effects of drilling protocol and bone density on the stability of implants according to different macrogeometries of the implant used: results of an in vitro study. Int J Oral Maxillofac Implants. 2020;35:955–964. doi: 10.11607/jomi.8176. [DOI] [PubMed] [Google Scholar]
- 12.Lindh C., Oliveira G.H.C., Leles C.R., Freire M.C.M., Ribeiro-Rotta R.F. Bone quality assessment in routine dental implant treatment among Brazilian and Swedish specialists. Clin Oral Implants Res. 2014;25:1004–1009. doi: 10.1111/clr.12221. [DOI] [PubMed] [Google Scholar]
- 13.Lekholm U., Zarb G.A. In: Tissue-integrated prostheses: osseointegration in clinical dentistry. Brånemark P.-I., Zarb G.A., Albrektsson T., editors. Quintessence; Chicago: 1985. Patient selection and preparation; pp. 199–209. [Google Scholar]
- 14.Trisi P., Rao W. Bone classification: clinical-histomorphometric comparison. Clin Oral Implants Res. 1999;10:1–7. doi: 10.1034/j.1600-0501.1999.100101.x. [DOI] [PubMed] [Google Scholar]
- 15.Wang T.M. National Taiwan University Graduate Institute of Clinical Dentistry School of Dentistry; Taiwan: 2014. Technical innovation for improving the reliability, stability and survival rates of dental implant: from engineering informatics to experiments. PhD dissertation. [Google Scholar]
- 16.Devlin H., Horner K., Ledgerton D. A comparison of maxillary and mandibular bone mineral densities. J Prosthet Dent. 1998;79:323–327. doi: 10.1016/s0022-3913(98)70245-8. [DOI] [PubMed] [Google Scholar]
- 17.Ribeiro-Rotta R.F., Lindh C., Rohlin M. Efficacy of clinical methods to assess jawbone tissue prior to and during endosseous dental implant placement: a systematic literature review. Int J Oral Maxillofac Implants. 2007;22:289–300. [PubMed] [Google Scholar]