Abstract
Background/purpose
Pulpectomy is the last means to preserve primary teeth with pulpitis or pulp necrosis. The aim of the study was to investigate the survival rate of primary teeth after pulpectomies and to explore the factors influencing the prognosis of pulpectomy.
Materials and methods
This retrospective study was performed on patients who received primary tooth pulpectomy in the Department of Pediatric Dentistry at Peking University Hospital of Stomatology between January 2014 and February 2019. The demographic characteristics of children and the information of teeth treated were collected, and the clinical and radiographic examination after treatment were evaluated. Survival analysis was performed to determine the influencing factor of pulpectomy failure.
Results
A total of 592 primary anterior teeth and 583 primary molars were included. The 30-month survival rate of primary anterior teeth was 58.5% and that of primary molars was 37.0%. The survival rate of postoperative primary molars was lower than that of primary anterior teeth (P < 0.05). Primary anterior tooth interventions with preoperative periapical lesions, Vitapex® filling, or nongeneral anesthesia treatment had a higher failure risk (P < 0.05). Treatment at an older age and glass ionomer cement filling indicated a higher failure risk for primary molar pulpectomies.
Conclusion
Primary anterior teeth after pulpectomies had a higher survival rate than primary molars. Periapical lesions, treatment methods, and root filling materials had significant impacts on the prognosis of primary anterior pulpectomies, and children's age significantly affected the prognosis of primary molar pulpectomies, which has not been reported before.
Keywords: Pulpectomy, Survival analysis, Tooth, Deciduous
Introduction
Dental caries in primary teeth are a common chronic disease worldwide, with a prevalence rate of up to 46.2%,1 especially in developing countries. In China, the fourth national oral epidemiological investigation showed that the prevalence of dental caries in children aged 5 years was 71.9% and that the mean decayed-missing-filled teeth (dmft) index was 4.24,2 both of which were considerably higher than those 10 years earlier (66.0%, dmft = 3.5).3 Dental caries in the primary dentition progress rapidly, often affecting the pulp within a short duration. A requirement analysis of outpatient treatment in a public dental hospital in China showed that 32.2% of children were diagnosed with pulp disease.4 The American Association of Pediatric Dentistry (AAPD) recommends pulpectomy as an elective treatment for periapical periodontitis in primary teeth and regards pulpectomy as a final treatment to retain primary teeth with diffuse irreversible pulpitis or pulp necrosis.5
Studies on primary tooth pulpectomies, mainly on filling materials,6, 7, 8 irrigants,9 and instrumentation methods,10,11 have been published and reported success rates between 56% and 100%, with a follow-up time mostly no more than 18 months and small sample sizes. There are few studies on the factors affecting the prognosis of deciduous tooth pulpectomies, and the conclusions have been inconsistent. The difference in the success rate of pulpectomy in previous studies and the inconsistent evaluation of influencing factors on treatment have confused clinicians, and this is not conducive to clinical treatment. Therefore, long-term follow-up studies with large sample sizes are imperative.
A large number of primary teeth treated with pulpectomies were evaluated in this study, with a follow-up time of up to five years. This study aims to evaluate the long-term survival rate of pulpectomies in primary teeth and to analyze the potential factors influencing their success.
Materials and methods
This retrospective study was conducted in accordance with the tenets of the Declaration of Helsinki for research involving human subjects, and approved by the Ethics Committee of Peking University School and Hospital of Stomatology (approval number: PKUSSIRB-201949122). Informed consent to use the records was obtained from the patients’ guardians.
Participants
The study participants were selected among healthy children under 9 years old who received primary teeth pulpectomies in the Department of Pediatric Dentistry at Peking University Hospital of Stomatology between January 2014 and February 2019. The inclusion criteria were as follows:
-
1)
Teeth treated because of irreversible pulpitis or pulp necrosis, with or without periodontitis, for which radiographic examination showed no involvement of the permanent successor and minimal or no root resorption.
-
2)
X-ray examination was performed before and after treatment.
-
3)
Teeth from patients that underwent regular postoperative examination with a follow-up time of no less than 18 months.
Teeth meeting the criteria below were excluded:
-
1)
Teeth that have undergone trauma before treatment.
-
2)
Teeth with abnormality.
-
3)
Children with systemic diseases that affect oral hygiene maintenance, such as autism.
-
4)
Teeth with incomplete medical records.
All pulpectomies were completed in compliance with the AAPD guidelines and isolated with rubber dams.5 A six-month visit interval was recommended. Clinical and radiographic examinations were conducted during every follow-up.
Data collection
The following information from an electronic medical record system (Beijing Jiahe Meikang Information Technology, Beijing, China) of Peking University Hospital of Stomatology was collected:
-
1)
Demographic characteristics, including gender, birthdate, and systemic history.
-
2)
Dental treatment information, including the history of trauma, the first visit date, rank of attending doctor (intern or expert), tooth position (anterior or posterior), treatment method (under general anesthesia (GA) or not [GA or non-GA]), periapical lesion (yes or no), clinical and radiographic manifestations, root filling material (iodoform zinc oxide paste12 or Vitapex® [Neo-Dental, Tokyo, Japan]), and crown restoration material (resin filling, preformed metal crown [PMC], or glass ionomer cement [GIC]).
-
3)
Information obtained during follow-up, including following visit dates, chief complaints, and clinical and radiographic examinations. If the tooth was already missing, the date of loss and the associated symptoms were recorded.
Clinical and radiological evaluation
The pulpectomy was considered clinically successful in the absence of pain, abnormal mobility, gingival pathology, and severe crown restoration defects necessitating root canal retreatment or extraction in relation to the tooth. If not, it was labeled as a clinical failure.
If the radiographic examination revealed a decrease in size or disappearance of the initial periapical lesions within 6 months,5 with no new appearances of periapical lesions and/or pathological root resorption, the treatment was classified as a radiological success; otherwise, it was classified as a radiological failure.
The interventional outcome was defined as overall failure if the treatment exhibited clinical or radiological failure. In addition, premature loss and delayed root resorption of primary teeth after treatment were classified as failure,5 and the natural loss of primary teeth with normal clinical and radiographic findings was classified as success. The primary teeth were evaluated for premature loss or delayed root resorption by comparison with the contralateral teeth and/or other adjacent teeth without pulp treatment. If there were no contralateral teeth or adjacent teeth without pulp treatment, it was estimated based on the development stage of the permanent successor.
For primary teeth with failed pulpectomies, the date of failure was defined as enddate (T1), and the status of those interventions was recorded as “failed”. If the primary tooth pulpectomies didn't failed and were lost to follow-up, the status of the treatment was recorded as “censored”, and the final follow-up date was recorded as enddate (T2). The initial treatment date of the tooth was recorded as entdate (T0), and the survival time (TS) was calculated as follow:
All periapical films involved in this study were re-examined. Radiographic examinations were independently performed by two pediatric dentists. Reevaluations were done to reach consensus when the decisions of the examiners were conflict. Cohen's kappa statistic showed excellent reproducibility between the two investigators, with a measurement agreement of 0.85 and intraexaminer reliability (over two weeks) of 0.87.
Statistical analysis
Statistical analyses were conducted using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). Univariate analysis of categorical variables was performed using the chi-square test. The survival rate of teeth after pulpectomy was determined using the Kaplan–Meier method, and the log-rank test was applied to compare the difference between survival rates. Cox regression analysis was performed to estimate the influencing factors of pulpectomy. Variables with P < 0.1 in the univariate analysis were included in the multivariate analysis to be explored as possible risk factors. Factors previously reported to influence success were also included. The Wald test (Backward: Wald) method was used, and the significance level of the selected and excluded variables was 0.05.
Results
In total, 494 children (261 boys and 233 girls) and 1175 primary teeth were included in the study. The mean chronological age was 4.3 years, ranging from 1.4 to 8.5 years. The mean follow-up time was 998 days, ranging from 119 to 1871 days.
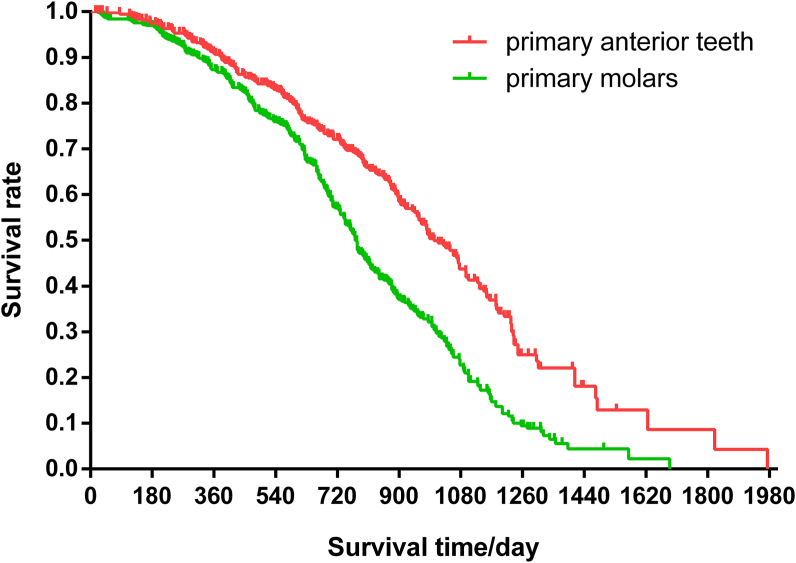
Among the 1175 primary teeth included, 592 were primary anterior teeth, and 583 were primary molars. There were 350 (59.1%) primary anterior teeth interventions and 220 (37.7%) primary posterior teeth interventions meeting the success criteria. The median survival time for primary anterior teeth was 1002 days and that for primary molars was 772 days. The survival rates of primary anterior teeth and primary molars are listed in Table 1. Statistical analysis showed that primary anterior teeth had a higher survival rate than primary molars (P < 0.001, Fig. 1). The primary anterior teeth and primary molars were analyzed separately in the following part because of their differences in the root canal morphology.
Table 1.
The survival rate of primary anterior teeth and primary molars after pulpectomies.
| Tooth position | 6 months | 12 months | 18 months | 24 months | 30 months | 36 months |
|---|---|---|---|---|---|---|
| Primary anterior teeth | 97.4% | 90.9% | 83.0% | 72.1% | 58.5% | 43.7% |
| Primary molars | 97.0% | 87.3% | 76.0% | 57.1% | 37.0% | 22.7% |
Figure 1.
The survival curves of primary anterior teeth and primary molars after pulpectomy
The follow-up results of primary anterior teeth
For primary anterior teeth, 242 teeth interventions were judged to have failed. Among them, 130 (53.7%) anterior teeth showed clinical failure and 203 (83.9%) anterior teeth showed radiographic failure with 110 of them being clinical normal; 2 (0.8%) teeth showed delayed root absorption. Two hundred and five teeth had X-rays at the moment of failure, 61 of them with succedaneous permanent tooth germ affected by primary teeth periapical periodontitis. The basic characteristics of the primary anterior teeth are presented in Table 2.
Table 2.
Basic information of primary anterior teeth and univariate analysis results.
| Factors | Censored | Failed | P∗ | |
|---|---|---|---|---|
| Age (year) | 350 | 242 | 0.078 | |
| Gender | Boy | 191 | 128 | 0.278 |
| Girl | 160 | 113 | ||
| Attending doctors | Intern | 25 | 40 | 0.002 |
| Expert | 326 | 201 | ||
| Treatment method | GA | 278 | 150 | 0.001 |
| Non-GA | 73 | 91 | ||
| Periapical lesion | No | 278 | 154 | 0.000 |
| Yes | 73 | 87 | ||
| Root canal filling materials |
Iodoform zinc oxide paste | 245 | 138 | 0.015 |
| Vitapex® | 106 | 103 | ||
| Crown restoration materials | Resin filling | 338 | 243 | -a |
| GIC filling | 8 | 3 | ||
∗Analyzed by Cox regression analysis, and the bold P value indicated that the difference was significant (P < 0.05).
GA, general anesthesia; GIC, glass ionomer cement; non-GA, non-general anesthesia.
The difference in sample size between the two groups was large, and no statistical test was conducted.
In the univariate analysis (Table 2), the survival rate of primary anterior teeth treated by experts was significantly higher than that of teeth treated by interns. The recurrence rate of primary anterior teeth with periapical lesions was higher than that of teeth without periapical lesions (P < 0.001). The anterior teeth treated under GA had a higher survival rate than teeth treated not under GA (P = 0.001), and teeth filled with iodoform zinc oxide paste had a higher survival rate than those filled with Vitapex® (P = 0.015) (Table 2).
Among the primary anterior teeth, 213 had crown restoration defects. The crown restoration defects can be divided into two categories: (i) severe restoration defect: the filling body/PMC of the teeth completely fell off, causing the orifice exposed in the oral cavity; (ii) non-severe restoration defect: secondary caries, filling body fractures etc. in which the orifice was still covered by the basing materials with or without imperfect filling body above.
Ninety-three successfully treated anterior teeth and 120 failed treated anterior teeth had filling defects. The incidence of filling body defects in the failed teeth was significantly higher than that in the successful teeth, and the chi-square test showed that the difference was statistically significant (Table 3).
Table 3.
Basic information of the crown fillings of primary anterior teeth after pulpectomies.
| Primary anterior teeth | With restoration defect |
Without restoration defect |
χ2 | P∗ | ||
|---|---|---|---|---|---|---|
| Severe restoration defect (N) | Non-severe restoration defect (N) | Total (N/%) | (N/%) | |||
| Successful | 0 | 93 | 93 (26.6%) | 257(73.4%) | 32.902 | 0.000 |
| Failed | 52 | 68 | 120 (49.6%) | 122(50.4%) | ||
∗Analyzed by chi-square test, and the bold P value indicated that the difference was significant (P < 0.05).
For primary anterior teeth, the failure risk of pulpectomies with GA was significantly lower than that of pulpectomies with no GA. Treatments of teeth with periapical lesions and Vitapex® filling were more likely to fail (P < 0.05) (Table 4).
Table 4.
Results of multivariate Cox regression analysis of primary anterior teeth after pulpectomy
| Co-variable | Subgroup | B | P∗ | HR | 95% CI for HR |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | 0.027 | 0.725 | 1.027 | 0.885 | 1.192 | |
| Attending doctors | Intern | 0 | 1 | |||
| Expert | −0.157 | 0.471 | 0.855 | 0.557 | 1.310 | |
| Treatment method | Non-GA | 0 | 1 | |||
| GA | −0.329 | 0.021 | 0.719 | 0.544 | 0.952 | |
| Periapical lesion | No | 0 | 1 | |||
| Yes | 0.353 | 0.014 | 1.424 | 1.073 | 1.889 | |
| Root canal filling material | Iodoform zinc oxide paste | 0 | 1 | |||
| Vitapex® | 0.322 | 0.015 | 1.380 | 1.064 | 1.790 | |
∗The bold P value indicated that the difference was significant (P < 0.05).
B, coefficient of regression; CI, confidence interval; GA, general anesthesia; HR, hazard ratio; non-GA, non-general anesthesia.
The follow-up results of primary molars
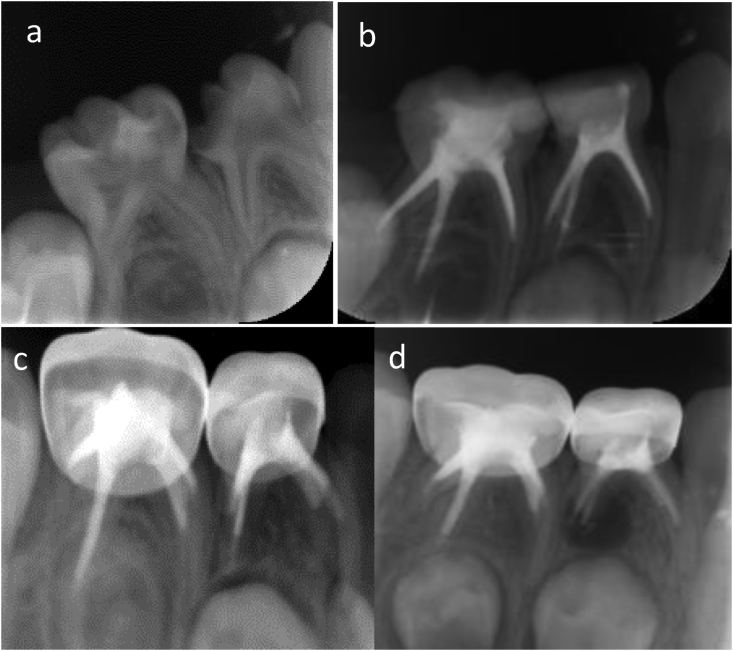
Of the 363 primary molars classified as failed (Fig. 2), 91 molars showed clinical failure, 353 molars suffered radiographic failure, and 1 tooth exhibited premature loss. The clinical and imaging findings of 271 primary molars were inconsistent, with normal clinical manifestations but abnormal radiographic examination. Of the 353 unsuccessful primary molar interventions with postoperative X-rays, 165 (46.7%) succedaneous permanent tooth germs were affected by periapical inflammation of the primary teeth. Basic information on the primary molars is presented in Table 5.
Figure 2.
The right mandibular first primary molar and second primary molar were treated with pulpectomies due to pulpitis caused by caries. a: The radiograph before treatment revealed no periapical radiolucency. b: The immediate postoperative radiograph showed adequate filling in distal root canals and slight underfilling in mesial root canals. c: Twelve months after pulpectomy, radiolucency was seen around the distal root of the first mandibular primary molar. d: Thirty-five months after pulpectomy, the area of radiolucency around the distal root of the first mandibular primary molar became larger, and the second primary molar also showed a periapical lesion around the mesial root. All the pulpectomies failed.
Table 5.
Basic information of primary molars after pulpectomy and univariate analysis results.
| Factors | Censored | Failed | P∗ | |
|---|---|---|---|---|
| Age (year) | 220 | 363 | 0.000 | |
| Gender | Boy | 124 | 183 | 0.185 |
| Girl | 96 | 180 | ||
| Attending doctors | Intern | 63 | 98 | 0.135 |
| Exporter | 157 | 265 | ||
| Treatment method | GA | 109 | 188 | 0.010 |
| Non-GA | 111 | 175 | ||
| Periapical lesion | No | 157 | 258 | 0.546 |
| Yes | 63 | 105 | ||
| Root filling materials | iodoform zinc oxide paste | 192 | 295 | 0.951 |
| Vitapex | 28 | 68 | ||
| Crown restoration material | Resin filling | 90 | 145 | 0.001 |
| GIC filling | 13 | 27 | ||
| PMC | 117 | 191 | ||
∗Analyzed by Cox regression analysis, and the bold P value indicated that the difference was significant (P < 0.05).
GA, general anesthesia; GIC, glass ionomer cement; non-GA, non-general anesthesia; PMC, preformed metal crown.
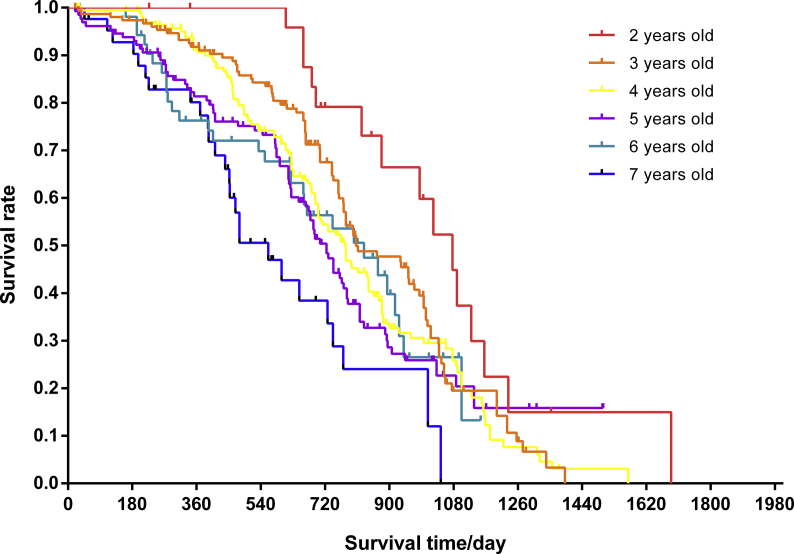
The univariate survival analysis (Table 5) showed that age had a significant impact on the failure risk of primary molars after pulpectomy (P < 0.001). A further analysis showed that the survival rate of primary molars of 2-year-old children was significantly higher than that of other age groups, and the survival rate of primary molars of over 7-year-old children was lower than that of other age groups (Fig. 3). Treatment under GA had a significantly lower failure risk than that not under GA (P = 0.010). The crown restoration material had a significant impact on the prognosis of molar pulpectomies (P = 0.001), and the recurrence rate of teeth with resin filling was lower than that with GIC filling.
Figure 3.
Survival curves of primary molars from children in different age groups after treatment.
Among the 583 primary molars, 88 molars had crown restoration defects during follow-up, including 20 severe restoration defects and 68 non-severe restoration defects. The classification of restoration defects was consistent with primary anterior teeth. The incidence of restoration defect between the molars survived after pulpectomy and the molars failed after pulpectomy showed no significant difference (P > 0.05) (Table 6).
Table 6.
Basic information of the crown restorations of primary molars after pulpectomies.
| Primary molars | With restoration defect |
Without restoration defect (N/%) | χ2 | Pa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Severe restoration defect (N) | Non-severe restoration defect (N) | Total (N/%) | ||||||||
| RF | GIC | PMC | RF | GIC | PMC | |||||
| Successful | 0 | 0 | 0 | 26 | 8 | 3 | 37(16.8%) | 183(83.2%) | 0.819 | 0.365 |
| Failed | 15 | 3 | 2 | 24 | 5 | 2 | 51(14.0%) | 312(86.0%) | ||
GIC, glass ionomer cement filling; PMC, preformed metal crown; RF, resin filling.
Analyzed by chi-square test.
The multivariate analysis results of the Cox regression showed that age and crown restoration material had a statistically significant impact on the failure risk of primary molar pulpectomies (Table 7). The failure risk of treatment increased with age, and the hazard ratio (HR) was 1.185 (95% CI, 1.082–1.297) (P < 0.001). Interventions with GIC restorations were more likely to fail than those with resin filling (P < 0.05).
Table 7.
Results of multivariate Cox regression analysis of primary teeth after pulpectomy
| Co-variable | Subgroup | B | P∗ | HR | 95% CI for HR |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | – | 0.169 | 0.000 | 1.185 | 1.082 | 1.297 |
| Attending doctors | Intern | 0 | 1 | |||
| Exporter | −0.041 | 0.762 | 0.960 | 0.737 | 1.251 | |
| Treatment method | Non-GA | 0 | 1 | |||
| GA | −0.015 | 0.936 | 0.985 | 0.682 | 1.422 | |
| Periapical lesion | No | 0 | 1 | |||
| Yes | −0.095 | 0.439 | 0.910 | 0.715 | 1.157 | |
| Root filling materials | Iodoform zinc oxide paste | 0 | 1 | |||
| Vitapex | 0.063 | 0.651 | 1.065 | 0.811 | 1.397 | |
| Restoration materials | Resin filling | 0 | 1 | |||
| GIC filling | 0.414 | 0.049 | 1.513 | 1.002 | 2.285 | |
| PMC | −0.138 | 0.231 | 0.871 | 0.695 | 1.092 | |
∗The bold P value indicated that the difference was significant (P < 0.05).
B, coefficient of regression; CI, confidence interval; GA, general anesthesia; GIC, glass ionomer cement; HR, hazard ratio; non-GA, non-general anesthesia; PMC, preformed metal crown.
Discussion
This study had a much larger sample size than previous studies on pulpectomy,13,14 with a mean follow-up time of 33 months and longest follow-up time of 62 months. The survival rate of primary anterior teeth at 24 months after pulpectomy was 72.1%, higher than 57.1% of primary molars. Studies have reported different success rates of pulpectomies between primary anterior teeth and primary molars, but the difference was not statistically significant due to the small sample size, especially in anterior teeth.15,16 This distinction is speculated to be caused by morphological differences in primary teeth. Most primary anterior teeth have a single canal and few lateral branches or root tip bifurcations,17 but different forms of the accessory root canal are common in primary molars. Morabito et al. observed 30 primary molars using a scanning electron microscope and found that 21 of them had accessory canals at the bottom of the pulp chamber, in which pulp tissue and necrotic tissue were observed.18 The complex structure of the root canal is not conducive to the removal of infection, and the remaining bacteria lead to pulpectomy failure.19 Therefore, primary anterior and posterior teeth were analyzed independently in this study.
Pulpectomies of primary anterior teeth with periapical lesions were more likely to fail than those of teeth without periapical lesions. It is difficult to remove all the pathogenic bacteria in the periapical tissue through chemo-mechanical preparation, and the residual bacteria can increase the postoperative failure risk.20 Chen et al. also reported worse prognosis of pulpectomy in primary teeth with periapical lesions.16 However, interventions in primary molars with periapical lesions had a similar survival rate to teeth without periapical lesions. As mentioned before, the canal system of primary molars is more complicated than that of primary anterior teeth, and it is speculated that there is more residual infection in the primary molar canal system after root canal preparation than in the root canals of anterior teeth, which can also cause occurrence of periapical periodontitis.
In anterior teeth, pulpectomies with non-GA had a lower survival rate than those with GA. Children who need pulpectomies of deciduous anterior teeth are young and always have poor cooperation. When treated under general anesthesia, the root canal can be prepared and disinfected more thoroughly without being affected by poor cooperation of children. Meanwhile, resin restoration, which is sensitive to the technique and humidity, could be carried out with good moisture control. It was reported that the time of secondary caries on teeth treated under GA was significantly later than that in the non-GA group.21 In this study, the percentage of filling defects in the GA group was 31.8%, which was lower than that in the non-GA group (47.0%). The occurrence of filling defect was related to the failure of treatment (Table 3).
Vitapex and iodoform zinc oxide pastes are commonly used root filling pastes.22 Some studies have shown that the success rate of iodoform zinc oxide paste pulpectomy is higher than that of Vitapex after treatment.13 However, other studies have shown different results.6,23 In this study, treatment with Vitapex filling had a higher failure risk than that with zinc oxide iodoform paste. Vitapex is easy to absorb after being overcharged,23 and the material in the root canal is absorbed faster than the root, resulting in emptiness in the root canal,24,25 which may be one of the reasons for the failure.
For primary molars, we found that treatment at older ages was more likely to fail than that at a younger age, and the difference was statistically significant. This finding has not been reported previously. According to previous studies on permanent teeth,26, 27, 28 root canal morphology changes with age, and secondary dentin deposition may change the root canal diameter or lead to severe canal calcification, increasing the difficulty of root canal preparation. In primary molars, similar age-related changes were also reported by Amano et al., indicating that the volume ratio between the pulp chamber and the crown is larger in the primary dentition than in the mixed dentition.29 The reason why the success rate of pulpectomy was affected by age may be related to changes in root canal anatomy with age. Ahmed suggested that it is necessary to study the relationship between canal morphology and pulpectomy failure.30 The discovery of the influencing factor of age is beneficial to predict the prognosis of pulpectomy before treatment, reminding doctors to pay special attention to checking the molar pulpectomies of older children.
In this study, the crown of primary molars was restored by resin filling, GIC filling and PMC. The results revealed that the failure risk of primary molar pulpectomies with GIC filling was higher than that of resin filing, and the difference between resin filling and PMC was not significant in the multivariate analysis. The teeth after GIC filling were prone to filling defects, with an incidence rate of 40.0%, which was higher than that of PMC (2.3%) and resin filling (27.7%). Fine crown restoration can prevent micro leakage and has an impact on the prognosis of pulpectomy.31 After pulpectomy, clinicians should attach importance to crown repair and carry out permanent restoration as soon as possible. Although the survival rate of PMC was higher than that of resin filling in terms of restoration materials,32 the prognosis of pulpectomy restored by PMC and resin composite showed no significant differences, considering the apical periodontal health was used as the outcome in this study. A similar result was reported by Moskovitz.33 The failure rate of pulpectomies with PMC and resin filling (RF) was 62.0% and 61.7% respectively, which were much higher than the incidence of crown restoration defect of PMC and RF mentioned above. This is because the recurrence of periapical periodontitis after root canal therapy is not only affected by crown restoration, but also affected by other factors such as case selection, evaluation criteria, etc.
There are some limitations to this study. First, the inconsistency between radiographic and clinical manifestations makes it difficult to detect periapical diseases on time. Regular radiographic examination is recommended for primary teeth after pulpectomy to find the periapical lesion in time. However, in children, the potential radiation damage caused by multiple radiographic evaluations should be carefully considered to determine the risk-benefit ratio. Second, this is a retrospective study based on existing case records, in which there may be a recording inaccuracy. To avoid false records, we also checked all of the X-ray films when the records were examined.
The survival rate of primary molars was much lower than that of primary anterior teeth. The presence of periapical lesions for anterior teeth and children's age for primary molars can be predictors for the prognosis of pulpectomy. For primary anterior teeth, treatment under GA and with iodoform zinc oxide paste filling had a lower failure risk.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The authors thank Xueying Li, from Peking University First Hospital, for help with the statistical analyses and the American Journal Experts editing team for their language editing services. This project was supported by grant Capital's Funds for Health Improvement and Research (Grant number: 2020-2-4105).
References
- 1.Kazeminia M., Abdi A., Shohaimi S., et al. Dental caries in primary and permanent teeth in children's worldwide, 1995 to 2019: a systematic review and meta-analysis. Head Face Med. 2020;16:22. doi: 10.1186/s13005-020-00237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X. People's Medical Publishing House; Beijing, China: 2018. Report of the fourth national oral health epidemiology investigation; p. 50. [Google Scholar]
- 3.Qi X.Q. People's Medical Publishing House; Beijing, China: 2008. Report of the third national oral health epidemiology investigation; p. 60. [Google Scholar]
- 4.Xia B., Qin M., Han Y., Zhang S. Children stomatology outpatient treatment requirements analysis and countermeasures. J Peking Univ (Heal Sci) 2013;45:92–96. [In Chinese, English abstract] [PubMed] [Google Scholar]
- 5.AAPD Council On Clinical Affairs Pulp therapy for primary and immature permanent teeth. Pediatr Dent. 2018;40:343–351. [PubMed] [Google Scholar]
- 6.Pramila R., Muthu M.S., Deepa G., Farzan J.M., Rodrigues S.J. Pulpectomies in primary mandibular molars: a comparison of outcomes using three root filling materials. Int Endod J. 2016;49:413–421. doi: 10.1111/iej.12478. [DOI] [PubMed] [Google Scholar]
- 7.Nakornchai S., Banditsing P., Visetratana N. Clinical evaluation of 3Mix and Vitapex as treatment options for pulpally involved primary molars. Int J Paediatr Dent. 2010;20:214–221. doi: 10.1111/j.1365-263X.2010.01044.x. [DOI] [PubMed] [Google Scholar]
- 8.Trairatvorakul C., Chunlasikaiwan S. Success of pulpectomy with zinc oxide-eugenol vs calcium hydroxide/iodoform paste in primary molars: a clinical study. Pediatr Dent. 2008;30:303–308. [PubMed] [Google Scholar]
- 9.Verma N., Sangwan P., Tewari S., Duhan J. Effect of different concentrations of sodium hypochlorite on outcome of primary root canal treatment: a randomized controlled trial. J Endod. 2019;45:357–363. doi: 10.1016/j.joen.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 10.George S., Anandaraj S., Issac J.S., John S.A., Harris A. Rotary endodontics in primary teeth - a review. Saudi Dent J. 2016;28:12–17. doi: 10.1016/j.sdentj.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azar M.R., Safi L., Nikaein A. Comparison of the cleaning capacity of Mtwo and Pro Taper rotary systems and manual instruments in primary teeth. Dent Res J. 2012;9:146–151. doi: 10.4103/1735-3327.95227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao D.H., Xie L.H., Liu H., Qin M., Han R., Zheng L.G. Formulation optimization of iodoform paste for root canal filling of deciduous teeth. Zhongguo yao xue hui. 2017;52:135–139. [In Chinese, English abstract] [Google Scholar]
- 13.Chen X., Liu X., Zhong J. Clinical and radiographic evaluation of pulpectomy in primary teeth: a 18-months clinical randomized controlled trial. Head Face Med. 2017;13:12. doi: 10.1186/s13005-017-0145-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cassol D.V., Duarte M.L., Pintor A.V.B., Barcelos R., Primo L.G. Iodoform vs calcium hydroxide/zinc oxide based pastes: 12-month findings of a randomized controlled trial. Braz Oral Res. 2019;33:e02–e03. doi: 10.1590/1807-3107bor-2019.vol33.0002. [DOI] [PubMed] [Google Scholar]
- 15.Coll J.A., Sadrian R. Predicting pulpectomy success and its relationship to exfoliation and succedaneous dentition. Pediatr Dent. 1996;18:57–63. [PubMed] [Google Scholar]
- 16.Chen Y., Li H., Li M., Yang L., Sun Q., Chen K. Analysis of survival and factors associated with failure of primary tooth pulpectomies performed under general anaesthesia in children from South China. Int J Paediatr Dent. 2020;30:225–233. doi: 10.1111/ipd.12589. [DOI] [PubMed] [Google Scholar]
- 17.Salama F.S., Anderson R.W., McKnight-Hanes C., Barenie J.T., Myers D.R. Anatomy of primary incisor and molar root canals. Pediatr Dent. 1992;14:117–118. [PubMed] [Google Scholar]
- 18.Morabito A., Defabianis P. A SEM investigation on pulpal-periodontal connections in primary teeth. ASDC (Am Soc Dent Child) J Dent Child. 1992;59:53–57. [PubMed] [Google Scholar]
- 19.Cancio V., Carvalho Ferreira D.D., Cavalcante F.S., et al. Can the Enterococcus faecalis identified in the root canals of primary teeth be a cause of failure of endodontic treatment? Acta Odontol Scand. 2017;75:423–428. doi: 10.1080/00016357.2017.1328742. [DOI] [PubMed] [Google Scholar]
- 20.Siqueira J.F.P., Rôças I.N.P. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod. 2008;34:1291–1301.e3. doi: 10.1016/j.joen.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 21.Zhou F., Xia B., Zhang S., Ma W.L., Xiao Y.M., Ge L.H. Comparison of long-term dental treatment effects of children treated under general anesthesia and passive restraint. Chin J Stomatol. 2017;52:96–102. doi: 10.3760/cma.j.issn.1002-0098.2017.02.009. [In Chinese, English absract] [DOI] [PubMed] [Google Scholar]
- 22.Smaïl-Faugeron V., Glenny A., Courson F., Durieux P., Muller-Bolla M., Fron Chabouis H. Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst Rev. 2018;5:CD003220. doi: 10.1002/14651858.CD003220.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mortazavi M., Mesbahi M. Comparison of zinc oxide and eugenol, and Vitapex for root canal treatment of necrotic primary teeth. Int J Paediatr Dent. 2004;14:417–424. doi: 10.1111/j.1365-263X.2004.00544.x. [DOI] [PubMed] [Google Scholar]
- 24.Nurko C., Ranly D.M., Garcia-Godoy F., Lakshmyya K.N. Resorption of a calcium hydroxide/iodoform paste (Vitapex) in root canal therapy for primary teeth: a case report. Pediatr Dent. 2000;22:517–520. [PubMed] [Google Scholar]
- 25.Ozalp N., Saroglu I., Sonmez H. Evaluation of various root canal filling materials in primary molar pulpectomies: an in vivo study. Am J Dent. 2005;18:347–350. [PubMed] [Google Scholar]
- 26.Morse D.R., Esposito J.V., Schoor R.S. A radiographic study of aging changes of the dental pulp and dentin in normal teeth. Quintessence Int. 1993;24:329–333. [PubMed] [Google Scholar]
- 27.Kiefner P., Connert T., Elayouti A., Weiger R. Treatment of calcified root canals in elderly people: a clinical study about the accessibility, the time needed and the outcome with a three-year follow-up. Gerodontology. 2017;34:164–170. doi: 10.1111/ger.12238. [DOI] [PubMed] [Google Scholar]
- 28.Morse D.R., Esposito J.V., Schoor R.S., Williams F.L., Furst M.L. A review of aging of dental components and a retrospective radiographic study of aging of the dental pulp and dentin in normal teeth. Quintessence Int. 1991;22:711–720. [PubMed] [Google Scholar]
- 29.Amano M., Agematsu H., Abe S., et al. Three-dimensional analysis of pulp chambers in maxillary second deciduous molars. J Dent. 2006;34:503–508. doi: 10.1016/j.jdent.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Ahmed H.M. Anatomical challenges, electronic working length determination and current developments in root canal preparation of primary molar teeth. Int Endod J. 2013;46:1011–1022. doi: 10.1111/iej.12134. [DOI] [PubMed] [Google Scholar]
- 31.Seale N.S. Stainless steel crowns improve success rate of root canal treatment in primary teeth. J Evid Base Dent Pract. 2005;5:205–206. doi: 10.1016/j.jebdp.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 32.Zahdan B.A., Szabo A., Gonzalez C.D., Okunseri E.M., Okunseri C.E. Survival rates of stainless steel crowns and multi-surface composite restorations placed by dental students in a pediatric clinic. J Clin Pediatr Dent. 2018;42:167–172. doi: 10.17796/1053-4628-42.3.1. [DOI] [PubMed] [Google Scholar]
- 33.Moskovitz M., Sammara E., Holan G. Success rate of root canal treatment in primary molars. J Dent. 2005;33:41–47. doi: 10.1016/j.jdent.2004.07.009. [DOI] [PubMed] [Google Scholar]