Abstract
Purpose
Prone position is known to improve acute lung injury, and chest radiographs are often necessary to monitor disease and confirm support device placement. However, there is a paucity of literature regarding radiographs obtained in this position. We evaluated prone radiographs for distinguishing features and ability to identify support devices.
Methods
Pairs of prone and supine radiographs obtained during the COVID-19 pandemic were assessed retrospectively. IRB approval and waiver of informed consent were obtained. Radiographs were assessed for imaging adequacy, distinguishing features, and support device identification (endotracheal tube, enteric tube, or central line). Radiographs were reviewed by ≥ 2 cardiothoracic radiologists.
Results
Radiographs from 81 patients (63yo ± 13, 30% women) were reviewed. Prone and supine radiographs were comparable for imaging the lung bases (81% vs. 90%, p = 0.35) and apices (93% vs. 94%, p = 1); prone radiographs more frequently had significant rotation (36% vs. 19%, p = 0.021). To identify prone technique, scapula tip located beyond the rib border was 89% sensitive (95%CI 80–95%) and 85% specific (76–92%), and a fundal stomach bubble was 44% sensitive (33–56%) and 90% specific (81–96%). For women, displaced breast shadow was 46% sensitive (26–67%) and 92% specific (73–99%). Prone and supine radiographs each identified > 99% of support devices. Prone exams trended toward increased rate of malpositioned device (12% vs. 6%, p = 0.07).
Conclusion
Scapula position reliably distinguishes prone from supine position; fundal stomach bubble or displaced breast shadow is specific for prone position. Prone radiographs reliably identify line and tube position, which is particularly important as prone patients appear at increased risk for malpositioned devices.
Keywords: Prone position, Chest radiography, Critical care, COVID-19
Introduction
Prone positioning is often used in the management of acute respiratory distress syndrome [1]. Placement of patients in the prone position (i.e., “proning”) with respiratory failure can improve oxygenation [2, 3] and lung recruitment [3]. As these patients are often critically ill, with multiple support devices, routine radiography is often performed to monitor for disease progression, complications, and device positioning. Assessment of support devices is particularly important after changing to or from prone position, as tubes can get dislodged or shifted [4–6].
The prone position is not a standard view for chest radiography and the images are frequently not labeled as such by technologists. Moreover, radiologists and other clinicians are not experienced in interpreting these exams. There is a paucity of literature on chest radiography of prone patients, and the imaging features in proned, critically ill patients have not been well characterized. Furthermore, their reliability for verifying line and tube position is unknown. This was previously difficult to address given the intermittent use and overall low frequency of proned patients. However, proning has seen widespread adoption during the COVID-19 pandemic [7, 8], providing a substantial number of cases to review.
We assessed image quality and distinguishing features of prone radiographs in critically ill patients admitted to the hospital during the COVID-19 pandemic. We also assessed the ability to localize support devices, specifically endotracheal tubes, enteric tubes, and central lines.
Materials and Methods
IRB approval was obtained for this retrospective study. Informed consent was waived and HIPAA compliance was maintained. We reviewed portable chest radiographs obtained in nine hospitals at two academic institutions. Critically ill patients admitted during the COVID-19 pandemic from March 2020 to February 2021, who had both supine and prone radiographs within one calendar day, were included.
Portable chest radiographs were obtained using digital radiography machines. The cassette was placed directly beneath the patient, in either supine or prone position. Source to image distance (SID) was maintained at greater than 40 inches. Grid use was not standard, but could be employed in larger patients. Typical parameters ranged from 100 to 110 for kVp and 1 to 3.2 for mAs. Images were identified as prone or supine based on technologist reporting or in the medical record if not recorded by the technologist. One pair of supine and prone radiographs for each patient was reviewed in consensus by at least two sub-specialty-trained cardiothoracic radiologists. Reviewing radiologists were blinded to patient positioning—any indication of position on the radiograph was concealed prior to review.
Radiograph quality was assessed by evaluation for obscuration/exclusion of a lung base or apex and presence of significant rotation. Specific imaging characteristics assessed were position of the inferior scapula tips with respect to the lateral rib shadows, location of the stomach gas bubble within the fundus, and medial or superior displacement of one or both breast shadows. If an endotracheal tube, enteric tube, or central venous catheter were present, we noted if the tube or line position could be assessed adequately, and if it was properly positioned.
The association between prone/supine and each variable was assessed using Fisher exact test. Significance level was set at p = 0.05. Sensitivity and specificity were also calculated for predicting prone position and provided with 95% confidence interval. Logistic regression analysis was used to estimate the joined effect of multiple variables with prone or supine positioning.
Results
Eighty-one patients were included in the study (Table 1). Mean age was 63 years (± 13) and 24/81 (30%) of patients were women. Prone and supine position were comparable for adequate imaging of the lung bases [prone 68/81 (81%) vs. supine positioning 73/81 (90%), p = 0.35] and apices [prone 75/81 (93%) vs. supine positioning 76/81 (94%), p = 1]. Significant rotation was more common in prone radiographs [prone 29/81 (36%) vs. supine positioning 15/81 (19%), p = 0.021].
Table 1.
Distinguishing features and limitations of prone and supine radiographs
| Prone | Supine | p-value | |
|---|---|---|---|
| Patient number (N) | 81 | 81 | |
| Base adequately imaged | 68 (84%) | 73 (90%) | 0.350 |
| Apex adequately imaged | 75 (93%) | 76 (94%) | 1 |
| Significant rotation | 29 (36%) | 15 (19%) | 0.021 |
| Scapula tip beyond rib border | 72 (89%) | 12 (15%) | <0.001 |
| Stomach gas bubble in fundus | 36 (44%) | 8 (10%) | <0.001 |
| Displaced breast shadow | 11/24 (46%) | 2/24 (8%) | 0.008 |
| Lines and tubes adequately imaged | 177/178 (99%) | 201/202 (99.5%) | 1 |
| Endotracheal tube | 67/67 (100%) | 76/76 (100%) | 1 |
| Enteric tube | 65/66 (99%) | 72/73 (99%) | 1 |
| Central line | 45/45 (100%) | 53/53 (100%) | 1 |
| Malpositioned line or tube | 21/178 (12%) | 13/202 (6%) | 0.073 |
| Endotracheal tube | 10/67 (15%) | 5/76 (7%) | 0.170 |
| Enteric tube | 10/66 (15%) | 7/73 (10%) | 0.438 |
| Central line | 1/45 (2%) | 1/53 (2%) | 1 |
Categorical variables compared with Fisher exact test
Prone exams more frequently demonstrated one or both scapula tips located beyond the lateral rib border [prone 72/81 (89%) vs. supine positioning 12/81 (15%), p < 0.001] and more frequently demonstrated a fundal stomach gas bubble [prone 36/81 (44%) vs. supine positioning 8/81 (10%), p < 0.001; Fig. 1].
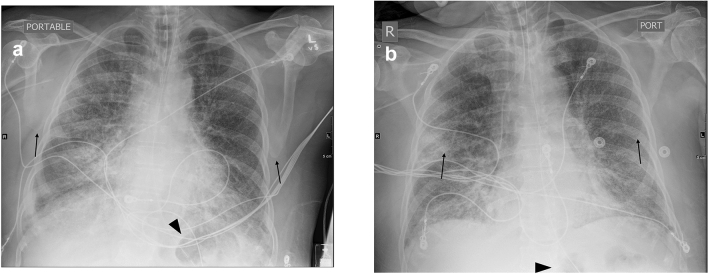
Fig. 1.
Distinguishing features of prone and supine radiographs demonstrated in a 61-year-old man. A, Prone radiograph demonstrates scapular tips (arrows) beyond the rib border and stomach gas bubble (arrowhead) localized at the fundus. B, Supine radiograph of the same patient demonstrates medial positioning of the scapular tips (arrows) and absence of gas at the expected location of the fundus. Gas seen more inferiorly is likely within the body of the stomach (arrowhead). Endotracheal and enteric tubes are well visualized in both positions
In women, a displaced breast shadow was more common with prone positioning [prone 11/24 (46%) vs. supine positioning 2/24 (8%), p = 0.008; Fig. 2]. To identify prone technique, scapular position was 89% sensitive (80–95%) and 85% specific (76–92%), fundal stomach bubble was 44% sensitive (33–56%) and 90% specific (81–96%), and a displaced breast shadow was 46% sensitive (26–67%) and 92% specific (73–99%). Logistic regression analysis showed that a lateral scapular tip (OR 37.0, p < 0.001) and fundal stomach bubble (OR 3.7, p = 0.023) were both predictive of prone positioning when each was in the model. Among women, the association between breast shadow displacement and patient position was not statistically significant (p = 0.4), with lateral scapular tip location and fundal stomach bubble being covariants.
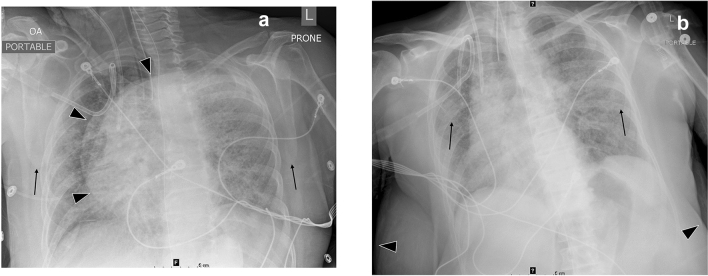
Fig. 2.
Distinguishing features of prone and supine radiographs for women demonstrated in a 64-year-old woman. A, Prone radiograph demonstrates medially displaced left breast shadow (arrowheads), in addition to scapula tips beyond the rib borders (arrows). B, Supine radiograph of the same patient demonstrates inferolateral positioning of breast shadows (arrowheads) and medial position of scapula tips (arrows); stomach gas bubble extends inferomedially, consistent with location in the gastric body. Endotracheal tube, enteric tube, and central line are well visualized in both positions
Both techniques reliably assessed line and tube position [prone 177/178 (99%) vs. supine positioning 202/203 (99.5%)]. Prone exams trended toward a higher rate of a malpositioned line or tube [prone 21/178 (12%) vs. supine positioning 13/202 (6%), p = 0.07].
Discussion
During the COVID-19 pandemic, proning of critically ill patients has become widespread and portable radiographs may be obtained while the patient is prone. In the present study, we found clear position-dependent differences between prone and supine portable chest radiographs. Scapular tip location beyond the rib border was most closely associated with prone positioning. When prone, the shoulders fall forward and the arms may be abducted, either of which will pull the scapulae laterally. The presence of a stomach gas bubble in the fundus was also associated with prone positioning, given the expected movement of gas to the most posterior location in the stomach; however, this finding is only helpful when a stomach bubble is present. Lastly, displacement of one or both breast shadows in women occurred more when prone; however, this finding did not add predictive value on logistic regression analysis.
Image quality was similar between prone and supine positioning. Radiographs in either position were usually adequate to image the base and apex. Prone radiographs were more likely to have significant rotation, but this affected only a minority of exams. Most importantly, prone radiographs reliably visualized support devices, including all endotracheal tubes and central lines. There was a trend toward more frequent line or tube malpositioning when patient was prone. This is not surprising, given the potential to dislodge devices during adjustment to the prone position [4–6] and underscores the need to evaluate support devices on prone radiographs.
The literature regarding radiography of prone patients is sparse. One publication from the era prior to widespread adoption of chest CT used prone position in stable patients to better evaluate the lungs in patients with pleural effusions. Postero-anterior radiographs in the prone position resulted in improved visualization of the lung bases, in the setting of moderate pleural effusions. Interestingly, the authors also performed cross-table lateral radiographs while prone, providing clear images of the lower lobes and posterior costophrenic angles. Similar to our findings, they noted that most cases had lateral scapulae and fundal stomach bubble (although, unlike in our study, they did not quantify their frequency). They found the breast shadows were usually lateral to the lung field—this is in contrast to our results and likely because their more stable patients could be precisely positioned [9]. This study used proning for diagnostic purposes, in non-critical patients, and therefore differs from our population. Regarding proning for therapeutic purposes, there is a single case report which followed a prone ICU patient with serial radiographs and demonstrated loss of the cardiac borders [10]. The authors emphasized this could be due to dependent atelectasis, which occurs anteriorly in the prone patient and should not necessarily be interpreted as worsening lung disease. This emphasizes that caution should be applied when comparing radiographs obtained in different positions, as changes in lung opacities may reflect technique rather than true change in disease extent.
Although prone radiography has not been assessed for critically ill patients or for COVID-19 patients specifically, other modalities of cardiothoracic imaging have been described for the prone position. Lung ultrasound, performed prior to and soon after proning, can predict response to proning in patients with ARDS due to COVID-19 [11], although this has mixed results for patients with ARDS due to other causes [12, 13]. Lung ultrasound has also been used to grade severity of COVID-19 pneumonia for supine or prone patients [14]. Trans-thoracic echocardiography has been studied more extensively, with a few small series establishing the feasibility of imaging prone COVID-19 patients [15–17]. Finally, case reports of COVID-19 patients have described use of prone chest CT [18, 19] and improved ventilation–perfusion matching while prone using electric impedance tomography [20].
Although potential benefits of proning were discovered as early as the 1970’s [2], improved outcomes and broader adoption are more recent developments [1]. The COVID-19 pandemic has ushered in widespread use of proning for critically ill patients, with demonstrable benefit [7]. Understanding the imaging-related benefits and drawbacks for prone patients has therefore recently become particularly relevant. Proning is likely to remain part of the management for acute lung injury, whether from COVID-19 or other causes.
Our patient cohort was collected over several months across numerous hospitals. However, limitations of the study include potential institution-specific practices or technologist labeling error. Subjective assessment of image quality is also a limitation, which was addressed by involving multiple readers.
Recognition of the chest radiographic features of proning should aid in interpretation of routine imaging in such patients, as in many instances the images are not specifically labeled. Physicians should take into account any change in position when comparing to prior exams. Critical care teams can be assured that prone radiographs do not diminish the ability to assess line placement.
Author Contributions
All authors contributed to the study conception and design. Preparation and data collection were performed by MS.L, RH, GM.V, AA.H, JJ, JM.L, CS.W, and LB.H. Data analysis was performed by MS.L and KY. MS.L wrote the first draft of the manuscript. All authors commented on prior drafts and read and approved the final version of the manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This study was approved by the institutional review board (IRB). Requirement for informed consent was waived.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 2.Douglas WW, Rehder K, Beynen FM, Sessler AD, Marsh HM. Improved oxygenation in patients with acute respiratory failure: the prone position. Am Rev Respir Dis. 1977;115(4):559–566. doi: 10.1164/arrd.1977.115.4.559. [DOI] [PubMed] [Google Scholar]
- 3.Galiatsou E, Kostanti E, Svarna E, Kitsakos A, Koulouras V, Efremidis SC, et al. Prone position augments recruitment and prevents alveolar overinflation in acute lung injury. Am J Respir Crit Care Med. 2006;174(2):187–197. doi: 10.1164/rccm.200506-899OC. [DOI] [PubMed] [Google Scholar]
- 4.Binda F, Galazzi A, Marelli F, Gambazza S, Villa L, Vinci E, et al. Complications of prone positioning in patients with COVID-19: a cross-sectional study. Intensive Crit Care Nurs. 2021 doi: 10.1016/j.iccn.2021.103088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Minonishi T, Kinoshita H, Hirayama M, Kawahito S, Azma T, Hatakeyama N, et al. The supine-to-prone position change induces modification of endotracheal tube cuff pressure accompanied by tube displacement. J Clin Anesth. 2013;25(1):28–31. doi: 10.1016/j.jclinane.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Wiggermann N, Zhou J, Kumpar D. Proning patients with COVID-19: a review of equipment and methods. Hum Factors. 2020;62(7):1069–1076. doi: 10.1177/0018720820950532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Langer T, Brioni M, Guzzardella A, Carlesso E, Cabrini L, Castelli G, et al. Prone position in intubated, mechanically ventilated patients with COVID-19: a multi-centric study of more than 1000 patients. Crit Care. 2021;25(1):128. doi: 10.1186/s13054-021-03552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathews KS, Soh H, Shaefi S, Wang W, Bose S, Coca S, et al. Prone positioning and survival in mechanically ventilated patients with coronavirus disease 2019-related respiratory failure. Crit Care Med. 2021;49(7):1026–1037. doi: 10.1097/CCM.0000000000004938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simonds B, Friedman PJ, Sokoloff J. The prone chest film. Radiology. 1975;116(1):11–17. doi: 10.1148/116.1.11. [DOI] [PubMed] [Google Scholar]
- 10.van der Werf TS, Wolf RF, Tulleken JE, Ligtenberg JJ, Zijlstra JG. The vanishing heart–deterioration on chest radiography with clinical improvement during prone position ventilation. Br J Radiol. 1998;71(844):447–449. doi: 10.1259/bjr.71.844.9659141. [DOI] [PubMed] [Google Scholar]
- 11.Avdeev SN, Nekludova GV, Trushenko NV, Tsareva NA, Yaroshetskiy AI, Kosanovic D. Lung ultrasound can predict response to the prone position in awake non-intubated patients with COVID19 associated acute respiratory distress syndrome. Crit Care. 2021;25(1):35. doi: 10.1186/s13054-021-03472-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haddam M, Zieleskiewicz L, Perbet S, Baldovini A, Guervilly C, Arbelot C, et al. Lung ultrasonography for assessment of oxygenation response to prone position ventilation in ARDS. Intensive Care Med. 2016;42(10):1546–1556. doi: 10.1007/s00134-016-4411-7. [DOI] [PubMed] [Google Scholar]
- 13.Wang XT, Ding X, Zhang HM, Chen H, Su LX, Liu DW, et al. Lung ultrasound can be used to predict the potential of prone positioning and assess prognosis in patients with acute respiratory distress syndrome. Crit Care. 2016;20(1):385. doi: 10.1186/s13054-016-1558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peschel G, Jung EM, Fisser C, Putz FJ, Wertheimer T, Sinner B, et al. Interstitial lung opacities in patients with severe COVID-19 pneumonia by bedside high-resolution ultrasound in association to CO2 retention. Clin Hemorheol Microcirc. 2021;77(4):355–365. doi: 10.3233/CH-200925. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Cruz E, Manzur-Sandoval D, Gopar-Nieto R, Murillo-Ochoa AL, Bejarano-Alva G, Rojas-Velasco G, et al. Transthoracic echocardiography during prone position ventilation: lessons from the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2020 doi: 10.1002/emp2.12239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gibson LE, Di Fenza R, Berra L, Bittner EA, Chang MG. Transthoracic echocardiography in prone patients with acute respiratory distress syndrome: a feasibility study. Crit Care Explor. 2020;2(8):e0179. doi: 10.1097/CCE.0000000000000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giustiniano E, Fazzari F, Bragato RM, Curzi M, Cecconi M. Trans-thoracic echocardiography in prone positioning COVID-19 patients: a small case series. SN Compr Clin Med. 2020 doi: 10.1007/s42399-020-00516-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGrath BA, Lowe R, Brady W, Sharman A, Felton T, Shelton CL. Computed tomography scanning in the prone position for a critically hypoxic patient with COVID-19. Anaesth Rep. 2020;8(1):71–72. doi: 10.1002/anr3.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sicuso C, Balzarini L, Lutman RF, Profili M, Lanza E, Politiabrini LS. Supine vs. prone chest CT in a COVID-19 patient during mechanical ventilation. Eurorad. 2020 doi: 10.35100/eurorad/case.16673. [DOI] [Google Scholar]
- 20.Zarantonello F, Andreatta G, Sella N, Navalesi P. Prone position and lung ventilation and perfusion matching in acute respiratory failure due to COVID-19. Am J Respir Crit Care Med. 2020;202(2):278–279. doi: 10.1164/rccm.202003-0775IM. [DOI] [PMC free article] [PubMed] [Google Scholar]