This cohort study assesses the association between perioperative hyperglycemia and surgical complications in a population of surgical patients with and without diabetes.
Key Points
Question
What is the association between perioperative hyperglycemia and surgical complications in all patients and what are potential consequences of not identifying perioperative hyperglycemia?
Findings
In this cohort study of 969 patients with diabetes and 4899 patients without diabetes, adjusted odds of experiencing any type of postoperative complication were consistently higher for patients without diabetes than for those with diabetes across a range of elevated blood glucose levels.
Meaning
Because neither diabetes misclassification nor underuse of insulin was responsible for perioperative hyperglycemia, the possibility of a biological mechanism should be considered.
Abstract
Importance
Surgical complications associated with perioperative hyperglycemia are conventionally associated with diabetes, but, paradoxically, prior cohort studies have found that patients without diabetes have greater risk of complications at similar levels of hyperglycemia compared with patients with diabetes.
Objective
To describe the association between perioperative hyperglycemia and surgical complications in a population of surgical patients without diabetes receiving routine blood glucose testing and insulin administration and to evaluate the potential correlation of perioperative hyperglycemia.
Design, Setting, and Participants
This retrospective cohort study of National Surgical Quality Improvement Program–defined complications after operation took place at a single academic medical center hospital from January 2013 to October 2016. Consecutive patients undergoing general, vascular, and gynecologic operations who were expected to have at least a 48-hour admission were included. Hyperglycemia was defined as blood glucose level of 140 mg/dL or higher within 24 hours after surgery. Multivariate regression was used to assess the association of hyperglycemia and complications, stratified by hyperglycemia severity and adjusted for diabetes status. Analysis began in February 2022.
Exposures
Routine blood glucose testing and insulin administration.
Main Outcomes and Measures
The main outcomes are odds of experiencing perioperative hyperglycemia and postoperative complication, comparing patients with and without diabetes.
Results
A total of 7634 patients (mean [SD] age, 53.5 [15.1] years; 6664 patients without diabetes [83.3%] and 970 patients with diabetes [17.7%]) underwent general (6204 [81.3%]), vascular (208 [2.7%]), and gynecologic (1222 [16%]) operations. Of these, 5868 (77%) had blood glucose testing (4899 individuals without diabetes [73.5%] and 969 [99.9%] with diabetes). Hyperglycemia occurred in 882 patients with diabetes (91%) and 2484 patients without diabetes (50.7%). Of those with blood glucose level more than 180 mg/dL, 1388 (72.7%) received insulin (658 patients with diabetes who had hyperglycemia [91%] and 680 patients without diabetes who had hyperglycemia [61%]). Adjusted odds of experiencing a complication were 83% greater for patients without vs with diabetes at blood glucose level of 140 to 179 mg/dL (odds ratio, 1.83 [95% CI, 0.93-3.6]), 49% greater for blood glucose level of 180 to 249 mg/dL (odds ratio, 1.49 [95% CI, 1.06-2.11]), and 88% greater for blood glucose level more than 250 mg/dL (odds ratio, 1.88 [95% CI, 1.11-3.17]). A similar trend was observed for serious complications. Insulin may mitigate the association of hyperglycemia and complications in patients without diabetes.
Conclusions and Relevance
In this study, with near universal blood glucose testing and frequent insulin use, patients without diabetes paradoxically had worse outcomes than patients with diabetes at similar levels of hyperglycemia. Insulin may mitigate this effect and broader use may improve outcomes.
Introduction
Perioperative hyperglycemia is common and known to substantially increase the risk of serious postoperative complications. When defined as blood glucose level of more than 140 mg/dL (to convert to millimoles per liter, multiply by 0.0555), perioperative hyperglycemia has been shown to occur in nearly 40% of surgical patients1 and is associated with complications including surgical site infection,2,3 myocardial infarction,4 and mortality.5 Because the harmful effects of hyperglycemia are commonly associated with a known diagnosis of diabetes, detection and treatment of perioperative hyperglycemia among the 15% of surgical patients with diabetes is an established quality metric and has been associated with decreased risk of adverse postoperative outcomes.6,7
However, perioperative hyperglycemia is also common among surgical patients without diabetes.1,2,8,9 Paradoxically, several retrospective studies have demonstrated that at similar levels of hyperglycemia, patients without diabetes face as much as a 50% greater risk of complications compared with their counterparts with diabetes.1,10,11 Although patients with diabetes are more likely overall to experience both hyperglycemia in the perioperative setting and postoperative complications, hyperglycemia appears to be more strongly associated with postoperative complications among patients without diabetes. The mechanisms underlying this paradoxical finding—that when patients without diabetes who have hyperglycemia face a greater risk of experiencing complications than do patients with diabetes—are not well understood; however, they are particularly relevant because patients without diabetes compose the majority of surgical patients.
There are multiple possible explanations for paradoxical poor outcomes among patients without diabetes who have hyperglycemia compared with patients with diabetes. Given that many adults in the US with diabetes are unaware of their diagnosis12 and testing for diabetes status is not a routine aspect of preoperative medical evaluation, it is possible that misclassification of diabetes status may have introduced bias to prior studies. Second, because testing for and therefore treatment of perioperative hyperglycemia are not routine among surgical patients without diabetes, it is possible that undertreatment of hyperglycemia among such patients increases the risk of complications because patients without diabetes are comparatively naive to episodes of hyperglycemia. Third, patients without diabetes who have poor outcomes may exhibit a unique physiologic response to surgical stress that results in levels of hyperglycemia similar to those of patients with known diabetes.
Given evidence suggesting an association between perioperative hyperglycemia and postoperative complications, a perioperative glycemic management program was developed and implemented at the University of Washington Medical Center. The program includes near universal blood glucose level testing and routine treatment of hyperglycemia for all surgical patients regardless of prior diabetes status. We aimed to assess the hyperglycemia paradox in a well-characterized prospective cohort defined by participation in this quality improvement initiative.
Methods
This was a prospective cohort study, including purposive sampling of consecutive patients undergoing general, vascular, and gynecologic operations with a planned admission at the University of Washington Medical Center between January 2013 and October 2016. Those who did not undergo glucose testing (23.1% of the cohort) were excluded from the analysis. Perioperative blood glucose and insulin administration data were obtained from the electronic medical record. Demographic information and diabetes status were obtained from the medical history, and postoperative complications were abstracted in accordance with participation in the American College of Surgeons National Surgical Quality Improvement Program.13 Data on race and ethnicity were not available. This study was exempted for review by the institutional review board of the University of Washington Medical Center.
Data collection was initiated in tandem with an institutionwide perioperative glycemic monitoring and management protocol. Regardless of diabetes status, patients had glucose testing on the day of surgery before the procedure was initiated; this was repeated intraoperatively at 60- to 90-minute intervals as needed and then in the morning on postoperative days 1 and 2 (or more often, based on clinical management). Hyperglycemia was defined as blood glucose level of 140 mg/dL or higher within 24 hours after surgery. An insulin algorithm was developed in collaboration with endocrinologists, the hospital medicine team, pharmacy, and anesthesia team. An insulin infusion was initiated for individuals with blood glucose levels greater than 140 mg/dL and was started in the preoperative, operative, and postanesthesia recovery units or intensive care unit (greater than 180 mg/dL was used as the threshold for treatment in the postoperative period on the floor), regardless of diabetes status, and continued after surgery. For this evaluation, hyperglycemia was defined as glucose levels of 140 mg/dL or higher and further characterized as mild (140-179 mg/dL), moderate (180-249 mg/dL), or severe (≥250 mg/dL). Perioperative hyperglycemia included any blood glucose level of 140 mg/dL or higher after initiating the procedure within the first 24 hours. Insulin use was determined by the prescription of any mode of insulin administration within 4 hours after a blood glucose level higher than 180 mg/dL. All patients received insulin under the guidelines of the algorithm until their blood glucose levels were within target range and they no longer needed insulin or transitioned to oral diet and medication. Preoperative insulin did not count as administration perioperatively.
A composite measure of any National Surgical Quality Improvement Program–defined postoperative complication within 30 days was used as the primary outcome (including superficial, deep, and organ space surgical site infection; wound disruption; pneumonia; unplanned intubation; deep vein thrombosis; pulmonary embolism; need for mechanical ventilation >48 hours; progressive kidney insufficiency; acute kidney failure; urinary tract infection; stroke; cardiac arrest; myocardial infarction; need for return to the operating room; and/or systemic sepsis). Serious complications included death or a subset of the above complications that included major morbidity events.
Demographic and clinical characteristics were compared among patients by level of hyperglycemia and diabetes status. Characteristics were summarized using frequency distributions for categorical variables and means and standard deviations for continuous variables. The percentage of patients experiencing any complications or serious complications was calculated at each level of hyperglycemia for diabetes and no diabetes groups with respective 95% CIs. Using multivariate regression, adjusted for potential confounders and stratified by level of hyperglycemia, the odds of experiencing any complication or a serious complication were then compared between patients with diabetes vs no diabetes. Variables accounted for in the regression analysis included age, baseline comorbidities, American Society of Anesthesiologists physical status class, body mass index, surgical specialty, and year of operation. Finally, among patients without diabetes who had hyperglycemia only, the odds of experiencing any complication or a serious complication were compared among those who did and did not receive insulin, adjusting for confounders listed above. Analysis began in February 2022 and was performed using R version 4.0.5 (R Foundation).
Results
The cohort consisted of 5868 patients who underwent general (4896 [83.4%]), vascular (152 [2.6%]), or gynecologic operations (820 [14%]) (Table). Among this cohort, 4899 patients (83%) did not have diabetes and 969 patients (17%) had diabetes. Of patients without diabetes, 23.8% (n = 1165) had a preoperative glycated hemoglobin A1c (HbA1c) test within 90 days. Of these, 78.7% (n = 917) were in the no-diabetes range (153 [13.1%] were in intermediate range [HbA1c, 6%-6.5%] and 95 [8.2%] had HbA1c levels greater than 6.5%). Hyperglycemia (blood glucose level, ≥140 mg/dL) occurred in 57% (n = 3366) of the cohort overall (2484 patients without diabetes [51%] and 882 patients with diabetes [91%]).
Table. Characteristics of Surgical Patients and Surgical Type by Hyperglycemia and Diabetes Status.
| Characteristic | Blood glucose level, No. (%) | Total (N = 5868) | |||
|---|---|---|---|---|---|
| Diabetes (n = 969) | No diabetes (n = 4899) | ||||
| <140 mg/dL (n = 87) | ≥140 mg/dL (n = 882) | <140 mg/dL (n = 2415) | ≥140 mg/dL (n = 2484) | ||
| Age, y | |||||
| 18-30 | 5 (5.75) | 15 (1.7) | 345 (14.3) | 123 (5) | 488 (8.3) |
| 31-40 | 9 (10.3) | 61 (6.9) | 399 (16.5) | 271 (10.9) | 780 (12.6) |
| 41-50 | 17 (19.5) | 140 (15.9) | 475 (19.7) | 382 (15.4) | 1014 (17.3) |
| 51-60 | 18 (20.7) | 259 (29.4) | 537 (22.2) | 649 (26.1) | 1463 (24.9) |
| 61-70 | 26 (29.9) | 271 (30.8) | 423 (17.5) | 616 (24.8) | 1336 (22.8) |
| 71-80 | 11 (12.6) | 113 (12.8) | 188 (7.8) | 369 (14.9) | 681 (11.6) |
| >80 | 1 (1.25) | 23 (2.6) | 48 (2) | 74 (3) | 146 (2.5) |
| Mean (SD) | 55.6 (14) | 58.3 (12.3) | 49.7 (16.1) | 56.6 (14.5) | 54 (15.3) |
| Median (IQR) | 58 (45-65) | 59 (51-67) | 50 (37-62) | 58 (47-67) | 55 (43-66) |
| Comorbidities | |||||
| Current smoker | 8 (9.2) | 88 (10) | 224 (9.28) | 237 (9.54) | 557 (9.49) |
| Obesity | 55 (63.2) | 603 (68.4) | 790 (32.7) | 1043 (42) | 2491 (42.5) |
| Cancer | 1 (1.2) | 30 (3.4) | 80 (3.3) | 254 (10.2) | 365 (6.2) |
| Hypertension | 59 (67.8) | 605 (68.6) | 617 (25.5) | 900 (36.2) | 2181 (37.2) |
| Surgery type | |||||
| General surgery | 81 (93.1) | 737 (83.6) | 1967 (81.4) | 2111 (85) | 4896 (83.4) |
| Vascular | 1 (1.2) | 30 (3.4) | 68 (2.9) | 53 (2.1) | 152 (2.6) |
| Gynecology | 5 (5.8) | 115 (13.0) | 380 (15.7) | 320 (12.9) | 820 (14) |
SI conversion factor: To convert blood glucose level to millimoles per liter, multiply by 0.0555.
In the cohort, 732 (12.4%) overall experienced any complication (594 patients without diabetes [12%; 95% CI, 11.1-12.9] and 138 patients with diabetes [14%; 95% CI, 11.8-16.1]). Among all patients, 513 (9.6%) experienced a serious complication (423 patients without diabetes [8.6%; 95% CI, 7.8-9.3] and 90 patients with diabetes [9.2%; 95% CI, 7.3-11]). At each level of hyperglycemia, the proportion of patients without diabetes who experienced any complication (Figure 1) was higher than that among patients with diabetes (blood glucose level, 140-179 mg/dL: 182 [13.3%; 95% CI, 11.4-15.1] vs 11 [6.8%; 95% CI, 2.9-10.6]; blood glucose level, 180-249 mg/dL: 211 [22%; 95% CI, 19.3-24.6] vs 69 [14%; 95% CI, 10.9-17]; and blood glucose level, >250 mg/dL: 67 [38%; 95% CI, 30.8-45.1] vs 56 [24%; 95% CI, 17.6-28.3]). Patients without diabetes also experienced higher rates of serious complications at similar levels of hyperglycemia (blood glucose level, 140-179 mg/dL: 127 [9%; 95% CI, 7.4-10.5] vs 7 [4%; 95% CI, 1-7.02]; blood glucose level, 180-249 mg/dL: 174 [18%; 95% CI, 15.5-20.4] vs 46 [9%; 95% CI, 6.4-11.5]; blood glucose level, ≥250 mg/dL: 51 [29%; 95% CI, 22.2-35.7] vs 36 [15%; 95% CI, 10.4-19.5]). After adjustment for confounders, this increased risk of complications persisted for the 3 levels of hyperglycemia for any complications (odds ratio [OR], 1.83 [95% CI, 0.93-3.6]; OR, 1.49 [95% CI, 1.06-2.11]; and OR, 1.88 [95% CI, 1.11-3.17], respectively) and for serious complications (OR, 1.57 [95% CI, 0.67-3.67]; OR, 1.87 [95% CI, 1.25-2.79]; and OR, 2 [95% CI, 1.1-3.6], respectively), although for the lowest hyperglycemia level the confidence intervals include 1 (Figure 2).
Figure 1. Percentage of National Surgical Quality Improvement Program (NSQIP) Events by Diabetes Status and Level of Hyperglycemia (N = 5686).
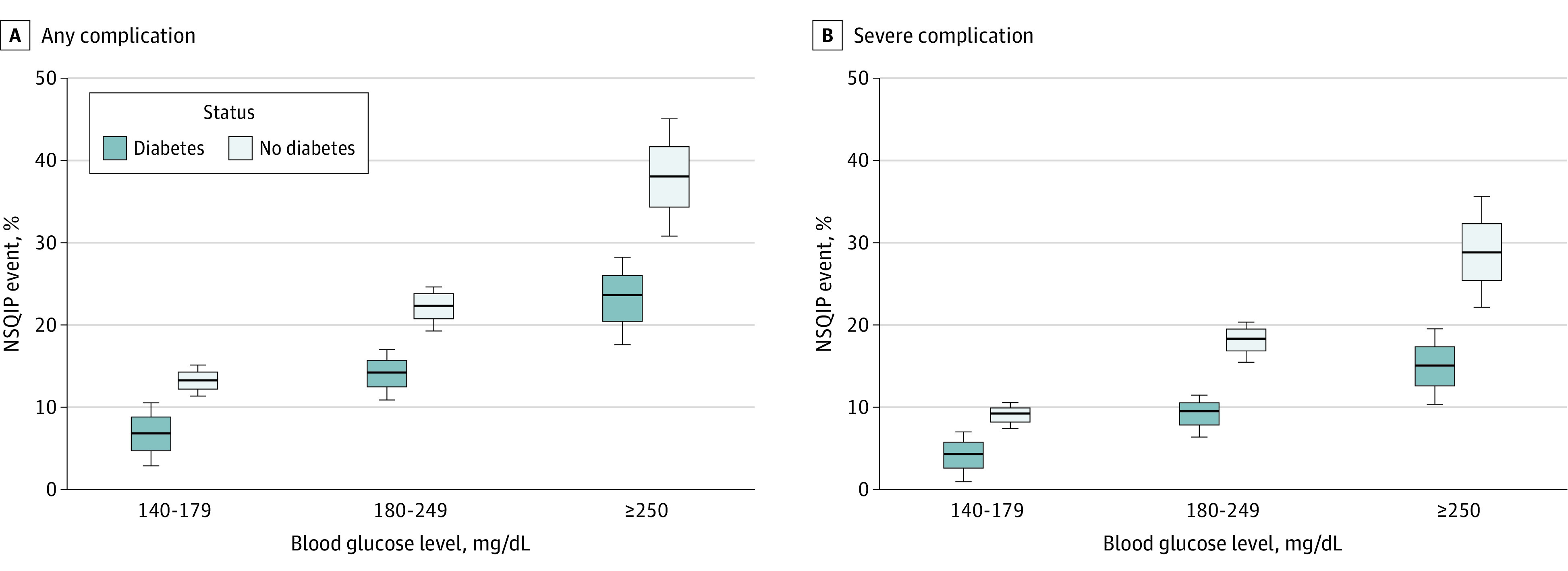
Figure 2. Adjusted Odds Ratio (OR) of American College of Surgeons National Surgical Quality Improvement Program (NSQIP) Event Among Patients Without Diabetes.
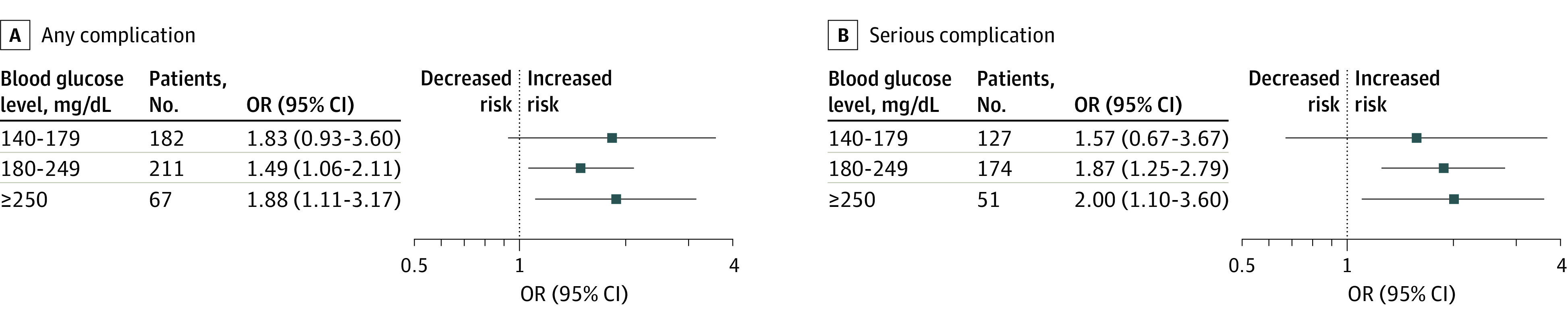
Reference is the OR of an event among patients with diabetes. Model adjusted for age, American Society of Anesthesiologists physical status class, body mass index group, comorbidities (smoking status, dyspnea, chronic obstructive pulmonary disease, congestive heart failure, hypertension, dialysis, cancer, chronic steroid use, weight loss, and bleeding disorder), need for preoperative transfusion, acute preoperative kidney failure, surgical specialty, and year of operation.
Within the cohort, 31% (n = 1840) experienced moderate or severe hyperglycemia (blood glucose level, >179 mg/dL), of which 73% (n = 1338) received insulin in response. Among the 23% (n = 1119) of patients without diabetes with moderate or severe hyperglycemia, 61% (n = 680) received insulin in response to hyperglycemia per institutional protocol; among the 74% (n = 721) of patients with diabetes with moderate or severe hyperglycemia, 91% (n = 658) received insulin.
Lower proportions of complications and serious complications were observed when comparing patients without diabetes who received insulin in response to hyperglycemia with those who did not and had hyperglycemia. The rate of any complications among patients without diabetes who received insulin compared with those who did not was similar (156 of 680 [22.9%] vs 122 of 439 [27.8%], respectively). Among patients without diabetes with moderate or severe hyperglycemia (>180 mg/dL), the adjusted odds of a complication or severe complication based on the receipt of insulin were 0.79 (95% CI, 0.58-1.07) and 0.79 (95%, 0.57-11), respectively.
Discussion
In a study of patients undergoing a variety of major surgical procedures, we found hyperglycemia within 24 hours to be common, occurring in nearly 6 of 10 patients overall and in almost half of patients without diabetes. At both moderate and severe levels of hyperglycemia, patients without diabetes faced a higher risk of experiencing a postoperative complication compared with their counterparts with diabetes. Insulin treatment appeared to mitigate the risk of complications among patients without diabetes with hyperglycemia, and underuse or inadequate use of insulin may still explain some aspect of the hyperglycemia paradox, but this assessment was limited by the number of observed events. These findings suggest that the hyperglycemia paradox of greater hyperglycemia-related postoperative complications in patients without diabetes is not the result of blood glucose testing in selected cohorts or underuse of insulin. Further inquiry into the underlying mechanism of the hyperglycemia paradox for patients without diabetes is needed.
Although the harmful risks of hyperglycemia are typically associated with diabetes, our findings suggest that perioperative hyperglycemia may be more deleterious in patients without diabetes because those with hyperglycemia experience a higher risk of complication compared with patients with diabetes experiencing similar levels of hyperglycemia.
This paradox of hyperglycemia and surgical outcomes in patients without diabetes has been demonstrated in previous retrospective cohort studies,1,10,11 showing that patients without diabetes with hyperglycemia have a substantial increase in odds of mortality and serious complications, such as cardiovascular events and a need for reoperation, compared with patients with diabetes. In a statewide cohort of surgical patients, Kotagal et al10 demonstrated a dose-response association in the risk of a composite outcome of adverse events, with worsening hyperglycemia for patients without diabetes. Similarly, Frisch et al1 showed an increasing risk of mortality among patients without diabetes with increasing blood glucose levels. Notably, this association was not seen in patients with diabetes with hyperglycemia in either study.
Prior studies were limited by the fact that only a minority of patients without diabetes underwent blood glucose testing in the perioperative period. This selective testing for hyperglycemia and resulting missing data, especially among patients without diabetes, left open the question of unmeasured confounding by indication. Our study addresses this limitation, as most surgical patients at our institution underwent blood glucose testing in the perioperative period. Our study coincided with the adoption of a comprehensive perioperative glycemic management strategy at the University of Washington Medical Center, which includes testing of all patients regardless of preoperative diabetes status. Widespread glucose testing (77%) and a substantially sized subcohort of patients without diabetes with HbA1c testing (24%) confirms those included were not simply misdiagnosed as not having diabetes and that confounding by indication was not the explanation for the hyperglycemia paradox.
However, we did not demonstrate an association between receipt of insulin in response to hyperglycemia and lower risk of complications among patients without diabetes. We measured treatment of hyperglycemia but not achievement of normoglycemia or glycemic control. It is possible that because most patients, including those without diabetes, received insulin in response to hyperglycemia, we were not able to discern a difference between patients with and without diabetes. Prior studies have shown that correction of hyperglycemia is associated with improved outcomes among hospitalized patients and those undergoing cardiac surgery independent of diabetes status.7,14
The fact that our health care system has committed to a protocol of universal blood glucose testing and routine insulin administration, yet 30% of patients with hyperglycemia still did not receive insulin, suggests continued reluctance to treat hyperglycemia, especially among patients without diabetes who are likely insulin naive.15 This appears to be an improvement, as Kotagal et al10 reported that 40% of patients without diabetes with moderate hyperglycemia (blood glucose level, 180-249 mg/dL) and approximately half with severe hyperglycemia received insulin in 2015. Jones et al16 showed that at low and moderate levels of hyperglycemia (blood glucose level, <240 mg/dL), patients without diabetes were less likely to receive insulin compared with patients with diabetes. They found that only at blood glucose levels of 250 mg/dL or greater was insulin administration equal between patients with and without diabetes. Although the risks associated with very strict glucose control, especially in the setting of critical illness, are significant,17 there is ample evidence showing that comprehensive glycemic management protocols are safe and effective and associated with very low rates of hypoglycemia.18
Perioperative hyperglycemia among patients without diabetes and the resulting paradox of complications is not well understood. Prior to this study, the possible explanations for the hyperglycemia paradox included selective glucose testing and misclassification of patients as not having diabetes when they had undiagnosed and thereby unmanaged diabetes. It is also possible that some proportion of the patients without diabetes with hyperglycemia in our cohort were incorrectly classified by diabetes status. The subgroup with HbA1c testing did show that a small proportion had a level more than 6.5, and a limitation of this study is that we did not have additional measures to classify these patients as having diabetes or prediabetes. Some estimates suggest that 1 of 4 individuals in the US with diabetes is unaware of their diagnosis.19 Preoperative screening for diabetes by fasting glucose or HbA1c levels is not routine. Among the patients in our cohort who underwent preoperative (within 30 days) HbA1c testing, 78.7% were in the normal range. Similarly, Wang et al20 report that undiagnosed and therefore untreated diabetes is likely not driving the disparity in complications between patients with and without diabetes. In their cohort of 6700 surgical patients initially classified as not having diabetes, only 8% overall and 15% of patients with hyperglycemia (blood glucose level, >100 mg/dL) went on to receive a diagnosis of diabetes by HbA1c testing in the year following surgery. Furthermore, in that study the odds of infectious complications increased significantly with higher glucose levels in the patients who were eventually classified as true patients without diabetes but not in those who were in the prediabetes range at the time of surgery and who went on to be diagnosed with diabetes.
It is not clear if hyperglycemia itself is a primary pathologic process that leads to complications or if it serves as a marker of increased underlying stress and inflammation. The latter might suggest that when patients without diabetes who normally have euglycemia (blood glucose level, <140 mg/dL) develop levels of hyperglycemia similar to patients with diabetes, this reflects an even greater underlying stress response and puts them at an increased risk of adverse outcomes. However, work by Thompson et al21 disputes this idea, as they showed that stress response, measured by C-reactive protein and interleukin 6, was similar among vascular surgery patients with and without diabetes who have hyperglycemia. This is an area in need of further exploration. This study was limited in that it did not gather evidence of physiologic stress.
Limitations
The present study has limitations. First, although a majority of patients at our institution underwent glucose testing, some were still missing a glucose value and were excluded from this analysis (0.01% of patients with diabetes and 26.5% of patients without diabetes). Some of the adjusted analyses involved a small number of patients and events (eg, blood glucose level >250 mg/dL in patients without diabetes with serious complications), leading to the possibility of a type II error when considering adjustment for potential confounders. Perioperative steroid use was not accounted for, and this can play a role in hyperglycemia. Some complications (eg, reintubation soon after extubation and prolonged ventilation) may have occurred prior to hyperglycemia was detected or insulin administration, and this may represent misspecification of the outcome.
Finally, because the National Surgical Quality Improvement Program defines diabetes status by preoperative insulin or oral glycemic use, it is possible that some degree of misclassification of diabetes status occurred within our cohort.
Conclusions
In a cohort with high levels of glucose testing and insulin use among patients with and without diabetes, patients without diabetes paradoxically had worse outcomes compared with patients with diabetes at similar levels of hyperglycemia. This is not likely explained by selective testing of blood glucose among patients without diabetes or misclassification of diabetes status, but may be associated with underuse/inadequate use of insulin or other biological mechanisms. These findings suggest the importance of continued perioperative glycemic monitoring, especially in those patients without a known history of diabetes, and highlights areas for further inquiry.
References
- 1.Frisch A, Chandra P, Smiley D, et al. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care. 2010;33(8):1783-1788. doi: 10.2337/dc10-0304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Latham R, Lancaster AD, Covington JF, Pirolo JS, Thomas CS Jr. The association of diabetes and glucose control with surgical-site infections among cardiothoracic surgery patients. Infect Control Hosp Epidemiol. 2001;22(10):607-612. doi: 10.1086/501830 [DOI] [PubMed] [Google Scholar]
- 3.Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585-591. doi: 10.1097/SLA.0b013e31818990d1 [DOI] [PubMed] [Google Scholar]
- 4.McAlister FA, Man J, Bistritz L, Amad H, Tandon P. Diabetes and coronary artery bypass surgery: an examination of perioperative glycemic control and outcomes. Diabetes Care. 2003;26(5):1518-1524. doi: 10.2337/diacare.26.5.1518 [DOI] [PubMed] [Google Scholar]
- 5.Schmeltz LR, DeSantis AJ, Thiyagarajan V, et al. Reduction of surgical mortality and morbidity in diabetic patients undergoing cardiac surgery with a combined intravenous and subcutaneous insulin glucose management strategy. Diabetes Care. 2007;30(4):823-828. doi: 10.2337/dc06-2184 [DOI] [PubMed] [Google Scholar]
- 6.Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg. 1999;67(2):352-360. doi: 10.1016/S0003-4975(99)00014-4 [DOI] [PubMed] [Google Scholar]
- 7.Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125(5):1007-1021. doi: 10.1067/mtc.2003.181 [DOI] [PubMed] [Google Scholar]
- 8.Mohan S, Kaoutzanis C, Welch KB, et al. Postoperative hyperglycemia and adverse outcomes in patients undergoing colorectal surgery: results from the Michigan surgical quality collaborative database. Int J Colorectal Dis. 2015;30(11):1515-1523. doi: 10.1007/s00384-015-2322-7 [DOI] [PubMed] [Google Scholar]
- 9.Kiran RP, Turina M, Hammel J, Fazio V. The clinical significance of an elevated postoperative glucose value in nondiabetic patients after colorectal surgery: evidence for the need for tight glucose control? Ann Surg. 2013;258(4):599-604. doi: 10.1097/SLA.0b013e3182a501e3 [DOI] [PubMed] [Google Scholar]
- 10.Kotagal M, Symons RG, Hirsch IB, et al. ; SCOAP-CERTAIN Collaborative . Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2015;261(1):97-103. doi: 10.1097/SLA.0000000000000688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg. 2013;257(1):8-14. doi: 10.1097/SLA.0b013e31827b6bbc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Diabetes Association . Diagnosis and classification of diabetes mellitus. Diabetes Care. 2006;29(suppl 1):S43-S48. [PubMed] [Google Scholar]
- 13.Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6-16. doi: 10.1016/j.jamcollsurg.2009.09.031 [DOI] [PubMed] [Google Scholar]
- 14.Giakoumidakis K, Eltheni R, Patelarou E, et al. Effects of intensive glycemic control on outcomes of cardiac surgery. Heart Lung. 2013;42(2):146-151. doi: 10.1016/j.hrtlng.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 15.Cook CB, Castro JC, Schmidt RE, et al. Diabetes care in hospitalized noncritically ill patients: more evidence for clinical inertia and negative therapeutic momentum. J Hosp Med. 2007;2(4):203-211. doi: 10.1002/jhm.188 [DOI] [PubMed] [Google Scholar]
- 16.Jones CE, Graham LA, Morris MS, et al. Association between preoperative hemoglobin A1c levels, postoperative hyperglycemia, and readmissions following gastrointestinal surgery. JAMA Surg. 2017;152(11):1031-1038. doi: 10.1001/jamasurg.2017.2350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Finfer S, Chittock DR, Su SY, et al. ; NICE-SUGAR Study Investigators . Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283-1297. doi: 10.1056/NEJMoa0810625 [DOI] [PubMed] [Google Scholar]
- 18.de Vries FE, Gans SL, Solomkin JS, et al. Meta-analysis of lower perioperative blood glucose target levels for reduction of surgical-site infection. Br J Surg. 2017;104(2):e95-e105. doi: 10.1002/bjs.10424 [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention . National Diabetes Statistics Report, 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf [Google Scholar]
- 20.Wang R, Panizales MT, Hudson MS, Rogers SO, Schnipper JL. Preoperative glucose as a screening tool in patients without diabetes. J Surg Res. 2014;186(1):371-378. doi: 10.1016/j.jss.2013.09.014 [DOI] [PubMed] [Google Scholar]
- 21.Thompson R, Khor S, Thornblade LW, Flum DR, Sobel M. The paradox of hyperglycemia and surgical outcomes in patients with and without diabetes. Surg Infect (Larchmt). 2019;20(4):338-339. doi: 10.1089/sur.2018.270 [DOI] [PMC free article] [PubMed] [Google Scholar]


