This cohort study investigates the association between daily sitting time and mortality and cardiovascular disease in countries of different economic levels.
Key Points
Question
Is daily sitting time associated with mortality and cardiovascular disease (CVD) in countries of different economic levels?
Findings
In this cohort study including 105 677 participants from 21 countries, higher sitting time was associated with an increased risk of all-cause mortality and major CVD, and the association was more pronounced in low-income and lower-middle–income countries. Meeting the World Health Organization recommendations for physical activity could effectively attenuate the risk of high sitting time.
Meaning
Reducing sedentary time along with increasing physical activity may be an important strategy for easing the global burden of premature deaths and CVD.
Abstract
Importance
High amounts of sitting time are associated with increased risks of cardiovascular disease (CVD) and mortality in high-income countries, but it is unknown whether risks also increase in low- and middle-income countries.
Objective
To investigate the association of sitting time with mortality and major CVD in countries at different economic levels using data from the Prospective Urban Rural Epidemiology study.
Design, Setting, and Participants
This population-based cohort study included participants aged 35 to 70 years recruited from January 1, 2003, and followed up until August 31, 2021, in 21 high-income, middle-income, and low-income countries with a median follow-up of 11.1 years.
Exposures
Daily sitting time measured using the International Physical Activity Questionnaire.
Main Outcomes and Measures
The composite of all-cause mortality and major CVD (defined as cardiovascular death, myocardial infarction, stroke, or heart failure).
Results
Of 105 677 participants, 61 925 (58.6%) were women, and the mean (SD) age was 50.4 (9.6) years. During a median follow-up of 11.1 (IQR, 8.6-12.2) years, 6233 deaths and 5696 major cardiovascular events (2349 myocardial infarctions, 2966 strokes, 671 heart failure, and 1792 cardiovascular deaths) were documented. Compared with the reference group (<4 hours per day of sitting), higher sitting time (≥8 hours per day) was associated with an increased risk of the composite outcome (hazard ratio [HR], 1.19; 95% CI, 1.11-1.28; P for trend < .001), all-cause mortality (HR, 1.20; 95% CI, 1.10-1.31; P for trend < .001), and major CVD (HR, 1.21; 95% CI, 1.10-1.34; P for trend < .001). When stratified by country income levels, the association of sitting time with the composite outcome was stronger in low-income and lower-middle–income countries (≥8 hours per day: HR, 1.29; 95% CI, 1.16-1.44) compared with high-income and upper-middle–income countries (HR, 1.08; 95% CI, 0.98-1.19; P for interaction = .02). Compared with those who reported sitting time less than 4 hours per day and high physical activity level, participants who sat for 8 or more hours per day experienced a 17% to 50% higher associated risk of the composite outcome across physical activity levels; and the risk was attenuated along with increased physical activity levels.
Conclusions and Relevance
High amounts of sitting time were associated with increased risk of all-cause mortality and CVD in economically diverse settings, especially in low-income and lower-middle–income countries. Reducing sedentary time along with increasing physical activity might be an important strategy for easing the global burden of premature deaths and CVD.
Introduction
Increased sitting time has become common in modern society owing to the popularization of electronic products, an increase in sedentary occupations, and changing patterns of transportation. Serial analyses reported total sitting time has substantially increased by nearly 1 hour per day among adults over the past decade in the US.1,2 The recent World Health Organization (WHO) 2020 global physical activity guideline now recommends limiting sedentary time and engaging in high levels of physical activity to reduce the detrimental effects of sitting time.3
Thus far, current evidence has been almost exclusively in high-income countries (HICs)4,5 and China.6,7,8 Previous studies suggested that the contextual patterns in which sedentary behavior occurs might vary substantially by socioeconomic status and social class.9,10 The health effects of sedentary behavior are not well documented for populations from low- and middle-income countries (LICs and MICs), where the patterns of activity are much different from HICs and the prevalence of a sedentary lifestyle has increased dramatically along with rapid urbanization.11,12,13 It is in these same countries where most of the global CVD burden exists.14 Therefore, the associations between sitting time and clinical outcomes based on studies predominately conducted in HICs cannot be directly extrapolated into populations residing in LICs and MICs.
In the present analysis, we aimed to determine the associations of self-reported sitting time with all-cause mortality and major CVD in countries at varying income levels using data from the Prospective Urban Rural Epidemiology (PURE) study. In addition, we also evaluated the joint association of sitting time and physical activity with clinical outcomes.
Methods
Study Design and Participants
The details about study design and participant enrollment have been previously published (eAppendix in the Supplement).15 The PURE study is a large-scale, prospective, cohort study recruiting participants aged 35 to 70 years across regions of Africa, Asia, Europe, the Middle East, and North and South America. This analysis includes information from 21 countries in which participants had completed at least 1 cycle of follow-up visits (4 HICs: Canada, Saudi Arabia, Sweden, and United Arab Emirates; 7 upper-middle–income countries [UMICs]: Argentina, Brazil, Chile, Malaysia, Poland, South Africa, Turkey; 5 lower-middle–income countries [LMICs]: China, Colombia, Iran, Palestine, the Philippines; and 5 LICs: Bangladesh, India, Pakistan, Tanzania, and Zimbabwe). Countries were categorized based on the 2006 World Bank classification at the time of inclusion. In participating countries, urban and rural communities were selected based on prespecified criteria to achieve a geographically and socioeconomically diverse population. Households and individuals aged 35 to 70 years within each community were approached using sampling strategies based on both representativeness and feasibility of long-term follow-up. We reported information by geographical regions (Africa, South Asia, Southeast Asia/China, Middle East, North America and Europe, South America) but not by race and ethnicity because there are more than 30 categories of ethnicity (collected by self-reported) within this multinational study. The baseline characteristics and mortality profiles were comparable with national statistics in participating countries.16 All participants provided written informed consent. This prospective cohort study was coordinated by the Population Health Research Institute (Hamilton, Canada), and local ethics approval was obtained by all collaborating sites. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Exposure
Information on sitting time and total physical activity was collected using the long-form International Physical Activity Questionnaire (IPAQ), which has been validated in multiple countries17,18,19,20 and is widely used in the international population-level surveillance studies21 and previous large-scale etiological studies.22,23,24 The total number of hours spent sitting per day was assessed using 2 questions: “During the last 7 days, how much time did you usually spend sitting on a usual (1) weekday and (2) weekend day?” Daily sitting time was calculated as a mean average sitting time per day ([5 × weekday +2 × weekend hours] / 7). According to recent literature,24,25 we categorized daily sitting time into the following groups: less than 4 hours per day, 4 to 6 hours per day, 6 to 8 hours per day, and 8 hours or more per day, with the lowest group used as the reference. Physical activity was reported in minutes per day of moderate to vigorous activity (MVPA) in 10-minute bouts as metabolic equivalents (METs) × minutes of MVPA and categorized as low (<600 METs), moderate (600-3000 METs), and high (>3000 METs) levels, corresponding to less than 150 minutes per week, 150 to 750 minutes per week, and more than 750 minutes per week of MVPA.26 Other covariates included age, sex, urban/rural residence, education, household wealth index (a validated index of household assets),27 marital status, occupational class, INTERHEART risk score (a composite index measuring cardiovascular risk burdens),28 smoking status, alcohol use, diet quality (PURE diet score),29 body mass index (BMI; calculated as weight in kilograms divided by height in meters squared), hypertension, diabetes, baseline chronic conditions, physical impairments, and symptoms of depression.30 Details of covariates are provided in the eAppendix in the Supplement.
Outcomes
The primary outcome was the composite of all-cause mortality and major cardiovascular events (cardiovascular mortality, nonfatal myocardial infarction, stroke, or heart failure). Secondary outcomes included individual components of the composite outcome. Details about outcome definitions and adjudication process are described in the eAppendix in the Supplement. For this analysis, we included all adjudicated events until August 31, 2021.
Statistical Analysis
Baseline characteristics were described for the overall population and stratified by different sitting groups. The association between daily sitting time and clinical outcomes was assessed using Cox proportional hazards frailty models with a random intercept of center-level clustering. The proportional hazard assumptions were assessed with log-log plots, and no variables violated the assumption. Covariates were identified a priori based on previous literature and proposed mechanisms underlying the associations between sitting time and clinical outcomes (eAppendix in the Supplement).31,32 Model 1 included age, sex, urban/rural residence, and a center random intercept. Model 2 additionally included country income levels, education, household wealth index, smoking status, physical activity, depression, physical impairments, and baseline chronic conditions. Restricted cubic splines were calculated using 3 knots at the 10th, 50th, and 90th percentiles to assess the dose-response association. Adjusted population attributable fractions (PAFs) were calculated to estimate the potential effect of risk factor reduction from a public health perspective.33 To study the consistency of associations between sitting time and the composite outcome, we conducted subgroup analyses by geographical regions, country income levels, urban/rural location, age, sex, education, household wealth index, BMI, hypertension, diabetes, and INTERHEART risk score. We also used tests of interaction to compare the associations between HICs and UMICs vs LMICs and LICs, and we conducted stratified and joint analyses to assess the association between sitting time and physical activity. In addition, isotemporal substitution models were built to assess the effect of replacing sitting time with physical activities.34 Further details of the statistical analyses are provided in the eAppendix in the Supplement. P values were 2-sided, and statistical significance was set at P < .05. All statistical analyses were conducted using SAS software, version 9.4 (SAS Institute).
Results
Between January 1, 2003, and December 4, 2016, 167 082 participants aged 35 to 70 years were enrolled in the first 2 phases of the PURE study. Information on vital status was available among 162 326 participants (97.2%), of which 117 170 had complete and plausible information on sitting time and physical activity. After excluding participants having preexisting CVD, cancer, or HIV (n = 11 493), a total of 105 677 participants were included in this analysis (eFigure 1 in the Supplement). The mean (SD) age was 50.4 (9.6) years; there were a total of 61 925 women (58.6%) and 43 752 men (41.4%).
The median sitting time at baseline was 4.0 (IQR, 2.6-6.0) hours per day, ranging from 2.6 hours per day in Poland and Chile to 7.3 hours per day in Saudi Arabia (eTable 1 in the Supplement). Participants with higher sitting time were more likely to be from urban areas and UMICs and HICs (HICs: ≥8 hours per day, 3220 of 11 965 [26.9%] vs <4 hours per day, 4428 of 48 091 [9.2%]; UMICs: ≥8 hours per day, 4365 of 11 965 [36.5%] vs <4 hours per day, 13890 of 48 091 [28.9%]). They had higher education (trade college/university: ≥8 hours per day, 3341 of 11 965 [27.9%] vs <4 hours per day, 8246 of 48 091 [17.2%]), higher INTERHEART risk scores (mean [SD] score: ≥8 hours per day, 11.7 [6.1] vs <4 hours per day, 10.0 [5.6]), and lower levels of physical activity (low [<600 MET]: ≥8 hours per day, 3591 of 11 965 [30.0%] vs <4 hours per day, of 7207 of 48 091 [15.0%]), and they were also more likely to have diabetes (≥8 hours per day, 1597 of 11 965 [13.3%] vs <4 hours per day, 4081 of 48 091 [8.5%]), depression (≥8 hours per day, 1660 of 11 965 [13.9%] vs <4 hours per day, 4691 of 48 091 [9.8%]), physical impairments (≥8 hours per day, 2298 of 11 965 [19.2%] vs <4 hours per day, 8072 of 48 091 [16.8%]), and chronic diseases at baseline (≥8 hours per day, 1249 of 11 965 [10.4%] vs <4 hours per day, 3196 of 48 091 [6.7%]) (Table 1).
Table 1. Baseline Characteristics of the Total Population and Stratified by Groups of Daily Sitting Time.
| Variables | No. (%) | ||||
|---|---|---|---|---|---|
| Total (N = 105 677) | <4 h (n = 48 091) | 4-6 h (n = 30 037) | 6-8 h (n = 15 584) | ≥8 h (n = 11 965) | |
| Daily sitting time, median (IQR), h/d | 4.0 (2.6-6.0) | 2.4 (1.7-3.0) | 4.8 (4.3-5.1) | 6.6 (6.0-7.0) | 9.4 (8.3-11.0) |
| Urban residence | 59 125 (55.9) | 23 763 (49.4) | 18 204 (60.6) | 9620 (61.7) | 7538 (63.0) |
| Age, mean (SD), y | 50.4 (9.6) | 50.2 (9.5) | 50.6 (9.6) | 50.5 (9.7) | 50.8 (9.5) |
| Women | 61 925 (58.6) | 28 692 (59.7) | 17 647 (58.8) | 9123 (58.5) | 6463 (54.0) |
| Men | 43 752 (41.4) | 19 399 (40.3) | 12 390 (41.2) | 6461 (41.5) | 5502 (46.0) |
| Country income levela | |||||
| HIC | 14 511 (13.7) | 4428 (9.2) | 3989 (13.3) | 2874 (18.4) | 3220 (26.9) |
| UMIC | 30 907 (29.2) | 13 890 (28.9) | 8310 (27.7) | 4342 (27.9) | 4365 (36.5) |
| LMIC | 49 926 (47.2) | 24 275 (50.5) | 14 531 (48.4) | 7190 (46.1) | 3930 (32.8) |
| LIC | 10 333 (9.8) | 5498 (11.4) | 3207 (10.7) | 1178 (7.6) | 450 (3.8) |
| Geographical regionb | |||||
| Africa | 3386 (3.2) | 2156 (4.5) | 803 (2.7) | 235 (1.5) | 192 (1.6) |
| South Asia | 8395 (7.9) | 4274 (8.9) | 2789 (9.3) | 1020 (6.5) | 312 (2.6) |
| Southeast Asia/China | 48 379 (45.8) | 24 962 (51.9) | 13 139 (43.7) | 6151 (39.5) | 4127 (34.5) |
| Middle East | 9818 (9.3) | 2151 (4.5) | 3127 (10.4) | 2494 (16.0) | 2046 (17.1) |
| North America and Europe | 16 056 (15.2) | 5311 (11.0) | 4584 (15.3) | 3136 (20.1) | 3025 (25.3) |
| South America | 19 643 (18.6) | 9237 (19.2) | 5595 (18.6) | 2548 (16.4) | 2263 (18.9) |
| Education | |||||
| None, primary, or unknown | 41 193 (39.0) | 19 757 (41.2) | 10 947 (36.5) | 5889 (37.8) | 4600 (38.5) |
| Secondary/high/higher secondary | 41 124 (39.0) | 20 006 (41.7) | 11 690 (39.0) | 5412 (34.8) | 4016 (33.6) |
| Trade or college/university | 23 206 (22.0) | 8246 (17.2) | 7358 (24.5) | 4261 (27.4) | 3341 (27.9) |
| Global wealth index, tertilec | |||||
| Low | 24 272 (23.2) | 14 129 (29.7) | 5743 (19.3) | 2611 (16.9) | 1789 (15.0) |
| Middle | 38 481 (36.8) | 18 109 (38.1) | 11 521 (38.7) | 5415 (35.0) | 3436 (28.8) |
| High | 41 937 (40.1) | 15 291 (32.2) | 12 504 (42.0) | 7446 (48.1) | 6696 (56.2) |
| Married, common law, or living with partner | 90 405 (85.7) | 41 519 (86.5) | 25 747 (85.9) | 13 231 (85.0) | 9908 (82.9) |
| Occupation | |||||
| Professional/managers | 18 439 (17.7) | 6664 (14.0) | 5810 (19.7) | 3339 (21.9) | 2626 (22.4) |
| Skilled workers | 33 610 (32.3) | 14 761 (31.0) | 10 211 (34.7) | 4895 (32.1) | 3743 (32.0) |
| Unskilled workers | 22 699 (21.8) | 13 291 (27.9) | 5204 (17.7) | 2464 (16.1) | 1740 (14.9) |
| Homemaker | 29 288 (28.2) | 12 889 (27.1) | 8235 (28.0) | 4564 (29.9) | 3600 (30.7) |
| INTERHEART score, mean (SD)d | 10.5 (5.8) | 10.0 (5.6) | 10.6 (5.8) | 11.0 (5.8) | 11.7 (6.1) |
| Smoking | |||||
| Former | 12 912 (12.3) | 5165 (10.8) | 3692 (12.4) | 2055 (13.2) | 2000 (16.8) |
| Current | 20 376 (19.4) | 9572 (20.1) | 5770 (19.3) | 2866 (18.5) | 2168 (18.2) |
| Never | 71 726 (68.3) | 32 953 (69.1) | 20 413 (68.3) | 10 601 (68.3) | 7759 (65.1) |
| Alcohol use | |||||
| Former | 4445 (4.3) | 1914 (4.0) | 1211 (4.1) | 650 (4.2) | 670 (5.7) |
| Current | 29 434 (28.3) | 12 828 (27.1) | 8680 (29.3) | 4348 (28.3) | 3578 (30.5) |
| Never | 70 150 (67.4) | 32 565 (68.8) | 19 714 (66.6) | 10 388 (67.5) | 7483 (63.8) |
| Physical activity, median (IQR), MET × min/wk | 2607.0 (956.0-5880.0) | 3006.0 (1125.0-6930.0) | 2796.0 (1128.0-5916.0) | 2119.5 (792.0-4473.0) | 1533.0 (414.0-3780.0) |
| Low (<600) | 18 469 (17.5) | 7207 (15.0) | 4471 (14.9) | 3200 (20.5) | 3591 (30.0) |
| Middle (600-3000) | 39 129 (37.0) | 16 775 (34.9) | 11 246 (37.4) | 6465 (41.5) | 4643 (38.8) |
| High (>3000) | 48 079 (45.5) | 24 109 (50.1) | 14 320 (47.7) | 5919 (38.0) | 3731 (31.2) |
| BMI, mean (SD)e | 26.3 (5.2) | 25.8 (4.9) | 26.3 (5.0) | 26.9 (5.4) | 27.7 (5.8) |
| PURE diet score, mean (SD)f | 3.7 (1.7) | 3.6 (1.7) | 3.7 (1.7) | 3.8 (1.7) | 4.0 (1.7) |
| Hypertensiong | 40 778 (40.7) | 18 777 (41.1) | 11 580 (40.3) | 5981 (39.8) | 4440 (41.3) |
| Diabetesh | 10 219 (9.7) | 4081 (8.5) | 2841 (9.5) | 1700 (10.9) | 1597 (13.3) |
| Depressioni | 11 268 (10.7) | 4691 (9.8) | 3065 (10.2) | 1852 (11.9) | 1660 (13.9) |
| Having ≥2 physical impairmentsj | 17 486 (16.6) | 8072 (16.8) | 4524 (15.1) | 2592 (16.7) | 2298 (19.2) |
| Baseline chronic diseasesk | 8129 (7.7) | 3196 (6.7) | 2318 (7.7) | 1366 (8.8) | 1249 (10.4) |
Abbreviations: BMI, body mass index; HIC, high-income country; LIC, low-income country; LMIC, lower-middle–income country; METs, metabolic equivalents; PURE, Prospective Urban Rural Epidemiology; UMIC, upper-middle–income country.
Defined according to 2006 World Bank classification at time of study entry.
North America and Europe includes Canada, Poland, Sweden, and Turkey. South America includes Argentina, Brazil, Chile, and Colombia. Middle East includes Iran, occupied Palestinian territory, Saudi Arabia, and United Arab Emirates. South Asia includes India and Pakistan. Southeast Asia includes Malaysia and the Philippines. Africa includes South Africa, Tanzania, and Zimbabwe.
Household wealth was defined by an index based on ownership of assets and housing characteristics and grouped into country-stratified tertiles.
The INTERHEART Risk Score is a validated score for quantifying risk factor burden that includes data on age, sex, status with respect to smoking, diabetes, high blood pressure, and family history of heart disease, waist-to-hip ratio, psychosocial factors, diet, and physical activity. Scores range from 0 to 48, with higher scores indicating greater risk factor burden.
Calculated as weight in kilograms divided by height in meters squared.
The PURE diet score was a composite diet score based on eight food types associated with a lower risk of cardiovascular disease or mortality in PURE: fruits, vegetables, legumes, nuts, fish, dairy, unprocessed red meat, and poultry; with each classified into high consumption (1 point) or low consumption (0 points) based on the median amount consumed in PURE (in grams per day).
Defined as blood pressure of 140/90 mm Hg or greater, self-reported hypertension, or use of antihypertensive medications.
Defined as fasting blood glucose level of 7 mmol/L or greater, self-reported diabetes, or taking hypoglycemic agents regularly.
Defined as a score of at least 4 on a 7-symptom depression score using an adapted version of the Short-Form Composite International Diagnostic Interview for major depressive disorders.
Having 0, 1, or 2 or more difficulties in grasping, walking, bending, reading, seeing people, speaking, hearing, and using walking aids.
Defined as having been diagnosed with hepatitis (or jaundice), chronic obstructive pulmonary disease, asthma, tuberculosis, malaria, or chagas.
During the median follow-up of 11.1 (IQR, 8.6-12.2) years, we recorded 6233 deaths and 5696 major cardiovascular events (2349 myocardial infarctions, 2966 strokes, 671 heart failure, and 1792 cardiovascular deaths) (eTable 2 in the Supplement). Table 2 shows the hazard ratios (HRs) of daily sitting time with clinical outcomes. In the multivariable-adjusted models, the risk of the composite outcome associated with sitting time was significantly increased above 6 hours per day (HR, 1.13; 95% CI, 1.06-1.21 for 6-8 hours per day; HR, 1.19; 95% CI, 1.11-1.28 for ≥8 hours per day; P for trend < .001). For individual outcomes, sitting more than 8 hours per day was associated with an HR of 1.20 (95% CI, 1.10-1.31) for all-cause mortality, 1.29 (95% CI, 1.10-1.51) for cardiovascular mortality, 1.17 (95% CI, 1.05-1.29) for noncardiovascular mortality, 1.21 (95% CI, 1.10-1.34) for major CVD, 1.20 (95% CI, 1.04-1.38) for myocardial infarction, 1.20 (95% CI, 1.03-1.40) for stroke, and 1.49 (95% CI, 1.16-1.90) for heart failure. The associations after categorizing participants into country-specific quintiles were also consistent (eTable 3 in the Supplement). In sensitivity analysis, we further adjusted for potential mediators (hypertension, diabetes, and BMI) or diet quality and found the HRs were not materially changed (eTable 4 in the Supplement). No appreciable differences were observed when excluding events within the first 5 years or participants with poor health conditions at baseline (eTable 5 in the Supplement). To address the specificity of the association, we selected injury as a negative control outcome and found a negative association for sitting time, which suggested that there was minimal potential for residual confounding and bias from other sources (eTable 6 in the Supplement). The E-value analysis showed that only a confounder with a risk factor of 1.62 to 2.34 above and beyond the measured confounders could alter the observed association, suggesting that weak unmeasured confounding could not explain the observed HRs (eTable 7 in the Supplement). Furthermore, the results were consistent for sitting time on weekdays or weekend days (eTable 8 in the Supplement). Multiple imputation for missing data on sitting time also yielded similar results (eTable 9 in the Supplement).
Table 2. Associations Between Daily Sitting Time and Clinical Outcomes.
| Variable | Sitting time, HR (95% CI) | P value for trend | |||
|---|---|---|---|---|---|
| <4 h/d (n = 48 091) | 4-6 h/d (n = 30 037) | 6-8 h/d (n = 15 584) | ≥8 h/d (n = 11 965) | ||
| Composite outcome | |||||
| Incidence ratea | 9.74 (9.47-10.02) | 8.93 (8.59-9.28) | 9.80 (9.31-10.32) | 10.25 (9.67-10.87) | NA |
| Model 1b | 1 [Reference] | 0.98 (0.93-1.03) | 1.13 (1.06-1.20) | 1.20 (1.12-1.29) | <.001 |
| Model 2c | 1 [Reference] | 1.00 (0.95-1.05) | 1.13 (1.06-1.21) | 1.19 (1.11-1.28) | <.001 |
| All-cause mortality | |||||
| Incidence rate | 5.87 (5.66-6.09) | 5.51 (5.25-5.78) | 6.13 (5.75-6.55) | 7.02 (6.55-7.53) | NA |
| Model 1 | 1 [Reference] | 0.99 (0.93-1.05) | 1.13 (1.04-1.22) | 1.22 (1.12-1.33) | <.001 |
| Model 2 | 1 [Reference] | 1.01 (0.95-1.08) | 1.12 (1.03-1.21) | 1.20 (1.10-1.31) | <.001 |
| CVD mortality | |||||
| Incidence rate | 1.66 (1.55-1.78) | 1.53 (1.39-1.67) | 1.91 (1.70-2.14) | 2.10 (1.85-2.39) | NA |
| Model 1 | 1 [Reference] | 0.95 (0.85-1.07) | 1.17 (1.01-1.35) | 1.33 (1.14-1.56) | <.001 |
| Model 2 | 1 [Reference] | 0.97 (0.86-1.10) | 1.14 (0.98-1.32) | 1.29 (1.10-1.51) | .002 |
| Non-CVD mortality | |||||
| Incidence rate | 4.21 (4.04-4.40) | 3.98 (3.76-4.21) | 4.23 (3.91-4.57) | 4.92 (4.52-5.35) | NA |
| Model 1 | 1 [Reference] | 1.00 (0.93-1.08) | 1.10 (1.01-1.21) | 1.18 (1.06-1.30) | <.001 |
| Model 2 | 1 [Reference] | 1.03 (0.95-1.11) | 1.11 (1.01-1.22) | 1.17 (1.05-1.29) | .001 |
| Major CVD | |||||
| Incidence rate | 5.69 (5.48-5.90) | 5.08 (4.82-5.34) | 5.65 (5.28-6.05) | 5.58 (5.15-6.04) | NA |
| Model 1 | 1 [Reference] | 0.96 (0.90-1.03) | 1.13 (1.04-1.23) | 1.22 (1.11-1.34) | <.001 |
| Model 2 | 1 [Reference] | 0.97 (0.91-1.04) | 1.13 (1.04-1.23) | 1.21 (1.10-1.34) | <.001 |
| Myocardial infarction | |||||
| Incidence rate | 2.10 (1.98-2.23) | 2.04 (1.88-2.21) | 2.61 (2.37-2.89) | 2.96 (2.66-3.30) | NA |
| Model 1 | 1 [Reference] | 0.94 (0.84-1.04) | 1.18 (1.04-1.34) | 1.22 (1.07-1.40) | <.001 |
| Model 2 | 1 [Reference] | 0.95 (0.86-1.06) | 1.19 (1.05-1.35) | 1.20 (1.04-1.38) | .002 |
| Stroke | |||||
| Incidence rate | 3.21 (3.05-3.37) | 2.65 (2.47-2.85) | 2.65 (2.40-2.93) | 2.02 (1.77-2.30) | NA |
| Model 1 | 1 [Reference] | 0.96 (0.88-1.05) | 1.08 (0.96-1.21) | 1.17 (1.01-1.36) | .05 |
| Model 2 | 1 [Reference] | 0.97 (0.89-1.06) | 1.08 (0.96-1.22) | 1.20 (1.03-1.40) | .03 |
| Heart failure | |||||
| Incidence rate | 0.59 (0.53-0.66) | 0.59 (0.51-0.68) | 0.66 (0.54-0.80) | 0.97 (0.81-1.18) | NA |
| Model 1 | 1 [Reference] | 1.10 (0.90-1.33) | 1.25 (0.98-1.59) | 1.56 (1.23-1.99) | <.001 |
| Model 2 | 1 [Reference] | 1.10 (0.90-1.33) | 1.22 (0.96-1.56) | 1.49 (1.16-1.90) | .002 |
Abbreviations: CVD, cardiovascular disease; NA, not applicable.
Incidence rate and its 95% CI was per 1000 person-years.
Minimally adjusted models were adjusted for age, sex, urban and rural location, and a random intercept for clustering of centers.
Multivariable adjusted models were additionally adjusted for country income level, education level, household wealth index, smoking status, physical activity, depression, baseline chronic diseases, and physical impairments.
The dose-response analysis shows the risk of the composite outcome increased linearly, and the results were also robust after excluding events within the first 5 years and participants with poor health conditions at baseline (eFigures 2 and 3 in the Supplement). For per-hour increase in sitting time, the HR for the composite outcome was 1.03 (95% CI, 1.02-1.04). When analyzed as a meta-analysis of country-specific estimates, the overall association between per-hour increase in sitting time and clinical outcomes remained statistically significant (HR, 1.02; 95% CI, 1.01-1.03) for the composite outcome (eFigure 4 in the Supplement).
When stratified by country income level, there was a significant interaction between country income level and daily sitting time for the composite outcome and all-cause mortality. The association of sitting time with the composite outcome was stronger in LICs and LMICs (≥8 hours per day: HR, 1.29; 95% CI, 1.16-1.44) compared with HICs and UMICs (HR, 1.08; 95% CI, 0.98-1.19; P for interaction = .02) (Figure 1). For the composite outcome, we found a positive significant association in LMICs and LICs, but not in HICs and UMICs (eTable 10 in the Supplement). When stratified by geographical region, we found that higher levels of sitting time were associated with the composite outcome in all regions except for North America and Europe (≥8 hours per day: HR, 1.06; 95% CI, 0.89-1.26), with the largest association observed in South Asia (≥8 hours per day: HR, 1.82; 95% CI, 1.41-2.34; P for interaction = .004). The association was more pronounced among participants with BMI less than 25 (≥8 hours per day: HR, 1.25; 95% CI, 1.11-1.41 for those with BMI < 25; HR, 1.12; 95% CI, 1.02-1.23 for those with BMI ≥ 25; P for interaction < .001), probable depression (≥8 hours per day: HR, 1.37; 95% CI, 1.12-1.67 for those with depression; HR, 1.16; 95% CI, 1.07-1.25 for those without depression; P for interaction = .046), and 2 or more physical impairments (≥8 hours per day: HR, 1.48; 95% CI, 1.29-1.69 for those with ≥2 physical impairments; HR, 1.09; 95% CI, 1.00-1.19 for those with 0-1 physical impairments; P for interaction = .001).
Figure 1. Comparison of Daily Sitting Time With the Composite of All-Cause Mortality and Major Cardiovascular Diseases Stratified by Country Income Level.
A, Composite outcome, B, all-cause mortality, and C, major cardiovascular disease (CVD) adjusted for age, sex, urban or rural residence, country income level, education level, household wealth index, smoking status, physical activity, depression, baseline chronic diseases, physical impairments, and a random intercept for clustering of centers. HIC indicates high-income country; HR, hazard ratio; LMIC, lower-middle–income country; LIC, low-income country; UMIC, upper-middle–income country.
When stratified by physical activity levels, we found directionally consistent results for the composite outcome across different physical activity stratums (low physical activity: HR, 1.23; 95% CI, 1.07-1.40 for ≥8 hours per day of sitting time; P for trend = .004; moderate physical activity: HR, 1.09; 95% CI, 0.96-1.23; P for trend = .04; high physical activity: HR, 1.20; 95% CI, 1.06-1.36; P for trend = .002) and no statistical evidence of heterogeneity (P for interaction = 0.58) (Figure 2A; eTable 11 in the Supplement). The results for mortality and major CVD showed slight disparities across different stratums, but higher sitting time was consistently associated with increased risk among the least physically active participants. In the joint analysis, the combination of higher sitting time and lower physical activity was associated with an increased risk of mortality and CVD (Figure 2B). Among those sitting for 8 hours per day or more, the hazard of the composite outcome was increased by between 17% and 50% across physical activity levels. However, participants who reported sitting 8 hours per day or more but had moderate to high physical activity had a similar risk (HR, 1.17; 95% CI, 1.04-1.32 for high physical activity; HR, 1.19; 95% CI, 1.06-1.34 for moderate physical activity) compared with those who sat the least (<4 hours per day) and also had low physical activity (HR, 1.16; 95% CI, 1.06-1.26). The results were similar when participants were cross-classified using a more detailed categorization for physical activity or stratified by country income levels (eFigures 5 and 6 in the Supplement).
Figure 2. Joint and Stratified Associations of Daily Sitting Time and Physical Activity With Clinical Outcomes.
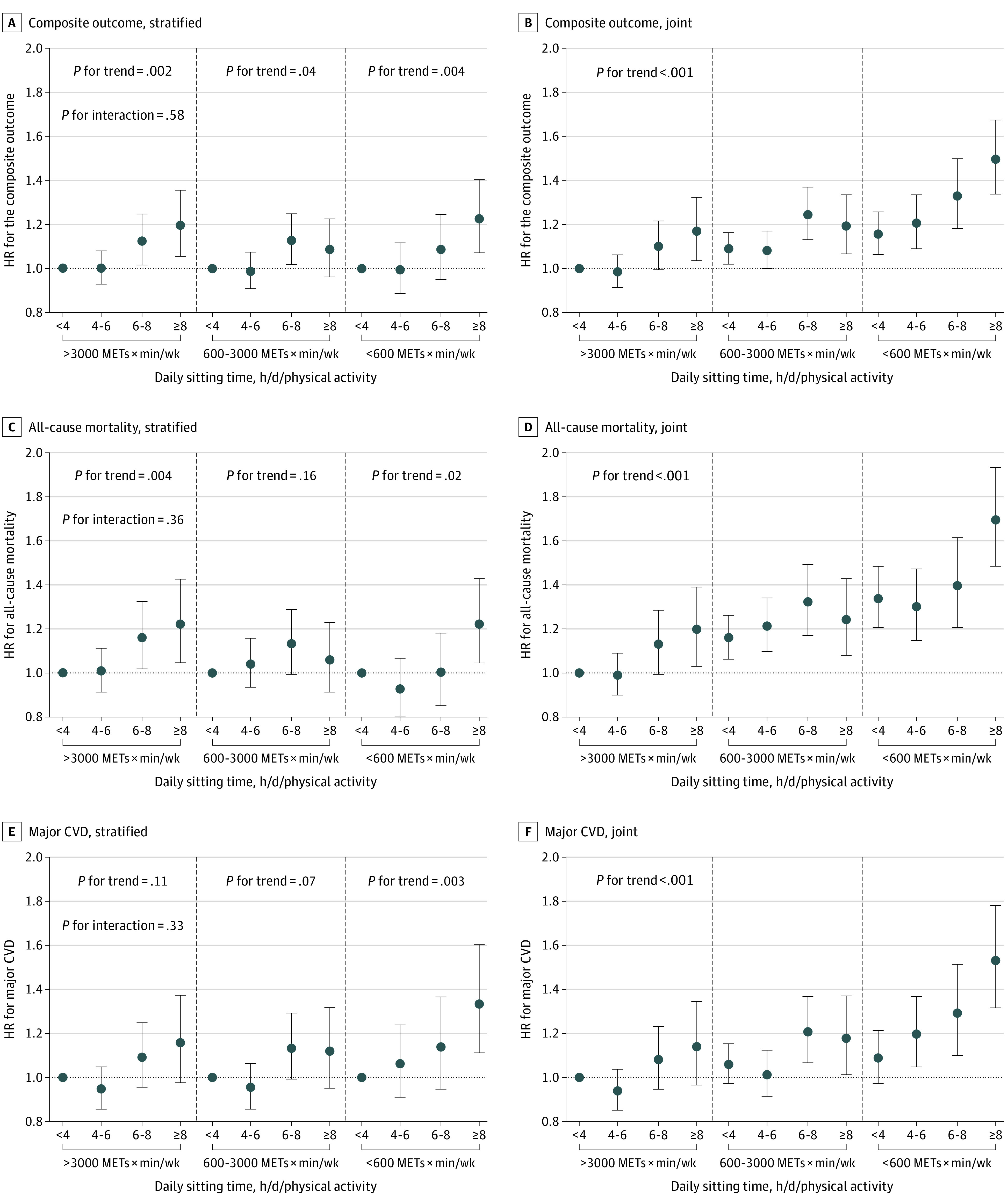
The categorization of physical activity corresponds to <150, 150-750, and >750 minutes per week of moderate-to-vigorous intensity of physical activity. A and B, Stratified and joint association for composite outcome, respectively; C and D, stratified and joint association for all-cause mortality, respectively; and E and F, stratified and joint association for major cardiovascular disease (CVD), respectively. Adjusted for age, sex, urban or rural residence, country income level, education level, household wealth index, smoking status, depression, baseline chronic diseases, physical impairments, and a random intercept for clustering of centers. Data are listed in eTable 5 in the Supplement. MET indicates metabolic equivalent; HR, hazard ratio.
Figure 3 shows the isotemporal replacement (per 30 minutes) effect of sitting with physical activities stratified by sitting levels. Among sedentary participants (sitting ≥4 hours per day), replacing 30 minutes of sitting time with total physical activity was associated with a 2% lower risk of the composite outcome (HR, 0.98; 95% CI, 0.97-0.99), with the effect being consistent across physical activity of different intensity. Substituting sitting time with recreational physical activity was associated with a more pronounced effect (HR, 0.95; 95% CI, 0.92-0.97) compared with that for nonrecreational physical activity (HR, 0.98; 95% CI, 0.97-0.99).
Figure 3. Estimated Risk for All-Cause Mortality and Major Cardiovascular Diseases (CVDs) With Substitution of 30 Minutes per Day of Daily Sitting Time With an Equal Amount of Time Spent in Physical Activity Among Participants With Low and High Levels of Sitting Time.
Adjusted for age, sex, urban or rural residence, country income level, education level, household wealth index, smoking status, depression, baseline chronic diseases, physical impairments, mutually adjusted for all activity classes, total time in all activity classes, and a random intercept for clustering of centers. HR indicates hazard ratio.
The 10-year adjusted PAF of excessive sitting time (more than 6 hours per day) was 3.7% for the composite outcome, 4.6% for mortality, and 3.5% for major CVD (eFigure 7 in the Supplement). The estimation is comparable with the PAFs for other lifestyle risk factors in PURE, such as physical inactivity, poor diet, and alcohol use (eTable 12 in the Supplement). The joint PAF of excessive sitting time and physical inactivity was 8.8% for mortality and 5.8% for CVD, which was nearly the same as the joint PAF of smoking (10.6% and 6.6%, respectively).
Discussion
In this large, international, prospective cohort study, we found daily sitting time was significantly associated with all-cause mortality and major CVD. By including diverse populations from countries at varying income levels, our study adds to the accumulating evidence on the risk of sitting time. Our data provide information from MICs and LICs, where the risk of increased sitting time is even more marked. Our findings support the WHO 2020 global guidelines for sedentary behavior and indicate that physical activity above the recommended level could attenuate the increased risk owing to sedentariness, and sedentary individuals may benefit from replacing sitting time with physical activity.
Overall, our study demonstrates a positive association of self-reported sitting time with all-cause mortality and major CVD, which is in line with previous meta-analyses (including studies using self-reported measurements from HICs)4,5,35,36 and recent prospective cohorts from China.6,7,8 Moreover, we found that the risk of composite outcome associated with sitting time increased in a linear manner, which was similar to a prospective cohort among 5638 older women from the US, demonstrating a linear relationship between objectively measured sedentary time and CVD.32 However, some previous meta-analyses using either subjective or objective measurements have suggested a nonlinear association with a potential threshold of sitting time, but the cutoff values were inconsistent.5,35,37,38,39 Previous meta-analyses using self-reported measurements generally estimated the threshold was 10 hours per day for incident CVD35 and 6 to 8 hours per day for mortality,5,37,38 whereas a large meta-analysis incorporating device-measured data reported the mortality risk significantly increased at levels higher than 9.5 hours per day.39 This difference may relate to variability in measurement methods. Accelerometer, which was generally used in existing studies, could provide a more accurate estimation of sedentary time than self-reported questionnaires, but it cannot differentiate between sitting and standing posture, and therefore, overestimates the time being sedentary.39,40 Therefore, although recommendations on limiting sitting time have emerged in recent public health guidelines, the specific quantitative threshold for sitting time still warrants further study.41
When stratified by country income levels, we observed a more pronounced association in LMICs and LICs compared with HICs and UMICs. The difference in the association might be partly explained by the different domains and patterns of sitting behaviors across different income levels; that is, television viewing time is more common among people with lower socioeconomic positions9 and showed a stronger association with outcomes compared with other sitting behaviors perhaps owing to coincident poor nutrition habits and prolonged and uninterrupted sedentary patterns.5,42 By contrast, spending more time in occupational sitting is often accompanied by higher socioeconomic status and healthier lifestyles, which might modify the excess mortality risk related to sitting time.42,43 Therefore, the association of total sitting time might be less pronounced in those with high socioeconomic levels. For example, the Whitehall II study, an occupational cohort of white-collar workers with high physical activity levels, reported a null association between total sitting time and mortality.44 This hypothesis was supported by subgroup analyses that sitting time showed a modest association among people with higher levels of education, household wealth, and occupation, but this requires further investigation of comparing associations between different types/domains of sedentary behavior in participants from a diverse context.
An important question of public health relevance in this area is the joint association of sitting time and physical activity. Similar to previous studies of recreational physical activity in HICs,24,25 we found that the association of sitting time with mortality plus major CVD was attenuated among those with higher levels of physical activity. Among those physically inactive participants, lowering sitting time was associated with a reduced risk of the composite outcome substantially, but the hazard in the low-sitting group (<4 hours per day) remained significantly higher compared with the reference group. This suggests that reducing sitting time alone is unlikely to achieve optimal health benefits without increasing physical activity. Our findings offer support for current guidelines that encourage “sit less and move more” for better health.3,45,46 Furthermore, prior findings also suggested that the mortality risk of a sedentary lifestyle was largely attenuated in the most physically active group (60-75 minutes per day in a meta-analysis harmonizing 13 prospective cohorts25; 300 minutes per week in a prospective cohort from Australia24). The current analysis differs in that some residual risk of the composite outcome and all-cause mortality owing to a sedentary lifestyle remained even among participants who reported greater than 750 minutes per week of MVPA. This difference could be explained by different domains of physical activity and sedentary behaviors and their varied health effects across different economic levels.26 Previous studies used recreational physical activity as the variable of interest, whereas most participants in PURE achieved high levels of physical activity through nonrecreational physical activity. Correspondingly, our isotemporal analysis showed that substituting sitting time with recreational physical activity could impart larger health benefits than nonrecreational physical activity, which corroborates with a large prospective cohort involving 154 614 older adults in the US, indicating that purposeful exercise could confer additional mortality protection against sedentariness than nonexercise activities.47
Our study showed that excessive sitting time (≥6 hours per day) accounted for 3.7% of the PAFs for the composite outcome, 4.6% for all-cause mortality, and 3.5% for major CVD. Of note, if reducing sitting time and increasing physical activity could be simultaneously achieved, the proportion of disease burden prevented is almost comparable with smoking.29,48 The recent WHO guideline states that adults should limit sedentary time and engage in 150 to 300 minutes per week of MVPA to reduce the detrimental effects of sedentary behaviors.3 Considering it might be challenging to achieve high levels of MVPA for physically inactive people, especially for older adults and those with chronic conditions or disabilities, reducing sitting time might be an important first step toward improving cardiovascular health.46
Strengths and Limitations
This study had several strengths, which included using data from 21 countries across 5 continents, high follow-up rates, rigorous approaches to measuring baseline variables, extensive covariates for adjustment, prospectively collected fatal and nonfatal events, and standardized adjudication of clinical events. However, our study also had some potential limitations. First, measurement error in self-reported variables is inevitable. We acknowledge that IPAQ may have compromised accuracy in capturing the absolute volumes of sitting time because it generally underestimates sitting time (2.5 hours per day) and only had fair to moderate agreement (correlation coefficient, 0.35; 95% CI, 0.32-0.39) against objective measurements.19,49 Unfortunately, device-based objective measurement of physical activity is likely too costly to be used in a large cohort study, especially in those resource-limited settings like some LICs and MICs in PURE. Self-report measurement could still be useful for grouping participants by their relative levels,40,50 but this would attenuate the associations toward the null because the information on sitting time was collected prospectively, and the measurement error of exposure would most likely be nondifferential with respect to disease status. Similarly, considering that the self-reported IPAQ tends to overestimate the physical activity levels, the real protective effect of physical activity against the risk associated with high sitting levels could be more pronounced and occur at a lower level than that reported in this study. Moreover, although the IPAQ has been validated in a wide range of countries, the self-report assessment might be culture-dependent, and cross-country differences in reporting sitting time are possible.17,18,19,20 However, our sensitivity analysis using country-specific quintiles and pooling country-specific estimates using a random-effects meta-analysis yielded similar findings to our primary analysis. A portion of the participants from India and Bangladesh were excluded from our primary analysis because IPAQ-measured sitting time was not administrated in the baseline questionnaire in these two countries. Our sensitivity analyses showed consistent findings after retaining participants from Bangladesh (using weekday sitting time as exposure) or conducting multiple imputation for those with missing exposure data. In addition, a causal relationship cannot be established owing to the possibility of reverse causality and residual confounding inherent in observational studies. However, a wide range of sensitivity analyses was conducted to test the robustness of our findings. In addition, the associations in our isotemporal modeling approaches were only derived from the statistical replacement but not from the actual changes in these behaviors.34
Conclusions
The results of our cohort study suggest that high sitting time was significantly associated with an increased risk of all-cause mortality and CVD in economically diverse settings, especially in LMICs and LICs. Moreover, the increased risks of high sitting time could be effectively offset by engaging in physical activity above currently recommended levels by the WHO. Our findings emphasize that reducing sedentary time along with increasing physical activity may be an important strategy for easing the global burden of premature deaths and CVD.
eAppendix. Funding, Staff, Methodology, and Analyses
eFigure 1. Flowchart Diagram of Participants Included in the Current Analysis
eFigure 2. Restricted Cubic Spline Curve for the Association of Daily Sitting Time With the Composite of Mortality Plus Major Cardiovascular Disease
eFigure 3. Restricted Cubic Spline Curve for the Association of Daily Sitting Time With the Composite of Mortality Plus Major Cardiovascular Disease After Excluding Participants Having Events Within the First 5 Years and Poor Health Condition at Baseline
eFigure 4. Meta-analysis of the Association of Sitting Time as a Continuous Exposure With Clinical Outcomes by Countries
eFigure 5. Joint Association of Physical Activity and Sitting Time With the Composite of All-Cause Mortality and Major Cardiovascular Events Using More Detailed Categorization of Physical Activity
eFigure 6. Joint Association of Physical Activity and Sitting Time With the Composite of All-Cause Mortality and Major Cardiovascular Events Stratified by Country Income Levels
eFigure 7. Adjusted 10-year Population Attributable Fractions and 95% CI of Prolonged Sitting Time (≥6 h/day)
eTable 1. Distribution of Daily Sitting Time in the Overall Population and Stratified by Geographical Region
eTable 2. Summary of Follow-up Events in the Overall Population and Stratified by Groups of Daily Sitting Time
eTable 3. Association of Country-Specific Quintiles of Sitting Time With Clinical Outcomes
eTable 4. Sensitivity Analysis for Further Adjusting for Potential Mediators or Confounders
eTable 5. Sensitivity Analysis for Addressing the Possibility of Reverse Causation
eTable 6. Sensitivity Analysis for Using the Injury as a Negative Control Outcome to Explore the Extent to Which the Association Between Sitting Time and Mortality Plus Major Cardiovascular Outcome is Explained by Confounding
eTable 7. Sensitivity Analysis for Assessing the Extent to Which the Association Between Sitting Time and Clinical Outcomes is Subject to Potential Unmeasured Confounding Factors
eTable 8. Sensitivity Analysis for Association of Weekday and Weekend Day Sitting Time With Clinical Outcomes
eTable 9. Multiple Imputation for Participants With Missing Data of Sitting Time
eTable 10. Subgroup Analyses of the Associations of Daily Sitting Time and the Composite Outcome
eTable 11. Stratified and Joint Association of Daily Sitting Time and Total Physical Activity With the Composite of All-Cause Mortality and Major CVD
eTable 12. Ten-Year Adjusted Population Attributable Fractions for Lifestyle Risk Factors
eReferences
References
- 1.Yang L, Cao C, Kantor ED, et al. Trends in sedentary behavior among the US population, 2001-2016. JAMA. 2019;321(16):1587-1597. doi: 10.1001/jama.2019.3636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du Y, Liu B, Sun Y, Snetselaar LG, Wallace RB, Bao W. Trends in adherence to the physical activity guidelines for Americans for aerobic activity and time spent on sedentary behavior among US adults, 2007-2016. JAMA Netw Open. 2019;2(7):e197597. doi: 10.1001/jamanetworkopen.2019.7597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451-1462. doi: 10.1136/bjsports-2020-102955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey DP, Hewson DJ, Champion RB, Sayegh SM. Sitting time and risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Prev Med. 2019;57(3):408-416. doi: 10.1016/j.amepre.2019.04.015 [DOI] [PubMed] [Google Scholar]
- 5.Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33(9):811-829. doi: 10.1007/s10654-018-0380-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu Q, Liu F, Li J, et al. Sedentary behavior and risk of incident cardiovascular disease among Chinese adults. Sci Bull. 2020;65(20):1760-1766. doi: 10.1016/j.scib.2020.05.029 [DOI] [PubMed] [Google Scholar]
- 7.Zhou W, Yan W, Wang T, et al. Independent and joint association of physical activity and sedentary behavior on all-cause mortality. Chin Med J (Engl). 2021;134(23):2857-2864. doi: 10.1097/CM9.0000000000001730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Zhou Q, Luo X, et al. Association between sedentary time and 6-year all-cause mortality in adults: the rural Chinese cohort study. J Nutr Health Aging. 2022;26(3):236-242. doi: 10.1007/s12603-022-1727-6 [DOI] [PubMed] [Google Scholar]
- 9.O’Donoghue G, Perchoux C, Mensah K, et al. ; DEDIPAC Consortium . A systematic review of correlates of sedentary behaviour in adults aged 18-65 years: a socioecological approach. BMC Public Health. 2016;16:163. doi: 10.1186/s12889-016-2841-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buck C, Loyen A, Foraita R, et al. ; DEDIPAC consortium . Factors influencing sedentary behaviour: a system based analysis using bayesian networks within DEDIPAC. PLoS One. 2019;14(1):e0211546. doi: 10.1371/journal.pone.0211546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dempsey PC, Biddle SJH, Buman MP, et al. New global guidelines on sedentary behaviour and health for adults: broadening the behavioural targets. Int J Behav Nutr Phys Act. 2020;17(1):151. doi: 10.1186/s12966-020-01044-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medina C, Jáuregui A, Hernández C, Shamah T, Barquera S. Physical inactivity and sitting time prevalence and trends in Mexican adults: results from 3 national surveys. PLoS One. 2021;16(7):e0253137. doi: 10.1371/journal.pone.0253137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ding C, Feng G, Yuan F, et al. Temporal trends and recent correlates in sedentary behaviors among Chinese adults from 2002 to 2010-2012. Int J Environ Res Public Health. 2019;17(1):158. doi: 10.3390/ijerph17010158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bowry AD, Lewey J, Dugani SB, Choudhry NK. The burden of cardiovascular disease in low- and middle-income countries: epidemiology and management. Can J Cardiol. 2015;31(9):1151-1159. doi: 10.1016/j.cjca.2015.06.028 [DOI] [PubMed] [Google Scholar]
- 15.Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S; PURE Investigators-Writing Group . The Prospective Urban Rural Epidemiology (PURE) study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. 2009;158(1):1-7.e1. doi: 10.1016/j.ahj.2009.04.019 [DOI] [PubMed] [Google Scholar]
- 16.Corsi DJ, Subramanian SV, Chow CK, et al. Prospective Urban Rural Epidemiology (PURE) study: baseline characteristics of the household sample and comparative analyses with national data in 17 countries. Am Heart J. 2013;166(4):636-646.e4. doi: 10.1016/j.ahj.2013.04.019 [DOI] [PubMed] [Google Scholar]
- 17.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381-1395. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 18.Rosenberg DE, Bull FC, Marshall AL, Sallis JF, Bauman AE. Assessment of sedentary behavior with the International Physical Activity Questionnaire. J Phys Act Health. 2008;5(suppl 1):S30-S44. doi: 10.1123/jpah.5.s1.s30 [DOI] [PubMed] [Google Scholar]
- 19.Bakker EA, Hartman YAW, Hopman MTE, et al. Validity and reliability of subjective methods to assess sedentary behaviour in adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2020;17(1):75. doi: 10.1186/s12966-020-00972-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wanner M, Probst-Hensch N, Kriemler S, Meier F, Autenrieth C, Martin BW. Validation of the long international physical activity questionnaire: influence of age and language region. Prev Med Rep. 2016;3:250-256. doi: 10.1016/j.pmedr.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bauman A, Ainsworth BE, Sallis JF, et al. ; IPS Group . The descriptive epidemiology of sitting: a 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41(2):228-235. doi: 10.1016/j.amepre.2011.05.003 [DOI] [PubMed] [Google Scholar]
- 22.van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172(6):494-500. doi: 10.1001/archinternmed.2011.2174 [DOI] [PubMed] [Google Scholar]
- 23.Bjørk Petersen C, Bauman A, Grønbæk M, Wulff Helge J, Thygesen LC, Tolstrup JS. Total sitting time and risk of myocardial infarction, coronary heart disease, and all-cause mortality in a prospective cohort of Danish adults. Int J Behav Nutr Phys Act. 2014;11:13. doi: 10.1186/1479-5868-11-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stamatakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. 2019;73(16):2062-2072. doi: 10.1016/j.jacc.2019.02.031 [DOI] [PubMed] [Google Scholar]
- 25.Ekelund U, Steene-Johannessen J, Brown WJ, et al. ; Lancet Physical Activity Series 2 Executive Committee; Lancet Sedentary Behaviour Working Group . Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? a harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-1310. doi: 10.1016/S0140-6736(16)30370-1 [DOI] [PubMed] [Google Scholar]
- 26.Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2643-2654. doi: 10.1016/S0140-6736(17)31634-3 [DOI] [PubMed] [Google Scholar]
- 27.Gupta R, Kaur M, Islam S, et al. Association of household wealth index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am J Hypertens. 2017;30(4):373-381. doi: 10.1093/ajh/hpw169 [DOI] [PubMed] [Google Scholar]
- 28.Yusuf S, Rangarajan S, Teo K, et al. ; PURE Investigators . Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371(9):818-827. doi: 10.1056/NEJMoa1311890 [DOI] [PubMed] [Google Scholar]
- 29.Yusuf S, Joseph P, Rangarajan S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395(10226):795-808. doi: 10.1016/S0140-6736(19)32008-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rajan S, McKee M, Rangarajan S, et al. ; Prospective Urban Rural Epidemiology (PURE) Study Investigators . Association of symptoms of depression with cardiovascular disease and mortality in low-, middle-, and high-income countries. JAMA Psychiatry. 2020;77(10):1052-1063. doi: 10.1001/jamapsychiatry.2020.1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chomistek AK, Manson JE, Stefanick ML, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: results from the Women’s Health Initiative. J Am Coll Cardiol. 2013;61(23):2346-2354. doi: 10.1016/j.jacc.2013.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bellettiere J, LaMonte MJ, Evenson KR, et al. Sedentary behavior and cardiovascular disease in older women: the Objective Physical Activity and Cardiovascular Health (OPACH) study. Circulation. 2019;139(8):1036-1046. doi: 10.1161/CIRCULATIONAHA.118.035312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laaksonen MA, Knekt P, Härkänen T, Virtala E, Oja H. Estimation of the population attributable fraction for mortality in a cohort study using a piecewise constant hazards model. Am J Epidemiol. 2010;171(7):837-847. doi: 10.1093/aje/kwp457 [DOI] [PubMed] [Google Scholar]
- 34.Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170(4):519-527. doi: 10.1093/aje/kwp163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pandey A, Salahuddin U, Garg S, et al. Continuous dose-response association between sedentary time and risk for cardiovascular disease: a meta-analysis. JAMA Cardiol. 2016;1(5):575-583. doi: 10.1001/jamacardio.2016.1567 [DOI] [PubMed] [Google Scholar]
- 36.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123-132. doi: 10.7326/M14-1651 [DOI] [PubMed] [Google Scholar]
- 37.Ku PW, Steptoe A, Liao Y, Hsueh MC, Chen LJ. A cutoff of daily sedentary time and all-cause mortality in adults: a meta-regression analysis involving more than 1 million participants. BMC Med. 2018;16(1):74. doi: 10.1186/s12916-018-1062-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013;8(11):e80000. doi: 10.1371/journal.pone.0080000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ekelund U, Tarp J, Steene-Johannessen J, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all-cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. doi: 10.1136/bmj.l4570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aunger J, Wagnild J. Objective and subjective measurement of sedentary behavior in human adults: a toolkit. Am J Hum Biol. 2022;34(1):e23546. doi: 10.1002/ajhb.23546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stamatakis E, Ekelund U, Ding D, Hamer M, Bauman AE, Lee IM. Is the time right for quantitative public health guidelines on sitting? a narrative review of sedentary behaviour research paradigms and findings. Br J Sports Med. 2019;53(6):377-382. doi: 10.1136/bjsports-2018-099131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim Y, Wilkens LR, Park SY, Goodman MT, Monroe KR, Kolonel LN. Association between various sedentary behaviours and all-cause, cardiovascular disease and cancer mortality: the Multiethnic Cohort Study. Int J Epidemiol. 2013;42(4):1040-1056. doi: 10.1093/ije/dyt108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garcia JM, Duran AT, Schwartz JE, et al. Types of sedentary behavior and risk of cardiovascular events and mortality in Blacks: the Jackson Heart study. J Am Heart Assoc. 2019;8(13):e010406. doi: 10.1161/JAHA.118.010406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pulsford RM, Stamatakis E, Britton AR, Brunner EJ, Hillsdon M. Associations of sitting behaviours with all-cause mortality over a 16-year follow-up: the Whitehall II study. Int J Epidemiol. 2015;44(6):1909-1916. doi: 10.1093/ije/dyv191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020-2028. doi: 10.1001/jama.2018.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dunstan DW, Dogra S, Carter SE, Owen N. Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev Cardiol. 2021;18(9):637-648. doi: 10.1038/s41569-021-00547-y [DOI] [PubMed] [Google Scholar]
- 47.Matthews CE, Moore SC, Sampson J, et al. Mortality benefits for replacing sitting time with different physical activities. Med Sci Sports Exerc. 2015;47(9):1833-1840. doi: 10.1249/MSS.0000000000000621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murray CJL, Aravkin AY, Zheng P, et al. ; GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-1249. doi: 10.1016/S0140-6736(20)30752-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Prince SA, Cardilli L, Reed JL, et al. A comparison of self-reported and device measured sedentary behaviour in adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2020;17(1):31. doi: 10.1186/s12966-020-00938-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Matthews CE, Moore SC, George SM, Sampson J, Bowles HR. Improving self-reports of active and sedentary behaviors in large epidemiologic studies. Exerc Sport Sci Rev. 2012;40(3):118-126. doi: 10.1097/JES.0b013e31825b34a0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Funding, Staff, Methodology, and Analyses
eFigure 1. Flowchart Diagram of Participants Included in the Current Analysis
eFigure 2. Restricted Cubic Spline Curve for the Association of Daily Sitting Time With the Composite of Mortality Plus Major Cardiovascular Disease
eFigure 3. Restricted Cubic Spline Curve for the Association of Daily Sitting Time With the Composite of Mortality Plus Major Cardiovascular Disease After Excluding Participants Having Events Within the First 5 Years and Poor Health Condition at Baseline
eFigure 4. Meta-analysis of the Association of Sitting Time as a Continuous Exposure With Clinical Outcomes by Countries
eFigure 5. Joint Association of Physical Activity and Sitting Time With the Composite of All-Cause Mortality and Major Cardiovascular Events Using More Detailed Categorization of Physical Activity
eFigure 6. Joint Association of Physical Activity and Sitting Time With the Composite of All-Cause Mortality and Major Cardiovascular Events Stratified by Country Income Levels
eFigure 7. Adjusted 10-year Population Attributable Fractions and 95% CI of Prolonged Sitting Time (≥6 h/day)
eTable 1. Distribution of Daily Sitting Time in the Overall Population and Stratified by Geographical Region
eTable 2. Summary of Follow-up Events in the Overall Population and Stratified by Groups of Daily Sitting Time
eTable 3. Association of Country-Specific Quintiles of Sitting Time With Clinical Outcomes
eTable 4. Sensitivity Analysis for Further Adjusting for Potential Mediators or Confounders
eTable 5. Sensitivity Analysis for Addressing the Possibility of Reverse Causation
eTable 6. Sensitivity Analysis for Using the Injury as a Negative Control Outcome to Explore the Extent to Which the Association Between Sitting Time and Mortality Plus Major Cardiovascular Outcome is Explained by Confounding
eTable 7. Sensitivity Analysis for Assessing the Extent to Which the Association Between Sitting Time and Clinical Outcomes is Subject to Potential Unmeasured Confounding Factors
eTable 8. Sensitivity Analysis for Association of Weekday and Weekend Day Sitting Time With Clinical Outcomes
eTable 9. Multiple Imputation for Participants With Missing Data of Sitting Time
eTable 10. Subgroup Analyses of the Associations of Daily Sitting Time and the Composite Outcome
eTable 11. Stratified and Joint Association of Daily Sitting Time and Total Physical Activity With the Composite of All-Cause Mortality and Major CVD
eTable 12. Ten-Year Adjusted Population Attributable Fractions for Lifestyle Risk Factors
eReferences




