Abstract
Under the burden caused by COVID-19 and rapid lifestyle changes, many people increased their screen time due to psychological needs and social requirements. The current study investigated the relationship between screen time changes and anxiety symptoms during the pandemic of COVID-19. Furthermore, we examined whether sleep and physical activity would mediate the association between screen time changes and anxiety. The self-developed questionnaire was delivered online to collect people’s changes in anxiety, sleep patterns, and screen time during COVID-19. 970 participants (74.4% female) with an average age of 23 years were involved in this study. After adjusting demographic variables, the ordinal logistic regression analyses revealed that a significant increase in screen time was linked with anxiety. Slightly increased screen time, slightly and significantly decreased screen time did not predict anxiety symptoms during the pandemic. The level of anxiety was significantly higher among respondents who reported decreased sleep quality. Sleep quality directly mediated the association between screen time changes and anxiety, while sleep latency did not. The longer sleep latency caused by increased screen time would amplify anxiety by affecting sleep quality. In addition, the relationship between screen time changes and anxiety was also mediated by physical activity. We concluded that the fluctuation of screen time in a modest range does not affect the anxiety level substantially. The significantly increased screen time would contribute to poor sleep (including longer sleep latency and worse sleep quality) and lack of physical activity, which would lead to higher levels of anxiety.
Keywords: COVID-19, Screen time changes, Anxiety symptoms, Sleep, Physical activity
Introduction
On January 30, 2020, the COVID-19 pandemic was listed as a public health emergency of international concern. The virus was later found to have human-to-human transmission characteristics and mainly spread through contact and respiratory droplets [1]. The unpredictable and uncontrollable pandemic caused widespread public anxiety and panic [2]. A recent review demonstrated the prevalence of anxiety symptoms ranging from 6.33 to 50.9% during the pandemic [3]. From March to April 2020, many countries implemented enforcement such as home quarantine, traffic control, and businesses and schools closures to stop the further escalation of the pandemic [4]. Cities with severe pandemics implemented a stay-at-home policy [5], people were not allowed out of the home and were required to do remote working at home or distance learning [6]. The social isolation led to a deterioration in psychological conditions, increasing feelings of loneliness and anxiety [7, 8]. The restrictions during the pandemic led to longer screen time for using Internet devices, seeking emotional relief, and ameliorating social isolation [9, 10]. Online work, study, and social interaction may also cause increased screen time. A survey covering 12,107 people showed that the screen time among Chinese residents was about 4.4 h during home quarantine [11].
During COVID-19, screen time rises significantly due to psychological needs and social requirements [12, 13]. Under the pressure of pandemics, people tend to use smartphones excessively to cope with negative emotions [10, 14]. However, excessive use of electronic devices (mobile phones, computers, TV, etc.) and persistently increased screen time have recently been linked to anxiety symptoms [10, 14–19]. The negative impact of excessive screen time on mental health may be exacerbated under highly stressful conditions like COVID-19. During the pandemic, people search online to access news about COVID-19, and excessive attention to such information could cause an increase in anxiety [2]. Meanwhile, the increased screen time may aggravate the lack of social interaction and physical activity caused by home quarantine, resulting in anxiety symptoms [20, 21]. Given the possible impact of screen time changes during COVID-19, we consider that excessive screen time would contribute to higher anxiety levels. Nevertheless, people were already had excessive screen time before the pandemic, and prolonged use of electronic devices negatively affects mental health [14–16]. The impact of total screen time on anxiety may not reflect the influence of changes in screen time due to COVID-19. We thus examined the effect of screen time changes on anxiety during the pandemic. In addition, the potential mechanism of the effect between screen time changes and anxiety during the pandemic is unknown, and we explored this further.
In recent years, several studies have indicated that sleep and physical activity might play significant roles in the relationship between screen time and negative emotion, but the underlying mechanism of sleep and physical activity in this relationship has not been examined totally [22–25]. Extensive research has shown that excessive screen time caused longer sleep latency, insufficient sleep duration, and poor sleep quality [26–29]. Excessive screen time, especially time spent in the evening, may delay bedtime. Blue light from digital devices could suppress melatonin and lead to circadian rhythm disorder, which ultimately causes poor sleep outcomes [26, 30, 31]. In addition, cognitive arousal for browsing the web may delay or disrupt sleep [32], given that screen use could affect sleep for these reasons, and excessive screen time may disturb sleep mainly by delayed sleeping time. Poor sleep quality is also linked with the prevalence of anxiety symptoms [33].
Similar to sleep, physical activity may mediate the relationship between screen time changes and anxiety. In previous studies, people with long screen time typically reported less time for physical activity [11, 34, 35]. Importantly, the benefits of physical activity on anxiety have been recognized, not only under normal conditions but also during the pandemic [36–42]. During COVID-19, people who achieved physical activity-recommended guidelines showed a significantly lower possibility of experiencing higher levels of anxiety [41]. Physical activity acts on multiple biological and psychological systems, leads to synergistic adaptations that effectively reduce anxiety symptoms [43], and tends to activate anti-inflammatory mechanisms to diminish oxidative stress [38]. Additionally, lower amounts of physical activity were associated with higher daily screen time during the pandemic [42].
In sum, sleep and physical activity may be mediators between screen time and anxiety during home quarantine of COVID-19. Our hypotheses are also supported by the digital displacement model, which interprets the indirect effect of screen time on mental health [20, 23]. The theory assumes that excessive screen time may displace the time of engaging in activities that are more beneficial for mental health, including face-to-face social interaction, sleep, exercise, reading, and time spent outdoors [20, 22, 44–46], and the affected activities would further affect negative emotion.
The present study aimed to determine whether screen time changes affect anxiety during COVID-19 and further examine the mechanism between screen time and anxiety changes. Therefore, we proposed the following hypotheses and built the corresponding model: (1) increased screen time caused by COVID-19 might have a negative effect on anxiety; (2) screen time changes may affect anxiety by affecting sleep latency and subjective sleep quality; (3) screen time changes may impact subjective sleep quality through sleep latency; (4) changes in screen time would affect anxiety through physical activity. The conceptual hypothesized model is shown in Fig. 1.
Fig. 1.
The conceptual model of this study
Methods
Participants and procedures
This was a cross-sectional study conducted from March to April 2020. The self-developed questionnaire was delivered on the website to comply with the policies for controlling COVID-19 transmission. The participants completed the questionnaire by clicking a link on social media. Through a convenience sampling method, a total of 1109 adults from 31 provinces in China filled in the questionnaire voluntarily online. Finally, 970 participants met the following criteria and were included in the data analysis: (1) aged 18 years and above, (2) completed the questionnaire correctly, (3) slept 6–10 h every night. Participants were asked to report their changes in screen time, physical activity, sleep, and mental conditions during the home quarantine for the COVID-19 pandemic. This study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Ethical Committee of the South China Normal University. Each participant signed informed consent before study commencement.
Measures
Anxiety
The following question assessed changes in the levels of anxiety: compared with the day before COVID-19, how has your anxiety level changed during the stay at home? A 5-point Likert scale was used to rate the item: 1 = dropped significantly, 2 = dropped slightly, 3 = unchanged, 4 = increased slightly, 5 = increased significantly.
Screen time changes
A single question assessed the changes in screen time: compared with the day before COVID-19, how would you rate the screen time changes (including computers, TVs, mobile phones, etc.) during the stay at home? The question was evaluated by a 5-point Likert scale: 1 = decreased significantly, 2 = decreased slightly, 3 = unchanged, 4 = increased slightly, 5 = increased significantly.
Sleep
Sleep latency: Four items were used to obtain the difference in sleep latency before and after the COVID-19 pandemic. Participants were asked to report the time it takes to fall asleep after going to bed or putting down the phone on weekdays and weekends before and after the pandemic. The changes in sleep latency were calculated as the difference between sleep latency before and after the pandemic.
Sleep quality: A single item measured sleep quality changes: compared with the days before the COVID-19 pandemic, how would you rate the changes in sleep quality during the stay at home? The item was rated by a 5-point Likert scale, from 1 (decreased significantly) to 5 (increased significantly).
Physical activity
A single item was used to obtain physical activity changes during the stay at home: compared with the day before the pandemic, how would you rate the changes in physical activity level? A 5-point Likert scale was employed to rate the item (e.g., 1 = decreased significantly, 5 = increased significantly).
Basic demographic characteristics
Four questions were designed to collect participants' basic information, including age (What is your current age?), gender (Male or female?), occupation (Student or working?), and location (Where do you live currently?).
Data analysis
The SPSS 20.0 was used for descriptive statistics (including continuous variables and percentages of discrete variables) and Spearman correlation analyses of all variables in this study. In descriptive statistics, the difference in sleep latency less than zero was discriminated as a decrease in sleep latency after COVID-19, more than zero was discriminated as an increase, and zero as unchanged. In addition, we conducted a series of ordinal logistic regression analyses to determine the strength of associations between screen time, sleep latency, sleep quality, physical activity, and anxiety by SAS University Edition. In regression analyses, we set the unchanged level of screen time as a reference to determine the effects of screen time on levels of anxiety. The unadjusted model detected the effect of screen time changes, sleep quality changes, sleep latency changes, and changes in physical activity on anxiety separately. Model 1 (basic adjusted model) included age, gender, occupation, screen time, and anxiety. Model 2 (partially adjusted model) included sleep latency and sleep quality based on Model 1, while Model 3 (fully adjusted model) incorporates physical activity indicators.
Furthermore, the hypothesized multiple mediation model was conducted to verify the mechanism between screen time and anxiety by Mplus 8.0. The fit indices: Chi-square value, root mean square error of approximation (RMSEA), comparative fit index (CFI), Tuck–-Lews index (TLI), and standardized root mean square residual (SRMR) were reported to evaluate model fit. The direct and indirect effects were assessed by the bootstrapping procedure. The direct effect of screen time changes, mediation effects of sleep latency, sleep quality, and physical activity on anxiety were significant if the range of 95% CI did not include zero, controlling the gender and occupation [47]. Moreover, the hypothesized model had adjusted for socio-demographic variables.
Result
Descriptive statistics
Table 1 shows the critical characteristics of the 970 participants. Individuals who participated in this study ranged from 18 to 40 years old (M = 23.00, SD = 4.76), 74.4% of them were female, and 79.1% were students (Table 1). 85.8% of the participants increased their screen time after the outbreak of COVID-19, and over half (53.3%) reported their level of anxiety to be higher than before. 26.1% indicated that they had lower sleep quality, while 21.6% had higher sleep quality than before the pandemic. 36.9% of participants took more time to fall asleep after going to bed, and more than half (51.5%) of the participants reduced their frequency of physical activity after the virus outbreak.
Table 1.
Descriptive statistics for the key characteristics of participants
| N | % | |
|---|---|---|
| Total | 970 | 100 |
| Age (years) | ||
| 18–25 | 549 | 56.6 |
| 26–30 | 315 | 32.5 |
| 31–40 | 106 | 10.9 |
| Gender | ||
| Male | 248 | 25.6 |
| Female | 722 | 74.4 |
| Occupation | ||
| Student | 767 | 79.1 |
| Working | 203 | 20.9 |
| Screen time | ||
| Decreased significantly | 7 | 0.7 |
| Decreased slightly | 31 | 3.2 |
| Unchanged | 100 | 10.3 |
| Increased slightly | 358 | 36.9 |
| Increased significantly | 474 | 48.9 |
| Anxiety | ||
| Decreased significantly | 42 | 4.3 |
| Decreased slightly | 58 | 6.0 |
| Unchanged | 353 | 36.4 |
| Increased slightly | 449 | 46.3 |
| Increased significantly | 68 | 7.0 |
| Sleep quality | ||
| Decreased significantly | 25 | 2.6 |
| Decreased slightly | 228 | 23.5 |
| Unchanged | 508 | 52.4 |
| Increased slightly | 151 | 15.6 |
| Increased significantly | 58 | 6.0 |
| Sleep latency | ||
| Decreased | 179 | 18.5 |
| Unchanged | 433 | 44.6 |
| Increased | 358 | 36.9 |
| Physical activity | ||
| Decreased significantly | 140 | 14.4 |
| Decreased slightly | 360 | 37.1 |
| Unchanged | 251 | 25.9 |
| Increased slightly | 153 | 15.8 |
| Increased significantly | 66 | 6.8 |
Correlations for age, gender, occupation, screen time, sleep, physical activity, and anxiety
The results of Spearman’s correlations are shown in Table 2. Higher level of anxiety was related to longer screen time (r = 0.21, p < 0.01) and longer sleep latency (r = 0.11, p < 0.01), whereas lower anxiety was linked with better sleep quality (r = − 0.27, p < 0.01) and more physical activity (r = − 0.23, p < 0.01). Screen time was significantly correlated with all variables (both p < 0.01). Moreover, sleep quality had a negative association with sleep latency (r = − 0.22, p < 0.01).
Table 2.
Correlation coefficient of all variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Screen time | 1 | |||||||
| 2. Anxiety | 0.21** | 1 | ||||||
| 3. Sleep quality | − 0.14** | − 0.27** | 1 | |||||
| 4. Sleep latency | 0.10** | 0.11** | − 0.22** | 1 | ||||
| 5. Physical activity | − 0.28** | − 0.23** | 0.23** | − 0.13** | 1 | |||
| 6. Age | − 0.18** | − 0.03 | 0.10** | 0.06 | 0.14** | 1 | ||
| 7. Gender | 0.10** | 0.04 | 0.01 | 0.04 | 0.03 | − 0.11** | 1 | |
| 8. Occupation | − 0.14** | − 0.13** | 0.11** | 0.06 | 0.12** | 0.59** | − 0.06 | 1 |
**p < 0.01
Association between screen time changes and anxiety by ordinal logistic regression
The effects of screen time on anxiety were significant in all models (see Table 3). A fully adjusted model (Model 3) was applied to verify the associations between screen time and anxiety, without covariance of sleep and physical activity. Under Model 3, the strength of association between screen time and anxiety had a further attenuation than Model 2. Physical activity had a significant effect on anxiety in Model 3. The participant who considered that the frequency of physical activity had decreased significantly was 2.76 times more likely to report higher anxiety (95% CI 1.79–4.26).
Table 3.
Association between screen time, sleep, physical activity and anxiety by ordinal logistic regression
| Predictors | Anxiety OR (95% CI) | |||
|---|---|---|---|---|
| Unadjusted model | Model 1 | Model 2 | Model 3 | |
| Age (years) | 1.01 (0.97–1.04) | 1.01 (0.98–1.05) | 1.01 (0.98–1.05) | |
| Gender | ||||
| Male | 0.91 (0.69–1.20) | 0.84 (0.64–1.11) | 0.79 (0.60–1.05) | |
| Female | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | |
| Occupation | ||||
| Student | 1.70 (1.16–2.49)** | 1.71 (1.16–2.51)** | 1.69(1.14–2.48)** | |
| Working | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | |
| Screen time | ||||
| Decreased significantly | 0.75 (0.18–3.11) | 0.78 (0.19–3.24) | 0.81(0.19–3.42) | 0.93 (0.22–3.98) |
| Decreased slightly | 0.79 (0.37–1.68) | 0.77 (0.36–1.62) | 0.84 (0.39–1.79) | 0.91 (0.43–1.96) |
| Unchanged | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Increased slightly | 1.28 (0.84–1.68) | 1.18 (0.78–1.79) | 1.14 (0.75–1.75) | 1.11 (0.72–1.72) |
| Increased significantly | 2.51 (1.67–2.77)*** | 2.28 (1.50–3.46)*** | 1.98 (1.29–3.03)** | 1.67 (1.08–2.59)* |
| Sleep quality | ||||
| Decreased significantly | 19.61 (8.55–43.48)*** | 15.63 (6.80–35.71)*** | 13.89 (5.92–32.26)*** | |
| Decreased slightly | 2.15 (1.58–2.92)*** | 1.86 (1.36–2.56)*** | 1.72 (1.25–2.36)*** | |
| Unchanged | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | |
| Increased slightly | 0.71(0.50–0.99)* | 0.68 (0.48–0.96)* | 0.68 (0.47–0.97)* | |
| Increased significantly | 0.31 (0.19–0.52)*** | 0.32 (0.19–0.53)*** | 0.31 (0.18–0.53)*** | |
| Sleep latency (mins) | 1.01 (1.00–1.02) | 1.00 (1.00–1.01) | 1.00 (0.99–1.01) | |
| Physical activity | ||||
| Decreased significantly | 3.70 (2.46–5.59)*** | 2.76 (1.79–4.26)*** | ||
| Decreased slightly | 1.50 (1.11–2.03)** | 1.26 (0.91–1.72) | ||
| Unchanged | 1.00 (ref) | 1.00 (ref) | ||
| Increased slightly | 1.02 (0.70–1.48) | 1.11 (0.75–1.65) | ||
| Increased significantly | 0.46 (0.28–0.76)** | 0.59 (0.35–0.99)* | ||
*p < 0.05, **p < 0.01, ***p < 0.001. The unadjusted model showed the result of logistic analysis for screen time, sleep quality, sleep latency and physical activity separately, without adjusting for age, gender and occupation
Test of multiple mediation model
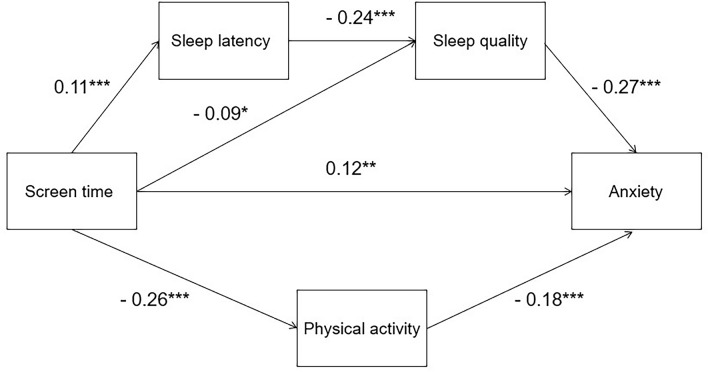
Controlling for age, gender and occupation, the model fit the data well, with χ2 = 6.36, p = 0.70, RMSEA = 0.02, CFI = 0.99, TLI = 0.98, SRMR = 0.06. In the estimated model, the direct paths from anxiety to sleep quality (β = − 0.27, p < 0.001), screen time (β = 0.12, p < 0.01), and physical activity (β = − 0.18, p < 0.001) were significant, while the path from anxiety to sleep latency was not significant (Fig. 2). Regarding the mediation effect of sleep quality, screen time was a significant predictor of anxiety. Thus, sleep quality was a mediator between screen time and anxiety, and the mediation effect was 0.024 (p < 0.05, Table 4). In contrast, the effect of screen time on anxiety was not significant when sleep latency acted as a mediating variable. Furthermore, sleep latency and sleep quality worked as serial mediators between screen time and anxiety, and the serial mediation effect was 0.007 (p < 0.01, Table 4). For the mediating variable of physical activity, screen time was also a significant predictor of anxiety (β = 0.048, p < 0.001, Table 4). No age, gender, or occupation effects on anxiety were observed.
Fig. 2.
The final model. **p < 0.01, ***p < 0.001. Age, gender and occupation were controlled
Table 4.
Results of multiple mediation model test
| Estimate | SE | P value | |
|---|---|---|---|
| Indirect effect paths | |||
| Screen time → sleep quality → anxiety | 0.024 | 0.011 | 0.028 |
| Screen time → physical activity → anxiety | 0.048 | 0.013 | 0.000 |
| Screen time → sleep latency → sleep quality → anxiety | 0.007 | 0.003 | 0.004 |
Discussion
In the current cross-sectional study, we conducted an online survey of screen time changes, anxiety, sleep, physical activity, and demographic variables among participants from China. The present results indicated that 85.8% of participants in our study spent more time on electronic devices, and significantly increased screen time predicted anxiety symptoms. The multiple mediation analysis confirmed the hypothesis that increasing screen time on anxiety might be partly attributed to the impact on individual sleep and physical activity, and the mediating effect of physical activity on anxiety symptoms was stronger than sleep.
Screen time changes and anxiety symptoms
The adverse effect of significantly increased screen time on anxiety during the pandemic of COVID-19 was observed in the current study. In ordinal logistic regression analyses, significantly increased screen time was associated with anxiety symptoms. The association between such screen time change and anxiety remained strong even after controlling demographic variables, since most people have increased the use of mobile phone for watching videos and playing games during COVID-19 [46]. With fewer opportunities for face-to-face communication during home quarantine, the non-social use of screen time may further reduce the perceived social support and cause anxiety symptoms [48, 49]. Information related to COVID-19 transmission and mortality obtained from the video might also aggravate anxiety [50]. In addition, people exhibit stress responses to emergency-caused changes, causing significant changes to their lifestyles under the threat of COVID-19 [51]. Increased screen time due to entertainment during home isolation may accelerate lifestyle changes and lead to negative mental health outcomes [51, 52].
In particular, slightly increased screen time, slightly and significantly decreased screen time did not predict anxiety symptoms in regression analysis. The findings suggested that a slight increase in screen time did not cause anxiety symptoms, and reducing screen time did not help to relieve individuals' anxiety, which means the change of screen time in a certain range does not affect the levels of anxiety. One study indicated that screen time of watching TV or videos was associated with anxiety and other psychological symptoms, while chatting and working were not [22]. During COVID-19, the increased screen time that resulted from the transformation of working and studying patterns may not influence individuals’ mental health [12]. Meanwhile, appropriate time of watching videos, playing games, and socializing online may be helpful to relieve the anxiety symptoms [53, 54], to a certain extent, offsetting the negative effect of deficient in mentally healthy activities due to increased screen time.
The impact of sleep and physical activity
In this study, people with poorer sleep quality had much higher odds of increasing anxiety than those who reported unchanged. The effect of sleep quality on anxiety was even stronger than screen time and physical activity. The sleep loss can result in an abnormal top-down prefrontal control of emotional regulation, thereby directly affecting responses to negative emotions [55]. Meanwhile, the negative impact of sleep quality changes reflected the effects of different aspects of sleep among people [56]. For instance, in mediation analysis, the difficulty in falling asleep contributed to worse sleep quality, causing increased levels of anxiety. In addition to difficulty falling asleep, delayed sleep patterns may also cause a decline in sleep quality. Due to home isolation, people do not have to wake up for work or study as early as before the pandemic of COVID-19 [57], and later bedtime and wake time were observed in numerous retrospective studies [9, 58, 59]. Circadian rhythm disorders were associated with increased trait and state anxiety during the pandemic [60]. Moreover, the fear of being infected and other affective issues during COVID-19 caused insomnia, and problems with sleep maintenance may lead to reduced sleep quality. A systematic review concluded that the sleep maintenance experience is likely to make a relatively larger contribution to the overall perception of sleep compared with onset [56], which may partly explain why the robust association between sleep quality and anxiety still persisted after controlling screen time and sleep latency.
In regression analyses, the attenuation in the odds ratios of screen time revealed the important role of sleep quality, sleep latency, and physical activity in the association between screen time changes and anxiety. The results of the multiple mediation analysis elucidated that the increase in screen time directly impacted anxiety and indirectly through sleep quality, which is closely related to mental health. Sleep latency did not directly mediate the association between screen time changes and anxiety. Consistent with previous studies, increased screen time was negatively correlated with sleep quality [27–29], while poorer sleep quality predicted a higher level of anxiety [3, 33, 61]. Additionally, the short sleep latency influenced by increasing screen time would lead to an increase in anxiety levels by reducing sleep quality in multiple mediation analyses. The following explanations may partially explain this phenomenon. During the pandemic period, using electronic devices before bedtime was significantly elevated [9]. Cognitive arousal for browsing the pandemic-related information from digital media makes individuals difficult to fall asleep, causing poorer sleep quality [62]. As we have mentioned, people may exhibit delayed circadian rhythm and irregular sleep duration, contributing to a decline in sleep quality [63]. Difficulty in falling asleep may be part of the reasons for the lower levels of sleep quality, which amplifies anxiety symptoms during the pandemic. Thus, sleep latency and sleep quality mediated the relationship between screen time and mental health, as previous studies showed [26, 32, 64].
Moreover, physical activity also mediated the relationship between screen time and anxiety. The reduction of physical activity is fostered by increasing screen time, and people with decreased physical activity reported a higher level of anxiety. The present findings correspond to studies indicating that increased screen time is often linked with sedentary behavior and less physical activity during COVID-19 [11, 65]. According to the digital displacement model, people using electronic devices would occupy the time for other behavior that benefit mental health, such as physical activity [20]. The higher levels of screen time caused by COVID-19 may increase the possibility of suffering from the Internet or mobile phone addiction [66]. Individuals with this addiction cannot limit or control their electronic devices even when they know the harmful consequences [67]. They cannot manage the time using electronic devices, which may lead to less time for physical activity (the interpretation might also be applied to screen time on sleep). Accordingly, health-related behaviors such as sleep and physical activity have changed with the Covid-19 pandemic [68]. Furthermore, in line with the available literature, increased physical exercise attenuates the negative impact of screen time on anxiety, which may contribute to physical health improvement [38]. On the other hand, reducing sleep quality and physical activity caused by screen time increases may amplify the sense of being out of control, contributing to a higher level of anxiety [69]. The above findings revealed the potential mechanism for the effect of screen time changes on anxiety and provided empirical evidence for the digital displacement model.
The current study was conducted during the global pandemic, and the sharply changing screen time in our study resulted from home quarantine. The negative effects of increasing screen time were not entirely due to the excessive use of electronic devices as before the pandemic, which also reflected the impact of rapid lifestyle changes on anxiety during COVID-19. Moreover, the increased screen time caused by COVID-19 might result in a higher possibility of suffering from Internet or mobile phone addiction and aggravate the delirious effects of screen time on health-related behaviors such as sleep and physical activity, contributing to the higher level of anxiety. Our findings indicated that appropriately limiting screen time, maintaining good sleep, and engaging in physical activity are warranted against the incidence of mental health disorders during the lockdown.
Limitations and future directions
The following limitations need to be considered. First, participants’ responses may be subjective due to the assessment of anxiety with a single item, and assessment with no validated scales may lead to information bias. For instance, participants may overestimate or underestimate actual screen time due to different periods [46]. Facing COVID-19 and changes in daily life, people are under unprecedented pressure and are experiencing severe psychological distress [4]. To reduce the burden, we tried to simplify our questionnaire as much as possible. Meanwhile, due to the sudden outbreak of COVID-19, it was challenging to measure screen time and anxiety before and after the pandemic directly. Therefore, we developed a questionnaire based on the research needs and used the variables of screen time changes and anxiety changes. Many studies revealed that screen time and anxiety levels increased under the burden of COVID-19, [10, 69], which can support our findings. In addition, several researchers have tested the validity of a single-item measure for evaluating mental health and found that a single-item measurement was used associated with multiple-item scale significantly [70–72]. Secondly, we used a convenience sampling method to recruit participants, which may cause selection bias. Due to the lockdown, it was extremely difficult to use the probability sampling method or conduct face-to-face interview. Similar to other studies conducted during the pandemic [73, 74], we used a convenience sampling method to obtain a large sample safely and quickly. Because the recruitment of participants in the current study was via the Internet, and young adults were much more familiar with complete investigation online than other groups, most of our participants were university students. However, since young adults tend to have the highest rates of screen time and smartphone usage, this group is also the primary population investigated in studies of screen time [75]. Our study is consistent with recent studies related to screen time in terms of sample composition [76, 77]. Moreover, to reduce the potential influence of this selection bias, we applied covariance analysis in the model to control the effect of age, gender, and occupation. Although the present results were relatively reliable, it is better to control the proportion of participants by age, gender, and occupation in future studies if possible. Thirdly, some correlation coefficients in our correlation analysis were relatively low but still significant, which may be due to the large size of the sample. Accordingly, we conducted ordinal logistic regression analyses and developed a multiple mediation model to further clarify the relationship between the variables. Fourthly, although the mediating effect of physical activity on anxiety symptoms is more robust than sleep in our study, the result may be attributed to the absence of other factors such as sleep duration and rhythm. Previous studies showed that there might be an interaction between exercise and sleep. For instance, walking before bed can lead to an increase in sleep latency [78–80]. Future research on screen time and anxiety should consider the interaction between sleep and physical activity. Fifthly, the cross-sectional design restricted our understanding of the long-term effect of screen time changes on anxiety. The cross-sectional studies were necessary to detect the immediate effects of screen time changes on anxiety. However, as we mentioned, the emergence of anxiety symptoms may be lasting or postponed during the pandemic. Longitudinal studies examining the association between screen time changes and anxiety symptoms during COVID-19 are warranted.
Although the study has the above limitations, the findings in our study revealed the effect of the magnitude of screen time variation on anxiety, and provided guidance for future investigations of potential mechanisms underlying screen time and anxiety. During the home quarantine of COVID-19, using electronic devices is common for entertainment and relaxation. Meanwhile, due to the continuous spread and outbreaks of the pandemic, online work and learning are still an important part of people's daily life. The increase in screen time became an inevitable trend, but the current findings indicated that a rapid rise in electronic device usage time would amplify negative emotion. Moreover, the significantly increased screen time would result in poor sleep and lack of physical activity. People should consciously reduce screen time and participate in other activities that help alleviate anxiety symptoms during the pandemic, such as exercising and communicating with others. Additionally, this study showed that people with significantly lower sleep quality were up to 19.61 times more likely to have increased anxiety than those who were unchanged, which revealed the importance of maintaining good quality sleep for mental health. Reducing the time spent on mobile phones and other electronic devices before bedtime might be an effective way to improve sleep quality and reduce the negative influence on anxiety symptoms.
Conclusions
This study revealed the adverse effect of significantly increased screen time caused by the pandemic on anxiety symptoms. Sleep latency, sleep quality, and physical activity can mediate the relationship between screen time changes and anxiety during the pandemic. Moreover, difficulty in falling asleep caused by increased screen time would contribute to poorer sleep quality, further amplifying anxiety symptoms. In sum, our findings suggested that the fluctuation of screen time in a certain range does not affect the level of anxiety. The significantly increased screen time would result in poor sleep, including longer sleep latency and worse sleep quality, and lack of physical activity, which would lead to higher levels of anxiety.
Acknowledgements
This work was supported by The MOE (Ministry of Education in China) Project of Humanities and Social Sciences (No. 21YJC190011) and Guangdong Basic and Applied Basic Research Foundation, China (No. 2019A1515012182).
Declarations
Conflict of interest
The authors report no conflict of financial or academic interest. All authors have read and approved the manuscript.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Ethical Committee of the South China Normal University (of the principal investigator N.M., Approval No. SCNU-PSY-2020-1-015).
Informed consent
Each participant signed informed consent before study commencement.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob AG. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li S, Wu Y, Zhang F, Xu Q, Zhou A. Self-affirmation buffering by the general public reduces anxiety levels during the COVID-19 epidemic. Acta Psychol Sin. 2020;52(7):886–894. doi: 10.3724/SP.J.1041.2020.00886. [DOI] [Google Scholar]
- 3.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi L, Lu Z-A, Que J-Y, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(7):e2014053. doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan A, Liu L, Wang C, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan. China JAMA. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mheidly N, Fares MY, Fares J. Coping with stress and burnout associated with telecommunication and online learning. Front Public Health. 2020;8:574969. doi: 10.3389/fpubh.2020.574969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruggieri S, Ingoglia S, Bonfanti RC, Coco GL. The role of online social comparison as a protective factor for psychological wellbeing: a longitudinal study during the COVID-19 quarantine. Pers Individ Dif. 2021;171:110486. doi: 10.1016/j.paid.2020.110486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiat. 2020;33(2):e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29(4):e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elhai JD, Yang H, McKay D, Asmundson GJ. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J Affective Disord. 2020;274:576–582. doi: 10.1016/j.jad.2020.05.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qin F, Song Y, Nassis GP, et al. Physical activity, screen time, and emotional well-being during the 2019 novel coronavirus outbreak in China. Int J Environ Res Public Health. 2020;17(14):5170. doi: 10.3390/ijerph17145170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDowell CP, Herring MP, Lansing J, Brower C, Meyer JD. Working from home and job loss due to the COVID-19 pandemic are associated with greater time in sedentary behaviors. Front Public Health. 2020;8:597619. doi: 10.3389/fpubh.2020.597619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meyer J, McDowell C, Lansing J, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health. 2020;17(18):1–13. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elhai JD, Levine JC, Hall BJ. The relationship between anxiety symptom severity and problematic smartphone use: a review of the literature and conceptual frameworks. J Anxiety Disord. 2019;62:45–52. doi: 10.1016/j.janxdis.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Boers E, Afzali MH, Conrod P. Temporal associations of screen time and anxiety symptoms among adolescents. Can J Psychiatry. 2020;65(3):206–208. doi: 10.1177/0706743719885486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cao H, Qian Q, Weng T, et al. Screen time, physical activity and mental health among urban adolescents in China. Prev Med. 2011;53(4–5):316–320. doi: 10.1016/j.ypmed.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Maras D, Flament MF, Murray M, et al. Screen time is associated with depression and anxiety in canadian youth. Prev Med. 2015;73:133–138. doi: 10.1016/j.ypmed.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 18.Twenge JM, Martin GN, Campbell WK. Decreases in psychological well-being among American adolescents after 2012 and links to screen time during the rise of smartphone technology. Emotion. 2018;18(6):765. doi: 10.1037/emo0000403. [DOI] [PubMed] [Google Scholar]
- 19.Wu X, Tao S, Zhang Y, Zhang S, Tao F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE. 2015;10(3):e0119607. doi: 10.1371/journal.pone.0119607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Twenge JM. More time on technology, less happiness? Associations between digital-media use and psychological well-being. Curr Dir Psychol Sci. 2019;28(4):372–379. doi: 10.1177/0963721419838244. [DOI] [Google Scholar]
- 21.Liu S, Wing YK, Hao Y, Li W, Zhang J, Zhang B. The associations of long-time mobile phone use with sleep disturbances and mental distress in technical college students: a prospective cohort study. Sleep. 2019;42(2):2. doi: 10.1093/sleep/zsy213. [DOI] [PubMed] [Google Scholar]
- 22.Kim S, Favotto L, Halladay J, Wang L, Boyle MH, Georgiades K. Differential associations between passive and active forms of screen time and adolescent mood and anxiety disorders. Soc Psych Psych Epid. 2020;55(6):1–10. doi: 10.1007/s00127-020-01833-9. [DOI] [PubMed] [Google Scholar]
- 23.Lamers F, Difrancesco S, Riese H, van Hemert B, Schoevers R, Penninx B. T118 objectively measured physical activity and sleep and its associations with depressive and anxiety disorders. Biol Psychiat. 2018;83(9):S174. doi: 10.1016/j.biopsych.2018.02.454. [DOI] [Google Scholar]
- 24.Sampasa-Kanyinga H, Colman I, Goldfield GS, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2020;17(1):72. doi: 10.1186/s12966-020-00976-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vandendriessche A, Ghekiere A, Van Cauwenberg J, et al. Does sleep mediate the association between school pressure, physical activity, screen time, and psychological symptoms in early adolescents? A 12-Country study. Int J Environ Res Public Health. 2019;16(6):1072. doi: 10.3390/ijerph16061072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Foley LS, Maddison R, Jiang Y, Marsh S, Olds T, Ridley K. Presleep activities and time of sleep onset in children. Pediatrics. 2013;131(2):276–282. doi: 10.1542/peds.2012-1651. [DOI] [PubMed] [Google Scholar]
- 27.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–58. doi: 10.1016/j.smrv.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Janssen X, Martin A, Hughes AR, Hill CM, Kotronoulas G, Hesketh KR. Associations of screen time, sedentary time and physical activity with sleep in under 5s: a systematic review and meta-analysis. Sleep Med Rev. 2020;49:101226. doi: 10.1016/j.smrv.2019.101226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kenney EL, Gortmaker SL. United States adolescents’ television, computer, videogame, smartphone, and tablet use: associations with sugary drinks, sleep, physical activity, and obesity. J Pediatr. 2017;182:144–149. doi: 10.1016/j.jpeds.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 30.LeBourgeois MK, Hale L, Chang A-M, Akacem LD, Montgomery-Downs HE, Buxton OM. Digital media and sleep in childhood and adolescence. Pediatrics. 2017;140(Supplement 2):S92–S96. doi: 10.1542/peds.2016-1758J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tandon A, Kaur P, Dhir A, Mäntymäki M. Sleepless due to social media? Investigating problematic sleep due to social media and social media sleep hygiene. Comput Hum Behav. 2020;113:106487. doi: 10.1016/j.chb.2020.106487. [DOI] [Google Scholar]
- 32.Li X, Buxton OM, Lee S, Chang A-M, Berger LM, Hale L. Sleep mediates the association between adolescent screen time and depressive symptoms. Sleep Med. 2019;57:51–60. doi: 10.1016/j.sleep.2019.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xiong W, Liu H, Gong P, et al. Relationships of coping styles and sleep quality with anxiety symptoms among Chinese adolescents: a cross-sectional study. J Affect Disord. 2019;257:108–115. doi: 10.1016/j.jad.2019.07.032. [DOI] [PubMed] [Google Scholar]
- 34.Christofaro DG, De Andrade SM, Mesas AE, Fernandes RA, Farias Junior JC. Higher screen time is associated with overweight, poor dietary habits and physical inactivity in Brazilian adolescents, mainly among girls. Eur J Sport Sci. 2016;16(4):498–506. doi: 10.1080/17461391.2015.1068868. [DOI] [PubMed] [Google Scholar]
- 35.Judice PB, Magalhaes JP, Rosa GB, Henriques-Neto D, Hetherington-Rauth M, Sardinha LB. Sensor-based physical activity, sedentary time, and reported cell phone screen time: a hierarchy of correlates in youth. J Sport Health Sci. 2021;10(1):55–64. doi: 10.1016/j.jshs.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Brit J Sports Med. 2011;45(11):886–895. doi: 10.1136/bjsports-2011-090185. [DOI] [PubMed] [Google Scholar]
- 37.Ma C, Zhou L, Xu W, Ma S, Wang Y. Associations of physical activity and screen time with suboptimal health status and sleep quality among Chinese college freshmen: a cross-sectional study. PLoS ONE. 2020;15(9):e0239429. doi: 10.1371/journal.pone.0239429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meira CM, Jr, Meneguelli KS, Leopoldo MPG, Florindo AA. Anxiety and leisure-domain physical activity frequency, duration, and intensity during Covid-19 pandemic. Front Psychol. 2020;11:3758. doi: 10.3389/fpsyg.2020.603770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taheri E, Heshmat R, Esmaeil Motlagh M, et al. Association of physical activity and screen time with psychiatric distress in children and adolescents: CASPIAN-IV study. J Trop Pediatrics. 2019;65(4):361–372. doi: 10.1093/tropej/fmy063. [DOI] [PubMed] [Google Scholar]
- 40.White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-specific physical activity and mental health: a meta-analysis. Am J Prev Med. 2017;52(5):653–666. doi: 10.1016/j.amepre.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 41.López-Bueno R, Calatayud J, Ezzatvar Y, et al. Association between current physical activity and current perceived anxiety and mood in the initial phase of COVID-19 confinement. Front Psychia. 2020;11:729. doi: 10.3389/fpsyt.2020.00729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith L, Jacob L, Trott M, et al. The association between screen time and mental health during COVID-19: a cross sectional study. Psychiatry Res. 2020;292:113333. doi: 10.1016/j.psychres.2020.113333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dunn AL, Trivedi MH, O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33(Supplement):609–610. doi: 10.1097/00005768-200106001-00027. [DOI] [PubMed] [Google Scholar]
- 44.Larson LR, Szczytko R, Bowers EP, Stephens LE, Stevenson KT, Floyd MF. Outdoor time, screen time, and connection to nature: troubling trends among rural youth? Env Behav. 2018;51(8):966–991. doi: 10.1177/0013916518806686. [DOI] [Google Scholar]
- 45.Przybylski AK. Digital screen time and pediatric sleep: evidence from a preregistered cohort study. J Pediatr. 2019;205:218–223. doi: 10.1016/j.jpeds.2018.09.054. [DOI] [PubMed] [Google Scholar]
- 46.Hodes LN, Thomas KGF. Smartphone screen time: Inaccuracy of self-reports and influence of psychological and contextual factors. Comput Hum Behav. 2021;115:106616. doi: 10.1016/j.chb.2020.106616. [DOI] [Google Scholar]
- 47.Chen JY, Strodl E, Huang LH, Chen YJ, Yang GY, Chen WQ. Early electronic screen exposure and autistic-like behaviors among preschoolers: the mediating role of caregiver-child interaction, sleep duration and outdoor activities. Child (Basel) 2020;7(11):200. doi: 10.3390/children7110200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li X, Chen W, Popiel P. What happens on facebook stays on facebook? The implications of facebook interaction for perceived, receiving, and giving social support. Comput Human Behav. 2015;51:106–113. doi: 10.1016/j.chb.2015.04.066. [DOI] [Google Scholar]
- 49.Özmete E, Pak M. The relationship between anxiety levels and perceived social support during the pandemic of COVID-19 in Turkey. Social Work Public Health. 2020;35(7):603–616. doi: 10.1080/19371918.2020.1808144. [DOI] [PubMed] [Google Scholar]
- 50.Su Z, McDonnell D, Wen J, et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Glob Health. 2021;17(1):1–8. doi: 10.1186/s12992-020-00654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dai W, Zhou J, Li G, Zhang B, Ma N. Maintaining normal sleep patterns, lifestyles and emotion during the COVID-19 pandemic: The stabilizing effect of daytime napping. J Sleep Res. 2021;30:e13259. doi: 10.1111/jsr.13259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Velten J, Bieda A, Scholten S, Wannemüller A, Margraf J. Lifestyle choices and mental health: a longitudinal survey with German and Chinese students. BMC Public Health. 2018;18(1):1–15. doi: 10.1186/s12889-018-5526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mauri M, Cipresso P, Balgera A, Villamira M, Riva G. Why is facebook so successful? Psychophysiological measures describe a core flow state while using facebook. Cyberpsychol Behav Soc Netw. 2011;14(12):723–731. doi: 10.1089/cyber.2010.0377. [DOI] [PubMed] [Google Scholar]
- 54.Ryan T, Xenos S. Who uses facebook? An investigation into the relationship between the big five, shyness, narcissism, loneliness, and facebook usage. Comput Hum Behav. 2011;27(5):1658–1664. doi: 10.1016/j.chb.2011.02.004. [DOI] [Google Scholar]
- 55.Chellappa SL, Aeschbach D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev 2021; 101583 [DOI] [PubMed]
- 56.Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. 2008;9:S10–S17. doi: 10.1016/S1389-9457(08)70011-X. [DOI] [PubMed] [Google Scholar]
- 57.Ong JL, Lau T, Massar SAA, et al. COVID-19-related mobility reduction: heterogenous effects on sleep and physical activity rhythms. Sleep. 2021;44(2):1–13. doi: 10.1093/sleep/zsaa179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gupta R, Grover S, Basu A, et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62(4):370–378. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sinha M, Pande B, Sinha R. Impact of COVID-19 lockdown on sleep-wake schedule and associated lifestyle related behavior: a national survey. J Public Health Res. 2020;9(3):1826. doi: 10.4081/jphr.2020.1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boiko DI, Skrypnikov AM, Shkodina AD, Hasan MM, Ashraf GM, Rahman M. Circadian rhythm disorder and anxiety as mental health complications in post-COVID-19. Environ Sci Pollut R. 2022;29:28062–28068. doi: 10.1007/s11356-021-18384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cox RC, Upender RP, Olatunji BO. Linking inhibition and anxiety symptoms following sleep restriction: the moderating role of prior sleep efficiency. Behav Res Ther. 2020;127:103575. doi: 10.1016/j.brat.2020.103575. [DOI] [PubMed] [Google Scholar]
- 62.Augner C. Associations of subjective sleep quality with depression score, anxiety, physical symptoms and sleep onset latency in students. Cent Eur J Public Health. 2011;19(2):115–117. doi: 10.21101/cejph.a3647. [DOI] [PubMed] [Google Scholar]
- 63.Soehner AM, Kennedy KS, Monk TH. Circadian preference and sleep-wake regularity: associations with self-report sleep parameters in daytime-working adults. Chronobiol Int. 2011;28(9):802–809. doi: 10.3109/07420528.2011.613137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhao J, Zhang Y, Jiang F, et al. Excessive screen time and psychosocial well-being: the mediating role of body mass index, sleep duration, and parent-child interaction. J Pediatr. 2018;202:157–162. doi: 10.1016/j.jpeds.2018.06.029. [DOI] [PubMed] [Google Scholar]
- 65.Schmidt SCE, Anedda B, Burchartz A, et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. 2020;10(1):21780. doi: 10.1038/s41598-020-78438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Boer M, Stevens GWJM, Finkenauer C, de Looze ME, van den Eijnden RJJM. Social media use intensity, social media use problems, and mental health among adolescents: Investigating directionality and mediating processes. Comput Hum Behav. 2021;116:106645. doi: 10.1016/j.chb.2020.106645. [DOI] [Google Scholar]
- 67.van Deursen AJAM, Bolle CL, Hegner SM, Kommers PAM. Modeling habitual and addictive smartphone behavior. Comput Hum Behav. 2015;45:411–420. doi: 10.1016/j.chb.2014.12.039. [DOI] [Google Scholar]
- 68.López-Bueno R, Calatayud J, Casaña J, et al. COVID-19 confinement and health risk behaviors in Spain. Front Psychol. 2020;11:1426. doi: 10.3389/fpsyg.2020.01426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brailovskaia J, Margraf J. The relationship between burden caused by coronavirus (Covid-19), addictive social media use, sense of control and anxiety. Comput Hum Behav. 2021;119:106720. doi: 10.1016/j.chb.2021.106720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lin Y-H, Chen H-C, Hsu N-W, Chou P. Validation of global self-rated health and happiness measures among older people in the Yilan study. Taiwan Front Public Health. 2020;8:346. doi: 10.3389/fpubh.2020.00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS. Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res. 2014;14(1):1–11. doi: 10.1186/1472-6963-14-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Botha F, Butterworth P, Wilkins R. Evaluating How Mental health changed in Australia through the COVID-19 pandemic: findings from the ‘taking the pulse of the nation’ (TTPN) survey. Int J Env Res Pub He. 2022;19(1):558. doi: 10.3390/ijerph19010558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brivio E, Oliveri S, Guiddi P, Pravettoni G. Incidence of PTSD and generalized anxiety symptoms during the first wave of COVID-19 outbreak: an exploratory study of a large sample of the Italian population. BMC Public Health. 2021;21(1):1–10. doi: 10.1186/s12889-021-11168-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen X, Liu P, Lei G-F, Tong L, Wang H, Zhang X-Q. Sleep quality and the depression-anxiety-stress state of frontline nurses who perform nucleic acid sample collection during COVID-19: a cross-sectional study. Psychol Res Behav Manag. 2021;14:1889. doi: 10.2147/PRBM.S338495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Olson JA, Sandra DA, Colucci ÉS, et al. Smartphone addiction is increasing across the world: a meta-analysis of 24 countries. Comput Hum Behav. 2022;129:107138. doi: 10.1016/j.chb.2021.107138. [DOI] [Google Scholar]
- 76.Guo N, Luk TT, Wang MP, et al. Self-Reported screen time on social networking sites associated with problematic smartphone use in chinese adults: a population-based study. Front Psychia. 2021;11:1518. doi: 10.3389/fpsyt.2020.614061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Claesdotter-Knutsson E, André F, Håkansson A. Gaming activity and possible changes in gaming behavior among young people during the COVID-19 pandemic: cross-sectional online survey study. JMIR Serious Games. 2022;10(1):e33059. doi: 10.2196/33059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bonnet MH, Arand DL. Activity, arousal, and the MSLT in patients with insomnia. Sleep. 2000;23(2):205–212. doi: 10.1093/sleep/23.2.1g. [DOI] [PubMed] [Google Scholar]
- 79.Lambiase MJ, Gabriel KP, Kuller LH, Matthews KA. Sleep and executive function in older women: the moderating effect of physical activity. J Gerontol A Biol Sci Med Sci. 2014;69(9):1170–1176. doi: 10.1093/gerona/glu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mead MP, Baron K, Sorby M, Irish LA. Daily associations between sleep and physical activity. Int J Behav Med. 2019;26(5):562–568. doi: 10.1007/s12529-019-09810-6. [DOI] [PubMed] [Google Scholar]